Abstract
Our article deals with pricing strategies in Swiss health insurance markets and focuses on the relationship between basic and supplementary insurance. We analyzed how firms' pricing strategies (i.e., pricing of basic and supplementary products) can create switching costs in basic health insurance markets, thereby preventing competition in basic insurance from working properly. More specifically, using unique market and survey data, we investigated whether firms use bundling strategies or supplementary products as low‐price products to attract and retain basic insurance consumers. To our knowledge, this is the first paper to analyze these pricing strategies in the context of insurance/health insurance. We found no evidence of bundling in the Swiss setting. We did however observe that firms used low‐price supplementary products that contributed to lock in consumers. A majority of firms offered at least one of such product at a low price. None offered low‐price products in both basic and supplementary markets. Low‐price insurance products differed across firms. When buying a low‐price supplementary product, consumers always bought their basic contract from the same firm. Furthermore, those who opted for low‐price supplementary products were less likely to declare an intention to switch basic insurance firms in the near future. This result was true for all risk category levels.
Keywords: bundling, consumer inertia, low‐price supplementary product, managed competition, pricing, supplementary insurance, Swiss health care systems, switching costs
1. INTRODUCTION
Competition in health insurance (HI) markets exists in various countries including the United States, the Netherlands, and Switzerland. The logic behind competition is that insurance providers are put under consumer pressure, theoretically forcing them to increase quality and/or decrease premiums. However, competition only works if enough consumers switch to more efficient insurers.
Literature on consumer behavior in competitive HI markets highlights low switching rates (SRs). In Switzerland, despite price differentials for identical benefit packages, yearly SR ranged between 2% and 5% between 1997 and 2007 (Lamiraud, 2014). Large variations in premiums and consumer inertia have been shown in the Netherlands where the initial high SR (26%) in 2006 following the implementation of competition was followed by consistently low rates (Boonen, Laske‐Aldershof, & Schut, 2016). In the U.S. private insurance market, on average, only 5% of employees of large firms switch each year (Buchmueller & Feldstein, 1996). Using a representative sample of privately insured people, Cunningham and Kohn (2000) argued that only 25% of switching is voluntary, the rest being due to changing jobs, or to the employer offering a new plan. Consumer inertia is also well documented in Medicare Part D (Ho, Hogan, & Scott Morton, 2017; Polyakova, 2016).
Why are SRs in HI markets low? Most research to date has investigated the question from the consumer's point of view, highlighting the following switching costs (SC): attachment to status quo (Samuelson & Zeckhauser, 1988; Strombom, Buchmueller, & Feldstein, 2002), choice overload (Frank & Lamiraud, 2009), reluctance to switch health care providers (Abraham, Feldman, Carlin & Christianson, 2006, fear of risk selection practices in supplementary insurance (SI) markets (Dormont, Geoffard, & Lamiraud, 2009; Roos & Schut, 2012), and lack of information (McCarthy & Tchernis, 2010). In the present paper, we look at the problem from a different angle. Economics literature shows that SC categories can include provider‐implemented pricing strategies (Farrell & Klemperer, 2007). We analyze how such strategies create SC in basic HI markets, thereby preventing competition from working properly. More specifically, we examine firms' pricing strategies in settings where providers offer both basic and supplementary products, making it possible for firms to link the conditions of these various products together. In particular, we investigate whether firms use bundling strategies or supplementary products as low‐price products to attract and retain basic insurance consumers.
We focused on the Swiss setting to study competition in basic HI markets as the country has several years of a near perfect health care competition market structure. More specifically, we examined market outcomes 10 years after the system was implemented. We found no evidence of bundling. We did however find evidence that low‐price supplementary products contribute to attract and lock in basic HI consumers.
In Section 2, we briefly discuss some of the literature related to multiproduct pricing. Section 3 presents Swiss HI markets, whereas Section 4 describes the unique dataset we collected. Methods and results are in Section 5, and concluding remarks are in Section 6.
2. MULTIPRODUCT PRICING
Bundling is the sale of two or more products as a package (Stremersch & Tellis, 2002). It can be more profitable than monopoly pricing (Adams & Yellen, 1976; Whinston, 1990). However, to attract customers, it must come at a discount with respect to the goods being sold separately (Matutes & Regibeau, 1992). Consequently, it is unclear which of the products generates profits.
Low product pricing is designed to attract customers likely to buy other products at regular prices/high prices. Various forms have been analyzed in the literature, for example, add‐on pricing and loss‐leader pricing. The former occurs when the base price for a product is advertised with the goal of selling additional “add‐ons” at higher prices at the point of sale (Ellison, 2005; Ellison & Ellison, 2009). For example, the quoted price for a hotel room typically does not include dinner or other services. This strategy permits price discrimination between consumers ready to pay a high price for the add‐on utility and those not interested in such options. Consequently, it increases profits (Armstrong & Vickers, 2001; Ellison, 2005). In loss‐leader pricing, products are sold at a low price (often at or below the retailer's marginal cost). They are heavily marketed (Holton, 1957; Simbanegavi, 2008) and provide incentives to shop in a particular store (Salop & Stiglitz, 1977; Varian, 1980). Once in the store, consumers also buy other goods (Beard & Stern, 2008; Hosken & Reiffen, 2007). Hence, profits occur from the sale of these other goods (Lal & Matutes, 1994).
Some empirical literature exists concerning bundling and low product pricing. Stahl, Schaefer, and Maass (2004) showed that the bundling of information by newspaper websites (mostly in the form of dossiers) is more profitable than selling single articles. Evans and Salinger (2004) analyzed the bundling of over‐the‐counter pain relievers and common cold medicines and found a substantial discount with respect to their individual costs. The empirical literature on low pricing is quite scarce. Loss‐leading activities are not usually tested directly from observed prices. DeGraba (2006) suggested examining the size of the basket of goods bought as an empirical test. A basket containing a loss‐leader should have a larger number of bought goods than a basket not containing a loss‐leader. Chevalier, Kashyap, and Rossi (2003) showed that loss‐leaders tend to be goods of more interest to customers, particularly in periods of large demand. Another indirect approach to examine loss‐leader activities is to compute the profit associated with product sales (Wang, 2015). Profits are expected to be low or negative on loss‐leader products.
To our knowledge, these strategies have not yet been analyzed in the context of insurance/HI.
3. SWISS HI MARKETS
3.1. The regulatory framework
Managed competition in basic HI was implemented in 1996 in Switzerland with the Federal Law on Social HI (LAMal).
The main regulatory features are described below.
All residents (including children) must have individual HI coverage. Individuals must take up insurance in their canton of residence. HI cannot be provided by an employer as a fringe benefit.
To avoid competition on coverage content, the law defines a standardized benefit package. Accordingly, all insurance firms must reimburse the same basket of goods. The level of cost sharing is also defined by law and is invariable across insurers. All contracts include a yearly deductible. The law defines six possible deductible levels (300, 500, 1,000, 1,500, 2000, and 2,500 CHF). Once the deductible level has been reached, enrollees pay a 10% coinsurance rate up to a maximum of 700 CHF. The coinsurance rate is 20% for medicines if an equivalent lower cost medicine exists.
Enrollees are completely free to choose their primary physician and have unlimited access to specialists. Physicians are paid on a fee‐for‐service basis. However, enrollees can voluntarily opt for contracts with a limited choice of physicians (see Point 4 below). Physicians who provide services within such contracts are paid on a per‐capita basis.
Premiums are community rated. This means that although they may differ between health plans, insurers must offer uniform premiums to people meeting all three of the following criteria: same age group (0–18, 19–25, and older than 25), same geographic area of residence, and same type of coverage. With regard to the type of coverage, three types of basic HI coverage are available: all firms must offer a contract with a low deductible that guarantees access to any physician. They can also offer contracts with higher deductibles and/or contracts with a limited choice of physicians. In 2007, 40.2% of enrollees opted for a 300 CHF deductible HI policy, whereas 43.0% chose plans with higher deductibles. Insurance covering a limited choice of providers (Health Maintenance Organization [HMO] or general practitioner‐type contracts) accounted for 16.9% of enrollees. Premiums are neither risk nor income related. Clients on low incomes receive subsidies from their canton of residence. In 2007, the mean yearly subsidy was 1,506 CHF per enrollee.
A canton‐level risk equalization mechanism exists whereby funds with a higher percentage of bad risks are compensated by the federal institution “Institution Commune Lamal” whereas those with a higher percentage of good risks have to give money to the same institution. Four risk‐adjustment variables are used: age, gender, the number of inpatient stays lasting at least 3 days, and drug costs higher than 5,000 CHF (during the previous year for both these variables). The inpatient stay variable has been used since January 2012 whereas the drug cost variable was introduced in January 2017 on a temporary basis and replaced in 2020 by the “Pharmaceutical Cost Group” risk‐adjustment variable.
