Abstract
Background and purpose
Neurology is rapidly evolving as a result of continuous diagnostic and therapeutic progress, which influences the daily work of neurologists. Therefore, updating residency training programmes is crucial for the future of neurology. Several countries are currently discussing and/or modifying the structure of their neurology residency training programme. A detailed and up‐to‐date overview of the available European residency training programmes will aid this process.
Methods
A questionnaire addressing numerous aspects of residency training programmes in neurology was distributed among 38 national representatives of the Resident and Research Fellow Section of the European Academy of Neurology.
Results
We obtained data from 32 European countries (response rate 84%). The median (range) duration of the residency training programmes was 60 (12–72) months. In the majority of countries, rotations to other medical disciplines were mandatory, mostly psychiatry (69%), internal medicine (66%) and neurosurgery (59%). However, the choice of medical fields and the duration of rotations varied substantially between countries. In 50% of countries, there were formal regulations regarding training in evidence‐based medicine, teaching skills and/or leadership qualities. In many countries (75%), residents had to take an examination.
Conclusions
We found substantial variation among European countries in the duration of residency training programmes, and especially in the choice of obligatory rotations to external medical disciplines. Despite a presumably similar spectrum of patients, neurology residency training programmes across Europe are not harmonized. The structure of the programme should be determined by its relevance for neurologists today and in the future.
Keywords: duration, education, Europe, examination, neurology, research fellows, residency training programme, residents, rotations
Introduction
Neurology is a rapidly evolving discipline as a consequence of the ever‐increasing number of diagnostic tools and novel therapeutic options over the last few decades [1]. These developments lead to higher demands on education. Additionally, as the prevalence of many neurological diseases rises with age and life expectancy in Europe increases, neurological care needs to expand to adequately serve the European population [2]. These factors will qualitatively and quantitatively increase the workload. Given these developments, it is essential that all European national healthcare systems prepare residents for the ongoing changes in neurology. The residency training programme for neurology is a key factor in ensuring high‐quality neurological care across Europe in the future.
Although the Union Europeéne des Médicines Spécialistes (UEMS), Section of Neurology has outlined standards for curricula in European Union countries [3], earlier studies on the structure and content of neurology residency training programmes in the various European countries revealed many differences across countries [4, 5]. In 2006, a survey among national delegates found that the duration of neurological training in Europe varied [mean (range), 57.6 (36–72) months] [4]. A more recent investigation of the neurology residency training programmes in 28 European countries among delegates at the UEMS, Section of Neurology found significant differences between residency programmes in Europe, especially with respect to external rotations [5].
Several countries have recently changed their residency training programme or are considering adaptations; therefore, a detailed update of the current structure of residency training programmes in Europe is warranted to substantiate the optimization process of national programmes.
In 2016, the Residents and Research Fellow Section (RRFS) of the European Academy of Neurology established a network of national representatives from European countries, aimed at facilitating cooperation between European neurology residents and researchers. The national representatives, either current neurology residents, PhD students or up to 3 years post‐PhD, were addressed to obtain detailed insights into the structure of their national neurology residency training programme.
Methods
We distributed a systematic questionnaire in English (Supporting information) among all national representatives, including over 30 questions addressing the following: responsible authorities involved in the development of residency training programmes; entry procedure; duration; prerequisites; institutions involved (university and teaching hospitals, outpatient clinics, private practices); disease‐specific subspecialties within neurology; mandatory and voluntary rotations to other medical disciplines; and examination. The questionnaires were sent to the 38 national representatives known to the RRFS at the time we initiated this study (October 2018). All returned questionnaires were checked manually (N.N.K. or M.v.d.M.); in the case of missing answers or queries, the respondent was contacted again.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Results
The national representatives of 32 of the contacted 38 countries returned the completed questionnaire (response rate 84%) (Fig. 1, Table S1).
Figure 1.

The 32 European countries from which data about the neurology residency training programmes were obtained.
Development of residency training programmes
Except for Malta, all 32 included countries had a national neurological society. In 25 out of the 31 countries (80%), the national society was involved in the residency training programme, but to varying extents; some teaching and educational committees designed the programme and provided advice, whereas others only had an advisory role. In 10 of the 16 countries with a junior neurological society, residents were involved in shaping the residency training programme. The Ministry of Education or Ministry of Health was involved in the residency training programme in six of the 32 countries.
