Abstract
Non-alcoholic steatohepatitis (NASH) is becoming a leading cause of cirrhosis with the burden of NASH-related complications projected to increase massively over the coming years. Several molecules with different mechanisms of action are currently in development to treat NASH, although reported efficacy to date has been limited. Given the complexity of the pathophysiology of NASH, it will take the engagement of several targets and pathways to improve the results of pharmacological intervention, which provides a rationale for combination therapies in the treatment of NASH. As the field is moving towards combination therapy, this article reviews the rationale for such combination therapies to treat NASH based on the current therapeutic landscape as well as the advantages and limitations of this approach.
Keywords: nonalcoholic steatohepatitis, hepatobiliary disease, liver
Introduction
In the context of therapies for liver diseases, the treatment of non-alcoholic steatohepatitis (NASH) represents a major unmet need. Therefore, treatment of NASH is a major focus of drug development worldwide. Currently, there are no Food and Drug Administration (FDA)-approved or European Medicines Agency (EMA)-approved therapies for NASH. As of December 2019, 84 interventional studies were ongoing and had enrolled patients to evaluate the therapeutic efficacy of treatments for NASH (www.clinicaltrial.gov). Most of these trials are testing new drugs as monotherapy with some trials investigating combination therapy for the treatment of NASH.
It is now well accepted that fibrosis stage is a major predictor of liver-related morbidity and mortality. FDA and EMA guidance documents indicate that for clinical approval of new drugs for the treatment of NASH, trials should include patients who have significantly higher risk of progression to cirrhosis and hepatic decompensation, as defined as those who have biopsy-proven NASH with stage 2 fibrosis or higher. The regulatory approval pathway for pharmacological therapies for NASH requires therapies to show clinical benefit in improving liver-related outcomes for full regulatory approval, which may take several years due to low event rates. To expedite drug development, liver histological improvements have been accepted as a surrogate for clinical improvements for a subpart H approval process. The subpart H approval endpoints include either one-stage improvement in liver fibrosis or resolution of NASH. This approval is contingent on showing clinical benefits over long-term follow-up for full approval.
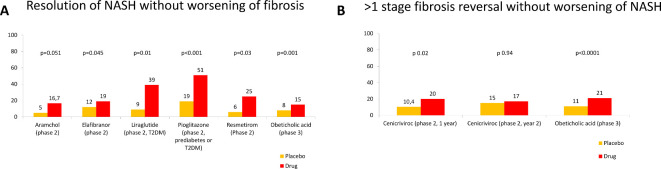
Several therapies have been investigated for the treatment of NASH-related fibrosis using liver histology improvement as an endpoint. It has been observed that the difference in treatment effect relative to placebo has been relatively small. The percentage of patients with histological resolution of NASH in completed trials of a drug as monotherapy does not exceed 32% over placebo and this holds true across drugs with different mechanisms of action (figure 1). This underlies the complexity of the pathophysiology of NASH, which is driven by a metabolic overload that places stress on hepatocytes, leading to cell damage, inflammation and fibrosis. Metabolic overload impacts not only the liver, but also adipose tissue, the endocrine pancreas, the immune system and the gut. This complex pathogenesis explains why several classes of drug are in development for the treatment of NASH, although one therapeutic target is unlikely to be sufficient when treating patients with NASH. As the success of drugs as monotherapy appears limited, combination of agents might seem a logical approach to increase efficacy, with numerous combinations possible. Logical combinations might see a drug with a metabolic mechanism of action combined with a drug with an anti-inflammatory or an antifibrotic mechanism of action. Some combinations might be selected based on specific patient characteristics, whereby patients are identified as potential responders to a combination. Except for patients with type 2 diabetes mellitus (T2DM), specific NASH subpopulations have not yet been well enough defined to become a selection or a stratification criterion in clinical trials precluding prespecified comparisons. The field investigating the role of combination therapy in the treatment of NASH is moving at a fast pace. In the current review, we discuss the rationale for such combination therapies to treat NASH based on the current therapeutic landscape as well as the advantages and limitations of this approach.
Figure 1.
