Abstract
Background
The longitudinal course of multiple symptom domains in adolescents treated for major depression is not known. Revealing the temporal course of general and specific psychopathology factors, including potential differences between psychotherapies, may aid therapeutic decision‐making.
Methods
Participants were adolescents with major depressive disorder (aged 11–17; 75% female; N = 465) who were part of the IMPACT trial, a randomized controlled trial comparing cognitive behavioral therapy, short‐term psychoanalytic psychotherapy, and brief psychosocial intervention. Self‐reported symptoms at baseline and 6, 12, 36, 52, and 86 weeks postrandomization were analyzed with bifactor modeling.
Results
General psychopathology factor scores decreased across treatment and one‐year follow‐up. Specific melancholic features and depressive cognitions factors decreased from baseline to 6 weeks. Conduct problems decreased across treatment and follow‐up. Anxiety increased by 6 weeks and then reverted to baseline levels. Obsessions–compulsions did not change. Changes in general and specific factors were not significantly different between the three psychotherapies during treatment. During follow‐up, however, conduct problems decreased more in brief psychosocial intervention versus cognitive behavioral therapy (1.02, 95% Bayes credible interval 0.25, 1.96), but not versus short‐term psychoanalytic psychotherapy.
Conclusions
The clinical response signature in this trial is best revealed by rapid reductions in depression symptoms and general psychopathology. Protracted improvements in general psychopathology and conduct problems subsequently occur. Psychosocial treatments for adolescent depression have comparable effects on general and specific psychopathology, although a psychoeducational, goal‐focused approach may be indicated for youth with comorbid conduct problems.
Keywords: Bifactor models, depression, psychotherapy, adolescent, psychopathology
Introduction
There is increasing empirical support for a general psychopathology factor that accounts for shared variance in diverse symptoms of mental illness (Caspi et al., 2014; Caspi & Moffitt, 2018; Castellanos‐Ryan et al., 2016; Laceulle, Vollebergh, & Ormel, 2015). Evidence for this general factor runs counter to most current clinical practices, which often focus on categorical diagnosis and associated narrow‐band questionnaires, and presumes disorder‐specific interventions (Caspi & Moffitt, 2018; Hopwood et al., 2019; Messer & Wampold, 2006; Rodriguez‐Seijas, Eaton, & Krueger, 2015). However, treatments often reduce symptoms in comorbid domains not explicitly targeted (Hilton et al., 2013; Weisz, McCarty, & Valeri, 2006), suggesting that interventions may decrease psychiatric symptoms overall, rather than those within a single category of psychopathology (Constantinou et al., 2019; Hopwood et al., 2019). We examined change in general and specific psychopathology factors among adolescents participating in psychosocial treatments for major depression in the IMPACT trial (Goodyer et al., 2017b, 2011). Use of the general psychopathology factor as an outcome variable has potential to provide new insights into symptom patterns over time and whether these patterns vary for different psychotherapies.
General psychopathology factor
The concept of a general factor of psychopathology was popularized by Caspi et al. (2014), building on evidence of overall internalizing and externalizing dimensions of psychopathology (Achenbach & Edelbrock, 1978; Lahey, Van Hulle, Singh, Waldman, & Rathouz, 2011). The general, ‘p’, factor is dimensional and empirically derived using bifactor modeling and captures shared variance in symptoms across the spectrum of psychopathology (Kotov et al., 2017; Krueger et al., 2018). Specific factors with variance unique to each symptom domain, not accounted for by the general factor, are also identified.
The p factor appears to reflect an overall liability to psychopathology, which may be explained by underlying emotion dysregulation, negative emotionality, and unwanted irrational thoughts (Carver, Johnson, & Timpano, 2017; Caspi et al., 2014; Caspi & Moffitt, 2018). Analyses in clinic and community samples support the reliability and validity of the general psychopathology factor (Carragher et al., 2016; Haltigan et al., 2018; Patalay et al., 2015; Waldman, Poore, van Hulle, Rathouz, & Lahey, 2016). Research on the general factor as a treatment outcome measure is now needed to understand treatment effectiveness in the context of empirically driven, dimensional models of psychopathology (Caspi & Moffitt, 2018; Hopwood et al., 2019).
IMPACT trial
The IMPACT trial was a multisite, randomized pragmatic superiority effectiveness trial comparing three structured psychosocial therapies for adolescents with a primary diagnosis of major depressive disorder (Goodyer et al., 2017b, 2011): cognitive behavioral therapy (CBT), focused on behavioral activation and identifying and modifying information processing biases; short‐term psychoanalytic psychotherapy (STPP), focused on giving meaning to the varieties of the client’s emotional experiences and addressing difficulties in the context of the developmental tasks of adolescence (Cregeen, Hughes, Midgley, Rhode, & Rustin, 2017); and brief psychosocial intervention (BPI), a goal‐oriented therapy focused on psychoeducation about depression and increasing positive activities (Goodyer et al., 2017a).
CBT, STPP, and BPI were associated with similar decreases in depression and psychosocial impairment at the end of the treatment (36 weeks) and one‐year follow‐up in the IMPACT trial (Goodyer et al., 2017b). In contrast, secondary outcomes of anxiety, obsessions/compulsions, and antisocial behaviors were significantly lower at the end of the treatment, in favor of the psychological therapies (CBT + STPP) compared to BPI, but no such difference was sustained at the conclusion of the study. This suggests BPI may have similar effects as the other therapies on depression symptoms, but psychological therapies such as CBT and STPP may have more immediate benefits for comorbid symptoms. The inclusion of nondepressive symptoms may make the general factor more sensitive to change and relevant to patients’ experience. Here we speculate that the psychological therapies may be more effective (or efficient) at reducing a general factor score more rapidly than BPI.
