Description
A 60-year-old male patient was diagnosed with SARS-CoV-2 infection by positive real-time fluorescence PCR using a nasopharyngeal swab specimen on the second day of symptoms. Due to mild clinical disease course with only cough and temperature up to 37.7°C, the patient was isolated at home for 14 days. The patient had an unremarkable medical history except for arterial hypertension (treated with β1-selective beta-blocker metoprolol) and for bronchial asthma (treated with inhaled topic β2-sympathomimetic agonists, either formoterol or salbutamol, with/without corticosteroids). No familial history of clotting problems was known. On day 14, a subjective improvement with disappearance of fever and cough was noted.
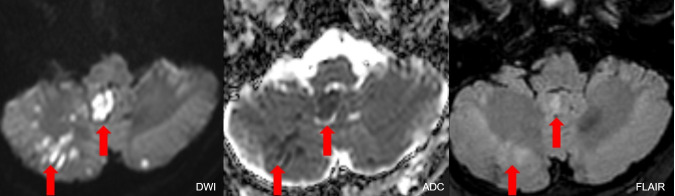
From day 14 to day 16, the patient complained of several short-lasting attacks of about 1 min with vertigo and occipital headache. On day 17, being without COVID-19 symptoms for 3 days, the patient got up in the morning with severe headache and with intense lasting vertigo and nausea. Ataxia and spontaneous nystagmus to the left were present. NIHSS (National Institute of Health Stroke Scale) was 1/42. A slight lymphopaenia with values of 0.76 (normal: 1.5–4 109/L) and a thrombocytosis of 459 (normal 150–400 109/L) was present presumably due to the recent COVID-19 disease. D-dimer were elevated with 2.54 mg/L (normal <0.60 mg/L). On precontrast CT, hyperdense artery sign in the right intracranial vertebral artery was observed. On postcontrast CT angiography, no opacification of the right intracranial vertebral artery and of the right posterior inferior cerebellar artery (PICA) was present. MRI on day 18 showed multifocal long-segment vessel occlusion with blooming artefact in the right intracranial vertebral artery and in the entire PICA on susceptibility-weighted MRI—minimum intensity projection images (figure 1). Extracranial vessels were not occluded. On diffusion-weighted imaging and on apparent diffusion coefficient maps, multiple areas with diffusion restriction and fluid-attenuated inversion recovery hyperintensity (partly marked with red arrows) were visible in vermis and both cerebellar hemispheres (figure 2).
Figure 1.
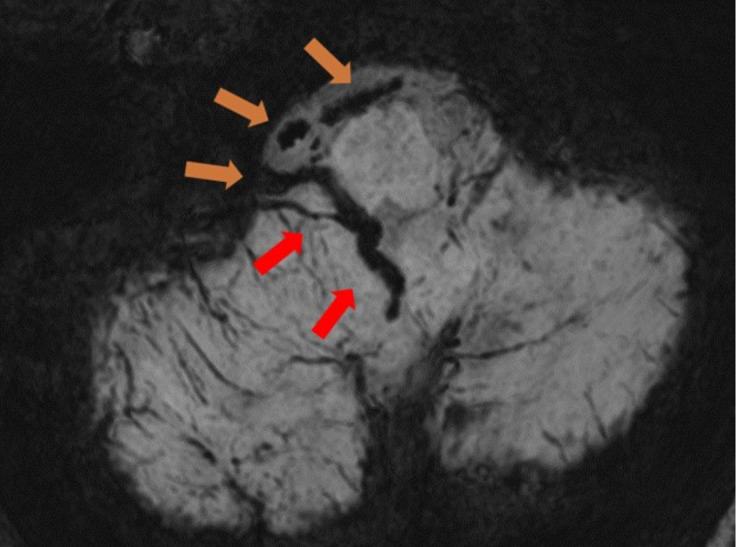
Minimum intensity projection of susceptibility weighted images presents multifocal acute hypointense thrombosis of the intracranial right vertebral artery (light brown arrows) and of the entire right PICA (red arrows).
Figure 2.
Multiple acute ischaemic areas in vermis and both cerebellar hemispheres with hyperintensity on diffusion-weighted imaging and reduced apparent diffusion coefficient due to diffusion restriction and with slight hyperintensity on fluid-attenuated inversion recovery are demonstrated, partly marked with red arrows.
Echocardiography on the 23rd day was normal and a cardiovascular embolic source was excluded. Long-term ECG over 72 hours was normal. The patient was treated with aspirin cardio and atorvastatin. He was sent to rehabilitation on the 25th day in unchanged neurological condition. An additional long-term ECG as well as laboratory investigations (with analysis of lupus anticoagulans, anti-cardiolipin antibodies and anti-beta-2-glycoprotein-1 antibodies) for exclusion of anti-phospholipid antibody syndrome were planned 3 months after hospital discharge. All results of these tests proved to be normal.
In this patient, with a previously uneventful medical history, a multifocal long-segment acute thrombosis of the intracranial right vertebral artery and of the entire length of the PICA resulted in multifocal acute ischaemic non-haemorrhagic infarcts in vermis and both cerebellar hemispheres. A thrombosis of this extent occurring not only in one but in two vessels is unusual even in patients with stroke with multiple cardiovascular risk factors. This long-segment thrombosis occurred shortly after mild COVID-19 disease. Therefore, we hypothesise that the vessel occlusion may have been caused by endotheliitis1 or as a consequence of an increased coagulopathy after COVID-19 disease2–7, even though a cardioembolic event due to paroxysmal atrial fibrillation (despite negative long-term ECG) or due to an previously undiagnosed homocystinaemia was not excluded.
Thrombotic complications with arterial and venous thromboses are reported in critically and severely ill patients suffering from COVID-19 in 31% of patients.2–5 7 Long-segment thromboses occurring in a subjectively recovered patient after a mild COVID-19 disease course has not been reported to date.
This case should arouse awareness of the possibility of severe ischaemic infarcts due to long-segment multivessel thrombosis in patients even after subjective recovery of a mild COVID-19 disease course.
Learning points.
Long-segment arterial thrombosis in multiple cerebral vessels is possible in COVID-19 disease.
The long-segment arterial thrombosis can even occur after clinical recovery in a mild disease course.
Footnotes
Contributors: ES, TS and SS-S wrote the paper. SS-S, JD and RI were the consulting physicians. JD and RI revised the paper.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lushina N, Kuo JS, Shaikh HA. Pulmonary, cerebral, and renal thromboembolic disease in a patient with COVID-19. Radiology 2020;296:E181–3. 10.1148/radiol.2020201623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Helms J, Kremer S, Merdji H, et al. Neurologic features in severe SARS-CoV-2 infection. New Engl J Med 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhang Y, Cao W, Xiao M, et al. [Clinical and coagulation characteristics of 7 patients with critical COVID-2019 pneumonia and acro-ischemia]. Zhonghua Xue Ye Xue Za Zhi 2020;41:E006. 10.3760/cma.j.issn.0253-2727.2020.0006 [DOI] [PubMed] [Google Scholar]
- 5.Mei H, Hu Y. [Characteristics, causes, diagnosis and treatment of coagulation dysfunction in patients with COVID-19]. Zhonghua Xue Ye Xue Za Zhi 2020;41:185–91. 10.3760/cma.j.issn.0253-2727.2020.0002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang Y, Xiao M, Zhang S, et al. Coagulopathy and antiphospholipid antibodies in patients with Covid-19. N Engl J Med 2020;382:e38. 10.1056/NEJMc2007575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klok FA, Kruip M, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]