Abstract
Background
This study investigated (i) whether compassion is associated with blood pressure or hypertension in adulthood and (ii) whether familial risk for hypertension modifies these associations.
Method
The participants (N = 1112–1293) came from the prospective Young Finns Study. Parental hypertension was assessed in 1983–2007; participants’ blood pressure in 2001, 2007, and 2011; hypertension in 2007 and 2011 (participants were aged 30–49 years in 2007–2011); and compassion in 2001.
Results
High compassion predicted lower levels of diastolic and systolic blood pressure in adulthood. Additionally, high compassion was related to lower risk for hypertension in adulthood among individuals with no familial risk for hypertension (independently of age, sex, participants’ and their parents’ socioeconomic factors, and participants’ health behaviors). Compassion was not related to hypertension in adulthood among individuals with familial risk for hypertension.
Conclusion
High compassion predicts lower diastolic and systolic blood pressure in adulthood. Moreover, high compassion may protect against hypertension among individuals without familial risk for hypertension. As our sample consisted of comparatively young participants, our findings provide novel implications for especially early-onset hypertension.
Electronic supplementary material
The online version of this article (10.1007/s12529-020-09886-5) contains supplementary material, which is available to authorized users.
Keywords: Blood pressure, Compassion, Personality, Familial risk, Health behavior, Hypertension
Introduction
The World Health Organization (WHO) has estimated that raised blood pressure causes even 12.8% of all deaths [1]. There is a great amount of evidence that even modest decreases in systolic blood pressure predict a substantially lower risk for major cardiovascular disease events, coronary heart disease, stroke, and heart failure [2, 3]. By now, it is widely known that certain psychological traits, especially anxiety and depression, increase the risk for raised blood pressure [4, 5]. However, recent research suggests that focusing on the positive determinants of health—instead of the negative ones—may be more helpful in obtaining the American Heart Association’s health goals of improving cardiovascular health [6]. Although some research suggests that personalities with higher emotional vitality have better cardiovascular health [7], the current evidence has remained scarce with regard to which specific positive personality traits that might promote better cardiovascular health and protect against raised blood pressure and hypertension.
Dispositional compassion for others might be one essential trait protecting against adverse cardiovascular outcomes. Compassion is defined as a disposition to feel concern for other’s suffering that is followed by the desire to alleviate the suffering [8]. Dispositional compassion includes three characteristics that may make it especially important in the context of heart diseases. Firstly, the onset of heart diseases is known to be affected both by affective and behavioral factors. Contrary to most previously investigated psychosocial factors (e.g., positive affect or amount of exercise), compassion includes simultaneously both an affective element (recognizing close other’s emotional distress and tolerating it) and a behavioral element (willingness to take the behavioral steps to reduce other’s distress) [9, 10]. Hence, compassion might include a beneficial psychological profile in the light of heart diseases. Secondly, the benefits of most psychosocial qualities are context-dependent: for example, the effectiveness of specific stress-coping strategies is very dependent on the psychosocial context where they take place [11]. Instead, compassion is suggested to represent a fundamental need for human being since it promotes possibilities to live in harmony with important others and protects from social exclusion [12]. Finally, while positive affectivity and other temperament traits have quite a strong biological basis, compassion is susceptible for environmental factors and can be effectively trained even within a relatively short time period [13–16], providing practical implications for interventions.
Additionally, personality traits may promote better cardiovascular health via more frequent favorable health behaviors [17, 18]. It has been demonstrated that high compassion is linked with a lower risk for excessive energy intake and eating-related problem behavior [19], with a lower risk for at-risk alcohol use and smoking [20, 21], and with lower consumption of some caffeine-including drinks [22]. Modification of those health behaviors, in turn, is shown to be a very effective treatment for raised blood pressure [23, 24]. Taken together, high compassion may likely promote favorable health behaviors and, in that way, protect against the incidence of raised blood pressure and hypertension.
Importantly, in addition to health behaviors, also genetic factors have a substantial influence on the incidence of raised blood pressure [25]. There is also evidence for a substantial transmission of hypertension from parents to their offspring [26]. Overall, it has been estimated that genetic factors contribute to as much as 50% of blood pressure variation [27].
The interaction between genetic factors and psychosocial factors in the occurrence of cardiovascular diseases has been widely demonstrated [27]. For those with familial risk for hypertension, the causes lie to larger extent in genes whereas health behaviors play somewhat a lesser role [28]. Previously, even such statements have been proposed that some individuals may have inherited hypertensive levels of blood pressure [28]. Accordingly, the relationship of compassion with blood pressure may be different among individuals with and without a familial risk for hypertension. Specifically, the potential protective role of compassion against the development of hypertension may be limited among individuals with a strong genetic risk for hypertension. Consequently, compassion may potentially protect against hypertension more strongly among such individuals who do not have familial risk for hypertension and whose hypertension is more strongly linked to adverse health behaviors, such as smoking, alcohol use, and obesity. This topic, however, has still remained unexplored.
To our knowledge, this is the first study to investigate the relationship of compassion for others with blood pressure and hypertension. Specifically, the aim of the present study was to examine (i) whether compassion for others is associated with diastolic or systolic blood pressure or hypertension in adulthood and (ii) whether a familial risk for hypertension modifies the association of compassion with hypertension and blood pressure. Intergenerational data with a 31-year prospective follow-up was used. The data provided possibilities to control for a wide range of covariates, including age, sex, participants’ and their parents’ socioeconomic factors, smoking status, alcohol use, body mass index, physical activity, and coffee consumption.
Materials and Methods
Participants
We used data from the prospective Young Finns Study. The participants were selected randomly from six age cohorts (born between 1962 and 1977) from the population register of the Social Insurance Institution. The Social Insurance Institution covers the whole population of Finland. The original sample included 3596 participants in the baseline measurement in 1980 (when participants were aged 3–18 years). The participants have been followed since then so that the latest follow-up measurement was in 2011 (participants were aged 24–49 years). The study was carried out in accordance with the Declaration of Helsinki. Furthermore, the design of the Young Finns Study was approved by all the Finnish universities with medical schools. Before participation, all the participants or their parents (for participants aged below 12 years) provided informed consent after the nature of the procedures had been fully explained. The design of the Young Finns Study is described with more detail elsewhere [29].
For this study, parental hypertension was assessed in 1980, 1983, 1986, 1989, 1992, 2001, and 2007; offspring’s blood pressure and the use of antihypertensive medications in 2001, 2007, and 2011; offspring’s hypertension in 2007 and 2011; compassion in 2001; parental socioeconomic factors in 1980; offspring’s socioeconomic factors in 2011; body mass index, smoking status, alcohol use, and physical activity in 2001, 2007, and 2011; and coffee consumption in 2001. A timeline of the study design is available in Supplementary Table 1. In the analyses, all the participants with data on study variables in at least one of the measurement times (e.g., data available on diastolic blood pressure in 2001, 2007, or 2011; or on offspring’s hypertension in 2007 or 2011) were included. Hence, the sample size slightly varied between the analyses (1112–1293 participants).
Measures
Dispositional Compassion
Dispositional compassion was evaluated with the version 9 of the Temperament and Character Inventory [30]. Dispositional compassion is a subscale of the character dimension Cooperativeness of the TCI. The scale of dispositional compassion (α = .86 in the sample of this study) consists of 10 self-rating statements (e.g., “It gives me pleasure to help others, even if they have treated me badly”; “It gives me pleasure to see my enemies suffer” [reverse scored]) that are rated with a 5-point Likert scale ranging from 1 (completely disagree) to 5 (completely agree). The mean score of compassion was calculated for all the participants who had data on at least 50% of the items. In the analyses, the standardized score (mean = 0; SD = 1; 10th percentile = − 1.293; 90th percentile = 1.094) of dispositional compassion was used. Previous studies have confirmed the reliability of the scale [31]. Moreover, the convergent and discriminant validity has also been confirmed, described in detail elsewhere [32]. Specifically, high values of the dispositional compassion have been shown to correlate with higher sociability, altruistic behavior, and positive emotionality [33, 34] whereas low values of the compassion are related to higher hostility, aggression, and narcissistic and psychopathic features [33, 35–37].
Diastolic and Systolic Blood Pressure and Antihypertensive Medications
Blood pressure was measured in sitting position after 5-min rest. A mercury sphygmomanometer at phases 1 and 2 and with a random zero sphygmomanometer (Hawksley & Sons Ltd) at phase 3 was used. Cuff size for the measurement covered two-thirds of the participant’s arm length. Korotkoff’s first phase was determined as the indicator of systolic blood pressure. Readings to the nearest even number of millimeters of mercury were conducted 3 times for each participant. In the analyses, the average values of diastolic and systolic blood pressure were used between the three measurements. Information about the use of antihypertensive was derived from health care records. Use of antihypertensive medications was included as covariate in the analyses when predicting blood pressure.
