Abstract
Background and objectives
International and national health policies advocate greater integration of emergency and community care. The Physician Response Unit (PRU) responds to 999 calls ‘taking the Emergency Department to the patient’. Operational since 2001, the service was reconfigured in September 2017. This article presents service activity data and implications for the local health economy from the first year since remodelling.
Methods
A retrospective descriptive analysis of a prospectively maintained database was undertaken. Data collected included dispatch information, diagnostics and treatments undertaken, diagnosis and disposition. Treating clinical teams recorded judgments whether patients managed in the community would have been (1) conveyed to an emergency department (ED)and (2) admitted to hospital, in the absence of the PRU. Hospital Episode Statistics data and NHS referencing costs were used to estimate the monetary value of PRU activity.
Results
1924 patients were attended, averaging 5.3 per day. 1289 (67.0%) patients were managed in the community. Based on the opinion of the treating team, 945 (73.3%) would otherwise have been conveyed to hospital, and 126 (9.7%) would subsequently have been admitted. The service was estimated to deliver a reduction of 868 inpatient bed days and generate a net economic benefit of £530 107.
Conclusions
The PRU model provides community emergency medical care and early patient contact with a senior clinical decision-maker. It engages with community providers in order to manage 67.0% of patients in the community. We believe the PRU offers an effective model of community emergency medicine and helps to integrate local emergency and community providers.
Keywords: prehospital care, emergency care systems
Key messages.
What is already known on this subject
There is growing need to explore new models of emergency medical care due to increasing demand year-on-year, workforce challenges, an aging population and changes in service utilisation.
The NHS Long Term Plan includes a shift towards improving community emergency care in order to reduce strain on hospital services.
There is some evidence that schemes such as extended paramedic programmes and physician-led community emergency care can be implemented safely to reduce hospital attendances.
What this study adds
This study provides an in-depth descriptive analysis of a Physician Response Unit (PRU), which aims to take the ED to the patient and deliver safe and effective emergency care in the community setting.
The PRU model saw 1924 patients over the 12-month period, with 67.0% of patients being treated successfully in the community with follow-up initiated in 43.5% in order to facilitate ongoing community acute care.
The PRU replaced the need for three ambulance responses per day, and delivered an estimated total net saving of £530 107 based on clinical team judgment of likelihood of conveyance to hospital and admission if seen by standard resources.
Introduction
Background
Emergency healthcare access in the UK is complex and variable, and emergency departments (EDs) are under pressure due to increasing attendances and crowding.1 2 National and international health policy is directed towards greater integration of emergency and community care in order to improve outcomes and support the emergency system in the face of widespread challenges.3–5 In 2001, the Physician Response Unit (PRU) was developed to provide a physician-paramedic team responding by car to 999 calls in the area local to The Royal London Hospital.6 The PRU was formed collaboratively between London’s Air Ambulance, London Ambulance Service (LAS) and Barts & The London NHS Trust (now Barts Health NHS Trust) to support local ED and ambulance service performance in anticipation of new national standards being introduced by the Department of Health.7 The PRU model addressed a number of key priorities outlined within this strategic white paper, including reducing waiting times to see an emergency physician, improving accuracy of triage of patients to the correct service, and increasing the proportion receiving an ambulance response within 8 min in those who were critically unwell.6 Between 2001 and 2017, the service underwent several reconfigurations, operating Monday to Friday 08:00–17:00, delivering a prehospital doctor and paramedic with a clinical focus on cardiac arrests and critical care. In September 2017, the PRU underwent redevelopment in order to support a full spectrum of emergency clinical caseload, and to offer fellowship opportunities to emergency medicine doctors.
Current service description
The current PRU operating model is a senior emergency medicine doctor (ST4+ or consultant) working alongside an emergency ambulance crew (EAC) clinician. Team members undergo a period of clinical and operational training specific to the service prior to independent practice. The PRU is dispatched by the LAS Emergency Operations Centre (EOC) to all categories of emergency call between hours of 08:00 and 20:00, 7 days a week. The service covers a geographical area focused on the borough of Tower Hamlets, but also responding within Newham, City and Hackney, Waltham Forest, and beyond: a catchment that incorporates more than four EDs. The EOC tasks the PRU as for other LAS resources, with consideration by the dispatchers regarding the nature of the emergency in order to maximise value and clinical benefit. LAS crews can also request PRU as an additional unit where enhanced clinical quality and value may be offered.
A ‘tasking aid’ is available at the EOC which outlines suitable clinical presentations and the broad scope of practice of the PRU. Appropriate calls are described as ‘Patients who normally need ED assessment and treatment and whom would sometimes be admitted to hospital, but where diagnostics and treatments may be offered in the community’. This includes complaints such as head injuries, wounds, suspected infections/sepsis, delirium, falls, diabetic emergencies, breathing difficulties, urinary problems and palliative care patients. The tasking aid also makes clear that the PRU will respond to any calls that it is asked to, that is, maintaining a broad and willing response in support of the ambulance service.
The PRU may also attend patients who appear to be very unwell but will benefit from physician-delivered interventions to enhance pre-hospital clinical care, such as those in cardiac arrest, major trauma patients, and unconscious or agitated patients or those requiring airway support. Dispatchers are discouraged from sending the PRU to cases of isolated mental health issues, or where the patient definitely requires conveyance to an ED and there is no benefit from immediate pre-hospital intervention.
The service is well equipped with a broad range of therapeutic and diagnostic equipment (table 1), aiming to replicate much of the ED capability, while offering clinicians the opportunity to consider environmental and social factors that may be more evident in the community setting.
Table 1.