The results of the IMPACT trial suggested that a dimensional, transdiagnostic analysis may enhance understanding of differences in treatment response. Narrow‐band (i.e., total scores within a symptom domain) measures of depression, anxiety, obsessions/compulsions, and conduct problems showed similar decreases across treatment and follow‐up, suggesting a common course of nondepressive and depressive symptoms (Goodyer et al., 2017b). The self‐report depression and anxiety scales used in the IMPACT trial have also previously shown a good fit for a latent bifactor model in community adolescents (n = 1,159), with a general factor and specific melancholic, cognitive, and anxiety factors (Brodbeck et al., 2014). A general psychopathology factor may therefore explain the transdiagnostic decline in symptoms in the IMPACT trial. Further, examining the longitudinal course of general and specific factors may provide novel information on change during treatment and follow‐up not seen using narrow‐band instruments. Here we speculate that specific factors have prognostic validity and are not merely carrying redundant variance.
Present study
Use of the general psychopathology factor as an outcome in clinical trials is limited and has not focused on youth with major depression (Constantinou et al., 2019; Wade, Fox, Zeanah, & Nelson, 2018). The present study examines change in general and specific psychopathology factors among adolescents with a primary diagnosis of major depression receiving one of three psychosocial interventions: CBT, STPP, and a reference standardized care as usual treatment, BPI. Considering prior findings from the IMPACT trial (Goodyer et al., 2017b) and analyses of the general factor in other clinical trials (Constantinou et al., 2019; Wade et al., 2018), we hypothesize that:
Symptom reductions will be reflected in decreases in the general factor across treatment and follow‐up.
Specific factors will show different patterns of change compared to the general factor, with greater reductions early in treatment and minimal subsequent change over follow‐up.
The established psychological therapies (CBT, STPP) will be associated with greater reductions compared with BPI in all factors during the treatment phase but not during follow‐up.
Methods
We analyzed data from the IMPACT trial (Goodyer et al., 2017b, 2017a, 2011) collected at baseline and nominal 6, 12, 36, 52, and 86 weeks postrandomization (for full protocol, see Goodyer et al., 2011). Participating adolescents were randomly assigned, between June 2010 and January 2013, to receive CBT (n = 154), STPP (n = 156), or BPI (n = 155; for CONSORT diagram, see Goodyer et al., (2017a, 2017b); see Table S1 for baseline characteristics by treatment group). There were no significant differences in selective serotonin reuptake inhibitor (SSRI) prescribing between treatments and no effect of SSRI prescribing on the primary outcome of self‐reported depressive symptoms (Goodyer et al., 2017b). Mean treatment length was 24.9 weeks (CBT), 27.9 weeks (STPP), and 27.5 weeks (BPI). Participants attended a median of nine therapy sessions (range = 0–43; BPI median = 6, IQR, 4–11; CBT median = 9, IQR 5–14; STPP median = 11, IQR 5–23).
Study population
Participants were recruited from 15 specialized outpatient mental health clinics in three urban or rural regions in England. All participants had an existing DSM‐IV diagnosis of moderate to severe major depressive disorder (Goodyer et al., 2017b, 2011). A total of 465 adolescents aged 11–17 (M = 15 years; 75% female; 85% self‐reported their ethnicity as White) were included in the present study (470 randomized; 5 withdrew consent). Comorbidity was relatively common, with 48% of participants meeting DSM‐IV criteria for one or more comorbid disorders.
Ethical considerations
All participating youth and parents provided informed consent to participate in the IMPACT trial. All study procedures were approved by the Cambridgeshire 2 Research Ethics Committee.
Measures
Adolescent self‐reports, completed at six time points, were used: (a) the Mood and Feelings Questionnaire (Costello & Angold, 1988), a 33‐item measure of depression symptoms; (b) the Revised Children’s Manifest Anxiety Scale (Reynolds & Paget, 1981; Reynolds & Richmond, 1978), a 28‐item anxiety questionnaire; (c) the short Leyton Obsessional Inventory (Bamber, Tamplin, Park, Kyte, & Goodyer, 2002), an 11‐item measure of obsessions and compulsions; and (d) an 11‐item antisocial behavior checklist derived from DSM‐IV criteria for conduct disorder (Goodyer et al., 2011). All items were rated on a 4‐point scale (never, sometimes, mostly, or almost always). Responses of mostly and almost always were collapsed (Goodyer et al., 2017b). Mean self‐ and parent ratings on the Health of the Nation Outcome Scales for Children and Adolescents (HoNOSCA; Gowers et al., 1999; Gowers, Levine, Bailey‐Rogers, Shore, & Burhouse, 2002) at each time point were used to measure overall symptom burden and impairment.
Statistical analysis
Analyses were carried out using Mplus 8.2 (Muthén & Muthén, 2017) with Bayesian methods equivalent to full information maximum likelihood (Muthén & Muthén, 2017) to handle missing data. Results were considered significant if the 95% Bayes credibility interval did not include zero. We used exploratory factor analysis of baseline self‐reported psychopathology items to identify their factor structure (see Appendix S1, Tables S2 and S3), which we then used in a multilevel confirmatory factor analysis (CFA) using data from all time points comparing: unidimensional, correlated factors, and orthogonal bifactor (with specific factors uncorrelated; see Figure 1 & Appendix S1) models. We calculated model‐based reliability coefficients for general and specific factors from the orthogonal bifactor model (see Appendix S1; Dueber, 2017) Using data from all time points, we regressed parent‐ and self‐reported HoNOSCA mean scores on factors from the orthogonal bifactor model to examine their convergent validity. We regressed the factors on dummy‐coded time points (Wright, Hopwood, Skodol, & Morey, 2016) to examine change over time and compared scores between adjacent time points (see Appendix S1). We used treatment‐specific variables in a multilevel CFA to compare change in general and specific factors in CBT, STPP, and BPI (see Appendix S1).
Figure 1.