Hypertension
The presence of participants’ and their parents’ hypertension was evaluated using self-rating questionnaires. Participants and their parents were asked whether they had been diagnosed with hypertension. A two-class variable was computed referring to whether participants had been diagnosed with hypertension or not in 2007 or 2011 (0 = not diagnosed; 1 = diagnosed). Regarding the familial risk for hypertension, a variable was computed indicating whether at least one parent reported having been diagnosed with hypertension in 1980, 1983, 1986, 1989, 1992, 2001, or 2007 (0 = not diagnosed; 1 = diagnosed).
When defining indicators of hypertension, the current study did not use cut-off scores of systolic and diastolic blood pressure or the use of antihypertensive medications because this would have resulted in ambiguities and potential for bias. That is, the cut-off points for blood pressure have remained a controversial topic (various cut-offs have been suggested) and, additionally, different cut-offs have been recommended for subpopulations like diabetics [38]. Furthermore, repeated measurements in various environments (that were not available) are needed before diagnosing hypertension [38]. Antihypertensive medications are often used for a variety of purposes (e.g., for migraine) in Finland (see the Finnish current care guidelines here: https://www.kaypahoito.fi/en/) and are, thus, not necessarily a reliable indicator of hypertension. Also in our sample, there were participants who reported having been diagnosed by a doctor with migraine, cerebral infarction, or psychiatric disorders (but not with hypertension) and who used antihypertensive medications. Hence, many participants seemed to be using antihypertensive medications due to other somatic or neuropsychiatric diseases.
Socioeconomic Factors
Participants’ and their parents’ socioeconomic factors included education and level of income. Parental educational level was classified into 3 categories (1, comprehensive school; 2, high school or occupational school; 3, academic level). Level of parental income included 8 categories (1, less than 15,000 Finnish mark (2523€) per year; 8, more than 100,000 Finnish mark (16,819€) per year). Participants’ education was defined as the number of educational years (ranging between 8 and 30 years). Participants’ level of income was assessed with a 13-point scale (1 = less than 5000€ per year; 13 = more than 60,000€ per year). All the continuous socioeconomic variables (i.e., parents’ level of income, participants’ number of educational years, participants’ level of income) were standardized (mean = 0, SD = 1). The socioeconomic factors were added to the analyses as separate variables.
Health Behaviors
Covariates included coffee consumption, smoking status, alcohol use, body mass index, physical activity, and socioeconomic factors in childhood and adulthood. Coffee consumption was defined as the number of cups of coffee per day. Body mass index was calculated as weight (kg) divided by height squared (m2). Body mass index was included in health behaviors since it reflects the balance between energy intake and consumption. Smoking status was determined by asking the participants how often they were smoking (1 = daily smoking; 5 = never smoked). Smoking status was classified into two categories (1 = daily smoking; 0 = not daily smoking). Alcohol use was measured by asking the participants for the number of intoxications per year (i.e., the use of 6 or more portions of alcohol at a time). The scale ranged from 1 (2 times or more per week) to 6 (less than once a year). All the covariates were standardized with the mean of 0 and standard deviation of 1.
The scale of physical activity included 5 items asking about participants’ physical activity (items can be found in Supplementary Material). The total score of physical activity was defined as the standardized mean of the standardized items (mean = 0, SD = 1), so that each item had an equal weight for the total score of physical activity. The mean score of physical activity was calculated for all the participants who had data on at least 50% of the items. The internal consistency for the scale of physical activity ranged between α = .80 and .83 in 2001–2011. This scale of physical activity has been used also previously [39].
Statistical Analyses
Attrition was examined by comparing the included and excluded participants with regard to study variables using chi-square tests and independent samples t tests. The association of offspring’s compassion with diastolic and systolic blood pressure was investigated using linear regression analyses. The mean scores of diastolic and systolic blood pressure between years 2007 and 2011 were predicted by compassion. The mean scores of diastolic and systolic blood pressure were calculated for all the participants with data available on blood pressure in baseline measurement 2001 and also in at least one of the outcome measurement points (2007 and 2011) (N = 1103). Model 1 was adjusted for diastolic/systolic blood pressure at the baseline measurement in 2001, age, sex, and use of antihypertensive medications in 2001, 2007, and 2011; model 2 was adjusted also for participants’ and their parents’ socioeconomic factors; and model 3 was adjusted also for health behaviors (coffee consumption, smoking status, alcohol use, body mass index, and physical activity).
Next, the associations of familial risk for hypertension and offspring’s compassion with hypertension were investigated using logistic regression analyses where offspring’s hypertension was predicted by compassion, familial risk for hypertension, and their interaction. Model 1 was adjusted for age and sex; model 2 also for participants’ and their parents’ socioeconomic factors; and model 3 also for health behaviors (smoking status, alcohol use, body mass index, physical activity, and coffee consumption). In the logistic regression analyses, the standardized mean scores of indicators of health behaviors (smoking status, alcohol use, body mass index, physical activity) between measurement years 2001, 2007, and 2011 were used. The mean scores of health behaviors were calculated for all the participants who had data available about health behaviors in at least one of the measurement years.
Results
The descriptive statistics of the study variables are shown in Table 1. Attrition analyses revealed that women were more likely to participate than men (41.3% vs. 31.3%, p < .001). Included participants were slightly older than excluded participants (31.67 vs. 31.31, p < .05). There was no attrition bias in the level of compassion or in the frequency of hypertension. However, included participants’ parents had more likely hypertension than excluded participants’ parents (63.2% vs. 52.3%, p < .001). Additionally, included participants had slightly lower level of diastolic blood pressure (74.87 vs. 76.20, p < .01) and systolic blood pressure (119.17 vs. 121.15, p < .001) than excluded participants. With regard to health behaviors, it was found that included participants had lower level of coffee consumption (3.25 vs. 3.68, p < .001), were less likely to smoke daily (17.6% vs. 23.8%, p < .001), used alcohol less frequently (4.57 vs. 4.31, p < .001), and were more active physically (0.02 vs. − 0.04, p < .01) than excluded participants. There was no attrition bias in body mass index or in the use of antihypertensive medications. Regarding socioeconomic factors, included participants had more educational years (15.61 vs. 14.85, p < .001) than excluded participants, but there was no attrition bias in the level of income. Finally, included participants’ parents had slightly higher level of income (4.91 vs. 4.73, p < .01) and were less likely to have low educational level (32.1% vs. 36.2%, p < .05) than excluded participants’ parents.
Table 1.