Non-exhaustive summary of diagnostic and therapeutic equipment carried by the Physician Response Unit
| Zoll X-series monitor: ● All standard observations 12-lead ECGAbbott iSTAT (Chem8+ & CG4+cartridges) ● Biochemistry panel incl. renal function ● Haemoglobin / haematocrit ● Arterial / venous blood gas (including lactate) Coaguchek ● International Normalised Ratio (INR) Urinalysis Urinary pregnancy test Peak Expiratory Flow Meter Opthalmoscope/Otoscope Blood Glucose Metre |
Medical care
Intravenous cannulation/blood taking equipment (peripheral and central lines) Large intravenous drug formulary ● Analgesics ● Antibiotics ● Anti-emetics ● Critical care medications including anaesthetic agents, sedatives and muscle relaxants ● Anti-convulsants ● Antiarrhythmics ● Tranexamic acid ● Thrombolytic agent ● Methoxyfluorane ● Salbutamol/ipratropium nebules/inhalers ● Various oral medications ● Entonox ● Prothrombin Complex Concentrate ● Hydroxycobalamin ● Pralidoxime ● Intravenous fluids Intraosseous access kit Oxygen/oxygen delivery apparatus |
Advanced cardiac arrest care
●Impedance Threshold Device (ResQPod) ●Active Compression-Decompression device ●Mechanical CPR (Autopulse) Pre-hospital emergency anaesthesia equipment ● Endotracheal tubes, supraglottic devices ● Bougies ● Airtraq ● Front of neck access kit ● End tidal CO2 colorimeter/continuous Co2 monitoring Woundcare ● Sutures; adhesive ● Dressings ● Benecast Splints (fracture management) Major trauma ● Hypertonic saline ● Thoracotomy kit ● Maxillofacial haemorrhage control ● Intercostal drains ● Haemostatic dressings ● Kendrick traction device ● Pelvic binder ● Combat Application Tourniquets Maternity equipment Laerdel Suction Unit |
| Other: PRU Directory of Services Remote access via computer to: ● Cerner Millennium ● East London Patient Record Personal Protective Equipment |
PRU, Physician Response Unit.
The PRU carries a computer with access to patients’ electronic records, allowing the team to review hospital and General Practitioner (GP) notes and results.
The expansion of the PRU has augmented the working relationships with community teams, available via a service directory created by the PRU team to facilitate onward care. Rapid response teams in each borough can arrange various interventions including clinical reviews, blood testing, intravenous antibiotic therapy at home, occupational therapy, physiotherapy and social worker input. In addition, there are district nursing teams, dedicated respiratory teams to provide ongoing care for patients with chronic obstructive airways disease, and local community hospice services. The PRU liaises closely with primary care services to communicate plans and arrange ongoing medical care as required. The service is able to arrange specialist review via acute ambulatory clinics such as an acute frailty clinic. Where patients require hospital conveyance, the PRU endeavours to deliver emergency therapies early in the patient journey, and referral to the appropriate receiving specialty.
The objective of this observational descriptive analysis is to delineate outcomes regarding service dispatch and clinical provision over a 12-month period, and provide an estimate of cost implications.
Methods
General methods
This study report has been written according to the Strengthening the Reporting of Observational studies in Epidemiology statement.8 Since September 2017, a prospectively maintained database was commenced collecting non-identifiable information regarding each patient encounter. Data collection and analysis was performed as ongoing service evaluation and was registered with the Barts Health NHS Trust Clinical Effectiveness Unit. Recorded items included tasking and demographic details, length of encounter, investigations and treatments delivered, and clinical disposition. Data were entered on the day of consultation by the treating team.
The classification of ambulance triage categories was standardised across the LAS, with dispatch categories guided by Advanced Medical Priority Dispatch System determinants. In October 2017, the ambulance response programme (ARP) was introduced in London9 setting out performance targets for ambulance dispatch. This had tasking implications for the service as the ARP mandates a conveying resource to be dispatched in some predetermined triage categories (the PRU not being equipped with an ambulance stretcher). Our 12-month data are presented below to include data both before and after introduction of the ARP.
Patient experience data was collated through the ‘I Want Great Care’ patient questionnaire utilised by the trust in the months of September and October 2017. Following this, data were captured using the ‘Friends and Family Test’. Only responses received from December 2017 to April 2018 were available and are included in the Results section.
Economic data
In order to estimate the potential cost savings, values were sourced from the 2017/2018 NHS referencing costs.10 The costs below were used in order for estimation of episode cost had the PRU not been utilised as a resource.
Average ambulance cost: ‘see, treat & refer’—£192.
Average ambulance cost: ‘see, treat & convey’—£252.
Average cost of ED attendance—£160.
Average cost of a non-elective inpatient admission per night (Barts Health NHS Trust)—£550.
For each encounter, the treating team indicated a response to the following questions in reference to those treated and left in the community:
In the absence of the PRU, do you think the patient would have been conveyed to the ED? (Likely/Unlikely/Unsure).
Do you think that the patient would have subsequently been admitted to hospital? (Likely/Unlikely/Possibly).
Responses were analysed by clinical encounter against Hospital Episode Statistics length-of-stay data and NHS reference costs to allow for an estimation of reimbursable activity in a ‘no-PRU’ model (i.e as if PRU were not dispatched to any of the patients) compared with the study population attended by the PRU. This enabled an assessment of sector-wide cost-impact associated with the reduction in activity for the ambulance service, ED and inpatient wards. In order to reduce the risk of overestimation due to subjective opinion, all answers given as ‘unsure’ (Q.1) or ‘possibly’ (Q.2) were counted as ‘unlikely’ in order to achieve a conservative binary dataset.
The PRU is funded separately from LAS and so is not a core ambulance service resource, such that when the PRU is tasked to a patient as a solo response, it can be considered to have made one standard LAS resource available for another emergency response.
Results
Dispatch data
In 12 months from September 2017 to September 2018, the PRU attended 1924 patients, averaging 5.3 patients per day (range 1–9). Of the 1924 calls attended by the PRU, 1366 (71.0%) were as a primary resource. A total of 558 (29.0%) consultations were crew requests for assistance from other ambulance resources. Overall, 335 (17.4%) were highest priority calls (R1, R2, C1), requiring an 8 min response time. In 1092 cases (56.8%), the PRU was the only service dispatched, reducing ambulance activity by a mean of 3.0 resources per day. Of note, an unknown number of patients may have required more than one additional resource, such as a first responder in addition to an ambulance. The median length of patient contact time was 01.