Health insurers must accept all applications for basic insurance.
Enrollees can switch firms twice a year, in June and December. All the individual needs to do is to write a letter to their health insurer.
These features describe price‐based competition. Freedom to choose one's basic insurance provider is strongly encouraged by the regulatory framework. Furthermore, enrollees have a very large choice of contracts. Although the number of insurers offering mandatory HI in Switzerland decreased between 1996 and 2007 (from 145 to 87), the mean number of HI plan choices for each consumer per canton increased over the same period from 39 to 57.
3.2. Stylized facts
One would expect strong price competition within each canton, with small premium differences across plans. However, the reality is very different. Premiums differ greatly across providers within the same canton, as the box plots of monthly premiums suggest in Figure 1. To assess variations in within‐canton posted premiums, we computed, for each canton, the coefficient of variation in premiums for the adult contract with the lowest deductible. Ranging from 0.05 to 0.13 in 2007, they were comparable with those from other studies investigating price dispersion in HI markets for homogenous goods (e.g., Medigap market; Maestas, Schroeder, & Goldman, 2009). The within‐canton variance has remained quite stable since 1996 (Dormont, Geoffard, & Lamiraud., 2009). This lack of premium convergence may be related to the ineffectiveness of competition. One important reason for this is low SRs.
FIGURE 1.
Box plot of adult monthly premium (for a 300 CHF deductible contract) in 2007. Source: Supply data (described in Section 3.1) [Colour figure can be viewed at wileyonlinelibrary.com]
3.2.1. Possible barriers to switching in basic Swiss HI markets
Transaction‐type SC can be ruled out as a possible barrier to switching in the Swiss basic insurance context, as the switching procedure is simple and free of charge as described above. The regulator has also endeavored to minimize quality‐related SC. In particular, enrollees can remain with the same physician or hospital even after switching insurer. Furthermore, the law defines a standardized benefit package. Although small variations may exist in the quality of services provided (e.g. different reimbursement timeframes), existing evidence suggests that they are minimal and do not play a major role in switching behavior. This is confirmed by a survey from 2009 on the quality of services provided by HI companies in basic HI where satisfaction scores were quite homogenous across companies (Chopard, 2010). According to our own survey data (described below), only 1.5% of enrollees reported a good quality of service with their current provider as a reason for not switching. This is consistent with Abraham, Feldman, Carlin, and Christianson (2006) who did not find any significant association between health plan satisfaction and switching behavior in the United States.
What about search costs as a barrier to switching? On the one hand, online comparison services provide price ranking for basic insurance products within each geographic pricing area, which should reduce search costs. On the other hand, individuals need to process available information and form a decision about their HI, which is a complex and time‐consuming exercise involving search costs. Furthermore, the cost of information processing increases as the choice set grows. In the Swiss context, where numerous health fund providers operate, Frank and Lamiraud (2009) suggested that consumers are overwhelmed by too much choice in basic insurance and that this inhibits switching between health plans.
Psychological SC such as the attachment to the status quo have also been emphasized in the Swiss setting. In particular, Frank and Lamiraud (2009) showed that the longer people stayed with the same plan, the less likely they were to express an intention to switch.
Another possible barrier to switching in basic HI markets is the relationship between basic insurance and SI.
SI covers services not included in the basic benefit package and is regulated by the Insurance Contract Law, which allows risk selection, and risk‐rated pricing (based on age and gender). It does not impose any constraint on the extent of supplementary coverage supplied. HI operators in Switzerland are private firms. Although they are not allowed to make a profit from basic insurance, they can from supplementary plans. For a consumer, basic and SI can be purchased from two different insurers or from the same insurer.
Although clear regulatory separation exists between basic and optional SI, in practice, both are strongly associated. More specifically, firms can operate in both markets and most individuals subscribe to the same provider for both types of insurance. SC generated by this association are consumer or firm based. For the former, Dormont, Geoffard, & Lamiraud (2009) showed that a supplementary contract reduces the probability of switching basic insurance provider for those with poor self‐perceived health but had no effect on enrollees with good/very good self‐perceived health. These empirical findings suggest that the main mechanism at work, in terms of SC, is the belief that insurers implement selection practices in supplementary HI markets. Specifically, if the customer thinks he/she is a bad risk and believes that insurers reject applications for supplementary contracts from individuals considered as such, he/she might refrain from switching, even for basic insurance. In this article, we examine the relationship between basic and supplementary HI from the providers' point of view. We analyze whether and how firms' pricing strategies of basic and supplementary products might induce consumer inertia in basic markets. In particular, we investigate whether firms use low‐price supplementary products to attract and retain basic insurance consumers, or whether they use bundling (i.e., selling joint basic and SI products at a lower price than buying these products individually from different insurers). At the time of the study, SI was supervised by the OFAP (Federal Office of Private Insurance), which granted health insurers great autonomy in setting tariffs provided that supplementary HI companies did not make losses overall. In particular, it was possible that health insurers made very low profits or even losses on certain supplementary products, which were compensated by costly (possibly abusively priced) premiums on other supplementary products.
4. DATA
We collected supply data in 2005, 2006, and 2007. Our supply data are unique because they incorporate SI market prices not collected by the regulator and not available on a single website. We also collected information on enrollees' choices in 2007 using a survey of individuals representative of the Swiss population. Studying insurance choices in Swiss HI markets is only possible with data from surveys. In Switzerland, individual‐level data are owned and safeguarded by each private insurance firm. Studying choices in basic and supplementary markets and switching between firms would still be impossible even if data for an individual firm could be acquired.
4.1. Supply data
4.1.1. Sources
Focusing only on adults, we constructed a supply database including price information about basic and SI markets.
For basic insurance, our source of information was the Federal Office for Public Health. For each insurance firm i within each canton c, the supply database recorded the monthly premium for each basic insurance contract b ( ). Switzerland has two types of basic insurance contracts: those with an unlimited (with six possible deductible levels) choice of providers and those with a limited choice (either HMO‐type or general practitioner‐type contracts, with the same choice of deductibles). A total of 18 possible contracts exist. We also incorporated information about the number of adults in all health plans per canton in the form of market share.
The authors collected price information concerning SI from each firm, via advertised prices, and from phone and website data collection, making this dataset unique. We considered four types of supplementary coverage: private room hospitalization (with a 2,000 CHF deductible), semiprivate room hospitalization (with a 2,000 CHF deductible), alternative medicines, and dental care. These products were chosen because they constitute some of the most popular SI products and are quite homogenous across firms. Hence, it is unlikely that differences in prices in these products reflect differences in quality (i.e., basket of goods reimbursed). We considered six risk categories defined by age (born in 1948, 1962, and 1977) and gender. For supplementary products, the supply database contained information about monthly premiums offered by each insurance plan (i), per canton (c), per risk category (r), and per SI product (s) ( ). This information was collected by the authors for the years 2005 to 2007 and was based on the assumption that the effective premium was related to the advertised premium in the same way for each firm in a given market, and that risk‐rating was mostly based on age and gender (as in online simulations).
In 2007, 87 firms were active in the basic insurance market in Switzerland. Of these, 50 also offered SI.
4.1.2. Insurance prices
Table 1 displays the mean monthly premium in 2007 (individual level) for basic insurance (300 CHF deductible level) and for each studied SI product according to risk category.
TABLE 1.
Mean and standard deviations of monthly insurance premiums in basic and supplementary insurance for adults (split into various risk categories for supplementary insurance) in Swiss Francs
| Type of health insurance | Mean (SD) | Females | Males | ||||
|---|---|---|---|---|---|---|---|
| Born in 1948 | Born in 1962 | Born in 1977 | Born in 1948 | Born in 1962 | Born in 1977 | ||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | ||
| Basic insurance (300 CHF deductible) | 287 (65) | ||||||
| Private room hospitalization | 141 (78) | 219 (54) | 125 (54) | 122 (36) | 213 (51) | 102 (79) | 68 (44) |
| Semiprivate room hospitalization | 90 (47) | 139 (30) | 78 (28) | 81 (27) | 135 (30) | 61 (32) | 43 (27) |
| Dental care | 30 (16) | 36 (17) | 31 (16) | 23 (12) | 36 (17) | 30 (15) | 22 (12) |
| Homeopathy/alternative medicine | 20 (12) | 27 (14) | 20 (14) | 17 (9) | 25 (15) | 18 (11) | 15 (10) |
| CV a (range b ) | CV a (range b ) | CV a (range b ) | CV a (range b ) | CV a (range b ) | CV a (range b ) | ||
|---|---|---|---|---|---|---|---|
| Private room hospitalization | (0.19–0.33) | (0.27–0.59) | (0.22–0.39) | (0.17–0.32) | (0.43–0.73) | (0.57–0.75) | |
| Semiprivate room hopsitalization | (0.15–0.29) | (0.22–0.56) | (0.24–0.42) | (0.17–0.31) | (0.41–0.73) | (0.51–0.78) | |
| Dental care | (0.42–0.49) | (0;44–0,54) | (0.51–0.57) | (0.39–0.47) | (0.41–0.51) | (0.43–0.57) | |
| Homeopathy/alternative medicine | (0.51–0.56) | (0.52–0.58) | (0.44–0.49) | (0.57–0.68) | (0.56–0.68) | (0.57–0.68) |
Source: Supply data.