The means, standard deviations (SD), frequencies, and ranges of the study variables
| Variable (measurement year) | Mean | SD | Range | Frequency (%) |
|---|---|---|---|---|
| Age in 2001 (years) | 31.67 | 5.03 | 24; 39 | |
| Sex (female) | 757 (58.1) | |||
| Parents | ||||
| Hypertension | 818 (63.2) | |||
| Educational level (1980) | ||||
| Comprehensive school | 418 (32.1) | |||
| High school or occupational school | 539 (41.4) | |||
| Academic level | 346 (26.6) | |||
| Level of income (1980) | 4.91 | 1.92 | 1; 8 | |
| Participants | ||||
| Compassion in 20011 | 3.68 | 0.64 | 1; 5 | |
| Systolic blood pressure (mmHg) | ||||
| 2001 | 115.96 | 12.90 | 80.67; 166.67 | |
| 2007 | 120.04 | 13.90 | 77.33; 168.67 | |
| 2011 | 118.26 | 13.90 | 83.33; 178.67 | |
| Diastolic blood pressure (mmHg) | ||||
| 2001 | 70.33 | 10.35 | 40.00; 111.33 | |
| 2007 | 75.23 | 11.08 | 42.00; 120.00 | |
| 2011 | 74.44 | 10.24 | 42.00; 113.33 | |
| Use of antihypertensive medications | ||||
| 2001 | 26 (2.0) | |||
| 2007 | 82 (6.8) | |||
| 2011 | 122 (9.5) | |||
| Hypertension (2007/2011) | 115 (8.8) | |||
| Coffee consumption (cups per day) (2001) | 3.25 | 2.60 | 0; 18 | |
| Daily smoker (2007/2011) | 229 (17.6) | |||
| Alcohol use (2007/2011) | 4.59 | 1.24 | 1; 6 | |
| Physical activity (2007/2011) | 0.02 | 0.64 | − 1.66; 1.86 | |
| Body mass index (2007/2011) | 25.69 | 4.47 | 16.86; 54.47 | |
| Number of educational years (2011) | 15.61 | 3.58 | 8; 34 | |
| Level of income (2011) | 7.32 | 3.02 | 1; 13 | |
1Unstandardized value of compassion. In the analyses, the standardized value of compassion (mean = 0, SD = 1) were used. The descriptive statistics were calculated for all the participants who were included in any analysis of this study (i.e., analysis about blood pressure or analysis about hypertension). Moreover, for alcohol use, physical activity, and body mass index, the mean between the measurement years was used
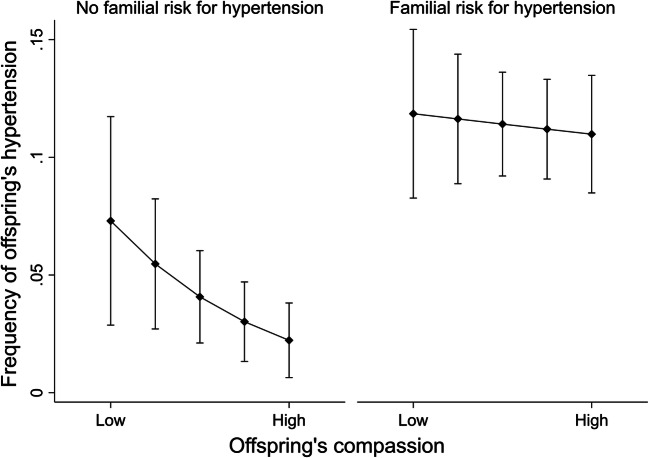
Table 2 shows the results of linear regression analyses when predicting diastolic and systolic blood pressure in 2007–2011 by compassion in 2001. The interaction effect of compassion with familial risk for hypertension was non-significant when predicting diastolic blood pressure (p = .330) and systolic blood pressure (p = .636). Hence, familial risk for hypertension was excluded from the models. Subsequently, the results revealed that high compassion predicted significantly lower levels of diastolic and systolic blood pressure when adjusted for age, sex, and parents’ and offspring’s socioeconomic factors (see Fig. 1). When adjusted also for participants’ health behaviors, the effect of compassion on diastolic and systolic blood pressure became non-significant.
Table 2.
The results of linear regression analyses when predicting blood pressure by compassion. Estimates with 95% confidence intervals (CI)
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| B | 95% CI | Beta | B | 95% CI | Beta | B | 95% CI | Beta | |
| Diastolic blood pressure (2007/2011) | |||||||||
| Age | 0.13** | 0.05; 0.22 | 0.07 | 0.08 | − 0.01; 0.17 | 0.04 | 0.06 | − 0.03; 0.15 | 0.03 |
| Sex1 | 3.13*** | 2.28; 3.99 | 0.16 | 3.22*** | 2.33; 4.12 | 0.16 | 2.77*** | 1.82; 3.72 | 0.14 |
| Baseline diastolic blood pressure (2001) | 0.58*** | 0.54; 0.63 | 0.61 | 0.58*** | 0.54; 0.63 | 0.62 | 0.55*** | 0.51; 0.60 | 0.59 |
| Parents’ level of income (1980) | − 0.10 | − 0.59; 0.38 | − 0.01 | 0.01 | − 0.46; 0.49 | 0.00 | |||
| Parents’ educational level (1980) | − 0.82* | − 1.48; − 0.17 | − 0.06 | − 0.86* | − 1.51; − 0.21 | − 0.07 | |||
| Participants’ level of income (2011) | − 0.10 | − 0.59; 0.38 | − 0.02 | − 0.23 | − 0.68; 0.23 | − 0.02 | |||
| Participants’ years of education (2011) | − 0.65** | − 1.09; − 0.21 | − 0.07 | − 0.55* | − 0.99; − 0.11 | − 0.06 | |||
| Coffee consumption (2001) | 0.12 | − 0.34; 0.59 | 0.01 | ||||||
| Smoking status2 (2007/2011) | − 0.80 | − 1.97; 0.37 | − 0.03 | ||||||
| Alcohol use (2007/2011) | − 0.42 | − 0.92; 0.08 | − 0.04 | ||||||
| Body mass index (2007/2011) | 1.29*** | 0.84; 1.75 | 0.13 | ||||||
| Physical activity (2007/2011) | − 0.11 | − 0.56; 0.34 | − 0.01 | ||||||
| Compassion (2001) | − 0.55* | − 0.99; − 0.11 | − 0.05 | − 0.50* | − 0.94; − 0.07 | − 0.05 | − 0.45* | − 0.88; − 0.02 | − 0.04 |
| Systolic blood pressure (2007/2011) | |||||||||
| Age | 0.32*** | 0.21; 0.43 | 0.13 | 0.27*** | 0.16; 0.38 | 0.10 | 0.23*** | 0.12; 0.35 | 0.09 |
| Sex1 | 3.15*** | 2.01; 4.29 | 0.12 | 3.10*** | 1.90; 4.30 | 0.12 | 2.48*** | 1.21; 3.75 | 0.10 |
| Baseline systolic blood pressure (2001) | 0.64*** | 0.59; 0.68 | 0.64 | 0.63*** | 0.59; 0.68 | 0.63 | 0.61*** | 0.57; 0.66 | 0.61 |
| Parents’ level of income (1980) | − 0.37 | − 0.98; 0.25 | − 0.03 | − 0.24 | − 0.85; 0.37 | − 0.02 | |||
| Parents’ educational level (1980) | − 0.57 | − 1.41; 0.26 | − 0.03 | − 0.60 | − 1.43; 0.23 | − 0.04 | |||
| Participants’ level of income (2011) | − 0.03 | − 0.60; 0.55 | 0.00 | 0.00 | − 0.58; 0.58 | 0.00 | |||
| Participants’ years of education (2011) | − 1.01*** | − 1.57; − 0.45 | − 0.08 | − 0.84** | − 1.41; − 0.27 | − 0.07 | |||
| Coffee consumption (2001) | 0.39 | − 0.20; 0.98 | 0.03 | ||||||
| Smoking status2 (2007/2011) | − 0.53 | − 2.02; 0.96 | − 0.02 | ||||||
| Alcohol use (2007/2011) | − 0.60 | − 1.24; 0.04 | − 0.04 | ||||||
| Body mass index (2007/2011) | 1.19*** | 0.61; 1.77 | 0.09 | ||||||
| Physical activity (2007/2011) | − 0.30 | − 0.88; 0.27 | − 0.02 | ||||||
| Compassion (2001) | − 0.61* | − 1.17; − 0.05 | − 0.04 | − 0.56* | − 1.11; − 0.00 | − 0.04 | − 0.48 | − 1.03; 0.07 | − 0.04 |
***p < .001; **p < .01; *p < .05. 1Female as the reference group. 2Participants without daily smoking as the reference group. N = 1112. Model 1, adjusted for age, sex, the baseline level of diastolic/systolic blood pressure, and the use of antihypertensive medications. Model 2, adjusted also for parents’ and offspring’s socioeconomic factors. Model 3, adjusted also for health behaviors. Compassion was standardized to mean = 0 and SD = 1. Hence, B refers to change in blood pressure (mmHg) per one-unit change (i.e., 1-SD change) in compassion
Fig. 1.
Predicted means with 95% confidence intervals of (i) diastolic blood pressure and (ii) systolic blood pressure (measured in 2007/2011) with different levels of compassion (measured in 2001), ranging from low (10th percentile) to high (90th percentile). Adjusted for age, sex, the use of antihypertensive medications in 2001, 2007, and 2011, and the baseline level of diastolic/systolic blood pressure in 2001
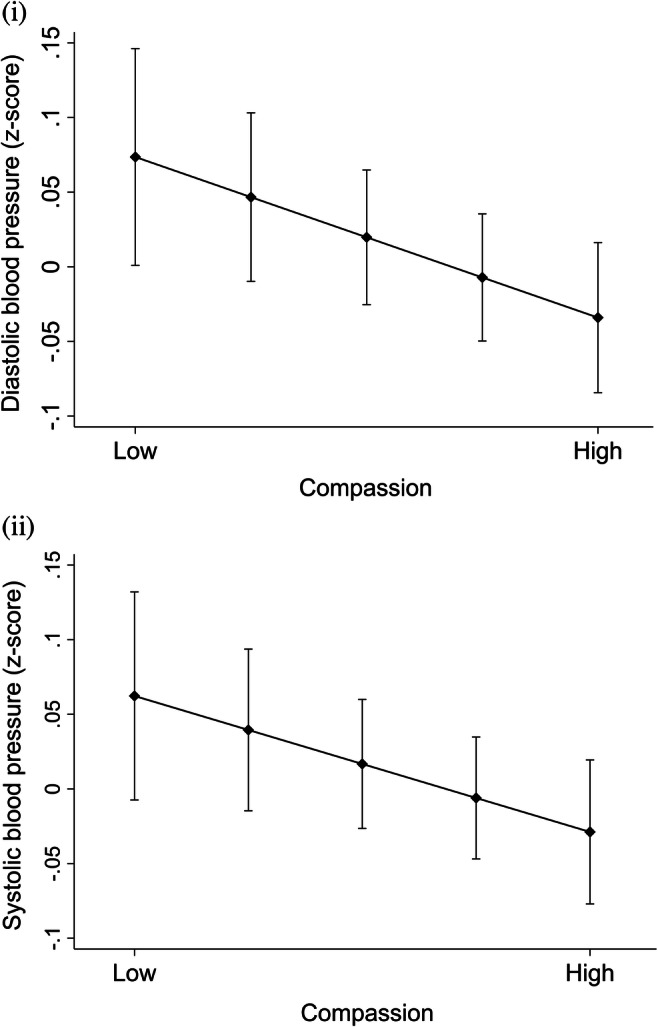
When predicting offspring’s hypertension by compassion in the total sample (without considering familial risk for hypertension), compassion did not have significant effect on hypertension in any of the models (p > .05) (for further information, see Supplementary Table 2). After adding familial risk for hypertension and the interaction effect between compassion and familial risk for hypertension, there was a significant positive interaction effect between compassion and the familial risk for hypertension (p = .030) in predicting offspring’s hypertension.