(A) Percentage of patients with resolution of non-alcoholic steatohepatitis (NASH) defined as ballooning 0 and inflammation 0–1, without worsening fibrosis in placebo and intervention arms of randomised clinical trials showing an effect. (B) Percentage of patients with more than one-stage improvement in fibrosis without worsening of NASH in placebo and intervention arms of randomised clinical trials showing an effect. The references are provided in the text, the data for the obeticholic acid phase 3 are based on study by Sanyal et al. 2
Drug classes suitable for combination therapy
FXR agonists
Farnesoid X receptor (FXR) is a transcription factor activated by bile acids. As such FXR regulates bile-acid metabolism, but since bile-acid biology is paced by food intake, FXR also controls hepatic metabolism. Drugs-activating FXR have demonstrated effects in cholestatic liver disease and are in advanced clinical development for NASH. In phase 2 clinical trials, FXR agonists have shown an improvement of hepatic histology. The front runner—obeticholic acid, which is a bile-acid derivative—has shown efficacy on liver fibrosis and significantly more patients receiving obeticholic acid 25 mg daily had resolution of NASH without worsening of fibrosis at 18 months when patients with F1 fibrosis were also included in the analysis in an interim analysis of a phase 3 trial (NCT02548351).1 2 In the FLIGHT.-FXR phase 2 study, tropifexor showed a decrease in steatosis, and a reduction in alanine aminotransferase (ALT) and gamma glutamyl transferase (GGT) circulating levels (NCT02855164).3 Major adverse effects related to FXR agonists include pruritus and increased low‐density lipoprotein (LDL) cholesterol, both of which are dose dependent, and decreased high-density lipoprotein cholesterol. LDL cholesterol increase may be managed by cotreatment with a statin. Regarding glucose metabolism, obeticholic acid has been reported in the phase 2 trial to increase circulating levels of insulin without affecting the glycaemia resulting in a significant increase in homoeostasis model assessment-estimated insulin resistance.4 Other FXR agonists that are being investigated include cilofexor (NCT03449446), EDP-305 (NCT03421431), EYP 001 (NCT03812029) and nidufexor (NCT02913105). Currently, there are no predictive biomarkers of response to an FXR agonist in patients with NASH and the response rate has been reported to be less than 25%. This provides a clear case for combining an FXR agonist with another drug to obtain a more robust response. Since stimulating FXR has pleotropic effects, such as improving steatosis, hepatic inflammation and fibrosis, an FXR agonist could be combined with different types of drugs. As the most advanced FXR agonist, obeticholic acid, has mostly demonstrated antifibrotic effects, it seems that this FXR agonist might benefit from combination with a second drug that has a metabolic mechanism of action, particularly one with a beneficial effect on lipoprotein metabolism. Indeed, several FXR agonists including tropifexor, cilofexor and obeticholic acid are currently being investigated in such a combination therapy (table 1).
Table 1.
Trials of combination therapies currently ongoing for the treatment of non-alcoholic steatohepatitis (NASH)
| Name/number | First drug | Second drug | Arms | Population | Duration, weeks | Endpoints | Secondary endpoints |
| CONTROL Phase 2 NCT02633956 |
Obeticholic acid | Atorvastatin | Placebo, 5, 10, 25 mg Obeticholic acid with atorvastatin 10, 20 mg | NASH F1–F3 F4 No decompensation |
16 | LDL cholesterol | Safety, tolerability, lipoproteins |
| TANDEM Phase 2 NCT03517540 |
Tropifexor | Cenicriviroc | Tropifexor dose 1 Cenicriviroc Tropifexor dose 1+cvc Tropifexor dose 2+cvc |
NASH F2/3 | 48 | AE | One-stage improvement in fibrosis Resolution of NASH |
| ELIVATE Phase 2 NCT04065841 |
Tropifexor | Licoglifozin | Tropifexor Licogliflozin Tropifexor +licogliflozin |
NASH F2/F3 | 48 | Resolution of NASH and no worsening of fibrosis OR improvement in fibrosis by at least one stage without worsening of NASH |
Improvement of fibrosis by two stages, reduction in body weight, change in liver fat content on MRI-PDFF, improvement of liver tests |