Coefficient of variation for premiums.
Between cantons.
Basic insurance offers a comprehensive package but was quite expensive with a mean premium equal to 287 CHF per month. The mean presented here included large variations, partly due to intercanton variations (Dormont, Geoffard, & Lamiraud, 2009). However, our method for defining low‐price products (see below) ruled out any potential difficulties with this problem in analysis.
Unsurprisingly, private room hospitalization was the most expensive supplementary product. The mean monthly premium was 141 CHF, with large variations between different risk groups. The average premium was approximately 219 and 122 CHF for 60‐ and 30‐year‐old female enrollees, respectively. Variance was very large for all six risk groups and mostly reflected within‐canton variations. We computed, for each risk category in each canton, the coefficient of variation in premiums. The coefficients of variation ranged from 0.17 to 0.75 in private room hospitalization markets (Table 1), indicating high price dispersion within competitive markets. Semiprivate room hospitalization coverage was the second most expensive SI product with a mean premium equal to 90 CHF. Dental care and homeopathy supplementary coverage were less expensive products with much lower price variation. Average premiums were similar for women and men, except for higher premiums for supplementary hospital‐based products for women born in 1977, possibly reflecting expected childbirth‐related costs.
4.2. The consumer dataset
We performed a survey of 3,016 individuals insured in 2007, representative of Swiss residents over 26 years old. Participants were asked about basic HI choices (e.g., the name of their current insurer and the reasons for choosing it, the amount of their deductible, and whether or not they had a “restricted choice of physician” contract) and the cost of their monthly basic insurance premium. For those who had SI, questions included the type of supplementary coverage they opted for, the name of the firm for each supplementary contract, and the premiums paid. They were also asked whether or not and why they had switched from one insurance firm to another during the previous 5 years (2003 to 2007) for basic insurance, and whether they intended to switch in the near future. Furthermore, they were asked about any changes to their SI contracts during the previous 5 years (e.g., subscription to new SI products, whether they stopped any of their supplementary contracts, or switched firms for any supplementary product) and the reasons for these changes. Socioeconomic and demographic information was also collected.
Descriptive statistics are provided in Table 2. In 2007, 11.6% of the enrollees intended to switch basic insurance health plans in the near future, with 5.2% intending to switch as early as 2008. Almost 17% had a subsidized basic insurance premium. A large majority (87.6%) had at least one SI product, the average number being 2.3 (±1.5). Homeopathy/alternative medicines insurance was chosen by 45.8% of the enrollees whereas 11.7% and 21.4%, respectively, opted for private and semiprivate hospital room coverage. Dental care was chosen by 11.3%.
TABLE 2.
Descriptive statistics of the survey (2007) (n = 3,016)
| % | % having supplementary cover with the same firm as for basic cover | % with low‐price products | |
|---|---|---|---|
| Age: [27, 35] | 12.7 | ||
| Age: [35, 50] | 35.01 | ||
| Age: [51, 65] | 29.31 | ||
| Age: >65 | 22.98 | ||
| Household income: <5,000 Swiss Francs per month | 34.4 | ||
| Household income: 5,000–8,000 Swiss Francs per month | 30.8 | ||
| Household income: >8,000 Swiss Francs per month | 34.8 | ||
| Subsidy for the Basic Insurance Premium | 16.8 | ||
| Gender: male | 46.4 | ||
| Education level: first cycle regular track (compulsory school) | 10.7 | ||
| Education level: second cycle regular track | 8.2 | ||
| Education level: short professional track | 49.0 | ||
| Education level: long professional track | 14.5 | ||
| Education level: university completed | 15.8 | ||
| Residing in urban setting | 69.1 | ||
| Presence of children in the household | 37.0 | ||
| Swiss citizen | 86.3 | ||
| Poor subjective health | 16.6 | ||
| Good subjective health | 44.8 | ||
| Very good subjective health status | 38.4 | ||
| Hospital stay (excluding childbirth) in 2006 | 11.1 | ||
| Number of visits to a physician in 2006 | |||
| 0 or 1 | 38.1 | ||
| 2 or 3 | 27.2 | ||
| 4 or more | 34.7 | ||
| Basic insurance contract with low deductible (300 CHF) | 37.2 | ||
| Intended to switch in the near future | 11.6 | ||
| Intended to switch in 2008 | 5.2 | ||
| Supplementary insurance contract | 87.6 | ||
| Subscribed to different companies for basic and supplementary contracts | 9.0 | ||
| Supplementary insurance contract for private room in hospital | 11.7 | 83.0 | 20.4 |
| Supplementary insurance contract for semiprivate room in hospital | 21.4 | 88.0 | 25.0 |
| Supplementary insurance contract for dental care | 11.3 | 92.0 | 9.8 |
| Supplementary insurance contract for homeopathy/alternative medicines | 45.8 | 89.0 | 31.5 |
Source: IEMS survey (2007).
5. EMPIRICAL METHODS AND RESULTS
We aimed to identify insurance firms' pricing strategies in Switzerland. First, in order to investigate the presence of low‐price product strategies to attract and retain basic insurance consumers, we identified potential low‐price products and then analyzed consumer behavior. Second, we investigated whether or not insurers employed bundling strategies.
5.1. Identification of low‐price products
5.1.1. Method
We identified low‐price products by examining the distribution of premiums across all firms in a given market. A market was defined as a given insurance product (i.e., basic insurance, private room hospitalization, semiprivate room hospitalization, alternative medicines, and dental care), for a given risk category, in a given geographical area (i.e., canton). This gave a total of 624 supplementary markets (i.e., 4 (supplementary products) * 3 (age categories) * 2 (gender) * 26 (cantons) markets). In each market, we defined low‐price products as products for which firms asked for a premium lower than the 15th percentile of the premium distribution.
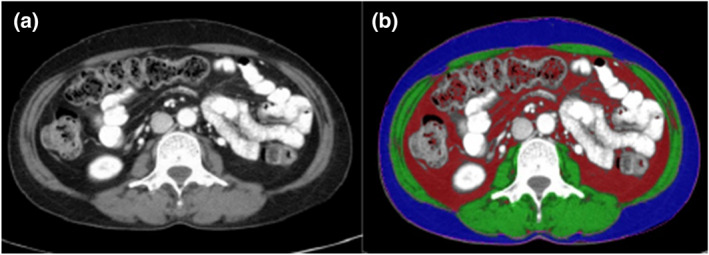
We chose this exogenous threshold based on the particular structure of the premium distribution which revealed, in the vast majority of the markets, two clear groups: firms with products priced at a low level and other firms that usually priced products at a similar, higher level. For some markets, we observed a more continuous distribution of premiums in the second group of firms. We defined the first group of firms as those offering low‐price products. To illustrate the methodology of identifying low‐price products, Figure 2 shows the premium distribution for dental care insurance, for all risk classes, in the canton of Zurich. We performed various sensitivity analyses and varied the threshold between 10% and 20%, which did not qualitatively change our overall results.
FIGURE 2.

Premium distribution for dental care supplementary insurance, for the six risk categories, in the canton of Zurich (2007). The vertical black line in each graph represents the 15th percentile of the premium distribution. Source: Supply data (described in Section 3.1). [Colour figure can be viewed at wileyonlinelibrary.com]
By definition, every market had some low‐price products. For example, for private room hospitalization, the number of low‐price products per market varied between 1 and 7.
5.1.2. What did markets look like?
In order to characterize firms' pricing strategies, we computed the proportion of supplementary markets where each firm offered a low‐price product (for each firm, the denominator was the number of supplementary markets in which it operated). This proportion was also computed for each SI product listed above (in this case the denominator was the number of risk categories covered by that firm summed over all cantons). The most common situation was the following: the firm discounted the chosen product for all six risk classes. This was true for all the cantons in which the firm operated. In a few cases, the firm discounted one supplementary product only for one single risk category. This may be because the firm believed it was likely to attract all family members after attracting one. Consequently, we considered that the firm sold one SI product as a low‐price product (coded 1 in columns 3–6 in Table 3) when this specific product was a low‐price product in more than 90% of markets where the firm sold this product or when the firm sold this product at a low price for one single risk category in all cantons. For basic insurance, we applied the same rule and considered that a firm sold basic insurance at a low price when its basic insurance contracts were low‐price products in more than 90% of markets where it sold those basic insurance products.