Because there was a significant interaction effect between familial risk for hypertension and compassion, the association of offspring’s compassion with hypertension was investigated separately among participants with and without familial risk for hypertension. Among individuals without familial risk for hypertension (Table 3), a 1-SD increase in compassion was related to 0.49 times lower odds for hypertension. Instead, among individuals with high familial risk for hypertension (Table 3), compassion was not related to hypertension. The effects were independent of age, sex, offspring’s and their parents’ socioeconomic factors, and health behaviors (i.e., smoking status, alcohol use, body mass index, physical activity, and coffee consumption). These results are illustrated in Fig. 2 where high compassion predicted a lower risk for hypertension among individuals without familial risk for hypertension but not among individuals with familial risk for hypertension.
Table 3.
The results of logistic regression analyses when predicting hypertension in 2007/2011 by compassion among participants with (N = 817) and without (N = 476) familial risk for hypertension. Estimates (B) and odds ratios (OR) with 95% confidence intervals (CI)
| Model 1 | Model 2 | Model 3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| B | OR | 95% CI | B | OR | 95% CI | B | OR | 95% CI | |
| Among participants without familial risk for hypertension | |||||||||
| Age | 0.18** | 1.20 | 1.07; 1.36 | 0.18** | 1.20 | 1.06; 1.36 | 0.20** | 1.22 | 1.06; 1.40 |
| Sex1 | 1.03 | 2.80 | 0.92; 8.50 | 0.87 | 2.38 | 0.70; 8.09 | 0.79 | 2.21 | 0.52; 9.37 |
| Parents’ level of income (1980) | − 0.36 | 0.70 | 0.40; 1.22 | − 0.29 | 0.75 | 0.40; 1.40 | |||
| Parents’ educational level (1980) | − 0.14 | 0.87 | 0.37; 2.08 | − 0.18 | 0.85 | 0.31; 2.25 | |||
| Participants’ level of income (2011) | 0.39 | 1.48 | 0.81; 2.68 | 0.54 | 1.71 | 0.87; 3.36 | |||
| Participants’ years of education (2011) | − 0.10 | 0.91 | 0.51; 1.61 | − 0.17 | 0.85 | 0.42; 1.69 | |||
| Coffee consumption (2001) | − 0.09 | 0.91 | 0.47; 1.75 | ||||||
| Smoking status2 (2007/2011) | − 0.78 | 0.46 | 0.07; 2.83 | ||||||
| Alcohol use (2007/2011) | 0.00 | 1.00 | 0.51; 1.98 | ||||||
| Body mass index (2007/2011) | 1.05*** | 2.85 | 1.70; 4.77 | ||||||
| Physical activity (2007/2011) | − 0.28 | 0.76 | 0.43; 1.33 | ||||||
| Compassion (2001) | − 0.66* | 0.52 | 0.30; 0.89 | − 0.69* | 0.50* | 0.29; 0.87 | − 0.71* | 0.49 | 0.26; 0.93 |
| Among participants with familial risk for hypertension | |||||||||
| Age | 0.12*** | 1.13 | 1.07; 1.18 | 0.12*** | 1.12 | 1.07; 1.18 | 0.10*** | 1.10 | 1.04; 1.17 |
| Sex1 | 0.31 | 1.36 | 0.88; 2.11 | 0.46 | 1.59 | 1.00; 2.53 | 0.15 | 1.16 | 0.70; 2.01 |
| Parents’ level of income (1980) | 0.06 | 1.06 | 0.81; 1.38 | 0.16 | 1.18 | 0.88; 1.57 | |||
| Parents’ educational level (1980) | − 0.12 | 0.89 | 0.62; 1.26 | − 0.19 | 0.83 | 0.57; 1.21 | |||
| Participants’ level of income (2011) | − 0.29 | 0.75* | 0.58; 0.96 | − 0.29* | 0.75 | 0.57; 0.98 | |||
| Participants’ years of education (2011) | − 0.04 | 0.96 | 0.75; 1.23 | − 0.02 | 0.98 | 0.76; 1.27 | |||
| Coffee consumption (2001) | 0.00 | 1.00 | 0.78; 1.28 | ||||||
| Smoking status2 (2007/2011) | − 0.66 | 0.52 | 0.26; 1.04 | ||||||
| Alcohol use (2007/2011) | − 0.37** | 0.69 | 0.53; 0.90 | ||||||
| Body mass index (2007/2011) | 0.79*** | 2.21 | 1.76; 2.77 | ||||||
| Physical activity (2007/2011) | − 0.22 | 0.80 | 0.62; 1.04 | ||||||
| Compassion (2001) | − 0.05 | 0.95 | 0.76; 1.20 | − 0.04 | 0.96 | 0.77; 1.21 | 0.03 | 1.03 | 0.80; 1.33 |
***p < .001; **p < .01; *p < .05. 1Female as the reference group. 2Participants without daily smoking as the reference group. Total N = 1293. Model 1, adjusted for age and sex. Model 2, adjusted also for parents’ and offspring’s socioeconomic factors. Model 3, adjusted also for health behaviors. Compassion was standardized to mean = 0 and SD = 1. Hence, OR refers to change in probability of hypertension per one-unit change (i.e., 1-SD change) in compassion
Fig. 2.
Predicted frequencies (%) with 95% confidence intervals of offspring’s hypertension (measured in 2007/2011) separately for participants with/without familial risk for hypertension (measured in 1980–2007) and with different levels of compassion (measured in 2001), ranging from low (10th percentile) to high (90th percentile). Adjusted for age and sex
Discussion
This was the first study to investigate the relationship of compassion for others with diastolic and systolic blood pressure and hypertension and whether familial risk might modify this relationship. High compassion predicted slightly lower levels of diastolic and systolic blood pressure in adulthood both among individuals with and without familial risk for hypertension. Additionally, familial risk for hypertension modified the association of compassion with hypertension in adulthood. That is, among individuals with no familial risk for hypertension, high compassion for others predicted a decreased risk for hypertension in adulthood, whereas among individuals with familial risk for hypertension, compassion for others was not related to hypertension in adulthood. This suggests that compassion has a health-protective effect but only in individuals who are at low genetic risk for hypertension.
We found that the effect of compassion on blood pressure somewhat attenuated after controlling for health behaviors, implying that the relationship of compassion with blood pressure may partially proceed via favorable health behaviors. This is in line with previous studies demonstrating that compassion is related to a lower risk for excessive energy intake, smoking, substance use, and caffeine-including drinks [19–22, 40] that, in turn, are linked with lower blood pressure [28, 41, 42]. Importantly, it has been suggested that certain types of health behaviors may have only a relatively transient effect on blood pressure over time. For example, alcohol use, physical activity, and coffee consumption may predict changes in blood pressure over the following hours but not thereafter [43–46]. Correspondingly, interventions targeting health behaviors are shown to effectively lower the level of blood pressure comparatively rapidly [47–49]. This may potentially provide one explanation why the link of compassion with variations in blood pressure levels (at single measurement times) may partially proceed via health behaviors, whereas the link of compassion with hypertension (i.e., a more stable and long-lasting form of raised blood pressure) was not attenuated and actually rather became stronger after controlling for health behaviors health behaviors.