Patient data
Of the 1924 patients seen during the study period, 1056 (55%) were females (table 2). Median age was 49 (range 0–104), with a bimodal peak in age distributions between 20–29 (16.7%) and 80–89 (13.8%). Six hundred and forty patients (33.2%) underwent diagnostic tests not normally available with regular ambulance service resources.
Table 2.
Patient and study demographics
| All patients (n=1924) | Conveyed (n=597) | Non-conveyed patients (n=1289) | Death in community (n=38) | ||||
| Likelihood of conveyance | Likelihood of hospital admission | ||||||
| Likely (n = 945) | Unsure/unlikely (n=344) | Likely (n=126) | Possibly/Unlikely (n= 1163) | ||||
| Sex n (%) | Male 868 (45.1) Female 1056 (54.9) |
Male 295 (49.4) Female 302 (50.6) |
Male 401 (42.4) Female 544 (57.6) |
Male 151 (43.9) Female 193 (56.1) |
Male 48 (38.1) Female 78 (61.9) |
Male 504 (43.3) Female 659 (66.7) |
Male 21 (55.3) Female 17 (44.7) |
| Median age (range) | 49 (0–104) | 52 (0–97) | 47 (0–104) | 44 (4–96) | 79 (20–84) | 43 (0–102) | 67 (18–95) |
| Paediatric patients (<18 years) n (%) | 177 (9.2) | 63 (10.6) | 92 (9.7) | 22 (6.4) | 0 (0) | 114 (9.8) | 0 (0) |
| Priority of calls n (%) |
Pre-ARP* (n=320) R1: 19 (5.9) R2: 110 (34.4) C1: 50 (15.6) C2: 109 (34.1) C3: 23 (7.2) C4: 9 (2.8) Post-ARP† (n=1604) Category 1: 156 (9.7) Category 2: 633 (39.5) Category 3: 750 (46.8) Category 4: 65 (4.0) |
Pre-ARP (n=95) R1: 4 (4.2) R2: 40 (42.1) C1: 19 (20.0) C2: 28 (29.5) C3: 1 (1.1) C4: 3 (3.1) Post-ARP† (n=502) Category 1: 85 (16.9) Category 2: 201 (40.1) Category 3: 204 (40.6) Category 4: 12 (2.4) |
Pre-ARP (n=129) R1: 4 (3.1) R2: 42 (32.6) C1: 21 (16.3) C2: 49 (38.0) C3: 9 (6.9) C4: 4 (3.1) Post-ARP† (n=816) Category 1: 34 (4.2) Category 2: 337 (41.3) Category 3: 408 (50.0) Category 4: 37 (4.5) |
Pre-ARP (n=89) R1: 4 (4.4) R2: 28 (31.6) C1: 10 (11.2) C2: 32 (36.0) C3: 13 (14.6) C4: 2 (2.2) Post-ARP† (n=255) Category 1: 6 (2.4) Category 2: 95 (37.3) Category 3: 138 (54.1) Category 4: 16 (6.3) |
Pre-ARP (n=25) R1: 2 (8.0) R2: 10 (40.0) C1: 5 (20.0) C2: 4 (16.0) C3: 3 (12.0) C4: 1 (4.0) Post-ARP† (n=101) Category 1: 5 (4.9) Category 2: 50 (49.6) Category 3: 40 (39.6) Category 4: 6 (5.9) |
Pre-ARP (n=193) R1: 6 (3.1) R2: 60 (31.1) C1: 26 (13.5) C2: 77 (39.9) C3: 19 (9.8) C4: 5 (2.6) Post-ARP† (n=970) Category 1: 35 (3.6) Category 2: 382 (39.4) Category 3: 506 (52.2) Category 4: 47 (4.8) |
Pre-ARP (n=7) R1: 7 (100) Post-ARP† (n=31) Category 1: 31 (100) |
| Method of dispatch n (%) | Primary dispatch: 1366 (71.0) Crew request: 558 (29.0) |
Primary dispatch: 475 (79.6) Crew request :122 (20.4) |
Primary dispatch: 604 (63.9) Crew request: 340 (36.1) |
Primary dispatch: 269 (78.2) Crew request: 76 (21.8) |
Primary dispatch: 49 (38.9) Crew request: 76 (61.1) |
Primary dispatch: 822 (70.7) Crew request: 340 (29.3) |
Primary dispatch: 28 (73.7) Crew request: 10 (26.3) |
| Median length of consultation (HH:MM) (range) | 01:11 (0:13–03:54) | 01:20 (0:14–3:54) | 01:10 (0:23–3:36) | 0:55 (0:13–2:32) | 01:35 (0:33–3:34) | 01:04 (0:13–02:37) | 01:29 (0:20–3:02) |
| Diagnostics not available to regular LAS resources n (%) | No of patients: 655 (34.0) POC bloods : 412 (21.4) POC VBG/ABG 357 (18.6) Urinalysis: 387 (20.1) UPT: 149 (7.7) |
No of patients: 179 (30.0) POC bloods : 130 (21.8) POC VBG/ABG 137 (22.9) Urinalysis: 69 (11.6) UPT: 22 (3.7) |
No of patients: 386 (40.8) POC bloods : 247 (26.1) POC VBG/ABG 196 (20.7) Urinalysis: 247 (26.1) UPT: 100 (10.6) |
No of patients: 81 (23.5) POC bloods : 26 (7.6) POC VBG/ABG 16 (4.7) Urinalysis: 71 (20.6) UPT: 27 (7.8) |
No of patients: 82 (65.1) POC bloods : 76 (60.3) POC VBG/ABG 60 (47.6) Urinalysis: 34 (27.0) UPT: 2 (1.59) |
No of patients: 385 (33.1) POC bloods : 197 (16.9) POC VBG/ABG 152 (13.1) Urinalysis: 284 (24.4) UPT: 125 (10.7) |
N/A |
| Diagnosis frequency | Most encountered
|
Most commonly conveyed§
|
Most likely to have been otherwise conveyed§
|
Unsure/unlikely to have been conveyed§
|
Most likely to have otherwise been admitted§
|
Possibly/unlikely to have been otherwise admitted§
|
N/A |
| Interventions performed on scene (non-exhaustive) n (%) |
Medications