TABLE 3.
Pricing patterns of firms who offered at least one low‐price supplementary product
| Firm | Share of supplementary markets c | Choice of low‐price supplementary products | |||
|---|---|---|---|---|---|
| Private room hospitalization b | Semiprivate room hospitalization b | Homeopathy/alternative medicine b | Dental care b | ||
| 1 a | 0.23 | 0 | 0 | 0 | 1 |
| 2 a | 0.21 | 1 | 0 | 0 | 0 |
| 3 a | 0.19 | 1 | 0 | 0 | 0 |
| 4 a | 0.27 | 1 | 0 | 0 | 0 |
| 5 | 0.26 | 1 | 0 | 0 | 0 |
| 6 | 0.31 | 0 | 0 | 1 | 0 |
| 7 | 0.32 | 0 | 0 | 0 | 1 |
| 8 | 0.23 | 0 | 0 | 1 | 0 |
| 9 | 0.51 | 1 | 1 | 0 | 0 |
| 10 | 0.34 | 0 | 0 | 0 | 1 |
| 11 | 0.34 | 0 | 0 | 0 | 1 |
| 12 | 0.48 | 1 | 1 | 0 | 0 |
| 13 | 0.29 | 1 | 0 | 0 | 0 |
| 14 | 0.47 | 1 | 1 | 0 | 0 |
| 15 | 0.28 | 0 | 0 | 0 | 1 |
| 16 | 0.17 | 0 | 0 | 1 | 0 |
| 17 | 0.43 | 1 | 1 | 0 | 0 |
| 18 | 0.51 | 1 | 1 | 0 | 0 |
| 19 | 0.22 | 1 | 0 | 0 | 0 |
| 20 | 0.19 | 0 | 1 | 0 | 0 |
| 21 | 0.26 | 1 | 0 | 0 | 0 |
| 22 | 0.28 | 1 | 0 | 0 | 0 |
| 23 | 0.24 | 1 | 0 | 0 | 0 |
| 24 | 0.21 | 0 | 1 | 0 | 0 |
| 0.58 | 0.29 | 0.13 | 0.21 | ||
Source: Supply data.
These firms sold basic insurance at a low price.
1 means that the product was sold at a low price, and 0 means that the product was not sold at a low price.
In which the firm offered at least one low‐price supplementary product.
Four interesting observations can be made from the results in Table 3.
First, no firm had market proportions (column 2) close to 100% out of the markets represented by the five products—four supplementary products plus one basic insurance product—considered in this analysis. This means that no one firm was cheaper overall (i.e., offering less expensive contracts for every type of cover). The shares of supplementary markets in which firms offered at least one low‐price supplementary product were between 0% and 51%.
Second, a majority of firms had one low‐price product. Seventy‐six percent of firms operating in both the basic and supplementary markets sold at least one low‐price product out of the five products considered here. Forty‐eight percent (i.e., 24 firms) sold at least one low‐price supplementary product. These firms represented a high proportion of all enrollees (60% in basic insurance). Accordingly, a large proportion of market activities involved the strategy of offering a low‐price product. We cannot exclude the possibility that firms with no low‐price products among the products we considered implemented a different strategy. However, it is likely that they had a low‐price product in supplementary coverage products not considered here. For example, one of the largest insurance firms in Switzerland (with a 13% market share in basic insurance in 2007) had no low‐price products among the products we analyzed yet offered one of the cheapest supplementary products for cross‐border (i.e., international travel) care.
Third, most firms discounted only one product (columns 3–6 in Table 4). Only four (i.e., 7% of the basic insurance provider market) could be considered cheap for both basic and supplementary contracts. Most firms who had low‐price supplementary products discounted one supplementary product (out of the four such products considered in our analysis). Seventy‐nine percent of firms with low‐price supplementary products discounted only one supplementary product. The other 21% discounted two, namely, private and semiprivate hospitalization. This pattern is consistent with Hess and Gerstner (1987). In their model to study loss‐leader pricing, stores sell only one “shopping good” (those goods used to determine which store to visit) and a selection of “impulse goods” (products bought on sight without price comparison across stores).
TABLE 4.
Choices in basic insurance for supplementary insurance enrollees, according to whether they opted for a low‐price supplementary product or not
| % having basic coverage with the same firm | p a | ||
|---|---|---|---|
| With non‐low‐price product for supplementary cover | With low‐price product for supplementary cover | ||
| Private room in hospital | 79 | 100 | <0.001 |
| Semiprivate room in hospital | 84 | 100 | <0.001 |
| Dental care | 88 | 100 | <0.001 |
| Homeopathy and alternative medicines | 87 | 100 | <0.001 |
| Mean premium in basic insurance c | p b | ||
|---|---|---|---|
| With non‐low‐price product for supplementary cover | With low‐price product for supplementary cover | ||
| Private room in hospital | 266 | 285 | <0.01 |
| Semiprivate room in hospital | 265 | 287 | <0.01 |
| Dental care | 260 | 298 | <0.01 |
| Homeopathy and alternative medicines | 239 | 264 | <0.01 |
Source: IEMS survey (2007).
Chi‐squared test.
Student's t test for mean comparison.
Basic contract with a 300 CHF deductible.
Fourth, the low‐price product differed between firms: 58% a private hospital room, 29% a semiprivate room, 13% alternative medicine, and 21% dental care. This pattern was similar in all markets. Hence, for a specific market, different insurers did not offer the same supplementary products at low prices. Effectively, firms engaged in market segmentation where each firm discounted a product which appealed most to a particular population subgroup. In this way, each firm chose a niche product for a population subgroup and discounted it. We observed this pattern across all firms despite a great deal of heterogeneity in terms of size, age, and perceived financial stability. For each market, both large and small firms offered low‐price products. That private room hospitalization was often used as a low‐price product may be explained by the fact that it is chosen by more profitable consumers (as suggested by DeGraba, 2006). Based on our survey data, consumers with private room hospitalization bought, on average, 3.1 supplementary products from a given insurer versus 2.2 for those without private room hospitalization in their basket of supplementary products. This difference was significant (p < 0.001).
We also examined pricing patterns for 2005 and 2006. Low‐price products were the same as in 2007, which suggests some short‐term stability in pricing strategies.
As our analysis is based on advertised premiums, one can argue that the actual premiums paid by consumers may be different, for example, if insurers take health status into account when setting SI premiums. We compared advertised (based on the six risk categories) and actual (i.e., self‐reported) premiums for the four supplementary products considered in our analysis. The mean difference between actual and advertised premiums was equal to 1.3 CHF (±0.8), 1.2 CHF (±0.5), 0.9 CHF (±0.4), and 0.6 CHF (±0.4) for, respectively, private room hospitalization, semiprivate room hospitalization, dental care, and alternative medicine. These results confirmed that advertised premiums were a good proxy for actual premiums paid and that the risk categories defined were an important factor when pricing contracts.
5.2. Consumer behaviors
5.2.1. Analyzing consumer reactions
We indirectly investigated the strategy of pricing certain products at a low cost to attract and retain basic insurance consumers. Low‐price products are supposed to incentivize customers to buy other insurance products from the same firm (i) and to induce consumer inertia (i.e., low levels of switching) (ii).
With regard to (i), we investigated two main questions: Are consumers who opt for a low‐price supplementary product more likely to take out basic insurance with the same firm? Are they more likely to subscribe to other supplementary products from the same firm?
With respect to (ii), we estimated an intention‐to‐switch model in basic insurance as follows:
In this model, j denotes the individual, and s denotes the type of SI product (s = 1, 2, 3, 4). The latent variable is based on the observed variable y j which can take two values: y j = 1 if the individual j intends to switch in the near future, and y j = 0 if she/he does not.
S js is a vector of SI products. S js = 1 if the individual j has a contract for product s.
LL js is a vector of low‐price SI products. LL js = 1 if the individual j has opted for one of the low‐price products for SI s.
g j represents the potential gains from switching health plans. It is measured as the (weighted) standard deviation in health plan premiums within a canton, as per Frank and Lamiraud (2009). This represents the expected difference in price if a typical person switched to the mean plan in a canton.
X j is a vector of individual characteristics. u j represents the disturbance which is supposed to follow a normal distribution. We also controlled for canton‐level fixed effects.