Hence, our findings suggested that the association of high compassion with a decreased risk for hypertension may proceed via some other pathways than health behaviors. Generally, it has been suggested that psychological factors may protect against raised blood pressure by altering central nervous system control of such physiological reactivity patterns that are related to cardiovascular functioning [18, 50]. By now, there is evidence that compassionate states are related to lower heart rate, higher respiratory sinus arrhythmia, and higher heart rate variability [51, 52] that, in turn, are linked with a lower risk for hypertension [53, 54]. Moreover, brain imaging studies have suggested that high compassion is related to higher activity in such brain structures that contribute to the regulation of blood pressure [55]. Taken together, hypertension is a comparatively stable trait resulting from a complex pattern of cardiovascular, endocrinological, and respiratory functioning [56], and this pattern may be affected by compassion.
Previously, several studies have found that individuals with genetic risk factors are more susceptible for environmental risk factors, when predicting coronary heart disease and myocardial infarction [57, 58]. Consequently, environmental risk factors and genetic vulnerabilities are suggested to be cumulated in the pathology of cardiovascular diseases [59]. This may result from epigenetic effects, indicating that environmental stressors activate heart disease–related genes that, in turn, predispose to increased risk for coronary heart disease or infarction [60].
Importantly, however, it has been highlighted that empirical evidence for the interplay between genetic and environmental factors in the context of hypertension is very limited [61]. Our findings suggested that high compassion predicts a decreased risk for hypertension only among individuals without familial risk for hypertension. This is in line with the statements that among individuals with a lack of genetic risk for hypertension, the protective role of psychological factors may be significant [28]. That is, in case an individual has lower genetic risk for hypertension, there may exist more variance in the incidence of hypertension to be explained by psychosocial factors such as compassion. This is also in line with a previous study reporting that amount of exercise had no effect on blood pressure in individuals with a specific genetic variant [62]. Moreover, as the lack of familial risk for hypertension may likely imply the presence of protective genes against hypertension, our results suggest that the protective effect of compassion may cumulate with protective genetic factors in the development and maintenance of healthy blood pressure levels.
Previously, it has been found that the role of genetic factors in the etiology of hypertension is especially strong in early-onset hypertension (i.e., onset before 55 years age) [63]. In the present study, the participants were aged below 55 years (34–49 years), so that all the cases of offspring’s hypertension could be classified as early-onset hypertension. Future studies could investigate whether the protective role of compassion might be stronger against late-onset hypertension that is less strongly transmitted from one generation to the next than early-onset hypertension [26], implying that the incidence of late-onset hypertension might be especially susceptible to psychosocial factors.
The present study had some methodological limitations that must be taken into consideration. Firstly, data were not available on participants’ hypertension in 2001. Hence, no firm conclusions can be made whether the hypertensive cases were incident before or after the measurement of compassion. However, because the youngest participants were only 24-year-olds at the measurement time of compassion, it is likely that most of the hypertension cases have emerged thereafter. Secondly, hypertension was assessed with self-report questionnaires, instead of using data from health care registers. Nevertheless, there is evidence that the self-reports of hypertension show an acceptable agreement with information from medical databases [64] and provide a highly accurate estimate of presence of hypertension [65, 66]. Additionally, parents were asked whether they had been diagnosed with hypertension by a doctor, not whether they mere thought having hypertension. Moreover, it has been demonstrated that the prevalence of undiagnosed hypertension is comparatively low among the Finnish population [67], suggesting that the knowledge of hypertension is at a high level in Finland. Hence, it has been concluded that self-reports can be used, with caution, as a measure of raised blood pressure or hypertension [64, 65].
Thirdly, compassion was measured with a self-rating questionnaire; it was susceptible to social desirability bias. Nevertheless, it is challenging to measure compassion with other measures than self-ratings since it reflects one’s internal feelings and experiences. Compassionate states could be measured with, for example, some electrophysiological measures such as heart rate variability [51]. However, heart rate variability does not reflect experience of compassion on a quite stable level over situations, and therefore was not suitable for the present study. Moreover, the reliability and validity of the compassion scale are shown to be high [31, 33, 34] and self-rating methods have been used also previously [52].
The present study had also several substantial strengths. Firstly, to our knowledge, this was the first study to investigate the relationship of compassion for others with blood pressure and hypertension. Secondly, this study used a comparatively large population-based sample (N = 1112–1293) that was likely to present the general population with regard to most of its characteristics. Thirdly, this study used intergenerational data with a 31-year prospective follow-up that enabled us to investigate whether familial risk for hypertension modifies the association of compassion with raised blood pressure. This kind of prospective study, clarifying how psychological and biological factors interact in the etiology of hypertension, has previously been demanded (5) but has not been conducted previously. Fourthly, this study could clarify potential pathways from compassion to blood pressure and hypertension by controlling for a variety of factors, such as age, sex, use of antihypertensive medications, socioeconomic factors, and health behaviors (coffee consumption, alcohol use, smoking status, body mass index, physical activity).
Previously, it has been estimated that the worldwide prevalence of hypertension is about 31% [68]. Among individuals with raised blood pressure, about 77% are using antihypertensive medications [69]. However, a severe concern has been expressed that antihypertensive medications seem not to be effective for a great portion of hypertensive patients [28], with estimates ranging from 12% to even 40% of the drug-treated population [70–72]. Furthermore, a substantial number of hypertensive patients experience a wide variety of side effect symptoms related to antihypertensive medications, for example, fatigue, insomnia, depressive symptoms, and weight gain [73].
Hence, there has been a wide consensus that, besides antihypertensive medications and lifestyle changes, hypertensive patients should be provided also with psychosocial interventions that aim at increasing stress management and relaxation [74–76]. Importantly, however, several intervention studies and meta-analyses have concluded that the current relaxation techniques, stress reduction programs, or cognitive-behavioral therapies seem not to be effective treatment methods for raised blood pressure [77–79]. Hence, there is an acute need for the development of novel psychosocial treatments. By now, intervention studies have suggested that practicing compassion might be a comparatively effective method to alleviate a range of psychiatric symptoms, such as depression, anxiety, stress, and psychotic symptoms [80, 81]. Our findings suggest that high compassion may predict lower diastolic and systolic blood pressure and also protect against hypertension among individuals without familial risk for hypertension. Future studies could investigate whether compassion-enhancing interventions might have beneficial effects on blood pressure.
Electronic Supplementary Material
(DOCX 40 kb).
Funding Information
Open access funding provided by University of Oulu including Oulu University Hospital. This study was supported financially by the Academy of Finland (M.H., grant number 308676); the Signe and Ane Gyllenberg Foundation (T.L, M.H.); and the Jenny and Antti Wihuri Foundation (L.P.-R.). The Young Finns Study has been financially supported by the Academy of Finland: Grants 322098, 286284, 134309 (Eye), 126925, 121584, 124282, 129378 (Salve), 117797 (Gendi), and 41071 (Skidi); the Social Insurance Institution of Finland; Competitive State Research Financing of the Expert Responsibility area of Kuopio, Tampere and Turku University Hospitals (grant X51001); the Juho Vainio Foundation; the Sigrid Juselius Foundation; the Yrjö Jahnsson Foundation; the Paavo Nurmi Foundation; the Finnish Foundation of Cardiovascular Research and Finnish Cultural Foundation; the Tampere Tuberculosis Foundation; the Emil Aaltonen Foundation; and Diabetes Research Foundation of Finnish Diabetes Association and EU Horizon 2020 (grant 755320 for TAXINOMISIS); and European Research Council (grant 742927 for MULTIEPIGEN project) and Tampereen Yliopistollisen sairaalan tukisäätiö.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Finnish universities with medical schools and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Before participation, all the participants or their parents (for participants aged below 12 years) provided informed consent after the nature of the procedures had been fully explained.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization (WHO). Raised blood pressure report. Available at: http://www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence_text/en/. Last Accessed on July 2, 2018.