Entry to the residency training programmes
In 19 of the 32 countries (59%), residents had to apply for a resident position to a centralized body, such as a College of Physicians, the council of Higher Education or the Ministry of Health. In Estonia, Moldova, Macedonia and Albania, the application had to be processed via one or two university hospitals. In the remaining 13 countries (41%), postgraduates applied directly to the hospital/department in which they wanted to be trained (Table S2).
Clinical settings for residency training – (university) hospitals and the outpatient sector
In 21 of the 32 countries (66%), it was obligatory to complete at least part of the residency in a university hospital; in seven of these countries, the entire programme was followed in a university hospital (Table 1). In the remaining 11 countries (34%), the full programme could be completed in non‐university hospitals. Many countries (65%) used a combination of university and non‐university hospitals to complete the residency training programme. Interestingly, in eight countries (25%) it was possible to be partly trained in private practices (France, Germany, Norway, Poland, Portugal, Spain, Sweden, Ukraine).
Table 1.
Institutions involved in the residency training programmes in Europe (data from 32 countries)
| Type of teaching hospital | |
|---|---|
| Obligation to complete at least part of the training in a university hospital | Whole training can be completed in non‐university hospitals |
| 21 countries (66%) | 11 countries (34%) |
| Albania, Belgium, Denmark, Estonia, France, Italy, Ireland, Latvia, Macedonia, Malta, Moldova, Netherlands, Norway, Romania, Serbia, Slovakia, Slovenia, Sweden, Switzerland, UK, Ukraine | Austria, Belarus, Croatia, Germany, Greece, Hungary, Lithuania, Poland, Portugal, Spain, Turkey |
| Residency training programme in the outpatient sector (either affiliated to a hospital as outpatient clinic or private practices) | |
|---|---|
| Possible (obligatory or voluntary) | Not possible |
| 22 countries (69%) | 10 countries (31%) |
| Belarus, Denmark, France, Germany, Hungary, Italy, Latvia, Lithuania, Macedonia, Malta, Moldova, Netherlands, Norway, Poland, Portugal, Slovakia, Slovenia, Spain, Sweden, Switzerland, UK, Ukraine | Albania, Austria, Belgium, Croatia, Estonia, Greece, Ireland, Romania, Serbia, Turkey |
| Training in private practices |
|---|
|
Possible in 8 countries (25%) France, Germany, Norway, Poland, Portugal, Spain, Sweden, Ukraine |
Duration of the neurology residency programmes
The median duration (range) of the neurology residency programme in the included countries was 60 (12–72) months. In the majority (87%), the total duration of the programme was 48–60 months (Fig. 2, top half).
Figure 2.
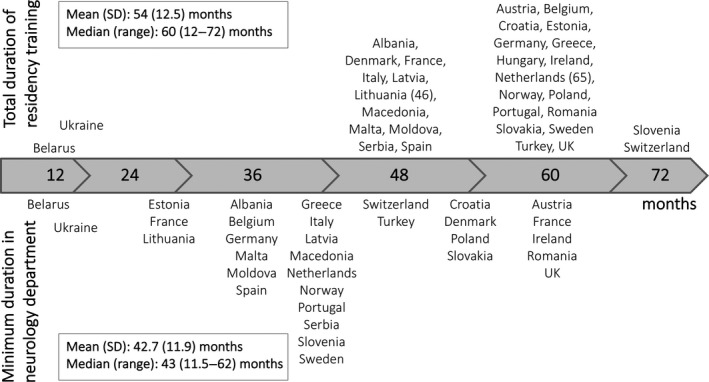
Duration of the neurology residency training programmes in 32 European countries: total duration (top) and minimum duration in neurology department (bottom).