Analgesia: 484 (25.2) Antibiotics: 169 (8.8) Other medications: 390 (20.3) Oxygen :17 (0.9) Intravenous fluids: 137 (7.1) Critical care interventions Cardiac arrest management: 58 (3.0) Airway support: 11 (0.57) RSI/intubation: 21 (1.1) Sedation: 9 (0.47) Trauma interventions Immobilisation/splinting: 11 (0.57) Fracture/dislocation management :45 (2.33) Wound closure/care: 126 (6.5) Other medical care Catheter care: 30 (1.6) Epistaxis management: 6 (0.3) Other Ongoing care facilitation: 37 (1.9) Non-clinical intervention: 15 (0.8) Advice/reassurance alone: 269 (14.0) No intervention/none documented: 423 (22.0) |
Medications
Analgesia: 152 (25.4) Antibiotics: 44 (7.4) Other medications: 130 (21.8) Oxygen: 5 (0.8) Intravenous fluids: 44 (7.4) Critical care interventions Cardiac arrest management: 28 (4.7) Airway support: 1 (0.2) RSI/intubation: 7 (1.2) Sedation: 2 (0.4) Trauma interventions Immobilisation/splinting: 3 (0.5) Fracture/dislocation management: 16 (2.7) Wound closure/care: 44 (7.4) Other medical care Catheter care: 14 (2.3) Epistaxis management: 3 (0.5) Other Ongoing care facilitation: 7 (1.2) Non-clinical intervention: 6 (1.0) Advice/reassurance alone: 98 (16.4) No intervention/none documented: 168 (28.1) |
Medications
Analgesia: 240 (25.4) Antibiotics: 93 (1.0) Other medications: 198 (21.0) Oxygen: 10 (1.1) Intravenous fluids : 63 (6.7) Critical care interventions Cardiac arrest management: 0 (0) Airway support: 1 (0.1) RSI/intubation: 0 (0) Sedation: 6 (0.6) Trauma interventions Immobilisation/splinting: 8 (0.8) Fracture/dislocation management: 24 (2.5) Wound closure/care: 56 (5.9) Other medical care Catheter care: 14 (1.5) Epistaxis management: 3 (0.3) Other Ongoing care facilitation: 21 (2.2) Non-clinical intervention: 9 (1.0) Advice/reassurance alone: 127 (13.4) No intervention/none documented: 159 (16.8) |
Medications
Analgesia: 92 (26.7) Antibiotics: 32 (9.3) Other medications: 62 (18.0) Oxygen: 2 (0.6) Intravenous fluids: 30 (8.7) Critical care interventions Cardiac arrest management: 0 (0) Airway support: 1 (0.3) RSI/intubation: 0 (0) Sedation: 1 (0.3) Trauma interventions Immobilisation/splinting: 0 (0) Fracture/dislocation management: 5 (1.5) Wound closure/care: 26 (7.6) Other medical care Catheter care: 2 (0.6) Epistaxis management: 0 (0) Other Ongoing care facilitation: 9 (2.6) Non-clinical intervention: 0 (0) Advice/reassurance alone: 44 (12.8) No intervention/none documented: 96 (27.9) |
Medications
Analgesia: 35 (27.8) Antibiotics: 7 (5.6) Other medications: 30 (23.8) Oxygen: 3 (2.4) Intravenous fluids: 10 (7.9) Critical care interventions Cardiac arrest management: 0 (0) Airway support: 0 (0) RSI/intubation: 0 (0) Sedation: 1 (0.8) Trauma interventions Immobilisation/splinting: 1 (0.8) Fracture/dislocation management: 2 (1.6) Wound closure/care: 7 (5.6) Other medical care Catheter care: 0 (0) Epistaxis management: 0 (0) Other Ongoing care facilitation: 1 (0.8) Non-clinical intervention: 3 (2.4) Advice/reassurance alone: 12 (9.6) No intervention/none documented: 28 (22.2) |
Medications
Analgesia: 297 (25.6) Antibiotics: 118 (10.1) Other medications: 230 (19.8) Oxygen: 9 (0.8) Intravenous fluids: 83 (7.1) Critical care interventions Cardiac arrest management: 0 (0) Airway support: 2 (0.2) RSI/intubation: 0 (0) Sedation: 6 (0.5) Trauma interventions Immobilisation/splinting: 7 (0.6) Fracture/dislocation management: 27 (2.3) Wound closure/care: 75 (6.4) Other medical care Catheter care: 16 (1.4) Epistaxis management: 3 (0.3) Other Ongoing care facilitation: 29 (2.5) Non-clinical intervention: 6 (0.5) Advice/reassurance alone: 159 (13.7) No intervention/none documented: 226 (19.3) |
Critical care interventions
Cardiac arrest management: 30 (78.9)‡ (including: 4: traumatic arrest) Airway support: 8 (21.0) RSI/intubation: 14 (36.8) Thoracostomies: 2 (5.3) |
*Pre-ARP categories of call included R1: immediately life-threatening, and R2: life-threatening, 8 min response time; C1, C2, C3: urgent care, 20–30 min response; C4: non-emergency, 4 hour response.
†Post-ARP categories of call: category 1: life-threatening, requiring 7 min response; category 2: emergency, 16 min response; category 3: urgent, 120 min response; category 4: less urgent requiring 180 min response. category 2–4 requires a conveying resource within timeframe.
‡NB Additional 8 arrests had no cardiac arrest management—PLE on scene.
§: values displayed are a % of overall diagnosis frequency)
ABG, arterial blood gas; POC, point of care; RSI, rapid sequence induction; TLOC, transient loss of consciousness; UPT, urine pregnant test; VBG, venous blood gas.