- 2.Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, Chalmers J, Rodgers A, Rahimi K. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–967. doi: 10.1016/S0140-6736(15)01225-8. [DOI] [PubMed] [Google Scholar]
- 3.Heerspink HJL, Ninomiya T, Zoungas S, de Zeeuw D, Grobbee DE, Jardine MJ, Gallagher M, Roberts MA, Cass A, Neal B, Perkovic V. Effect of lowering blood pressure on cardiovascular events and mortality in patients on dialysis: a systematic review and meta-analysis of randomised controlled trials. Lancet. 2009;373:1009–1015. doi: 10.1016/S0140-6736(09)60212-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meng L, Chen D, Yang Y, Zheng Y, Hui R. Depression increases the risk of hypertension incidence: a meta-analysis of prospective cohort studies. J Hypertens. 2012;30:842–851. doi: 10.1097/HJH.0b013e32835080b7. [DOI] [PubMed] [Google Scholar]
- 5.Player MS, Peterson LE. Anxiety disorders, hypertension, and cardiovascular risk: a review. Int J Psychiatry Med. 2011;41:365–377. doi: 10.2190/PM.41.4.f. [DOI] [PubMed] [Google Scholar]
- 6.Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, van Horn L, Greenlund K, Daniels S, Nichol G, Tomaselli GF, Arnett DK, Fonarow GC, Ho PM, Lauer MS, Masoudi FA, Robertson RM, Roger V, Schwamm LH, Sorlie P, Yancy CW, Rosamond WD, American Heart Association Strategic Planning Task Force and Statistics Committee Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic impact goal through 2020 and beyond. Circulation. 2010;121:586–613. doi: 10.1161/CIRCULATIONAHA.109.192703. [DOI] [PubMed] [Google Scholar]
- 7.Trudel-Fitzgerald C, Gilsanz P, Mittleman MA, Kubzansky LD. Dysregulated blood pressure: can regulating emotions help. Curr Hypertens Rep. 2015;17:92. doi: 10.1007/s11906-015-0605-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goetz JL, Keltner D, Simon-Thomas E. Compassion: an evolutionary analysis and empirical review. Psychol Bull. 2010;136:351–374. doi: 10.1037/a0018807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gilbert P. Compassion: concepts, research and applications. London: Routledge; 2017. [Google Scholar]
- 10.Gilbert P, Mascaro J. Compassion: fears, blocks, and resistances: an evolutionary investigation. In: Seppälä M, Simon-Thomas E, Brown SK, Worline MC, Cameron L, Doty JR, editors. The Oxford handbook of compassion science. Oxford University Press: New York; 2017. pp. 399–420. [Google Scholar]
- 11.DeLongis A, Holtzman S. Coping in context: the role of stress, social support, and personality in coping. J Pers. 2005;73:1633–1656. doi: 10.1111/j.1467-6494.2005.00361.x. [DOI] [PubMed] [Google Scholar]
- 12.Sheldon KM, Elliot AJ. Goal striving, need satisfaction, and longitudinal well-being: the self-concordance model. J Pers Soc Psychol. 1999;76:482–497. doi: 10.1037//0022-3514.76.3.482. [DOI] [PubMed] [Google Scholar]
- 13.Jazaieri H, Jinpa GT, McGonigal K, Rosenberg EL, Finkelstein J, Simon-Thomas E, Cullen M, Doty JR, Gross JJ, Goldin PR. Enhancing compassion: a randomized controlled trial of a compassion cultivation training program. J Happiness Stud. 2013;14:1113–1126. [Google Scholar]
- 14.Kirby JN. Compassion interventions: the programmes, the evidence, and implications for research and practice. Psychol Psychother. 2017;90:432–455. doi: 10.1111/papt.12104. [DOI] [PubMed] [Google Scholar]
- 15.Kirby JN, Tellegen CL, Steindl SR. A meta-analysis of compassion-based interventions: current state of knowledge and future directions. Behav Ther. 2017;48:778–792. doi: 10.1016/j.beth.2017.06.003. [DOI] [PubMed] [Google Scholar]
- 16.Mongrain M, Chin JM, Shapira LB. Practicing compassion increases happiness and self-esteem. J Happiness Stud. 2011;12:963–981. [Google Scholar]
- 17.Ushakov VA, Ivanchenko SV, Gagarina AA. Psychological stress in pathogenesis of essential hypertension. Curr Hypertens Rev. 2016;12:203–214. doi: 10.2174/1573402112666161230121622. [DOI] [PubMed] [Google Scholar]
- 18.Smith TW. Personality as risk and resilience in physical health. Curr Dir Psychol Sci. 2006;15:227–231. [Google Scholar]
- 19.Vervaet M, Van Heeringen C, Audenaert K. Personality-related characteristics in restricting versus binging and purging eating disordered patients. Compr Psychiatry. 2004;45:37–43. doi: 10.1016/j.comppsych.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 20.Gluschkoff K, Pulkki-Råback L, Elovainio M, et al. Is it good to be good? Dispositional compassion and health behaviors. Ann Behav Med. 2018;53:665–673. [DOI] [PubMed]
- 21.Schiep S, Cieślik K. Personality dimensions and nicotine dependence and withdrawal symptoms: the mediating role of self-directness. Pol Psychol Bull. 2011;42:169–177. [Google Scholar]
- 22.Lara DR, Antoniolli E, Frozi J, Schneider R, Ottoni GL. Distinct personality traits associated with intake of coffee, tea, and cola drinks and smoking. J Caffeine Res. 2011;1:101–108. [Google Scholar]
- 23.Baena CP, Olandoski M, Younge JO, Buitrago-Lopez A, Darweesh SKL, Campos N, Sedaghat S, Sajjad A, van Herpt TTW, Freak-Poli R, van den Hooven E, Felix JF, Faria-Neto JR, Chowdhury R, Franco OH. Effects of lifestyle-related interventions on blood pressure in low and middle-income countries: systematic review and meta-analysis. J Hypertens. 2014;32:961–973. doi: 10.1097/HJH.0000000000000136. [DOI] [PubMed] [Google Scholar]
- 24.Bond BJ. Lifestyle intervention strategies for the prevention and treatment of hypertension: a review. Am J Lifestyle Med. 2011;5:346–360. [Google Scholar]
- 25.Padmanabhan S, Newton-Cheh C, Dominiczak AF. Genetic basis of blood pressure and hypertension. Trends Genet. 2012;28:397–408. doi: 10.1016/j.tig.2012.04.001. [DOI] [PubMed] [Google Scholar]
- 26.Niiranen TJ, McCabe EL, Larson MG, et al. Risk for hypertension crosses generations in the community: a multi-generational cohort study. Eur Heart J. 2017;38:2300–2308. doi: 10.1093/eurheartj/ehx134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang B, Liao C, Zhou B, Cao W, Lv J, Yu C, Gao W, Li L. Genetic contribution to the variance of blood pressure and heart rate: a systematic review and meta-regression of twin studies. Twin Res Hum Genet. 2015;18:158–170. doi: 10.1017/thg.2015.8. [DOI] [PubMed] [Google Scholar]
- 28.Carretero OA, Oparil S. Essential hypertension: part I: definition and etiology. Circulation. 2000;101:329–335. doi: 10.1161/01.cir.101.3.329. [DOI] [PubMed] [Google Scholar]
- 29.Raitakari OT, Juonala M, Rönnemaa T, et al. Cohort profile: the cardiovascular risk in Young Finns Study. Int J Epidemiol. 2008;37:1220–1226. doi: 10.1093/ije/dym225. [DOI] [PubMed] [Google Scholar]
- 30.Cloninger CR, Przybeck TR, Švrakić DM. The Temperament and Character Inventory (TCI): a guide to its development and use. St. Louis: Center for Psychobiology of Personality, Washington; 1994. [Google Scholar]
- 31.Hansenne M, Delhez M, Cloninger CR. Psychometric properties of the Temperament and Character Inventory–Revised (TCI–R) in a Belgian sample. J Pers Assess. 2005;85:40–49. doi: 10.1207/s15327752jpa8501_04. [DOI] [PubMed] [Google Scholar]
- 32.Hintsanen M, Gluschkoff K, Dobewall H, Cloninger CR, Keltner D, Saarinen A, Wesolowska K, Volanen SM, Raitakari OT, Pulkki-Råback L. Parent–child-relationship quality predicts offspring dispositional compassion in adulthood: a prospective follow-up study over three decades. Dev Psychol. 2019;55:216–225. doi: 10.1037/dev0000633. [DOI] [PubMed] [Google Scholar]
- 33.García Ó, Aluja A, García LF, Escorial S, Blanch A. Zuckerman-Kuhlman-Aluja Personality Questionnaire (ZKA-PQ) and Cloninger’s Temperament and Character Inventory Revised (TCI-R): a comparative study. Scand J Psychol. 2012;53:247–257. doi: 10.1111/j.1467-9450.2012.00943.x. [DOI] [PubMed] [Google Scholar]