| Proof-of-concept study NCT02781584 |
Cilofexor | Firsocostat Selonsertib |
Selonsertib Firsocostat Cilofexor Cilo+Sel Sel+Firso Cilo+Firso Firso cirrhotics Cilo cirrhotics Cilo+Sel + Firso Firso+Feno 48 Firso +Feno145 |
NASH F2/3 some F4 | 12 | TEAEs TESAEs TELAs |
|
| ATLAS Phase 2 NCT03449446 |
Cilofexor | Firsocostat Selonsertib |
Sel+Firso + placebo Sel+Cilo + placebo Sel+placebo + placebo Firso +placebo + placebo Cilo+placebo + placebo 3 placebos Firso+Cilo + placebo |
NASH F3/4 | 48 | AEs TELA One-stage improvement in fibrosis without worsening NASH |
|
| Phase 2 NCT03987074 |
Cilofexor | Semaglutide Firsocostat |
Semaglutide Firso+Sema Sema+Cilo 30 Sema+Cilo 100 Sema+Firso + Cilo |
NASH F2/3 | 24 | TEAEs TESAEs TELA |
|
| Phase 2A NCT03776175 |
PF-05221304, ACC inhibitor | PF-06865571, DGAT2 Inhibitor |
PF-05221304 PF-06865571 Placebo PF-05221304 + PF-06865571 |
NAFLD | 6 | Steatosis (MRI-PDFF) | Safety, tolerability |
ACC, acetyl-CoA carboxylase; AEs, adverse events; Cilo, cilofexor; CVC, cenicriviroc; DGAT2, diacylglycerol acyltransferase 2; Firso, firsocostat; LDL, low-density lipoprotein; MRI-PDFF, MRI proton density fat fraction; NAFLD, non-alcoholic steatohepatitis; Sel, selonsertib; Sema, semaglutide; TEAEs, treatment-emergent adverse events; TELAs, treatment-emergent laboratory abnormalities; TESAEs, treatment-emergent serious adverse events.
Norursodeoxycholic acid, a bile acid derivative like many FXR agonists, but which is not an FXR agonist showed in a double-blind randomised, placebo-controlled phase 2 trial without histology a dose-dependent reduction in serum ALT (NCT03872921).5
PPAR agonists
Peroxisone proliferator-activated receptors (PPARs) comprise a family of three transcription factors—PPAR-α, PPAR-δ and PPAR-γ—which are involved in lipid and glucose metabolism, and have anti-inflammatory effects. Schematically, PPAR-α plays a key role in fatty acid metabolism including absorption, transport and β-oxidation, PPAR-δ inhibits inflammatory macrophage phenotypes contributing to its anti-inflammatory effects, regulates the β-oxidation of free fatty acids and improves glucose homeostasis, and PPAR-γ regulates fatty acid storage and adipogenesis and improves insulin sensitivity in adipose tissue, liver and skeletal muscle. The PPAR-γ agonist pioglitazone at the dose of 30 mg failed to demonstrate an improvement of NASH compared with placebo in the PIVENS trial (NCT00063622).6 However, at a dose of 45 mg, pioglitazone resolved NASH in a significantly greater proportion of patients with pre-diabetes or T2DM compared with placebo (51% vs 19%; NCT00994682).7 Pioglitazone’s favourable effect was confirmed in a recent meta-analysis.8 Although the American Association for the Study of Liver Diseases9 and European Association for the Study of Liver10 guidelines recommend pioglitazone for use in patients with biopsy-proven NASH, there are several side effects associated with this drug, including weight gain and fluid retention, and the increased risk of bone fracture, which limits its potential for combination with anti-NASH treatments. A second-generation PPAR-γ agonist designed to selectively modulate the entry of pyruvate into the mitochondria is currently being investigated in a phase 2b clinical trial (NCT02784444).
Several dual PPAR agonists are in clinical development with different agonistic profiles: elafibranor is a PPAR-α and PPAR-δ agonist, saroglitazar is a PPAR-α and PPAR-γ agonist, and lanifibranor is a pan-PPAR agonist. Based on positive findings from a phase 2 study (NCT01694849),11 elafibranor is currently in phase 3 development (NCT02704403). Saroglitazar improved liver biochemistries and hepatic steatosis in a phase 2 study (NCT03061721)12 and the results from the lanifibranor phase 2 trial (NCT03008070) are yet to be reported. The development of seladelpar, a PPAR-δ agonist, was halted due to unexpected findings in a NASH phase 2 trial (NCT03551522). Combination trials are being planned for PPAR agonists in NASH. As drugs with strong metabolic effects, it would be logical to combine PPARs with drugs with anti-inflammatory and antifibrotic properties.