5.2.2. Individual choices for SI
In Table 2, most people (between 83 and 92%, depending on the type of supplementary cover) took out both basic and supplementary products with the same insurance firm. There were no significant differences (with respect to self‐assessed health status, health care utilization, gender, age, income, or education level) between consumers who bought basic and SI from the same insurer and consumers who bought both types of insurance from two different providers (Appendix S1). Few people chose the lowest‐price products despite their characteristics being identical to those of the most expensive products. For example, only 9.8% of those who took out dental care insurance opted for a low‐price product.
Table 4 displays the percentages of enrollees who took out both basic and supplementary coverage with the same firm, according to whether they opted for a low‐price supplementary product or not. The results are striking: 100% of those with a low‐price supplementary product had basic coverage with the same insurance provider (vs. between 79% and 88%, depending on the supplementary product type, for those without such a product). This result was true for all risk category levels.
Note that, with respect to health risk, individuals choosing low‐price supplementary products were not different from those with more expensive supplementary products. In particular, self‐assessed health status and health care utilization (measured by the number of doctor visits per year and the probability of a hospital stay during the previous year) did not significantly differ between those with and those without low‐price supplementary products (Table 5). This finding rules out the possibility that low premiums reflect more favorable risks (i.e., healthier applicants are not in fact charged lower prices for supplemental coverage) or that insurers use low prices in supplemental coverage to screen for low‐risk consumers. This finding is strengthened by the fact that average income and the percentage of enrollees with a university degree did not significantly differ between those opting for low‐price products and those who did not.
TABLE 5.
Characteristics of individuals with supplementary cover who had low‐price products and those with non‐low‐price products
| Very good subjective health status (%) | Number of visits to a physician in 2006 (mean) | Hospital stay in 2006 (%) | Male (%) | Completed university (%) | Income b (mean) | |
|---|---|---|---|---|---|---|
| Low‐price product for private room in hospital | 40.85 | 3.81 | 13.89 | 54.17 | 33.33 | 7.46 |
| Non‐low‐price product for private room in hospital | 47.62 | 4.04 | 13.5 | 45.26 | 31.39 | 7.17 |
| p a | 0.38 | 0.75 | 0.932 | 0.178 | 0.752 | 0.53 |
| Low‐price product for semiprivate room in hospital | 40.37 | 3.95 | 14.91 | 41.61 | 21.38 | 6.84 |
| Non‐low‐price product for semiprivate room in hospital | 36.9 | 4.54 | 14.88 | 43.4 | 18.01 | 6.53 |
| p a | 0.432 | 0.303 | 0.995 | 0.693 | 0.36 | 0.62 |
| Low‐price product for dental care | 40.19 | 3.9 | 9.35 | 53.27 | 12.54 | 6.15 |
| Non‐low‐price product for dental care | 41.48 | 3.78 | 13.97 | 53.28 | 12.15 | 5.76 |
| p a | 0.822 | 0.82 | 0.232 | 0.999 | 0.1 | 0.27 |
| Low‐price product for homeopathy/alternative medicines | 36.76 | 4.3 | 10.29 | 45.59 | 22.79 | 6.17 |
| Non‐low‐price product for homeopathy/alternative medicines | 40.36 | 4.19 | 10.8 | 37.95 | 18.83 | 5.72 |
| p a | 0.417 | 0.84 | 0.857 | 0.083 | 0.32 | 0.28 |
Source: IEMS survey (2007).
Comparison of characteristics between the group with low‐price products and the group with non‐low‐price products. Chi‐squared test and Student's t test for mean comparison for dichotomous and continuous variables, respectively.
The survey records household income as a categorical variable with 11 categories (1 is the lowest income category, 11 is the highest income category).
Furthermore, the basket of goods bought from a given insurer was larger when a low‐price supplementary product was chosen. Participants with a low‐price product (out of the four products considered here) bought on average 3.2 supplementary products from a given insurer, as opposed to 2.1 supplementary products by those who did not buy a low‐price supplementary product. This difference is significant (p < 0.001).
Table 6 displays the results of the intention‐to‐switch model. The coefficients for the variables indicating a low‐price product choice were all negative. Most were significant, except for private room hospital cover (significant at the 10% level). Having a low‐price SI product was associated with a lower probability of an intention‐to‐switch basic insurance cover to another firm. Variables indicating that the individual holds SI contracts for specific products were not significant, confirming that having a low‐price product is what matters. Coefficients for individual characteristics are in line with previous findings (Frank & Lamiraud, 2009). Estimated coefficients for the variable measuring relative price (g) were positive and significant, suggesting that the larger the price differential between the consumer's plan and other options, the more likely the consumer intended to switch. Older individuals were not as likely to announce any intention to switch, whereas education, income, gender, health status, the presence of children in the household, residing in an urban location, and Swiss citizenship had no significant effects. We also tested to what extent the results for the low‐price supplementary product variables were affected for different sets of control variables but found no evidence that they were affected. We also investigated whether the impact of low‐price supplementary products could vary depending on individual characteristics. To do this, we estimated the intention‐to‐switch by adding cross effects (for example of age groups with the low‐price product supplementary dummies) to the model. These specifications led to a loss in precision yielding many nonsignificant coefficients. In addition, we considered whether indicators of health plan “quality” affected the results on intent‐to‐switch by including measures of administrative costs and the size of plan reserves. Neither of these variables had coefficient estimates that were significantly different from zero. Nor did we find any evidence that the estimated coefficients for the low‐price supplementary products were affected by including these variables. However, some descriptive evidence that quality differences affected choice behavior emerged from the analysis of the reasons which survey respondents gave for being insured with their current basic insurance provider. Between 3.6% and 5.3% of respondents declared that they had chosen their basic HI operator because of the good quality of service provided. These results are displayed in Table 7 and are commented on in the next subsection. However, only 2.5% of those who switched basic HI reported that a good quality of service was the reason they changed provider.
TABLE 6.
Logit intention‐to‐switch estimates (intention to switch = 1)
| Coef | t | |
|---|---|---|
| Low‐price product for private room in hospital | −0.11 | −1.62 |
| Private room in hospital | −0.20 | −0.98 |
| Low‐price product for semiprivate room in hospital | −0.61 | −2.17 |
| Semiprivate room in hospital | −0.03 | −0.18 |
| Low‐price product for dental care | −0.28 | −2.24 |
| Dental care | −0.16 | −0.89 |
| Low‐price product for homeopathy/alternative medicines | −0.63 | −1.98 |
| Homeopathy/alternative medicines | −0.09 | −0.95 |
| g a | 0.02 | 2.29 |
| Male | 0.12 | 1.28 |
| Poor subjective health | ref | ref |
| Good subjective health | −0.09 | −0.65 |
| Very good subjective health status | −0.21 | −1.37 |
| Age: [27, 35] | ref | ref |
| Age: [35, 50] | −0.45 | −4.00 |
| Age: [51, 65] | −0.74 | −5.58 |
| Age: >65 | −1.92 | −5.65 |
| Education level: compulsory school | ref | ref |
| Education level: short professional track | −0.03 | −0.16 |
| Education level: second cycle regular track | 0.20 | 0.9 |
| Education level: long professional track | 0.19 | 0.93 |
| Education level: university completed | 0.08 | 0.39 |
| Income | −0.06 | −0.67 |
| Presence of children in the household | 0.12 | 1.42 |
| Urban setting | 0.17 | 1.28 |
| Swiss citizen | −0.01 | −0.06 |
Note: Canton fixed effects are included. Source: IEMS survey (2007).
(Weighted) standard deviation in health plan premiums within a canton.
TABLE 7.