- 34.Schmidt KM, Llewellyn PL, Taylor GJ, Weber PG, Hong B, Sellers R, Wise C, Wolak C, McGaw L, Nielson S. Cloninger’s Temperament and Character Inventory correlates with personality characteristics of organ donation advocates. J Clin Psychol Med Settings. 2003;10:173–185. [Google Scholar]
- 35.De Fruyt F, De Clercq BJ, Van de Wiele L, Van Heeringen K. The validity of Cloninger’s psychobiological model versus the five-factor model to predict DSM-IV personality disorders in a heterogeneous psychiatric sample: domain facet and residualized facet descriptions. J Pers. 2006;74:479–510. doi: 10.1111/j.1467-6494.2006.00382.x. [DOI] [PubMed] [Google Scholar]
- 36.Lee J, Min SK, Kim KH, et al. Differences in temperament and character dimensions of personality between patients with Hwa-byung, an anger syndrome, and patients with major depressive disorder. J Affect Disord. 2012;138:10–116. doi: 10.1016/j.jad.2011.12.014. [DOI] [PubMed] [Google Scholar]
- 37.Paal T, Bereczkei T. Adult theory of mind, cooperation, Machiavellianism: the effect of mindreading on social relations. Personal Individ Differ. 2007;43:541–551. [Google Scholar]
- 38.Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I, ESC Scientific Document Group. de Backer G, Heagerty AM, Agewall S, Bochud M, Borghi C, Boutouyrie P, Brguljan J, Bueno H, Caiani EG, Carlberg B, Chapman N, Cífková R, Cleland JGF, Collet JP, Coman IM, de Leeuw PW, Delgado V, Dendale P, Diener HC, Dorobantu M, Fagard R, Farsang C, Ferrini M, Graham IM, Grassi G, Haller H, Hobbs FDR, Jelakovic B, Jennings C, Katus HA, Kroon AA, Leclercq C, Lovic D, Lurbe E, Manolis AJ, McDonagh TA, Messerli F, Muiesan ML, Nixdorff U, Olsen MH, Parati G, Perk J, Piepoli MF, Polonia J, Ponikowski P, Richter DJ, Rimoldi SF, Roffi M, Sattar N, Seferovic PM, Simpson IA, Sousa-Uva M, Stanton AV, van de Borne P, Vardas P, Volpe M, Wassmann S, Windecker S, Zamorano JL, Windecker S, Aboyans V, Agewall S, Barbato E, Bueno H, Coca A, Collet JP, Coman IM, Dean V, Delgado V, Fitzsimons D, Gaemperli O, Hindricks G, Iung B, Jüni P, Katus HA, Knuuti J, Lancellotti P, Leclercq C, McDonagh TA, Piepoli MF, Ponikowski P, Richter DJ, Roffi M, Shlyakhto E, Simpson IA, Sousa-Uva M, Zamorano JL, Tsioufis C, Lurbe E, Kreutz R, Bochud M, Rosei EA, Jelakovic B, Azizi M, Januszewics A, Kahan T, Polonia J, van de Borne P, Williams B, Borghi C, Mancia G, Parati G, Clement DL, Coca A, Manolis A, Lovic D, Benkhedda S, Zelveian P, Siostrzonek P, Najafov R, Pavlova O, de Pauw M, Dizdarevic-Hudic L, Raev D, Karpettas N, Linhart A, Olsen MH, Shaker AF, Viigimaa M, Metsärinne K, Vavlukis M, Halimi JM, Pagava Z, Schunkert H, Thomopoulos C, Páll D, Andersen K, Shechter M, Mercuro G, Bajraktari G, Romanova T, Trušinskis K, Saade GA, Sakalyte G, Noppe S, DeMarco DC, Caraus A, Wittekoek J, Aksnes TA, Jankowski P, Polonia J, Vinereanu D, Baranova EI, Foscoli M, Dikic AD, Filipova S, Fras Z, Bertomeu-Martínez V, Carlberg B, Burkard T, Sdiri W, Aydogdu S, Sirenko Y, Brady A, Weber T, Lazareva I, Backer TD, Sokolovic S, Jelakovic B, Widimsky J, Viigimaa M, Pörsti I, Denolle T, Krämer BK, Stergiou GS, Parati G, Trušinskis K, Miglinas M, Gerdts E, Tykarski A, de Carvalho Rodrigues M, Dorobantu M, Chazova I, Lovic D, Filipova S, Brguljan J, Segura J, Gottsäter A, Pechère-Bertschi A, Erdine S, Sirenko Y, Brady A. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021–3104. doi: 10.1093/eurheartj/ehy339. [DOI] [PubMed] [Google Scholar]
- 39.Hirvensalo M, Magnussen CG, Yang X, Telama R, Heinonen I, Hutri-Kähönen N, Salin K, Viikari J, Raitakari OT, Tammelin TH. Convergent validity of a physical activity questionnaire against objectively measured physical activity in adults: the cardiovascular risk in Young Finns Study. Adv Phys Educ. 2017;7:457–472. [Google Scholar]
- 40.Evren C, Evren B, Yancar C, Erkiran M. Temperament and character model of personality profile of alcohol-and drug-dependent inpatients. Compr Psychiatry. 2007;48:283–288. doi: 10.1016/j.comppsych.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 41.Fuchs FD, Chambless LE, Whelton PK, Nieto FJ, Heiss G. Alcohol consumption and the incidence of hypertension: the atherosclerosis risk in communities study. Hypertension. 2001;37:1242–1250. doi: 10.1161/01.hyp.37.5.1242. [DOI] [PubMed] [Google Scholar]
- 42.Niskanen L, Laaksonen DE, Nyyssönen K, et al. Inflammation, abdominal obesity, and smoking as predictors of hypertension. Hypertension. 2004;44:859–865. doi: 10.1161/01.HYP.0000146691.51307.84. [DOI] [PubMed] [Google Scholar]
- 43.Cornelissen VA, Verheyden B, Aubert AE, Fagard RH. Effects of aerobic training intensity on resting, exercise and post-exercise blood pressure, heart rate and heart-rate variability. J Hum Hypertens. 2010;24:175–182. doi: 10.1038/jhh.2009.51. [DOI] [PubMed] [Google Scholar]
- 44.Mesas AE, Leon-Muñoz LM, Rodriguez-Artalejo F, Lopez-Garcia E. The effect of coffee on blood pressure and cardiovascular disease in hypertensive individuals: a systematic review and meta-analysis. Am J Clin Nutr. 2011;94:1113–1126. doi: 10.3945/ajcn.111.016667. [DOI] [PubMed] [Google Scholar]
- 45.Rosito AG, Danni Fuchs F, Duncan BB. Dose-dependent biphasic effect of ethanol on 24-h blood pressure in normotensive subjects. Am J Hypertens. 1999;12:236–240. doi: 10.1016/s0895-7061(98)00237-4. [DOI] [PubMed] [Google Scholar]
- 46.Quinn TJ. Twenty-four hour, ambulatory blood pressure responses following acute exercise: impact of exercise intensity. J Hum Hypertens. 2000;14:547–553. doi: 10.1038/sj.jhh.1001106. [DOI] [PubMed] [Google Scholar]
- 47.Neter JE, Stam BE, Kok FJ, Grobbee DE, Geleijnse JM. Influence of weight reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2003;42:878–884. doi: 10.1161/01.HYP.0000094221.86888.AE. [DOI] [PubMed] [Google Scholar]
- 48.Whelton SP, Chin A, Xin X, He J. Effect of aerobic exercise on blood pressure: a meta-analysis of randomized, controlled trials. Ann Intern Med. 2002;136:493–503. doi: 10.7326/0003-4819-136-7-200204020-00006. [DOI] [PubMed] [Google Scholar]
- 49.Xin X, He J, Frontini MG, Ogden LG, Motsamai OI, Whelton PK. Effects of alcohol reduction on blood pressure: a meta-analysis of randomized controlled trials. Hypertension. 2001;38:1112–1117. doi: 10.1161/hy1101.093424. [DOI] [PubMed] [Google Scholar]
- 50.Cuffee Y, Ogedegbe C, Williams NJ, Ogedegbe G, Schoenthaler A. Psychosocial risk factors for hypertension: an update of the literature. Curr Hypertens Rep. 2014;16:483. doi: 10.1007/s11906-014-0483-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kirby JN, Doty JR, Petrocchi N, Gilbert P. The current and future role of heart rate variability for assessing and training compassion. Front Public Health. 2017;5:40. doi: 10.3389/fpubh.2017.00040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stellar JE, Cohen A, Oveis C, Keltner D. Affective and physiological responses to the suffering of others: compassion and vagal activity. J Pers Soc Psychol. 2015;108:572–585. doi: 10.1037/pspi0000010. [DOI] [PubMed] [Google Scholar]
- 53.Masi CM, Hawkley LC, Rickett EM, Cacioppo JT. Respiratory sinus arrhythmia and diseases of aging: obesity, diabetes mellitus, and hypertension. Biol Psychol. 2007;74:212–223. doi: 10.1016/j.biopsycho.2006.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Thayer JF, Yamamoto SS, Brosschot JF. The relationship of autonomic imbalance, heart rate variability and cardiovascular disease risk factors. Int J Cardiol. 2010;141:122–131. doi: 10.1016/j.ijcard.2009.09.543. [DOI] [PubMed] [Google Scholar]