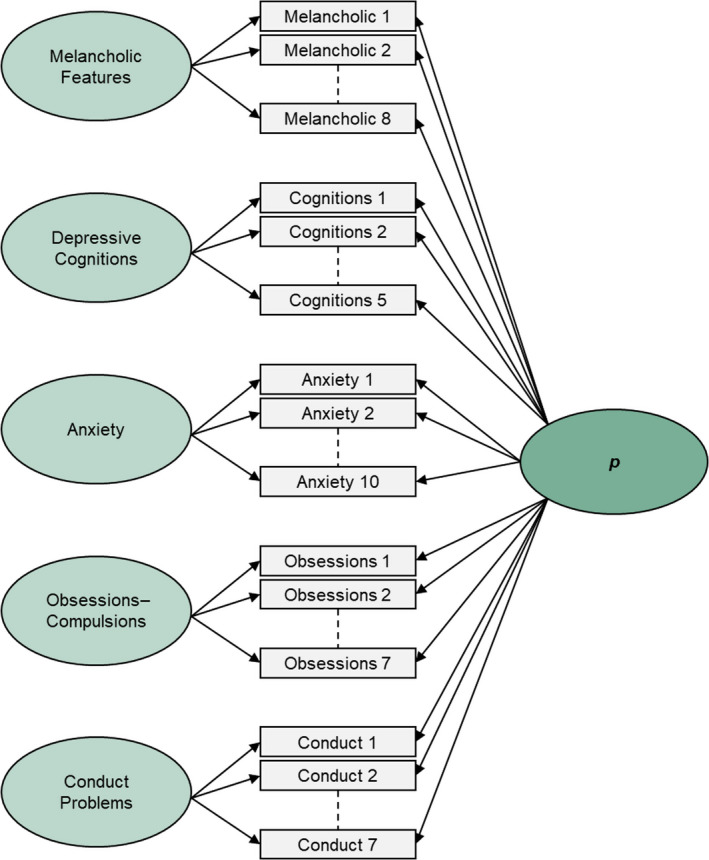
Orthogonal bifactor model [Colour figure can be viewed at wileyonlinelibrary.com]
Results
Multilevel CFA
Both the orthogonal bifactor model (Figure 1), including a general factor and five specific factors (melancholic features, depressive cognitions, anxiety, obsessions–compulsions, and conduct problems), and the correlated factor model fit well, although the orthogonal bifactor model’s fit was superior (see Table 1, Appendix S1 and Table S4).
Table 1.
Fit statistics for multilevel confirmatory factor analysis across six time points
| Model | FP | χ2 | RMSEA | CFI | BICa | ΔBICa |
|---|---|---|---|---|---|---|
| Unidimensional | 111 | 16,723.09 | .110 | .866 | 114,936.84 | – |
| Five correlated factors | 121 | 4,636.37 | .056 | .967 | 109,178.53 | 5,758.31 |
| Orthogonal bifactor | 148 | 3,134.42 | .045 | .979 | 108,386.26 | 797.27 |
BIC, Bayesian information criterion; CFI, comparative fit index; FP, free parameters; RMSEA, root mean squared error of approximation.
BIC values were obtained by rerunning the analysis with the maximum likelihood estimator. Change in BIC is calculated from the model in the line above.
In the orthogonal bifactor model, the general factor, along with the conduct problems and obsessions–compulsions specific factors, demonstrated adequate reliability, whereas evidence was mixed for the depressive cognitions factor, and reliability scores were somewhat lower for the melancholic features and anxiety specific factors (see Appendix S1). Higher general factor and specific conduct problems and melancholic features factor scores were associated with greater symptom burden and impairment across time. Higher depressive cognitions factor scores were associated with more self‐ but not parent‐reported symptom burden and impairment. Anxiety and obsessions–compulsions factor scores were inversely related to symptom burden and impairment (see Table 2 and Table S5 for further analyses).
Table 2.
Multivariate regression of symptom burden and impairment ratings on general and specific factors
| Variable | Estimate | Posterior SD | p | 95% Bayes CI | Significance | |
|---|---|---|---|---|---|---|
| Lower 2.5% | Upper 2.5% | |||||
| Self‐reported impairment | ||||||
| General factor | 0.675 | 0.015 | <.001 | 0.644 | 0.705 | * |
| Melancholic features | 0.159 | 0.028 | <.001 | 0.104 | 0.213 | * |
| Depressive cognitions | 0.091 | 0.025 | <.001 | 0.042 | 0.139 | * |
| Anxiety | −0.053 | 0.024 | .015 | −0.100 | −0.005 | * |
| Obsessions–compulsions | −0.056 | 0.020 | .003 | −0.096 | −0.016 | * |
| Conduct problems | 0.184 | 0.022 | <.001 | 0.141 | 0.227 | * |
| Parent‐reported impairment | ||||||
| General factor | 0.480 | 0.027 | <.001 | 0.426 | 0.531 | * |
| Melancholic features | 0.096 | 0.040 | .009 | 0.017 | 0.173 | * |
| Depressive cognitions | 0.039 | 0.037 | .146 | −0.034 | 0.112 | |
| Anxiety | −0.099 | 0.038 | .005 | −0.173 | −0.024 | * |
| Obsessions–compulsions | −0.072 | 0.032 | .012 | −0.134 | −0.010 | * |
| Conduct problems | 0.213 | 0.033 | <.001 | 0.148 | 0.277 | * |
Standardized estimates. CI = credibility interval. One‐tailed p values based on the posterior distribution can be interpreted as the proportion of the posterior distribution that is below zero (or, for negative estimates, above zero).
95% Bayes credibility interval does not contain 0.
Change over time
General factor scores decreased significantly between time points from baseline to 52 weeks (see Figure 2 and Table S6). Specific melancholic features, depressive cognitions, and conduct problems factors decreased significantly from baseline to 6 weeks but did not otherwise change significantly between adjacent time points. In supplementary analyses, conduct problems further decreased across treatment and follow‐up, despite nonsignificant differences between adjacent time points (see Table S7 and Appendix S1). In contrast, the anxiety factor increased significantly from baseline to 6 weeks and then decreased significantly between 12 and 36 weeks. Anxiety scores at 6 and 12 weeks were significantly higher than baseline but did not differ from baseline at subsequent time points. There was no change in obsessions–compulsions factor scores. In preliminary analyses, there were no differences in change over time by participant sex or geographic region (see Tables S8 and S9).
Figure 2.