Metabolic enzyme inhibitors
Steroyl-CoA desaturase-1 (SCD-1) converts saturated fatty acids to monounsaturated fatty acids. SCD-1 downregulation reduces hepatic lipogenesis, enhances insulin sensitivity and promotes lipid oxidation. Aramchol is a liver-targeted SCD-1 inhibitor that, in a 52-week, phase 2b, placebo-controlled, randomised trial, promoted NASH resolution and fibrosis-stage reduction with a favourable safety and tolerability profile (NCT02279524),13 and is currently being tested in the phase 3/4 ARMOR clinical trial (NCT04104321).
Acetyl-CoA carboxylase (ACC) converts acetyl-CoA to malonyl-CoA. Inhibition of ACC reduces hepatocellular malonyl-CoA levels, which in turn increases mitochondria beta-oxidation and decreases polyunsaturated fatty-acid synthesis; the net effect is improvement in hepatic steatosis. In a phase 2 trial of firsocostat, an ACC inhibitor, 126 patients with NASH treated at a dose of 20 mg daily for 12 weeks had a 29% relative reduction of liver fat (NCT02856555).14 PF-05221304, a liver-directed ACC inhibitor, is being investigated in a phase 2 trial to assess its pharmacodynamics, safety and tolerability over 16 weeks in patients with non-alcoholic fatty liver disease (NAFLD; NCT03248882).15
Diacylglycerol acyltransferase 2 (DGAT2) controls the final step in triglyceride synthesis. A DGAT2 inhibitor, PF-06865571, is in early clinical development and so there is currently limited published information on this drug.
Ketohexokinase (KHK) or hepatic fructokinase metabolises dietary fructose by phosphorylation to produce fructose-1-phosphate. PF-06835919 is a KHK inhibitor that has been shown to decrease steatosis in a phase 2 trial in patients with NAFLD (NCT03256526).16
Thyroid hormone receptor beta agonists
Selective thyroid hormone receptor beta (TRβ) agonist can modulate lipid metabolism without the side effects which are mediated by thyroid hormone receptor α. VK2809 and resmetirom are two TRβ agonists that are currently in clinical development. In phase 2 trials, both of these medications have been shown to effectively reduce liver fat content and LDL cholesterol (NCT02927184 and NCT02912260).17 18 The efficacy and safety of VK2809 are currently being investigated in patients with biopsy-proven NASH in the phase 2B VOYAGE clinical trial (NCT04173065). In a phase 2b trial, Harrison et al have recently demonstrated that resmetirom was significantly better than placebo in reducing liver fat content over 12 and 36 weeks. Furthermore, they also reported that NASH resolution rate was 27% and 6% in the resmetirom and placebo groups, respectively. Resmetirom is now being assessed in the large, phase 3 MAESTRO-NASH clinical trial to test its efficacy and safety in patients with NASH and stage 2 or 3 fibrosis (NCT03900429).
Mitochondria pyruvate carrier inhibitors
Pyruvate fuels the tricarboxylic acid cycle to produce citrate and oxaloacetate, which supports lipogenesis and neoglucogenesis, respectively. The mitochondrial pyruvate carrier (MPC) transports pyruvate across the mitochondria so that it can interact with the enzymes of the cycle. MSDC-0602K is an MPC inhibitor that has been evaluated in a 52-week, phase 2b dose-ranging clinical trial in subjects with biopsy-proven NASH. MSDC-0602K led to significant reductions in glucose, glycated haemoglobin (HbA1c), insulin, liver enzymes and NAFLD Activity Score (NAS) compared with placebo (NCT02784444).19 The efficacy of MSDC-0602K in both glycaemic control and NASH resolution will be assessed in a phase 3 clinical trial in patients with TD2M and NASH (NCT03970031).