Clinical data in terms of the primary diagnosis assigned by the PRU treating team and treatment outcomes are depicted in figure 1. A further breakdown of the most commonly encountered diagnoses according to whether the patient was conveyed to an ED or left at home, taking into consideration the opinions of the treating clinical team as to the most likely outcomes had a standard ambulance resource been dispatched, is shown in table 2.
Figure 1.
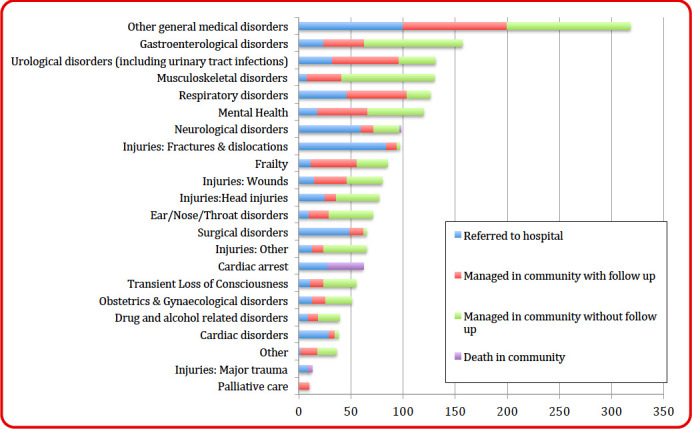
Primary diagnosis assigned by treating team with treatment outcomes.
Treatment outcome data
Treatments given are outlined in table 2. A total of 1289 patients (67.0%) patients were managed in the community, with 597 (31.0%) conveyed to hospital. Thirty-eight patients (2.0%) died on scene, with dispatch criteria given as cardiac arrest. In 30 of these patients, resuscitation attempts were unsuccessful. In eight cases, resuscitation was not attempted as patients were considered to be unsalvageable.
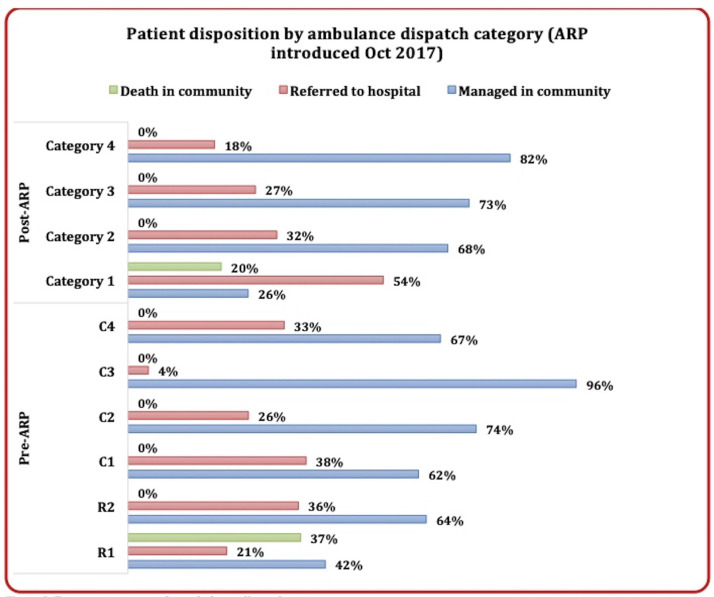
Figure 2 demonstrates outcomes by dispatch category. A quarter (25.8%) of patients categorised as requiring immediate assistance (category 1) were managed in the community. All deaths occurred in category 1 patients. Of those conveyed to hospital, 75% were transported by LAS ambulance, and 19% were taken to the ED in the PRU vehicle. Patients transported in the PRU vehicle were those that were considered to be safe and stable to do so, that is, did not require monitoring or ongoing medical interventions during transport.
Figure 2.
Treatment outcomes by ambulance dispatch category.
Of the 1289 patients who were managed in the community, follow-up was arranged in 561 (43.5%) (table 3). The attending PRU team estimated that of those managed in the community, 945 (73%) were likely to have been taken to hospital by a standard LAS resource. Of these, an estimated 126 (13%) were considered likely to have subsequently been admitted to hospital.
Table 3.
Disposition data and team opinion regarding likely standard care pathway and cost impact data
| Activity | Number | % | |
| Total patients seen by PRU | 1924 | 100 | |
| Managed in community | 1289 | 67.0 | |
| Referred to hospital | 597 | 31.0 | |
| Death at scene | 38 | 2.0 | |
| Patients who were managed in community | 1289 | 100 | |
| Managed in community with follow-up | 561 | 43.5 | |
| Managed in community without follow-up | 728 | 56.5 | |
| Communication with general practitioner | 245 | 19.0 | |
| Patients who were referred to hospital | 597 | 100 | |
| Referral direct to specialist team | 169 | 28.3 | |
| Conveyance by PRU | 115 | 19.3 | |
| Conveyance by LAS | 424 | 71.0 | |
| Unspecified conveyance (incl patient’s own) | 58 | 9.7 | |
| Likelihood of conveyance if PRU had not been dispatched | 1289 | 100 | |
| Likely | 945 | 73.3 | |
| Unsure | 140 | 10.9 | |
| Unlikely | 204 | 15.8 | |
| Likelihood of admission if had otherwise been conveyed | 1289 | 100 | |
| Likely | 126 | 9.8 | |
| Possibly | 179 | 13.9 | |
| Unlikely | 984 | 76.3 | |
| Cost of PRU activity | Unit cost (£) | Number | Total cost (£) |
| Reduction in LAS activity | |||
| Presumed LAS activity with a no PRU model | |||
| See and treat or refer | £192 | 369 | £70 848 |
| See, treat and convey | £252 | 1555 | £391 860 |
| Total cost | 1924 | £462 708 | |
| Cost of LAS involvement in current PRU model | |||
| See, treat and refer (i.e crew request) | £192 | 393 | £75 456 |
| See, treat and convey | £252 | 459 | £115 668 |
| Total cost | 852 | £191 124 | |
| Net benefit of PRU model versus no PRU model | £271 584 (a) | ||
| Reduction in hospital activity | |||
| ED attendances (patients deemed likely to have been otherwise conveyed to ED) | £160 | 945 | £151 200 |
| Nightly cost local non-elective inpatient bed (source: Barts Health NHS Trust Business Intelligence Unit) | £550 | 126 patients (868 bed days) |
£477 400 |
| Net benefit of PRU model to acute trusts versus no PRU model | £628 600 (b) | ||
| PRU operational costs | |||
| WTE PRU fellow posts (registrar) | £39 250 | 5×0.5 WTE | £196 250 |
| Consultant sessions (PAs) | £12 000 | 6 | £72 000 |
| LAS staffing enhancement | – | – | £60 000 |
| Non-recurrent costs (equipment, IT, expendables) | – | – | £10 000 |
| Rapid response vehicle lease | £16 160 | 1 | £16 160 |
| Managerial support | – | – | £15 667 |
| Total operational costs of PRU | £370 077 (c) | ||
| Overall net benefit ((a+b)–c) | £530 107 | ||
Expressed as n (%) unless otherwise stated.