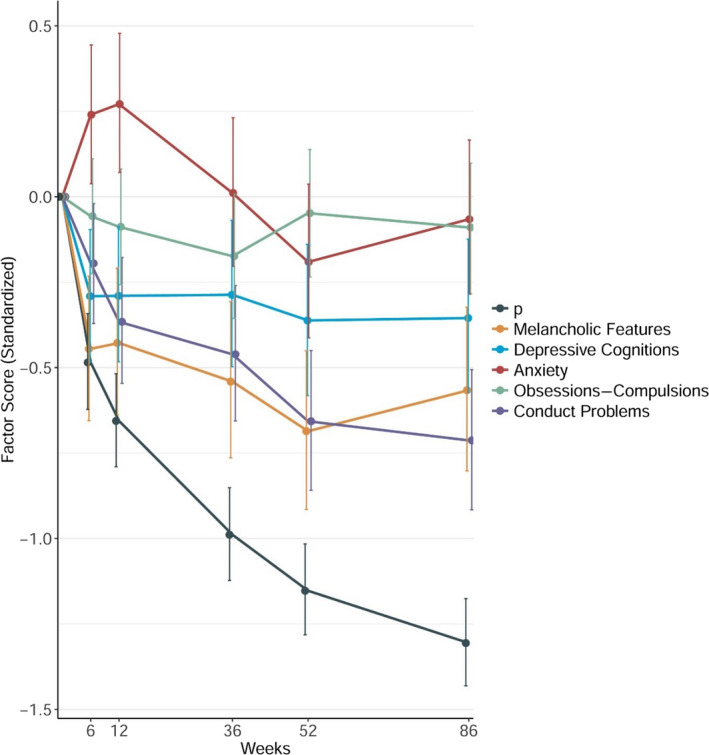
General and specific factor scores across treatment and follow‐up. Error bars represent the 95% Bayes credibility interval. Factors are derived from orthogonal bifactor modeling, in which each item loads on the general p factor has its remaining variance accounted for by one of the five specific factors [Colour figure can be viewed at wileyonlinelibrary.com]
Treatment effects
CBT and STPP, and STPP and BPI, did not differ in their associations with changes in factor scores across time (see Figure 3, and Tables S10 and S11). However, there was a significantly larger decrease in conduct problems from 36 to 52 weeks (i.e., post‐treatment phase) in BPI compared with CBT, although not compared with STPP. No other treatment differences were significant. An analysis comparing BPI versus [CBT + STPP] showed similar results (see Appendix S1 and Table S12).
Figure 3.

Change in general and specific factor scores by treatment type. BPI, brief psychosocial intervention; CBT, cognitive behavioral therapy; and STPP, short‐term psychoanalytical psychotherapy. Error bars represent the 95% Bayes credibility interval. Factors are derived from orthogonal bifactor modeling, in which each item loads on the general p factor has its remaining variance accounted for by one of the five specific factors [Colour figure can be viewed at wileyonlinelibrary.com]
Discussion
To our knowledge, this study is the first to examine the effects of psychosocial therapy on general and specific psychopathology factors in adolescents presenting with major depression and comorbid conditions. A latent bifactor model with five specific factors and a general psychopathology factor fitted the data well. Consistent with our first hypothesis, the general p factor (containing variance from all 37 psychopathology items) decreased significantly across treatment and one‐year follow‐up. In contrast, in line with our second hypothesis, specific factors showed less consistent decreases over time. For example, specific melancholic features and depressive cognitions factors decreased only during the initial weeks of therapy, whereas anxiety factor scores initially increased and then returned to baseline, and conduct problems factor scores continued to decrease across treatment and follow‐up. The course of the general and specific factors reveals novel insights into change across treatment and follow‐up not evident when using the sum scores from each of the narrow‐band domain measures reported in the original study (Goodyer et al., 2017b).
The general psychopathology factor and the specific conduct problems factor showed continued decreases across treatment and into follow‐up. These continued decreases across time suggest that general psychopathology and specific conduct problems are the two factors that may be most responsive to therapy, including further improvements once therapy has ended. In the main IMPACT trial analysis (Goodyer et al., 2017b), significant decreases in anxiety, depression, obsessions–compulsions, and antisocial behavior were noted. Previous randomized controlled trials of psychotherapy for depression have also demonstrated improvements in comorbid symptom domains, including anxiety, attention‐deficit/hyperactivity disorder, and conduct problems (Asarnow et al., 2009; Hilton et al., 2013). Our results suggest that decreases in these various symptom domains can be best understood as overall decreases in psychopathology, rather than improvements in discrete symptom areas. These broad decreases in psychopathology may be attributed to improvements in transdiagnostic processes believed to underlie the general psychopathology factor, such as negative emotionality, emotion dysregulation, or unwanted irrational thoughts (Asarnow et al., 2009; Carver et al., 2017; Caspi et al., 2014; Caspi & Moffitt, 2018). The present findings parallel those of longitudinal and intervention studies, which have reported a steady decrease in general psychopathology (Constantinou et al., 2019; Wade et al., 2018; Wright et al., 2016). Decreases in specific conduct problems during and following psychosocial treatment have also been reported in institutionalized children placed in foster care (Wade et al., 2018), and in adolescents being treated for conduct problems (Constantinou et al., 2019). The marked decrease in conduct problems in our model is notable in comparison with results of studies using narrow‐band domain measures, which have found inconsistent effects on conduct problems in adolescents being treated for depression (Goodyer et al., 2017b; Weisz et al., 2006).
We hypothesized that specific factors might differ in the amount they change during treatment and follow‐up. We note the rapid decrease from baseline to 6 weeks for general psychopathology and some specific factors (melancholic, depressive cognitions, and conduct): This may index a mechanism common to all the therapies, such as feeling understood or instilling a sense of hope. The lack of any further significant change in melancholic and depressive cognitions factors suggests that their subsequent levels may index more trait‐like features or components less responsive to psychological intervention. Higher melancholic features and depressive cognitions scores were also associated with greater symptom burden and impairment, in line with evidence that specific internalizing, independent of the general factor, is related to psychosocial impairment severity (Haltigan et al., 2018). Thus, even after structured psychotherapy, adolescents may experience residual symptoms specific to melancholy (e.g., anhedonia, fatigue) and depressive thinking that are associated with ongoing impairment. Further research is needed to determine the longitudinal relevance of persistent melancholy and depressive cognitions to treatment response and relapse. Therapies that better address residual depressive symptoms are also needed.