In addition to a medical degree, some countries required candidates to pass postgraduate examinations prior to the neurology residency training programme (Estonia, Italy, Norway, Portugal, Slovenia, Spain, UK), whereas others named different or additional requirements, such as foundation programmes (i.e. the first 2 years of working as a doctor in surgery, general and internal medicine), prior work experience in the field of neurology or training in general medicine (Austria, Denmark, Ireland, Norway, Portugal, Serbia, Slovenia, Sweden, UK). Because of the prerequisites in Ireland and the UK, the total duration from medical school graduation until certification as a neurologist added up to 96 and 120 months, respectively (Table S2). See Table S3 for the national representatives’ opinion on the duration.
The median (range) training time spent in a neurology department (the total duration of the residency training programme minus external rotations and prerequisites) was 43 (11.5–62) months (Fig. 2, bottom half).
Disease‐specific subspecialty training in neurology
We aimed to identify which of the following specific disease categories residents were required to see during residency training: neurovascular diseases (including stroke), epilepsy, neuromuscular diseases, movement disorders, neurocognitive disorders (including dementia), immune‐mediated disorders [including multiple sclerosis and other (auto‐)immune disorders], infectious diseases, headache, neurotraumatology, neuro‐oncology and pain syndromes. In 17 of the 32 countries (53%), the respondents stated that all of these categories were seen during their residency training; however, this differed between hospitals within a single country. Neurotraumatology, neuro‐oncology and pain syndromes were not seen in 47%, 25% and 16% of countries, respectively. In these countries, the respective disorders were part of residency training programmes in neurosurgery, oncology and anaesthesiology.
The way in which knowledge of and experience with the above‐mentioned diseases were acquired differed between countries. Some had specific rotations to subspecialty sections within the neurology department, such as multiple sclerosis, movement disorders, headache, etc. Others responded that they saw a wide variety of neurological diseases while working on the neurology ward or in the outpatient clinic.
Although most respondents spent training time in a stroke unit, a defined mandatory period in a stroke unit was only required in 17/32 countries (53%) (duration 1–12 months). Training on the intensive care unit, with a duration of 1–6 months, was specified in the 15 national programmes (47%).
Clinical neurophysiology was either a separate field of training or integrated within the neurology training programme. In 21/32 countries (66%), residents learned to perform and interpret clinical neurophysiological examinations, such as electroencephalography, electromyography, nerve conduction studies and ultrasound, during the residency training programme. The method of obtaining knowledge about clinical neurophysiology differed between countries, from a brief theoretical course to a defined minimum number of investigations to be performed.
External rotations to other medical disciplines/departments
All countries included in the study, except Belgium and Romania, had mandatory rotations to other medical departments prior to or during the residency training programme, mostly to psychiatry (22 countries, 69%), internal medicine (21; 66%) and neurosurgery (19; 59%) (Table 2), and less frequently to radiology (12; 38%) and paediatric neurology (12; 38%). In a few countries, the training programme included very short rotations in a wide range of other disciplines, e.g. neurorehabilitation (six countries), ophthalmology (3), ear/nose/throat clinic (2) and anaesthesiology (2). In the 22 countries with a mandatory psychiatry rotation, the duration was generally short (up to 4 months), with the exception of Germany (12 months). For internal medicine, rotation lasted up to 3 months in 10/21 countries. In contrast, Switzerland, Ireland and the UK required a duration of 12, 24 and 36 months in internal medicine, respectively. In the latter two countries this was part of the foundation programme. The duration of rotations to neurosurgery ranged mostly between 1 and 3 months, whereas Albania and Norway required 6 months. Voluntary rotations to other medical disciplines during residency were possible in 10/32 countries (31%), allowing different time periods and departments to be accredited as part of the neurology residency training programme (Table 3).
Table 2.