Reasons for being insured with current Lamal insurance provider and for being insured with the current supplementary insurance provider
| Reasons for being insured with the current Lamal insurer | ||||||||
|---|---|---|---|---|---|---|---|---|
| All sample (n = 3,016) | Changed insurers for at least one supplementary or contracted a new supplementary in 2005, 2006, or 2007 (n = 254) | |||||||
| Parents' advice | Low/moderate premiums | Agent's advice | Friends' advice | Advertisement campaigns | Good quality of service | Offered cheap supplementary products | Offered cheap supplementary products | |
| % | % | % | % | % | % | % | % | |
| Low‐price product for private room in hospital | 12.6 | 12.2 | 3.1 | 7.1 | 13.7 | 5.3 | 79.1 | 92.8 |
| Non‐low‐price product for private room in hospital | 13.9 | 25.2 | 3.2 | 7.2 | 12.6 | 5.2 | 12.0 | 10.1 |
| Low‐price product for semiprivate room in hospital | 12.1 | 14.5 | 2.9 | 7.2 | 13.4 | 4.8 | 81.5 | 94.4 |
| Non‐low‐price product for semiprivate room in hospital | 11.6 | 24.2 | 2.9 | 7.3 | 12.9 | 4.9 | 9.8 | 9.7 |
| Low‐price product for dental care | 11.5 | 12.8 | 2.8 | 7.5 | 14.0 | 5.4 | 73.5 | 90.5 |
| Non‐low‐price product for dental care | 14.2 | 27.8 | 3.2 | 7.8 | 13.5 | 5.1 | 14.2 | 13.2 |
| Low‐price product for homeopathy/alternative medicines | 12.2 | 13.6 | 2.9 | 7.5 | 12.8 | 3.6 | 77.5 | 92.5 |
| Non‐low‐price product for homeopathy/alternative medicines | 11.0 | 26.3 | 3.1 | 7.2 | 13.1 | 3.9 | 11.4 | 12.9 |
| Parents' advice | Reasons for being insured with the current insurer for supplementary coverage | |||||||
|---|---|---|---|---|---|---|---|---|
| Low/moderate premiums | Agent's advice | Friends' advice | Good quality of service | Advertisement campaigns | Offered other good supplementary products | Had basic insurance contract with the same firm | ||
| % | % | % | % | % | % | % | % | |
| Low‐price product for private room in hospital | 0.3 | 98.6 | 3.3 | 1.4 | 2.3 | 88.6 | 10.5 | 1.5 |
| Non‐low‐price product for private room in hospital | 0.5 | 16.7 | 2.8 | 1.6 | 2.1 | 12.5 | 30.6 | 20.4 |
| Low‐price product for semiprivate room in hospital | 1.7 | 95.7 | 2.7 | 1.4 | 1.8 | 85.5 | 4.2 | 2.8 |
| Non‐low‐price product for semiprivate room in hospital | 1.4 | 12.8 | 2.5 | 1.9 | 1.9 | 13.5 | 25.8 | 22.7 |
| Low‐price product for dental care | 0.8 | 96.8 | 3.1 | 1.9 | 1.8 | 92.6 | 8.7 | 2.7 |
| Non‐low‐price product for dental care | 0.9 | 14.6 | 2.7 | 2.1 | 2.1 | 12.4 | 29.4 | 24.6 |
| Low‐price product for homeopathy/alternative medicines | 1.1 | 94.9 | 3.1 | 2.2 | 1.7 | 89.4 | 9.5 | 1.8 |
| Non‐low‐price product for homeopathy/alternative medicines | 1.2 | 15.8 | 2.6 | 1.9 | 1.5 | 9.5 | 32.7 | 23.8 |
Source: IEMS survey (2007).
We considered the possibility that low‐price product variables might be endogenous in the intention‐to‐switch equation, whereby those who chose a low‐price supplementary product might have also chosen a low‐price basic insurance product with the same firm. Two possible mechanisms exist here. One is that they wanted to optimize their consumption basket. The other is that a given firm was more efficient at providing insurance products and was cheap in both the basic and SI markets. Irrespective of the mechanism at play, this situation is unlikely to happen, as very few firms offered low‐price products for both basic and supplementary markets, something confirmed by the following test. For each type of supplementary contract, we computed the mean premium in basic insurance (under the assumption of a basic contract with a 300 CHF deductible) for those with and those without a low‐price supplementary product. The results reported in Table 4 suggest that the average premium in basic insurance was significantly higher for those with a low‐price supplementary product. As an additional test, we also ran the intention‐to‐switch equation excluding individuals having a supplementary contract with one of the four firms identified above as being cheap for both the basic and supplementary contracts. The results were not qualitatively different from those in Table 6.
All these findings suggest that a low‐price supplementary product strategy contributes to attract and retain basic insurance consumers. However, the picture changes when looking at a low‐price basic insurance product strategy to attract consumers. Nineteen percent of our sample had such a product. They were significantly less likely to buy supplementary products from the same firm (see Appendix S2). Individuals with low‐price basic insurance products were typically in better health and younger than those who chose more expensive basic insurance products (see Appendix S3). The pattern observed could be the result of risk selection strategies in supplementary markets, in that enrollees in good health, unlike their poor health counterparts, can easily shop around for cheaper supplementary products from other providers. Furthermore, those looking for the cheapest basic insurance products may make more informed decisions for each insurance product they buy, (optimally) taking out basic and supplementary products with two different providers. Note that those opting for low‐price basic insurance products were significantly less likely to take out SI (Appendix S3), which also suggests that the low‐price basic insurance strategy to attract consumers to supplementary products may not be effective. In conclusion, we did not find any evidence of low pricing strategies for basic insurance products.
5.2.3. Interpreting the results
Our results provide an insight into consumer choices for basic and supplementary HI products. Most people in our sample had supplementary cover and took out basic insurance with the same insurer. There are several possible explanations as to why consumers buy basic insurance and SI from the same insurer, including a low‐price supplementary product strategy, quality of services, insurance brokering, and habit. A low‐price supplementary product strategy assumes that a sufficient number of consumers are interested in a specific SI product and that they base their search on this product, comparing prices across firms or responding to advertisements (Hess & Gerstner, 1987; Lal & Matutes, 1994). Once this initial supplemental choice is made, it would appear that they buy basic insurance from the same provider.
It is important to note that at the time of the study, no single website provided a comparison of premiums across all insurance firms in supplementary markets. Let us assume that a consumer, at the time of the study, was interested in a contract for private room hospitalization and a contract for alternative medicine. There was no easy way to compare offers between firms for these two contracts. Accordingly, customers would have had to search for each supplementary HI product separately. Given the complexity of such a search, it may be the case that enrollees focused on one single specific product when they shopped for HI products.
In order to investigate how enrollees make choices in the Swiss HI markets, we looked at the reasons which enrollees reported for their choices of basic insurance (Table 7). Interestingly, some people selected a basic insurance plan because it offered cheap supplementary products. This was true for a majority of individuals (between 73.5% and 81.5% depending on the specific product), with a low‐price supplementary product versus a minority (approximately 10%) in the group without a low‐price product. This finding suggests that some individuals actually subscribed to an insurance firm for basic insurance because it offered cheap supplementary products. This is consistent with the idea that enrollees may be attracted to basic insurance products through low‐price supplementary products. However, it could be argued that current low‐price products (i.e., at the time of this study) were not low‐price products when they were bought by individuals. In order to control for this potential bias, we investigated the reasons reported for the choice of firm for basic insurance in the subsample of enrollees who changed insurers for at least one supplementary contract or who subscribed to a new SI contract in the previous 3 years. The results are reported in the last column of Table 7 and confirm that low‐price supplementary products did in fact contribute to attract consumers to basic insurance products. The other reasons displayed in Table 7 show that some people chose a health plan based on their parents' advice (between 11.0% and 13.9% of respondents, depending on the type of low‐price supplementary product offered), friends' advice (between 7.1% and 7.8%), an agent's advice (between 2.8% and 3.2%), and a good quality of service (between 3.6% and 5.3%). These reasons did not differ between those with and without a low‐price product.
We also looked at the reasons for choosing a given provider for SI (Table 7). For those with low‐price supplementary products, the two main reasons were low premiums (between 94.9% and 98.6% of enrollees depending on the low‐price supplementary product offered) and advertisement campaigns (between 85.5% and 92.6%), which is consistent with the strategy of attracting consumers through low‐price products. For those without low‐price products, the two main reasons were the provision of other good quality supplementary products by the same firm (between 25.8% and 32.7%) and the fact that they held a basic insurance contract with the same firm (between 20.4% and 24.6%). Other reasons (e.g., parents' advice, agent's advice, and friends' advice) enrollees reported for being insured with the current SI seemed to play a minor role, as they accounted for only 4% of responses.
Finally, one might wonder whether the total amount paid to a given insurer (including basic and supplementary products) was heterogeneous across firms as homogeneity would certainly partly explain consumer switching inertia. To investigate this, we looked at the standard deviation of the total premium paid by enrollees who had three or four products with the same insurance firm. The standard deviation was quite large (Table 8), which suggests heterogeneity.
TABLE 8.
Sum of premiums for basic and supplementary contracts when all contracts are provided by the same provider
| Mean total premium a (SD) | |
|---|---|
| Basic insurance b + Private room in hospital + Dental care | 534 (145) |
| Basic insurance b + Private room in hospital + Homeopathy/alternative medicines | 608 (246) |
| Basic insurance b + Semiprivate room in hospital + Dental care | 488 (311) |
| Basic insurance b + Semiprivate room in hospital + Homeopathy/alternative medicines | 431 (215) |
| Basic insurance b + Private room in hospital + Dental care + Homeopathy/alternative medicines | 757 (365) |
| Basic insurance b + Semiprivate room in hospital + Dental care + Homeopathy/alternative medicines | 552 (421) |
Source: IEMS survey (2007).