In contrast, the specific anxiety factor increased from baseline to 6 weeks and then decreased to baseline levels by 36 weeks, marking the end of the treatment phase, consistent with evidence from previous bifactor modeling of an increase in specific anxiety with treatment onset (Constantinou et al., 2019). This pattern may reflect the potential for therapy to initially increase anxiety, followed by eventually becoming more comfortable with the experience. The published results of the IMPACT trial and other trials using narrow‐band domain measures have not captured this unique symptom course, instead showing consistent decreases in anxiety across treatment (Goodyer et al., 2017b; Kerns, Read, Klugman, & Kendall, 2013; Young et al., 2012). The specific anxiety factor derived from bifactor modeling, a pure index of anxiety once overall psychopathology has been controlled, may therefore represent a novel and potentially more precise aspect of anxiety symptomatology not measured in previous clinical trials. The specific anxiety factor was related to lower levels of symptom burden/impairment in the present study. Of note, this is consistent with some previous evidence of an inverse association between the internalizing factor derived through bifactor modeling and impairment (Caspi et al., 2014; Lahey et al., 2015). One possible interpretation is that specific anxiety symptoms, net of overall psychopathology, may not require further intervention in adolescents who have received a successful structured course of psychotherapy for depression and may even be adaptive. However, as it is also possible that this finding may be artefactual, further research using a broader set of anxiety items and a more comprehensive measure of function is needed to confirm this suggestion.
Interestingly, there was no statistically significant change in the specific obsessions–compulsions factor over time. We speculate that obsessions and compulsions, at least those indexed by the current specific factor, are unlikely to contribute substantially to treatment response or time to recovery. Indeed, the specific obsessions–compulsions factor was inversely related to symptom burden and impairment as rated by youth and their parents, consistent with previous evidence from bifactor modeling (Laceulle, Chung, Vollebergh, & Ormel, 2019). As with the anxiety specific factor, this negative association may have been due to this factor being adaptive or may have been artefactual, and needs further investigation. Further analyses of treatment outcomes using bifactor modeling, including different psychopathology measures, may increase our understanding of how various therapies are associated with changes in general and specific aspects of psychopathology (Caspi & Moffitt, 2018).
When we examined the pattern of scores across time by therapy type, the results were not consistent with our third hypothesis: Patients receiving established psychological treatments (CBT, STPP) did not show greater reductions in any factor during the treatment phase compared to those receiving BPI. Changes in general and specific factor scores were comparable for the three therapies during the treatment phase. The original IMPACT trial reported no superiority effects for established psychological treatments compared with BPI. The authors speculated that the comparable results of the three therapies may be explained by either: a) similar mechanisms underpinning therapeutic response (other than time itself), often referred to as ‘common factors’ (Messer & Wampold, 2006; Wampold, 2015); or b) the three therapies having specific mechanisms that operate to bring about the same observed end points but by different therapeutic routes (equifinality; Calderon et al., 2019; Goodyer et al., 2017b; Midgley et al., 2018). Bifactor modeling provides some added value to the second of these suggestions, noting that BPI is associated with an additional decline in conduct factor scores post‐treatment compared to CBT. This may index a unique advantage of BPI over CBT (but not STPP) for major depression cases with high baseline conduct symptoms. Perhaps, the greater emphasis on ameliorating peer and family relationships and school functioning, both of which predict less antisocial behavior (Dishion, Patterson, Stoolmiller, & Skinner, 1991), or more liaison with carers and agencies, contributed to continued decreases in conduct problems in BPI compared to CBT; although it is notable that STPP, which is not traditionally viewed as a treatment for conduct disorder, also demonstrated a decline in conduct factor scores, possibly due to the fact that it focuses on the emotional difficulties that may underlie conduct problems. If these findings are replicated, this would be the first suggestion that clinicians might be able to personalize treatment for depressed adolescents based on their conduct problem severity.
Limitations
Several limitations of the current study should be noted. First, in terms of the measures used, the items in our analysis were identified through an exploratory factor analysis of baseline data and did not include social anxiety, impulsivity, or executive dysfunction. In addition, given the self‐report nature of our data and the depressive cognitions items having a common stem, shared method variance may have increased associations between items. Although representative of a well‐fitting factor structure, the items may also not be those most sensitive to intervention. In addition, measures were not always administered precisely at the given number of weeks planned; therefore, our results should not be used to make specific determinations about the number of weeks at which change may be observed. Second, reliabilities were somewhat low for the melancholic features and anxiety specific factors; therefore, it is important not to overinterpret the meaning of these specific factors. Third, around 30% of all participants in each group took a SSRI medication during the trial, and our analysis did not allow for an examination of medication onset effects. Future research, including randomized controlled trials, is needed to examine the effect of SSRIs on general and specific psychopathology factors. Finally, further validity analyses using other criterion measures, including objective and/or biological indicators, are needed. The current study also has many strengths, including a relatively large clinical sample of adolescents, multiple measurement points during treatment and follow‐up, random assignment, and the ability to compare three types of structured psychotherapy delivered in routine, free to access, clinical practice.
Conclusion
In a recent editorial evaluating the state of the science regarding the general psychopathology factor, Ronald asked: ‘Instead of treating specific symptoms, or disorders, should we treat p?’ (Ronald, 2019, p. 499). The present results suggest that perhaps we already are. With the emphasis on manualized, disorder‐specific therapies over the past three decades (Forbes, Rapee, & Krueger, 2019; Roy‐Byrne, 2017), further research in other samples will be important to understand the extent to which evidence‐based interventions may have broad effects on general psychopathology (Hopwood et al., 2019). Future investigations of change in general and specific psychopathology factors with modular and transdiagnostic therapy approaches are also needed (Bilek & Ehrenreich‐May, 2012; Chorpita & Weisz, 2009; Chorpita et al., 2013; Ehrenreich‐May et al., 2017). Similarly, investigations of transdiagnostic prevention programs with the potential for broad effects on psychopathology may prove especially useful (Forbes et al., 2019). Additionally, the potential importance of specific factors in bifactor models of symptom change during treatment not observed using traditional, disorder‐specific, measurement approaches should not be overlooked as these may aid personalized treatment decision‐making.