- 55.Immordino-Yang MH, McColl A, Damasio H, Damasio A. Neural correlates of admiration and compassion. Proc Natl Acad Sci U S A. 2009;106:8021–8026. doi: 10.1073/pnas.0810363106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Staessen JA, Wang J, Bianchi G, Birkenhäger WH. Essential hypertension. Lancet. 2003;361:1629–1641. doi: 10.1016/S0140-6736(03)13302-8. [DOI] [PubMed] [Google Scholar]
- 57.Leander K, Hallqvist J, Reuterwall C, Ahlbom A, de Faire U. Family history of coronary heart disease, a strong risk factor for myocardial infarction interacting with other cardiovascular risk factors: results from the Stockholm Heart Epidemiology Program (SHEEP) Epidemiology. 2001;12:215–221. doi: 10.1097/00001648-200103000-00014. [DOI] [PubMed] [Google Scholar]
- 58.Pezzini A, Grassi M, Zotto ED, Archetti S, Spezi R, Vergani V, Assanelli D, Caimi L, Padovani A. Cumulative effect of predisposing genotypes and their interaction with modifiable factors on the risk of ischemic stroke in young adults. Stroke. 2005;36:533–539. doi: 10.1161/01.STR.0000155741.31499.c2. [DOI] [PubMed] [Google Scholar]
- 59.Schwartz AR, Gerin W, Davidson KW, Pickering TG, Brosschot JF, Thayer JF, Christenfeld N, Linden W. Toward a causal model of cardiovascular responses to stress and the development of cardiovascular disease. Psychosom Med. 2003;65:22–35. doi: 10.1097/01.psy.0000046075.79922.61. [DOI] [PubMed] [Google Scholar]
- 60.Whayne TF. Epigenetics in the development, modification, and prevention of cardiovascular disease. Mol Biol Rep. 2015;42:765–776. doi: 10.1007/s11033-014-3727-z. [DOI] [PubMed] [Google Scholar]
- 61.Franks PW. Identifying genes for primary hypertension: methodological limitations and gene–environment interactions. J Hum Hypertens. 2009;23:227–237. doi: 10.1038/jhh.2008.134. [DOI] [PubMed] [Google Scholar]
- 62.Franks PW, Bhattacharyya S, Luan JA, et al. Association between physical activity and blood pressure is modified by variants in the G-protein coupled receptor 10. Hypertension. 2004;43:224–228. doi: 10.1161/01.HYP.0000109319.63240.08. [DOI] [PubMed] [Google Scholar]
- 63.Wang NY, Young JH, Meoni LA, Ford DE, Erlinger TP, Klag MJ. Blood pressure change and risk of hypertension associated with parental hypertension: the Johns Hopkins Precursors Study. Arch Intern Med. 2008;168:643–648. doi: 10.1001/archinte.168.6.643. [DOI] [PubMed] [Google Scholar]
- 64.Tormo MJ, Navarro C, Chirlaque MD, Barber X. Validation of self diagnosis of high blood pressure in a sample of the Spanish EPIC cohort: overall agreement and predictive values. J Epidemiol Community Health. 2000;54:221–226. doi: 10.1136/jech.54.3.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Martin LM, Leff M, Calonge N, Garrett C, Nelson DE. Validation of self-reported chronic conditions and health services in a managed care population. Am J Prev Med. 2000;18:215–218. doi: 10.1016/s0749-3797(99)00158-0. [DOI] [PubMed] [Google Scholar]
- 66.Robinson JR, Young TK, Roos LL, Gelskey DE. Estimating the burden of disease: comparing administrative data and self-reports. Med Care. 1997;35:932–947. doi: 10.1097/00005650-199709000-00006. [DOI] [PubMed] [Google Scholar]
- 67.Korhonen PE, Kivelä SL, Kautiainen H, Järvenpää S, Kantola I. Health-related quality of life and awareness of hypertension. J Hypertens. 2011;29:2070–2074. doi: 10.1097/HJH.0b013e32834bbca7. [DOI] [PubMed] [Google Scholar]
- 68.Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, Chen J, He J. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016;134:441–450. doi: 10.1161/CIRCULATIONAHA.115.018912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gu Q, Burt VL, Dillon CF, Yoon S. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: the National Health and Nutrition Examination Survey, 2001 to 2010. Circulation. 2012;126:2105–2114. doi: 10.1161/CIRCULATIONAHA.112.096156. [DOI] [PubMed] [Google Scholar]
- 70.Holmqvist L, Boström KB, Kahan T, Schiöler L, Hasselström J, Hjerpe P, Wettermark B, Manhem K. Prevalence of treatment-resistant hypertension and important associated factors—results from the Swedish Primary Care Cardiovascular Database. J Am Soc Hypertens. 2016;10:838–846. doi: 10.1016/j.jash.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 71.Lloyd-Jones DM, Evans JC, Larson MG, O’donnell CJ, Roccella EJ, Levy D. Differential control of systolic and diastolic blood pressure: factors associated with lack of blood pressure control in the community. Hypertension. 2000;36:594–599. doi: 10.1161/01.hyp.36.4.594. [DOI] [PubMed] [Google Scholar]
- 72.Persell SD. Prevalence of resistant hypertension in the United States, 2003–2008. Hypertension. 2011;57:1076–1080. doi: 10.1161/HYPERTENSIONAHA.111.170308. [DOI] [PubMed] [Google Scholar]
- 73.Tedla YG, Bautista LE. Drug side effect symptoms and adherence to antihypertensive medication. Am J Hypertens. 2015;29:772–779. doi: 10.1093/ajh/hpv185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Daskalopoulou SS, Khan NA, Quinn RR, et al. The 2012 Canadian hypertension education program recommendations for the management of hypertension: blood pressure measurement, diagnosis, assessment of risk, and therapy. Can J Cardiol. 2010;28:270–287. doi: 10.1016/j.cjca.2012.02.018. [DOI] [PubMed] [Google Scholar]
- 75.Hackam DG, Khan NA, Hemmelgarn BR, Rabkin SW, Touyz RM, Campbell NR, Padwal R, Campbell TS, Lindsay MP, Hill MD, Quinn RR, Mahon JL, Herman RJ, Schiffrin EL, Ruzicka M, Larochelle P, Feldman RD, Lebel M, Poirier L, Arnold JM, Moe GW, Howlett JG, Trudeau L, Bacon SL, Petrella RJ, Milot A, Stone JA, Drouin D, Boulanger JM, Sharma M, Hamet P, Fodor G, Dresser GK, Carruthers SG, Pylypchuk G, Burgess ED, Burns KD, Vallée M, Prasad GV, Gilbert RE, Leiter LA, Jones C, Ogilvie RI, Woo V, McFarlane P, Hegele RA, Tobe SW, Canadian Hypertension Education Program The 2010 Canadian Hypertension Education Program recommendations for the management of hypertension: part 2–therapy. Can J Cardiol. 2010;26:249–258. doi: 10.1016/s0828-282x(10)70379-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Kuneš J, Zicha J. The interaction of genetic and environmental factors in the etiology of hypertension. Physiol Res. 2009;58:S33–S41. doi: 10.33549/physiolres.931913. [DOI] [PubMed] [Google Scholar]
- 77.Dickinson HO, Mason JM, Nicolson DJ, Campbell F, Beyer FR, Cook JV, Williams B, Ford GA. Lifestyle interventions to reduce raised blood pressure: a systematic review of randomized controlled trials. J Hypertens. 2006;24:215–233. doi: 10.1097/01.hjh.0000199800.72563.26. [DOI] [PubMed] [Google Scholar]
- 78.Rainforth MV, Schneider RH, Nidich SI, Gaylord-King C, Salerno JW, Anderson JW. Stress reduction programs in patients with elevated blood pressure: a systematic review and meta-analysis. Curr Hypertens Rep. 2007;9:520–528. doi: 10.1007/s11906-007-0094-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Stetter F, Kupper S. Autogenic training: a meta-analysis of clinical outcome studies. Appl Psychophysiol Biofeedback. 2002;27:45–98. doi: 10.1023/a:1014576505223. [DOI] [PubMed] [Google Scholar]
- 80.Leaviss J, Uttley L. Psychotherapeutic benefits of compassion-focused therapy: an early systematic review. Psychol Med. 2015;45:927–945. doi: 10.1017/S0033291714002141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lucre KM, Corten N. An exploration of group compassion-focused therapy for personality disorder. Psychol Psychother. 2013;86:387–400. doi: 10.1111/j.2044-8341.2012.02068.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 40 kb).