Obligatory rotations to external medical disciplines: psychiatry, internal medicine, neurosurgery (data from 32 countries)
| Obligatory rotation to psychiatry (69%) a | |||
|---|---|---|---|
| No rotation | ≤4 months | 6 months | 12 months |
| 10 countries (31%) | 15 countries (47%) | 3 countries (9%) | 1 country (3%) |
| Austria, Belgium, France, Ireland, Malta, Netherlands, Norway, Romania Switzerland, Ukraine | Belarus, Croatia, Denmark, Estonia, Hungary, Italy, Latvia, Macedonia, Moldova, Poland, Portugal, Serbia, Slovakia, Spain, Turkey | Albania, Greece, Slovenia | Germany |
| Obligatory rotation to internal medicine (66%) | |||
|---|---|---|---|
| No rotation | ≤3 months | 6–9 months | ≥12 months |
| 11 countries (34%) | 13 countries (41%) | 3 countries (9%) | 3 countries (9%) |
| Albania, Belarus, Belgium, Croatia, Denmark, France, Germany, Netherlands, Norway, Romania, Ukraine | Austria, Hungary, Italy, Latvia, Macedonia, Malta, Moldova, Poland, Portugal b , Serbia, Slovakia, Spain, Turkey | Estonia, Greece, Slovenia | Ireland c , Switzerland, UK c |
| Obligatory rotation to neurosurgery (59%) | |||
|---|---|---|---|
| No rotation | 1 month | 2–3 months | 6 months |
| 11 countries (34%) | 5 countries (16%) | 8 countries (25%) | 2 countries (6%) |
| Austria, Belarus, Belgium, Croatia, France, Germany, Greece, Romania, Switzerland, Turkey, Ukraine | Italy, Latvia, Macedonia, Serbia, Slovakia | Demark, Estonia, Hungary, Malta, Netherlands, Portugal, Slovenia, Spain | Albania, Norway |
In the UK, part of the foundation programme; Lithuania and Sweden have a rotation to psychiatry, duration is missing.
During general training.
During the foundation programme.
Table 3.
Voluntary rotations to external medical disciplines
| Voluntary rotations to external medical fields in the residency training programme of 10 countries (31%) | ||
|---|---|---|
| Country | Time (months) | Medical fields accounted for in the residency programme |
| Belgium | 24 | Internal medicine, psychiatry |
| Germany | 12 | Internal medicine, general medicine, neurosurgery, neuropathology, neuroradiology, physiology, anatomy |
| Netherlands | 12 | Any medical field with link to neurology, research, teaching or management |
| Norway | 12 | Research or other clinical department, or laboratory or in health administration/social medicine or in general medicine |
| Switzerland | 12 | Neuroradiology, neurosurgery, neuropaediatrics, psychiatry, intensive care |
| Portugal | 11 | Any medical field with link to neurology |
| France | 6 | Any medical field |
| Slovenia | 6 | Any medical field, often research |
| Sweden | 3 | Any medical field |
| Estonia | 2 | Clinical genetics, internal medicine, ophthalmology |
Thrombectomies in the residency training programmes
In all countries included in this survey, thrombectomies were performed, mostly by (interventional) neuroradiologists, but in five countries also by neurologists (France, Greece, Hungary, the Netherlands, Turkey). Only in Spain and France did the respondents state that it was possible to learn to perform thrombectomies during the neurology residency training programme.
Evidence‐based medicine, teaching and leadership training
Training in evidence‐based medicine was specifically defined as a part of the neurology residency training programme in 14/32 countries (44%). In 21 countries (66%), there was no mandatory defined training in teaching or medical leadership skills. However, attention to these aspects of medical training varied greatly between hospitals within a single country.
Examinations
An examination was required in 24/32 countries (75%), during (21 countries, 66%) and/or at the end (24; 75%) of the residency training programme. In 54% of these 24 countries, the final examination was centrally organized, mostly consisting of an oral and a written part (11; 46%). The representatives from Spain, Denmark and Sweden reported that there were no obligatory examinations within the residency training programme.
In 14/32 countries (44%), neurologists reported that they were required to provide proof of continuing medical training after obtaining their neurology degree to maintain their registration as a neurologist, accomplished by obtaining continuing medical education (CME) points, following courses and visiting congresses.
Discussion
In most European countries, exposure to a similarly wide range of patients and diseases can be expected. Our results, however, reveal that there are still many differences between neurology residency training programmes across Europe. Underlying reasons might be in part historical and political, influenced by how and when neurology evolved into an independent specialism. Shedding more light on the origins of the disparities between neurology residency training programmes will therefore require historical research, which was outside the scope of the present study.
The UEMS, Section of Neurology published a guideline for residency training programmes in Europe [3]. The most important recommendations of the guideline were: (i) a duration of 5 years for the residency training programme, of which 4 years should be within the neurology department; (ii) evidence‐based training in different fields of neurology; (iii) examination(s) during or at the end of the residency programme; (iv) regular quality assessments of the residency training programme; and (v) a system facilitating/ensuring lifelong learning.