Supporting information
Appendix S1 . Online supplementary material.
Table S1 . Baseline participant demographics and clinical characteristics by treatment condition.
Table S2 . Summary of exploratory factor analysis of baseline data (n = 465).
Table S3 . Items and loadings by factor from final iteration of the exploratory factor analysis.
Table S4 . Standardized factor loadings for multilevel orthogonal bifactor model.
Table S5 . Multivariate regression of six impairment‐specific ratings on general and specific factors.
Table S6 . Change in general and specific factor scores across time.
Table S7 . Additional comparisons of change in the specific conduct problems factor across time.
Table S8 . Comparison of change in factor scores between males and females.
Table S9 . Comparison of change in factor scores between three regions.
Table S10 . Change in general and specific factor scores across time by treatment type.
Table S11 . Comparison of change in factor scores between psychosocial treatments.
Table S12 . Comparison of change in factor scores between BPI and CBT + STPP.
Acknowledgements
The IMPACT trial was funded by the National Institute for Health Research Health Technology Assessment Programme UK (project number 06/05/01). The present study was supported by the Cundill Centre for Child and Youth Depression at the Centre for Addiction and Mental Health, Toronto, Canada. The funders had no role in the development, execution, or interpretation of the present analysis. The views expressed in this publication are those of the authors and do not necessarily reflect those of the HTA Programme, NIHR UK, National Health Service, the Department of Health, UK, or the Cundill Centre for Child and Youth Depression. I.M.G., P.O.W., and R.K. received consulting fees from Lundbeck. The remaining authors have declared that they have no competing or potential conflicts of interest.
Key points.
Evidence of the reliability and validity of the general psychopathology, ‘p’, factor, has accumulated in recent years.
This study provides novel information on how three types of psychotherapy influence general and specific aspects of psychopathology.
General factor and specific conduct problems factor scores decrease across treatment and follow‐up, whereas melancholic and depressive cognitions decrease only in the initial 6 weeks.
Longitudinal courses of general and specific factors are similar across therapies, although conduct problems decrease more post‐therapy after brief psychosocial intervention than cognitive behavioral therapy, but not short‐term psychoanalytic psychotherapy.
Bifactor modeling reveals symptom changes not observed using domain sum scores, including differences that may aid selection of psychotherapy for depressed adolescents.
Conflict of interest statement: See Acknowledgements for full disclosures.
Contributor Information
Madison Aitken, Email: madison.aitken@mail.utoronto.ca.
Ian M. Goodyer, Email: ig104@cam.ac.uk.
References
- Achenbach, T.M. , & Edelbrock, C.S. (1978). The classification of child psychopathology: A review and analysis of empirical efforts. Psychological Bulletin, 85, 1275–1301. [PubMed] [Google Scholar]
- Asarnow, J.R. , Emslie, G. , Clarke, G. , Wagner, K.D. , Spirito, A. , Vitiello, B. , … & Brent, D. (2009). Treatment of selective serotonin reuptake inhibitor‐resistant depression in adolescents: Predictors and moderators of treatment response. Journal of the American Academy of Child and Adolescent Psychiatry, 48, 330–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bamber, D. , Tamplin, A. , Park, R.J. , Kyte, Z.A. , & Goodyer, I.M. (2002). Development of a short Leyton obsessional inventory for children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 41, 1246–1252. [DOI] [PubMed] [Google Scholar]
- Bilek, E.L. , & Ehrenreich‐May, J. (2012). An open trial investigation of a transdiagnostic group treatment for children with anxiety and depressive symptoms. Behavior Therapy, 43, 887–897. [DOI] [PubMed] [Google Scholar]
- Brodbeck, J. , Goodyer, I.M. , Abbott, R.A. , Dunn, V.J. , St Clair, M.C. , Owens, M. , … & Croudace, T.J. (2014). General distress, hopelessness‐suicidal ideation and worrying in adolescence: Concurrent and predictive validity of a symptom‐level bifactor model for clinical diagnoses. Journal of Affective Disorders, 152–154, 299–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calderon, A. , Schneider, C. , Target, M. , Midgley, N. , Goodyer, I.M. , Reynolds, S. , … & Fonagy, P. (2019). ‘Interaction structures’ between depressed adolescents and their therapists in short‐term psychoanalytic psychotherapy and cognitive behavioural therapy. Clinical Child Psychology and Psychiatry, 24, 446–461. [DOI] [PubMed] [Google Scholar]
- Carragher, N. , Teesson, M. , Sunderland, M. , Newton, N.C. , Krueger, R.F. , Conrod, P.J. , … & Slade, T. (2016). The structure of adolescent psychopathology: A symptom‐level analysis. Psychological Medicine, 46, 981–994. [DOI] [PubMed] [Google Scholar]
- Carver, C.S. , Johnson, S.L. , & Timpano, K.R. (2017). Toward a functional view of the p factor in psychopathology. Clinical Psychological Science, 5, 880–889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi, A. , Houts, R.M. , Belsky, D.W. , Goldman‐Mellor, S.J. , Harrington, H. , Israel, S. , … & Moffitt, T.E. (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2, 119–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi, A. , & Moffitt, T.E. (2018). All for one and one for all: Mental disorders in one dimension. American Journal of Psychiatry, 175, 831–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castellanos‐Ryan, N. , Brière, F.N. , O’Leary‐Barrett, M. , Banaschewski, T. , Bokde, A. , Bromberg, U. , … & Conrod, P. (2016). The structure of psychopathology in adolescence and its common personality and cognitive correlates. Journal of Abnormal Psychology, 125, 1039–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chorpita, B.F. , & Weisz, J.R. (2009). MATCH‐ADTC: Modular approach to therapy for children with anxiety, depression, trauma, or conduct problems. Satellite Beach, FL: PracticeWise LLC. [Google Scholar]