Sum of premiums for basic and supplementary contracts when all contracts are provided by the same provider.
On the basis of a basic contract with a 300 CHF deductible.
5.3. Implementing a bundling test
For an insurer i implementing a bundling strategy, we have
where P is the premium, s is a given supplementary product, and b is the basic insurance product (for a given deductible and specific HMO options).
We implemented a simple bundling test. For each individual having basic and SI contracts with the same provider, we computed the theoretical total HI premium (in other words, the total sum of basic and supplementary contracts, for each type of supplementary contract) he/she would pay by choosing the cheapest basic product on the market (keeping his/her deductible and HMO choices constant) and staying with his/her current provider for supplementary contracts. We compared the mean of the previous variable with the mean total premium that the insured individual paid for his/her combination of basic and supplementary contract with the same provider. Note that this test ensured that the basket of products remained unchanged for each individual.
Table 9 shows that the total mean monthly premium paid for basic coverage and a private hospital room contract with the same insurer was 543 CHF. If these individuals had switched their basic insurance to the least expensive basic product, the mean premium would have been reduced to 479 CHF (the deductible being held constant). This difference was statistically significant. Furthermore, we saw the same pattern for the other supplementary products. Separating the products by buying them from different firms would have been cheaper. We interpret this as evidence against bundling strategies.
TABLE 9.
Sum of premiums for basic and supplementary contracts, by the type of supplementary contract
| Mean current premium a when buying supplementary and basic coverage from the same company | Mean theoretical premium a when buying basic coverage from the cheapest company | p | |
|---|---|---|---|
| Private room in hospital | 543 | 479 | <0.01 |
| Semiprivate room in hospital | 458 | 398 | <0.01 |
| Dental care | 376 | 316 | <0.01 |
| Homeopathy/alternative medicines | 359 | 306 | <0.01 |
Source: IEMS survey (2007).
Sum of premiums for basic and supplementary contracts.
Furthermore, it is commonly believed that insurers offer supplementary products at a discounted premium if the consumer also has basic insurance with the same firm. However, the consistency between self‐reported premiums and advertised premiums in supplementary markets (see above) suggests that this is not true, and further confirms our assumption that no bundling strategies exist in the Swiss market.
6. CONCLUSION
A better understanding of the effectiveness of competition in the HI market is of major value for policy makers. Potential barriers to switching may explain the persistence of system inefficiencies.
In this article, using novel data, we investigated SC generated by insurers' pricing strategies. Using a definition of low‐price products based on the distribution of premiums, we identified firms offering low‐price products in every market considered. A majority offered at least one low‐price product (most offered only one). These products differed across firms. Results point to a consistent finding that low‐price supplementary products contribute to attract consumers to basic contracts and discourage switching between health plans in basic insurance. Consumers who bought a low‐price supplementary product always bought their basic contract from the same firm and less frequently reported any intention to switch basic insurance firms. The analysis of the reasons respondents reported for being insured with their current basic insurance provider showed that most individuals with low‐price supplementary products subscribed to an insurance firm for basic insurance because it offered cheap supplementary products. The two main reasons reported for subscribing low‐price supplementary products were low premiums and advertising campaigns, which is consistent with the marketing strategy of attracting consumers through low‐price supplementary products.
Our article greatly contributes to the industrial organization literature focusing on multiple‐product pricing as, to our knowledge, this is the first work to investigate bundling and low‐price product strategies in the context of HI. It also complements the literature studying consumer inertia in HI markets, which to date has mostly been performed from the consumer's not the firm's perspective. We identified pricing strategies that create SC and therefore prevent managed competition from working properly in the Swiss HI market.
Our identification of low‐price products relies on our hypothesis that the supplementary products we studied were homogenous. It must be acknowledged that our price analysis was short term (over 2005–2007). Nevertheless, the group of low‐price products remained stable over this 3‐year period. Investigating pricing patterns over a longer period of time would certainly be useful. Furthermore, as mentioned above, FINMA—the regulatory authority for supplementary health insurers—has been controlling tariffs since 2009 in a stricter fashion than its predecessor, by making sure that insurance companies are financially sound for each SI product taken out individually. It would be interesting to study whether our results still hold under this enforced price regulation.
Supporting information
Appendix S1. Supporting Information
Lamiraud K, Stadelmann P. Switching costs in competitive health insurance markets: The role of insurers' pricing strategies. Health Economics. 2020;29:992–1012. 10.1002/hec.4111
[The copyright line for this article was changed on 02 July 2020 after original online publication.]
Footnotes
There is no specific system for the elderly.
With regard to geographic areas, there are up to three pricing areas per canton. However, most cantons have only one. Furthermore, where there are two or three pricing areas, the prices any given insurance firm sets for any given insurance contract are very similar across all pricing areas within the same canton. Consequently, we can suppose that there are effectively 26 areas of price competition (Switzerland has 26 cantons).
Statistics on compulsory HI 2007 (T.11.07), Federal Office of Public Health. Another type of contract exists entitled “bonus insurance.” Here, the enrollee's premium is reduced gradually for every year that he/she does not make any claim to the HI fund for reimbursement. The starting premium is 10% higher than the standard premium. It can then fall to 50% of the starting premium within 5 years. Very few enrollees opt for this type of contract.
Statistics on compulsory HI 2007 (T.4.01), Federal Office of Public Health, Switzerland. For most covered people, subsidies do not cover the full premium. Consequently, those subsidized still have an incentive to search for cheaper premiums.
Templates are freely available on well‐known websites. Consumers with a basic insurance policy with the standard deductible of CHF 300 can cancel this policy with 3‐month notice at the end of June or with 1‐month notice at the end of December in any year. This means that the notice of cancelation must reach the HI fund by March 31 or November 30 in order to be effective. For HI policies with a higher deductible or with a restricted choice of doctors, cancelation can only occur at the end of the year, usually with 3‐month notice, that is, notice of cancelation must reach the HI fund by September 30 to be effective.
For a review, see Lamiraud (2014).
Deductibles and coinsurance costs for basic insurance are not reimbursable by taking out supplementary coverage.
Even if an enrollee has both a basic and supplementary insurance product with the same firm, specific conditions (e.g., cancelation periods) exist for each. Furthermore, the enrollee will get a specific premium bill for each contract. In general, the cancelation period for SI differs from that for basic HI. An insurer cannot terminate an SI contract if the enrollee chooses to leave the insurer to find basic insurance cover elsewhere. In theory, insurers are allowed to end a contract or change its conditions when the enrollee's health status deteriorates. However, to our knowledge, no insurance company has ever done so when the deterioration is not clearly linked to the enrollee's behavior.
Since January 1, 2009, supplementary HI has been supervised by FINMA (the Swiss Financial Market Supervisory Authority). FINMA's first priority is to check whether the products offered (i.e., each specific supplementary product) are financially sound, as well as ensuring that policyholders are protected from abusive insurance practices. Hence, although health insurers in the SI market can still make small profits on supplementary products, it has become difficult or even impossible for them to offer discounts that would result in losses for a specific supplementary product (https://www.finma.ch/en/supervision/insurers/sector-specific-tools/approval-of-supplementary-health-insurance-tariffs/).
https://www.bag.admin.ch/bag/fr/home/suche.html#primes. We considered premiums including accident insurance cover.
There are up to three pricing areas in each canton for basic insurance. However, in 2007, 15 cantons had only one pricing region, five had two, and six had three. In the latter two scenarios, the ranking of premiums was similar between pricing areas, as suggested by spearman correlation coefficients (0.94 on average). In particular, the cheapest companies, and therefore low‐price products (see definition section 4), did not change across within‐canton pricing areas.
Mandatory basic HI only covers the treatment of dental complications resulting from major, unavoidable diseases of the masticatory system.
We would like to thank our research assistant, Lam Nguyen, who helped us collect price data in all cantons and who compared the extent of cover for each supplementary product between firms through phone calls and online search. Chopard (2010) also identified the same four supplementary products as being homogenous in her study, however focusing exclusively on the canton of Vaud. Cross‐border care, a very popular supplementary product, was excluded from our analysis because associated products exhibited too much heterogeneity between companies.
Age and gender were used as risk categories because online pricing simulations are based on these two characteristics. Three age categories were created (individuals aged 30, 45, and 59 in 2007) because our online search revealed a degree of age‐related nonlinearity in prices of SI. In particular, pricing was quite homogenous for some age groups (26/34, 35/49, and 50/59). Note that the online search did not make it possible to obtain data for people older than 59.