IT, information technology; PA, programmed activities; PRU, Physician Response Unit; WTE, whole time equivalent.
Cost impact data
Cost impact data are detailed in table 3. In the study period, the operational cost of the PRU was £370 077. An estimation of total episode activity was calculated for standard care (no PRU) and PRU models. For ambulance activity within a standard care model, it was estimated that 369/1924 patients would have been seen and treated by LAS, whereas 1555 patients would have been conveyed to ED. This total activity cost is ~£462 708. In the PRU model, 852 patients also received a LAS resource, of which 393 were seen and treated, and 459 were conveyed to ED, costing £191 124. Therefore, the reduction in ambulance activity was ~£271 584.
For ED activity, there was an estimated reduction of 945 attendances, representing a cost of ~£151 200. For inpatient activity, there were 126 patients (mean age 75.5 years) for whom an admission would likely have occurred, with total expected bed occupancy of 868 days, costing ~£477 400.
Combining the above data, the PRU is estimated to have made a contribution to reducing system-wide activity that would cost ~£900 184. Offsetting the operational cost, this represents a net efficiency of ~£530 107.
Patient experience data
Patient experience data are displayed in table 4. A total of 84 responses were received from September 2017 to April 2018. 98.1% of 52 patients were extremely likely to recommend the service. Earlier data showed that the PRU ranked highly compared with other Barts Health services, with a mean score of 4.97 and 4.92 out of 5 for the months of September and October 2017, respectively.
Table 4.
Patient experience data
| Friends and family test | |
| How likely would you be to recommend this service to friends and family? (December 2017 to April 2018) (n=52) Extremely likely 98.1% Likely 1.9% | |
| I Want Great Care | |
|
September 2017 (n=13) Rank out of 219 services: 10th Mean score: 4.97/5 Dignity/respect: 5/5 Involvement: 4.92/5 Information: 5/5 Staff: 5/5 |
October 2017 (n=19) Rank out of 252 services: 24th Mean score: 4.92/5 Dignity/respect: 5/5 Involvement: 4.89/5 Information: 4.84/5 Staff: 5/5 |
Discussion
Our data demonstrate that of 1924 patients seen over the 365-day period, 67.0% were managed within the community. Utilisation of additional community services occurred in 43.5% of those patients. A net cost saving of £530 107 is estimated, but costs of delivery of follow-up pathways used have not been calculated, limiting the accuracy of overall cost calculations. However, the proposed benefits of the PRU model reach beyond empirical data. The PRU delivers a senior doctor to the patient, allowing for earlier diagnostic and definitive therapeutic interventions not normally available with standard ambulance resources. It is widely considered that the key intervention is this delivery of a senior clinical decision-maker into the out-of-hospital consulting environment. They are empowered by situation-specific information which aids more patient-focused decision-making than the generic clinical approach in the ED might allow. It has previously been demonstrated that early senior review of patients presenting to an ED can prevent unnecessary hospital admissions and improve streamlining of care to appropriate outpatient facilities.11 Access to community pathways is less embedded in the behaviours of emergency doctors when working within our ED than when working on the PRU, and we identify a clear learning opportunity for the ED to shift towards a more community-oriented model of care. In addition, the training and experiential learning of a secondment on the PRU may allow ambulance service clinicians to develop more autonomous skills and practice.
Collated patient feedback reported high levels of satisfaction which may be unsurprising given patient expectation of conveyance to hospital, prolonged ED waiting times and consultation with a more junior EM clinician.
Feasibility data relating to the PRU in its original format was published in 2006.6 The majority of calls attended at that time were categorised as life-threatening, requiring an 8 minute response. Subsequently, their non-conveyance rate was 18.2%. Interestingly, the PRU now demonstrates a higher non-conveyance of highest category calls (26% for category 1). Potential reasons include natural variation in case mix, which may be a reflection of the risk management mechanisms within the ambulance triage system, but also may follow from the service being delivered by emergency physicians who are more familiar with local healthcare infrastructure, and are supported in their decision-making by point-of-care IT, diagnostics and access to community follow-up.