- Chorpita, B.F. , Weisz, J.R. , Daleiden, E.L. , Schoenwald, S.K. , Palinkas, L.A. , Miranda, J. , … & Gibbons, R.D. (2013). Long‐term outcomes for the Child STEPs randomized effectiveness trial: A comparison of modular and standard treatment designs with usual care. Journal of Consulting and Clinical Psychology, 81, 999–1009. [DOI] [PubMed] [Google Scholar]
- Constantinou, M.P. , Goodyer, I.M. , Eisler, I. , Butler, S. , Kraam, A. , Scott, S. , … & Fonagy, P. (2019). Changes in general and specific psychopathology factors over a psychosocial intervention. Journal of the American Academy of Child and Adolescent Psychiatry, 58, 776–786. [DOI] [PubMed] [Google Scholar]
- Costello, E.J. , & Angold, A. (1988). Scales to assess child and adolescent depression: checklists, screens, and nets. Journal of the American Academy of Child and Adolescent Psychiatry, 27, 726–737. [DOI] [PubMed] [Google Scholar]
- Cregeen, S. , Hughes, C. , Midgley, N. , Rhode, M. , & Rustin, M. (2017). Short‐term psychoanalytic psychotherapy for adolescents with depression: A treatment manual. In Catty J. (Ed.). London: Karnac. [Google Scholar]
- Dishion, T.J. , Patterson, G.R. , Stoolmiller, M. , & Skinner, M.L. (1991). Family, school, and behavioral antecedents to early adolescent involvement with antisocial peers. Developmental Psychology, 27, 172–180. [Google Scholar]
- Dueber, D.M. (2017). Bifactor indices calculator: A Microsoft Excel‐based tool to calculate various indices relevant to bifactor CFA models. 10.13023/edp.tool.01 [DOI]
- Ehrenreich‐May, J. , Kennedy, S. , Sherman, J. , Bilek, E. , Buzzella, B. , Bennett, S. , & Barlow, D.H. (2017). Unified protocols for transdiagnostic treatment of emotional disorders in children and adolescents. New York: Oxford University Press. [Google Scholar]
- Forbes, M.K. , Rapee, R.M. , & Krueger, R.F. (2019). Opportunities for the prevention of mental disorders by reducing general psychopathology in early childhood. Behaviour Research and Therapy, 119, 103411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodyer, I.M. , Reynolds, S. , Barrett, B. , Byford, S. , Dubicka, B. , Hill, J. , … & Fonagy, P. (2017a). Cognitive‐behavioural therapy and short‐term psychoanalytic psychotherapy versus brief psychosocial intervention in adolescents with unipolar major depression (IMPACT): A multicentre, pragmatic, observer‐blind, randomised controlled trial. Health Technology Assessment, 21, 1–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodyer, I.M. , Reynolds, S. , Barrett, B. , Byford, S. , Dubicka, B. , Hill, J. , … & Fonagy, P. (2017b). Cognitive behavioural therapy and short‐term psychoanalytical psychotherapy versus a brief psychosocial intervention in adolescents with unipolar major depressive disorder (IMPACT): A multicentre, pragmatic, observer‐blind, randomised controlled superiori. The Lancet Psychiatry, 4, 109–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodyer, I.M. , Tsancheva, S. , Byford, S. , Dubicka, B. , Hill, J. , Kelvin, R. , … & Fonagy, P. (2011). Improving mood with psychoanalytic and cognitive therapies (IMPACT): A pragmatic effectiveness superiority trial to investigate whether specialised psychological treatment reduces the risk for relapse in adolescents with moderate to severe unipolar depres. Trials, 12, 175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gowers, S.G. , Harrington, R.C. , Whitton, A. , Lelliott, P. , Beevor, A. , Wing, J. , & Jezzard, R. (1999). Brief scale for measuring the outcomes of emotional and behavioural disorders in children. British Journal of Psychiatry, 174, 413–416. [DOI] [PubMed] [Google Scholar]
- Gowers, S.G. , Levine, W. , Bailey‐Rogers, S. , Shore, A. , & Burhouse, E. (2002). Use of a routine, self‐report outcome measure (HoNOSCA–SR) in two adolescent mental health services. British Journal of Psychiatry, 180, 266–269. [DOI] [PubMed] [Google Scholar]
- Haltigan, J.D. , Aitken, M. , Skilling, T. , Henderson, J. , Hawke, L. , Battaglia, M. , … & Andrade, B.F. (2018). “P” and “DP:” Examining symptom‐level bifactor models of psychopathology and dysregulation in clinically referred children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 57, 384–396. [DOI] [PubMed] [Google Scholar]
- Hilton, R.C. , Rengasamy, M. , Mansoor, B. , He, J. , Mayes, T. , Emslie, G.J. , … & Brent, D.A. (2013). Impact of treatments for depression on comorbid anxiety, attentional, and behavioral symptoms in adolescents with selective serotonin reuptake inhibitor‐resistant depression. Journal of the American Academy of Child and Adolescent Psychiatry, 52, 482–492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopwood, C.J. , Bagby, R.M. , Gralnick, T. , Ro, E. , Ruggero, C. , Kotov, R. , … & Zimmermann, J. (2019). Integrating psychotherapy with the hierarchical taxonomy of psychopathology (HiTOP). Journal of Psychotherapy Integration. Advanced online publication. 10.1037/int0000156 [DOI] [Google Scholar]
- Kerns, C.M. , Read, K.L. , Klugman, J. , & Kendall, P.C. (2013). Cognitive behavioral therapy for youth with social anxiety: Differential short and long‐term treatment outcomes. Journal of Anxiety Disorders, 27, 210–215. [DOI] [PubMed] [Google Scholar]
- Kotov, R. , Krueger, R.F. , Watson, D. , Achenbach, T.M. , Althoff, R.R. , Bagby, R.M. , … & Zimmerman, M. (2017). The hierarchical taxonomy of psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126, 454–477. [DOI] [PubMed] [Google Scholar]