Regarding the duration, we observed a broad range in the total duration of programmes and in the minimum duration spent in the neurology department itself. Not all countries fulfilled the requirements regarding the total duration and the time spent in the neurology department. Clinical neurophysiology was counted as an integral part of neurology in some countries, whereas in others it was regarded as a separate speciality.
External rotations are heavily under debate in several countries. We observed a wide range in duration and structure of external rotations, including rotations to disciplines not directly related to neurology, such as gastroenterology, pulmonology and haematology. The conflict here is to provide exposure to neighbouring disciplines, while allowing sufficient time for the increasingly complex neurological core curriculum. Knowledge gained about comorbidities in external rotations such as internal medicine can be valuable in an ageing population and the multimorbidity seen in neurological patients. Rotations to (neuro)radiology are of great value for interpreting patients’ magnetic resonance imaging and computed tomography scans at first hand, with potentially immediate treatment consequences. However, the rapid developments in diagnostic and therapeutic options for many neurological disorders means that subspecialization has increased. To fulfil the future need for highly specialized neurologists, it could be argued that residents should have the possibility of being trained more extensively in one or more specific fields during their training. Therefore, amplifying the opportunities for voluntary external rotations as part of the residency training programmes might strengthen subspecialization within neurology. However, broadly trained neurologists remain essential, especially in private practices (outpatient clinics) or when on call as attending neurologist. Thus, there is also an argument for postponing further subspecialization to the period after the completion of a ‘broad neurology’ residency training.
Examination is an important element of the residency training programme, according to the UEMS. Most countries had an examination during and/or at the end of the residency training programme, although the format differed between countries. Harmonization of a European examination has been initiated via The European Board of Examination, organized by the UEMS, Section of Neurology. However, in none of the countries included in this survey is it national policy to consider this examination equal to their own national examination.
Lastly, the requirements of a system of regular quality assessments and facilitation of lifelong learning were not fully met in most investigated countries.
According to the CanMEDS model, a model for residency training developed in Canada [6], a medical professional should have multiple competences, including research, teaching, medical leadership, collaboration and communication skills, in addition to medical skills. Some of the included countries offered the possibility of gaining experience in such skills, which was valued as important according to recent surveys among residents and young neurologists in the USA [7, 8].
Our survey has some strengths and limitations. We performed a comprehensive survey addressing multiple topics in many European countries, which was feasible via the RRFS national representatives’ network. Thereby, we were able to obtain interesting information and provide an updated overview that continues and extends prior investigations [4, 5]. However, a single RRFS national representative might not be aware of all aspects of the residency programme in her or his country, nor of all the requirements or obligations they face as a neurologist, leading to a possible underestimation of the countries who actually have a system of life‐long learning. Therefore, we did not assess teaching communication skills, use of competencies and/or a portfolio, as these may vary between hospitals in a single country. Moreover, we missed data from 15 European countries. Therefore, the data presented may not be representative of Europe as a whole.
Harmonization of European residency training programmes has been recommended [5]. Nevertheless, there are currently still many differences in the training programmes, mainly involving the spectrum of neurological disease categories to which residents are exposed. Although most countries have some sort of examination, the duration, structure, external rotations and training in evidence‐based medicine are still very different across Europe. Thus, in spite of previous recommendations and current guidelines [3, 4], our survey indicates that we are still far from a harmonized residency training programme [4]. In only 10/16 countries that had a junior neurological society was this society involved in the development of the training programme. We strongly encourage the involvement of junior neurologists in the constant process of optimizing the education of residents, which is vital in shaping the future of neurology.
Conclusion
The neurology residency training programmes across Europe showed many differences. The patient spectrum in neurology and their needs for neurological care (and therefore the knowledge and skills that have to be acquired by neurologists in training) are quite uniform across Europe. Thus, it was surprising that the length of the residency, the mandatory external rotations and many other aspects of this survey showed such variations. We recommend a critical evaluation of residency training programmes by relevance for neurologists today and in future in the light of global medical developments. Subspecialization within neurology can be strengthened by a greater emphasis on voluntary rotations to all kinds of medical departments relevant to the career plans of the individual neurologist in training, instead of obligatory rotations that might not always suit the requirements of current neurological practise. The UEMS and European Academy of Neurology should work on clear‐cut recommendations for the curriculum, to be used as a rational basis for the development of training programmes and the necessary organizational requirements.