The activity data and disposition outcomes of the PRU demonstrate that many patients seeking emergency care via ambulance can be managed outside of the ED. This may also be indicative of patient’s perceptions of their emergency need and a trend towards a ‘need-it-now’ society, but also of the difficulty some report in navigating access to local primary healthcare systems. The public has been signposted to seek medical help for a number of symptoms such as chest pain or weakness suggestive of stroke.12 Specific factors are also associated with higher ambulance service usage such as being of an ethnic minority, having a lower income, increasing age, influence from caregivers and accessibility of primary care.13 These elements are particularly evident in inner city London, and likely play a part in the dynamic shift of how both LAS and London EDs are utilised. The primary care sector is also seeing increasing demand for its’ services against limited capacity, manifesting as longer waiting times, an increasing trend in telephone consultations, fewer patients having named GPs and home visits being less common than previously.14 These factors have contributed to rising demand across the emergency sector.15
The ‘NHS Long Term Plan’16 outlines how the NHS should evolve in the face of growing concern regarding funding, staff shortages, increasing equalities and an ageing population. This includes an increase in emergency treatment in a community-based setting, with aims such as advanced practitioners working with ambulance services to help reduce pressure on hospital services. Services such as the PRU fulfil this remit. Evidence suggests that extended paramedic schemes, treating people with minor acute illnesses, are as safe as conveyance and standard ED treatment.17 However, the PRU sees large numbers of clinically complex patients, and therefore the authors feel that it is the delivery of a senior emergency doctor to a patient’s home, armed with additional diagnostics, access to hospital records and links with various community-based acute care services which allow for the treatment of patients who would otherwise require ED attendance and potential admission.
There are several similar units such as the Welsh PRU, whose 2016 data demonstrated a non-conveyance rate of 58%, with direct referrals to hospital specialists further reducing ED conveyances.18 19 Other services operating within the UK include the Oxford-based Emergency Care Response Unit20 and a prehospital medical response unit in Ireland which reports a non-conveyance rate of 31%.21
Our data suggest an expanded model could aid in reducing overcrowding in the ED, and illustrate that alternative care can be delivered effectively outside of the standard emergency pathway. Comparing non-conveyance rates by the PRU to 2015–2016 data for ambulance trusts across England, which states a mean non-conveyance rate of 38% (range 23%–51%), the PRU is able to manage almost double the number of patients in the community.22 Non-conveyance of suitable patients by the PRU has also reduced their potential for over-investigation and a prolonged ED encounter. The mean patient encounter length with the PRU was 77 min, significantly shorter than a standard ED encounter.23 There are clinical benefits with regards to non-conveyance of the elderly and infirm, especially those with dementia, where a hospital episode increases the incidence of disorientation, falls, nosocomial infections and deconditioning.24
Prevention of avoidable attendance and admission to hospital brings significant psychosocial benefits to patients as well as health economic benefits to systems.25 26 The provision of holistic patient-centred care is closely correlated with overall patient satisfaction; this is particularly the case with provision of emotional support.26–28 These key elements are of particular focus during patient consultation with the PRU, where the benefit of seeing one patient at a time outside of the constraints of an ED clinical environment allows delivery of high-quality care, and high levels of patient and staff satisfaction. It could be argued that as challenges to recruitment into emergency medicine continue, emergency physicians are required more than ever on the ‘shop floor’.29 However, attractive fellowship opportunities such as these may aid recruitment and retention to the specialty and help the development of community emergency medicine and associated benefits.
Study limitations
The major limitation of this study is the inherent bias introduced in the analysis of estimated activity savings and associated costs. Our data are subjective and limited to the opinions of the duty team relating to their perceived alternative outcomes had the PRU not attended the patient. We recognise the methodological shortcomings of this approach and that the evaluation method used has not undergone validation. We have therefore endeavoured to apply conservative interpretations of the collated data, using only the cases deemed likely to have been conveyed or admitted to count towards potential cost savings generated. All episodes where the team answered unsure or possibly were not counted towards potential service impact data, which has likely led to an underestimation of true impact. A full-scale cost analysis will be undertaken using independent case review in the future in order to accurately quantify this data; however, we believe the message this manuscript delivers in terms of system-wide benefits is integral to the service description.
An additional limitation of this study is the lack of available recontact data. This information is difficult to collate given the various avenues with which a patient could make further contact with an NHS resource, and is further confounded by the density of hospitals located within close proximity to one another. Data obtained through the LAS indicates that only 5/1288 (0.4%) patients seen by the PRU and managed in the community recontacted the LAS within 24 hours; however, this is likely to be an underestimation of overall recontact rates. A multiagency collaboration is required in order to fully capture these data, or moving forward, obtaining consent for further contact with each patient to identify final treatment outcomes and recontact rates. We aim to address this with future research.
Conclusion
The PRU is a model of integration and collaboration, delivering patient-centred emergency care with favourable health economic impact. The service has produced a reduction in ambulance conveyances and ED attendances, helping to reduce risk of over-investigation and avoid unnecessary patient encounters in the ED. It has generated cost savings and a reduction in inpatient bed days, which impacts on hospital overcrowding and exit block. Moreover, it has highlighted that emergency care can be delivered in alternative ways through provision of a senior clinical decision-maker and enhanced clinical capabilities including a directory of accessible community providers. We believe the operating model has the potential to provide significant benefits to patients, staff and the wider urgent and emergency healthcare infrastructure. There is ample opportunity for further research in this area.
Acknowledgments
Special thanks to Mr Bill Leaning who although not directly involved with this submission has been integral to the service development of the Physician Response Unit.
Footnotes
Twitter: @tonyjoy81, @LisaRamage, @smitchinson1, @_Oliver_Kirby, @GreenhalghRob
Contributors: TJ: concept and design, acquisition of data, data analysis and interpretation, manuscript draft, revision and approval. LR: concept and design, data analysis and interpretation, manuscript draft, revision and approval. SM: data analysis and interpretation, manuscript revision and approval. OK: concept, manuscript draft and approval. RG: manuscript revision and approval. GD and DG: concept, manuscript revision and approval.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request.
Press release: No.
References
- 1. Maguire D, Dunn P, Mckenna H. How hospital activity in the NHS in England has changed over time. The King’s Fund, 2016. Available: www.kingsfund.org.uk/publications/hospital-activity-funding-changes [Accessed Nov 2018].
- 2. NHS England A&E Attendances and Emergency Admissions March 2018 Statistical Commentary, 2018. Available: www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-and-activity/ae-attendances-and-emergency-admissions-2017-18/ [Accessed Nov 2018].