- Krueger, R.F. , Kotov, R. , Watson, D. , Forbes, M.K. , Eaton, N.R. , Ruggero, C.J. , Pincus, A.L. (2018). Progress in achieving quantitative classification of psychopathology. World Psychiatry, 17, 282–293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laceulle, O.M. , Chung, J.M. , Vollebergh, W.A.M. , & Ormel, J. (2019). The wide‐ranging life outcome correlates of a general psychopathology factor in adolescent psychopathology. Personality and Mental Health. Advanced online publication. 10.1002/pmh.1465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laceulle, O.M. , Vollebergh, W.A.M.M. , & Ormel, J. (2015). The structure of psychopathology in adolescence: Replication of a general psychopathology factor in the TRAILS study. Clinical Psychological Science, 3, 850–860. [Google Scholar]
- Lahey, B.B. , Rathouz, P.J. , Keenan, K. , Stepp, S.D. , Loeber, R. , & Hipwell, A.E. (2015). Criterion validity of the general factor of psychopathology in a prospective study of girls. Journal of Child Psychology and Psychiatry and Allied Disciplines, 56, 415–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey, B.B. , Van Hulle, C.A. , Singh, A.L. , Waldman, I.D. , & Rathouz, P.J. (2011). Higher‐order genetic and environmental structure of prevalent forms of child and adolescent psychopathology. Archives of General Psychiatry, 68, 181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer, S.B. , & Wampold, B.E. (2006). Let’s face facts: Common factors are more potent than specific therapy ingredients. Clinical Psychology: Science and Practice, 9, 21–25. [Google Scholar]
- Midgley, N. , Reynolds, S. , Kelvin, R. , Loades, M. , Calderon, A. , Martin, P. , & O’Keeffe, S. (2018). Therapists’ techniques in the treatment of adolescent depression. Journal of Psychotherapy Integration, 28, 413–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén, L.K. , & Muthén, B.O. (2017). Mplus user’s guide (8th edn). Los Angeles: AUTHOR. [Google Scholar]
- Patalay, P. , Fonagy, P. , Deighton, J. , Belsky, J. , Vostanis, P. , & Wolpert, M. (2015). A general psychopathology factor in early adolescence. The British Journal of Psychiatry, 207, 15–22. [DOI] [PubMed] [Google Scholar]
- Reynolds, C.R. , & Paget, K.D. (1981). Factor analysis of the Revised Children’s Manifest Anxiety Scale for Blacks, Whites, males, and females with a national normative sample. Journal of Consulting and Clinical Psychology, 49, 352–359. [DOI] [PubMed] [Google Scholar]
- Reynolds, C.R. , & Richmond, B.O. (1978). Revised children’s manifest anxiety scale. Los Angeles: Western Psychological Services. [Google Scholar]
- Rodriguez‐Seijas, C. , Eaton, N.R. , & Krueger, R.F. (2015). How transdiagnostic factors of personality and psychopathology can inform clinical assessment and intervention. Journal of Personality Assessment, 97, 425–435. [DOI] [PubMed] [Google Scholar]
- Ronald, A. (2019). The psychopathology p factor: Will it revolutionise the science and practice of child and adolescent psychiatry? Journal of Child Psychology and Psychiatry and Allied Disciplines, 60, 497–499. [DOI] [PubMed] [Google Scholar]
- Roy‐Byrne, P. (2017). Transdiagnostic cognitive behavioral therapy and the return of the repressed. JAMA Psychiatry, 74, 867–868. [DOI] [PubMed] [Google Scholar]
- Wade, M. , Fox, N.A. , Zeanah, C.H. , & Nelson, C.A. (2018). Effect of foster care intervention on trajectories of general and specific psychopathology among children with histories of institutional rearing: a randomized clinical trial. JAMA Psychiatry, 75, 1137–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waldman, I.D. , Poore, H.E. , van Hulle, C. , Rathouz, P.J. , & Lahey, B.B. (2016). External validity of a hierarchical dimensional model of child and adolescent psychopathology: Tests using confirmatory factor analyses and multivariate behavior genetic analyses. Journal of Abnormal Psychology, 125, 1053–1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wampold, B.E. (2015). How important are the common factors in psychotherapy? An update. World Psychiatry, 14, 270–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weisz, J.R. , McCarty, C.A. , & Valeri, S.M. (2006). Effects of psychotherapy for depression in children and adolescents: A meta‐analysis. Psychological Bulletin, 132, 132–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright, A.G.C. , Hopwood, C.J. , Skodol, A.E. , & Morey, L.C. (2016). Longitudinal validation of general and specific structural features of personality pathology. Journal of Abnormal Psychology, 125, 1120–1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young, J.F. , Makover, H.B. , Cohen, J.R. , Mufson, L. , Gallop, R.J. , & Benas, J.S. (2012). Interpersonal psychotherapy‐adolescent skills training: anxiety outcomes and impact of comorbidity. Journal of Clinical Child and Adolescent Psychology, 41, 640–653. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1 . Online supplementary material.
Table S1 . Baseline participant demographics and clinical characteristics by treatment condition.
Table S2 . Summary of exploratory factor analysis of baseline data (n = 465).
Table S3 . Items and loadings by factor from final iteration of the exploratory factor analysis.
Table S4 . Standardized factor loadings for multilevel orthogonal bifactor model.
Table S5 . Multivariate regression of six impairment‐specific ratings on general and specific factors.
Table S6 . Change in general and specific factor scores across time.
Table S7 . Additional comparisons of change in the specific conduct problems factor across time.
Table S8 . Comparison of change in factor scores between males and females.
Table S9 . Comparison of change in factor scores between three regions.
Table S10 . Change in general and specific factor scores across time by treatment type.
Table S11 . Comparison of change in factor scores between psychosocial treatments.
Table S12 . Comparison of change in factor scores between BPI and CBT + STPP.