Firms only active in the basic insurance market were typically very small and often offered insurance products for historical reasons (e.g., professional funds).
The survey was carried out by the Link Institute, a leader in market and social research in Switzerland. We would like to thank Tarik Yalcin (IEMS, University of Lausanne) for helping us carry out such a survey (referred to as IEMS survey).
That is, end of 2002.
At the time of the survey, subsidies were provided by the canton authority independently of the insurance firm chosen. Hence, SC were not higher for those benefiting from subsidies.
For basic insurance, we built the ranking for each of the 18 possible basic insurance contracts, that is, 26 * 18 (468) markets.
We did not analyze this product because the heterogeneity across products. Homogenous products are required to compare premiums.
This was computed for the subsample of individuals between 26 and 59 years old (n = 1947) for private and semiprivate hospitalization.
This is still the case today.
Years for which we collected exhaustive supply data concerning prices in supplementary markets.
REFERENCES
- Abraham, J. M. , Feldman, R. , Carlin, C. , & Christianson, J. (2006). The effect of quality information on consumer health plan switching: Evidence from the Buyers Health Care Action Group. Journal of Health Economics, 25, 762–781. 10.1016/j.jhealeco.2005.11.004 [DOI] [PubMed] [Google Scholar]
- Adams, W. J. , & Yellen, J. L. (1976). Commodity bundling and the burden of monopoly. The Quarterly Journal of Economics, 90, 475–498. 10.2307/1886045 [DOI] [Google Scholar]
- Armstrong, M. , & Vickers, J. (2001). Competitive price discrimination. RAND Journal of Economics, 32, 579–605. 10.2307/2696383 [DOI] [Google Scholar]
- Beard, T. R. , & Stern, L. (2008). Continuous cross subsidies and quantity restrictions. Journal of Industrial Economics, 56, 840–861. 10.1111/j.1467-6451.2008.00364.x [DOI] [Google Scholar]
- Boonen, L. H. H. M. , Laske‐Aldershof, T. , & Schut, F. T. (2016). Switching health insurers: The role of price, quality and consumer information search. European Journal of Health Economics, 17, 339–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchmueller, T. C. , & Feldstein, P. J. (1996). Consumers' sensitivity to health plan premiums: Evidence from a natural experiment in California. Health Affairs, 15, 143–151. 10.1377/hlthaff.15.1.143 [DOI] [PubMed] [Google Scholar]
- Chevalier, J. A. , Kashyap, A. K. , & Rossi, P. E. (2003). Why don't prices rise during periods of peak demand? Evidence from scanner data. American Economic Review, 93, 15–37. 10.1257/000282803321455142 [DOI] [Google Scholar]
- Chopard, L . “Statistical and qualitative analysis of the supply of supplementary health insurance on the canton of Vaud (in French).” Professinal Thesis n° 147 (2010). Master of Advanced Studies in Health Economics and Management (MASHEM), University of Lausanne. http://www.chuv.ch/bdfm/cdsp/85150.pdf
- Cunningham, P. J. , & Kohn, L. (2000). Health plan switching: Choice or circumstance? Health Affairs, 19, 158–164. [DOI] [PubMed] [Google Scholar]
- DeGraba, P. (2006). The loss leader is a turkey: Targeted discounts from multiproduct competitors. International Journal of Industrial Organization, 24, 613–628. [Google Scholar]
- Dormont, B. , Geoffard, P. Y. , & Lamiraud, K. (2009). The influence of supplementary health insurance on switching behaviour: Evidence from Swiss data. Health Economics, 18, 1339–1356. 10.1002/hec.1441 [DOI] [PubMed] [Google Scholar]
- Ellison, G. (2005). A model of add‐on pricing. The Quarterly Journal of Economics, 120, 585–637. [Google Scholar]
- Ellison, G. , & Ellison, S. F. (2009). Search, obfuscation, and price elasticities on the internet. Econometrica, 77, 427–452. [Google Scholar]
- Evans, D. , and Salinger, M. “An empirical analysis of bundling and tying: Over‐the‐counter pain relief and cold medicines.” CESifo Working Paper no. 1297 (2004).
- Farrell, J. , & Klemperer, P. (2007). Coordination and lock‐in: Competition with switching costs and network effects In Armstrong M. & Porter R. (Eds.), Handbook of industrial organization (Vol. 3) (pp. 1967–2072). Amsterdam, Elsevier. [Google Scholar]
- Frank, R. G. , & Lamiraud, K. (2009). Choice, price competition and complexity in markets for health insurance. Journal of Economic Behavior and Organization, 71, 550–562. 10.1016/j.jebo.2009.04.005 [DOI] [Google Scholar]
- Hess, D. H. , & Gerstner, E. (1987). Loss leader pricing and rain check policy. Marketing Science, 6, 358–374. 10.1287/mksc.6.4.358 [DOI] [Google Scholar]
- Ho, K. , Hogan, J. , & Scott Morton, F. (2017). The impact of consumer inattention on insurer pricing in the Medicare Part D program. The Rand Journal of Economics, 48, 877–905. 10.1111/1756-2171.12207 [DOI] [Google Scholar]
- Holton, R. H. (1957). Price discrimination at retail: The supermarket case. The Journal of Industrial Economics, 6, 13–32. 10.2307/2097745 [DOI] [Google Scholar]
- Hosken, D. , & Reiffen, D. (2007). Pricing behavior of multiproduct retailers. The B.E. Journal of Theoretical Economics, 7(1), . 10.2202/1935-1704.1354 [DOI] [Google Scholar]
- Lal, R. , & Matutes, C. (1994). Retail pricing and advertising strategies. Journal of Business, 67, 345–370. 10.1086/296637 [DOI] [Google Scholar]
- Lamiraud, K. (2014). Switching costs in competitive health insurance markets In Culyer A. J. (Ed.), Encyclopedia of health economics (Vol. 3). San Diego: Elsevier. 10.1016/B978‐0‐12‐375678‐7.01312‐2 [Google Scholar]
- Maestas, N. , Schroeder, M. , and Goldman, D. “Price variation in markets with homogeneous goods: The case of Medigap.” National Bureau of Economic Research Working Paper no. 14679 (2009).
- Matutes, C. , & Regibeau, P. (1992). Compatibility and bundling of complementary goods in a duopoly. Journal of Industrial Economics, 40, 37–54. 10.2307/2950626 [DOI] [Google Scholar]
- McCarthy, I. M. , & Tchernis, R. (2010). Search costs and Medicare plan choice. Health Economics, 19, 1142–1165. 10.1002/hec.1539 [DOI] [PubMed] [Google Scholar]
- Polyakova, M. (2016). Regulation of Insurance with adverse selection and switching costs: evidence from Medicare Part D. American Economic Journal: Applied Economics, 8, 165–195. [Google Scholar]
- Roos, A. F. , & Schut, F. (2012). Spillover effects of supplementary on basic health insurance: Evidence from the Netherlands. The European Journal of Health Economics, 13, 51–62. 10.1007/s10198-010-0279-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salop, S. , & Stiglitz, J. E. (1977). Bargains and ripoffs: A model of monopolistically competitive price dispersion. Review of Economic Studies, 44, 493–510. [Google Scholar]
- Samuelson, W. , & Zeckhauser, R. (1988). Status quo bias in decision making. Journal of Risk and Uncertainty, 1, 7–59. 10.1007/BF00055564 [DOI] [Google Scholar]
- Simbanegavi, W. “Loss leader or low margin leader? Advertising and the degree of product.” MPRA Paper no. 9694 (2008).
- Stahl, F. , Schaefer, M. F. , & Maass, W. (2004). Strategies for selling paid content on newspaper and magazine web sites: An empirical analysis of bundling and splitting of news and magazine articles. International Journal on Media Management, 6, 59–66. 10.1080/14241277.2004.9669382 [DOI] [Google Scholar]
- Stremersch, S. , & Tellis, G. J. (2002). Strategic bundling of products and prices: A new synthesis for marketing. The Journal of Marketing, 66, 55–72. 10.1509/jmkg.66.1.55.18455 [DOI] [Google Scholar]
- Strombom, B. A. , Buchmueller, T. C. , & Feldstein, P. J. (2002). Switching costs and health plan choice. Journal of Health Economics, 21, 89–116. 10.1016/S0167-6296(01)00124-2 [DOI] [PubMed] [Google Scholar]
- Varian, H. R. (1980). A model of sales. American Economic Review, 70, 651–659. [Google Scholar]
- Wang, Z. “Supermarket and gasoline: An empirical study of bundled discount. Resources for the future.” Discussion paper (2015).
- Whinston, M. D. (1990). Tying, foreclosure, and exclusion. American Economic Review, 80, 837–859. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Supporting Information