- 3. UEC Review Team and ECIST Transforming Urgent & Emergency Care Services in England. NHS England, 2015. Aug Available: www.england.nhs.uk/wp-content/uploads/2015/06/trans-uec.pdf [Accessed Nov 2018].
- 4. Lecky F, Mason S, Benger J, et al. Framework for quality and safety in the emergency department. International Federation for emergency medicine, 2012. Available: www.ifem.cc/wp-content/uploads/2016/03/Framework-for-Quality-and-Safety-in-the-Emergency-Department-2012.doc.pdf [Accessed Nov 2018]. [DOI] [PubMed]
- 5. National Health Service Five year forward view, 2014. Available: www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf [Accessed Nov 2018].
- 6. Bell A, Lockey D, Coats T, et al. Physician response unit -- a feasibility study of an initiative to enhance the delivery of pre-hospital emergency medical care. Resuscitation 2006;69:389–93. 10.1016/j.resuscitation.2005.10.013 [DOI] [PubMed] [Google Scholar]
- 7. Department of Health Reforming emergency care, 2001. Available: https://webarchive.nationalarchives.gov.uk/20120106112528/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4058836.pdf [Accessed Nov 2018].
- 8. Knottnerus A, Tugwell P. STROBE--a checklist to strengthen the reporting of observational studies in epidemiology. J Clin Epidemiol 2008;61:323 10.1016/j.jclinepi.2007.11.006 [DOI] [PubMed] [Google Scholar]
- 9. NHS England Ambulance response programme review, 2018. Available: www.england.nhs.uk/publication/the-ambulance-response-programme-review/ [Accessed Nov 2018].
- 10. Department of Health Nhs reference costs 2017-18, 2016. Available: https://improvement.nhs.uk/documents/1972/1_-_Reference_costs_201718.pdf [Accessed April 2019].
- 11. White AL, Armstrong PAR, Thakore S. Impact of senior clinical review on patient disposition from the emergency department. Emerg Med J 2010;27:262–5. 10.1136/emj.2009.077842 [DOI] [PubMed] [Google Scholar]
- 12. Dombrowski SU, Mackintosh JE, Sniehotta FF, et al. The impact of the UK ‘Act FAST’ stroke awareness campaign: content analysis of patients, witness and primary care clinicians’ perceptions. BMC Public Health 2013;13:915 10.1186/1471-2458-13-915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Booker MJ, Shaw ARG, Purdy S. Why do patients with 'primary care sensitive' problems access ambulance services? A systematic mapping review of the literature. BMJ Open 2015;5:e007726 10.1136/bmjopen-2015-007726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Baird B, Charles A, Honeyman M, et al. Understanding pressures in general practice. The kings fund, 2016. Available: www.kingsfund.org.uk/publications/pressures-in-general-practice [Accessed Nov 2018].
- 15. Department of Health Tackling demand together: a toolkit for improving urgent and emergency care pathways by understanding increases in 999 demand, 2009. Available: https://webarchive.nationalarchives.gov.uk/20130123200641/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_106925 [Accessed Nov 2018].
- 16. National Health Service NHS long term plan, 2019. Available: https://www.longtermplan.nhs.uk/online-version/overview-and-summary/ [Accessed Apr 2019].
- 17. Mason S, Knowles E, Freeman J, et al. Safety of paramedics with extended skills. Acad Emerg Med 2008;15:607–12. 10.1111/j.1553-2712.2008.00156.x [DOI] [PubMed] [Google Scholar]
- 18. Rutherford A. Groundbreaking team helps cut ambulance journeys to Gwent A&E. South Wales Argus, 2015. [Google Scholar]
- 19. Rogerson T. 2016 finalist - Aneurin Bevan UHB and Welsh Ambulance Service Trust (WAST) for a service provided by Aneurin Bevan UHB & WAST to put Emergency Department consultants on the road to see and treat patients before hospital, 2016. [Google Scholar]
- 20. Holbrook EN-C. Enhanced care response unit: prehospital experience for all trainees. Emergency Medicine Journal Supplement 2014. [Google Scholar]
- 21. Deasy C, Ryan D, O'Donnell C, et al. The impact of a pre-hospital medical response unit on patient care and emergency department attendances. Ir Med J 2008;101:44–6. [PubMed] [Google Scholar]
- 22. O’Cathain A, Knowles E, Bishop-Edwards L. Understanding variation in ambulance service non-conveyance rates: a mixed methods study. Southampton (UK: NIHR Journal Library; Health Services and Delivery Research, 2018. [PubMed] [Google Scholar]
- 23. NHS England Hospital accident and emergency activity, 2016-17. Available: https://digital.nhs.uk/data-and-information/publications/statistical/hospital-accident-emergency-activity/2016-17 [Accessed Nov 2018].
- 24. Inouye SK. Delirium in older persons. N Engl J Med 2006;354:1157–65. 10.1056/NEJMra052321 [DOI] [PubMed] [Google Scholar]
- 25. Shepperd S, Doll H, Angus RM, et al. Avoiding hospital admission through provision of hospital care at home: a systematic review and meta-analysis of individual patient data. CMAJ 2009;180:175–82. 10.1503/cmaj.081491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Shepperd S, Iliffe S, Doll HA, et al. Admission avoidance Hospital at home. Cochrane Database Syst Rev 2016;9:CD007491 10.1002/14651858.CD007491.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ellis S. The patient-centred care model: holistic/multiprofessional/reflective. Br J Nurs 1999;8:296–301. 10.12968/bjon.1999.8.5.6677 [DOI] [PubMed] [Google Scholar]
- 28. Rathert C, Williams ES, McCaughey D, et al. Patient perceptions of patient-centred care: empirical test of a theoretical model. Health Expect 2015;18:199–209. 10.1111/hex.12020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Health Education England, NHS England, NHS Improvement, Royal College of Emergency Medicine Securing the future workforce for emergency departments in England, 2017. Available: https://improvement.nhs.uk/documents/1826/Emergency_department_workforce_plan_-_111017_Final.3.pdf