Disclosure of conflicts of interest
G. Deuschl reports personal fees from Boston Scientific, Cavion, Functional Neuromodulation and Thieme Publishers, and grants from Medtronic outside the submitted work. None of the other authors declares any financial or other conflict of interest with respect to the topic of this research.
Supporting information
Table S1 The questionnaire was distributed to the national representatives of the following European countries (38), of which 32 responded.
Table S2 Prerequisites and entry to the residency programme.
Table S3 National representatives’ opinions on the total duration of the respective residency programme of his/her country.
Acknowledgements
We are very grateful for the contributions of the RRFS of the European Academy of Neurology representatives as part of the junior national representatives’ network, who completed the survey and therefore enabled this analysis: Albania (Aida Quka), Austria (Simon Fandler‐Höfler), Belarus (Ivan Goursky), Belgium (Tim Kelderman), Croatia (Vana Kosta), Denmark (Asger Toke Guld), Estonia (Liisa Kõrv), France (Philippe Codron and Lila Autier), Germany (Nina Kleineberg), Greece (Marianthi Breza), Hungary (Péter Orosz), Ireland (Hugh Kearney), Italy (Francesco Di Lorenzo), Latvia (Krista Svilāne), Lithuania (Irena Zagorskienė), North Macedonia (Marija Babunovska), Malta (Malcolm Vella), Moldova (Elena Costru‐Tasnic), Netherlands (Noor Godijn), Norway (Ida Bakke), Poland (Stanisław Szlufik), Portugal (Vanessa Carvalho), Romania (Tiu Vlad), Serbia (Marija Grunauer), Slovakia (Igor Straka), Slovenia (Eva Zupanic), Spain (David García Azorín and Maria Usero Ruiz), Sweden (Björn Evertsson), Switzerland (David Schreier), Turkey (Hatice Kurucu), UK (Samuel Shribman) and Ukraine (Kateryna Antonenko).
See commentary by M. de Visser et al. on page 1354.
References
- 1. Josephson SA. 100 Years of JAMA Neurology and the journey back to the beginning. JAMA Neurol 2019; 76: 1279–1280. [DOI] [PubMed] [Google Scholar]
- 2. GBD 2016 Neurology Collaborators. Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 2019; 18: 459–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. https://www.uems‐neuroboard.org/web/images/docs/exam/European‐Training‐Requirements‐Neurology‐accepted‐version‐21Oct16.pdf (accessed 06/12/2019)
- 4. Struhal W, Sellner J, Lisnic V, Vecsei L, Muller E, Grisold W. Neurology residency training in Europe – the current situation. Eur J Neurol 2011; 18: e36–e40. [DOI] [PubMed] [Google Scholar]
- 5. Zis P, Kuks JB. An up‐to‐date overview of neurology training in Europe. Eur J Neurol 2016; 23: e66–e74. [DOI] [PubMed] [Google Scholar]
- 6. Frank JR, Langer B. Collaboration, communication, management, and advocacy: teaching surgeons new skills through the CanMEDS Project. World J Surg 2003; 27: 972–978. [DOI] [PubMed] [Google Scholar]
- 7. Mahajan A, Cahill C, Scharf E, et al Neurology residency training in 2017: A survey of preparation, perspectives, and plans. Neurology 2019; 92: 76–83. [DOI] [PubMed] [Google Scholar]
- 8. Jordan JT, Mayans D, Schneider L, Adams N, Khawaja AM, Engstrom J. Education research: Neurology resident education: Trending skills, confidence, and professional preparation. Neurology 2016; 86: e112–e117. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1 The questionnaire was distributed to the national representatives of the following European countries (38), of which 32 responded.
Table S2 Prerequisites and entry to the residency programme.
Table S3 National representatives’ opinions on the total duration of the respective residency programme of his/her country.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