FGF21 agonists
Fibroblast growth factor 21 (FGF21) is produced by the liver, adipose tissue and pancreas, and has pleiotropic metabolic effects including increasing energy expenditure, improving insulin sensitivity, reducing sugar intake and browning adipose tissue. The beta receptor of FGF21 is expressed in hepatocytes where it stimulates mitochondria beta-oxidation. In adipocytes, FGF21 stimulates the production of adiponectin. Pegbelfermin, a pegylated FGF21 analogue, administered for 16 weeks decreased hepatic fat fraction assessed by MRI proton density fat fraction (MRI-PDFF) in a phase 2 study (NCT02413372).20 The efficacy and safety of pegbelfermin, which has to be injected subcutaneously, are currently being investigated in phase 2b clinical trials: FALCON 1 (NCT03486899) in patients with NASH with bridging fibrosis; and FALCON 2 (NCT03486912) in those with NASH and compensated cirrhosis.
GLP-1 agonists
Glucagon-like peptide-1 (GLP-1) is an incretin hormone secreted by intestinal L cells at the postprandial phase. GLP-1 agonists target GLP-1 receptors expressed in various organs including the pancreas, intestine, adipose tissue and brain. GLP-1 regulates plasma glucose levels by stimulating glucose-dependent insulin secretion and inhibiting glucagon secretion. In addition, GLP-1 induces weight loss by reducing gastric emptying time while enhancing satiety by activation of GLP-1 receptors in the hypothalamus.
In the LIRA-NAFLD study, liraglutide treatment for 6 months in patients with uncontrolled T2DM was associated with weight reduction and a significant relative liver fat reduction of 31%, as assessed by magnetic resonance spectroscopy (NCT02721888).21 In a meta-analysis using data from the liraglutide clinical trial programme of >4000 patients with T2DM, liraglutide 1.8 mg daily showed a significant reduction of liver enzymes compared with placebo.22 Although this result was mainly mediated by weight loss and glycaemic control, these preliminary data led to the initiation of the LEAN study—a multicentre, double-blinded, randomised, placebo-controlled phase 2 trial that included 52 patients with NASH with and without diabetes—to further assess the safety and efficacy of liraglutide (NCT01237119).23 The LEAN study demonstrated a significant histological resolution of NASH without worsening of fibrosis in patients treated with liraglutide 1.8 mg daily compared with placebo. GLP-1 therapy is associated with GI side effects, such as nausea and vomiting, which occur at the initiation of the treatment. Furthermore, it is administered, like pegbelfermin, by subcutaneous injections making it inconvenient for some patients to self-administer. The new generation of GLP-1 agonists (dulaglutide, semaglutide, extended-release exenatide and albiglutide) has a longer duration of action with the advantage of weekly subcutaneous injection. Semaglutide 0.1, 0.2 and 0.4 mg once daily, which are different doses than the dose of semaglutide approved for the treatment of T2DM (1 mg weekly), is currently being tested in a phase 2b clinical trial in patients with NASH (NCT02970942). This large, multicentre, randomised clinical trial will provide confirmation of the effect of GLP-1 agonist on NASH resolution. Oral GLP-1 therapies are currently being tested with promising results for improving glycaemic control and weight loss.24 25 Cardiovascular safety has been demonstrated for GLP-1 agonists as a class effect in patients with T2DM.26–29 These trials have demonstrated a significant reduction of major adverse cardiac events using the composite endpoint of cardiovascular death, non-fatal myocardial infarction or non-fatal stroke.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide and GLP-1 receptor agonist, which has been investigated in patients with T2DM. In a 26-week, double-blind, randomised, phase 2 study in patients with T2DM, tirzepatide demonstrated a significant dose-dependent reduction of HbA1c up to −1.94% at 15 mg compared with—0.06% for placebo, and a potent dose-dependent weight reduction up to −11.3 kg for tirzepatide compared with −0.4 kg for placebo and −2.7 kg for dulaglutide.30 The efficacy of tirzepatide in patients with NASH is currently being investigated in the phase 2b SYNERGY-NASH trial (NCT04166773).
Cotadutide is a dual GLP-1 and glucagon receptor agonist that has been investigated in a 26-week, double-blind, phase 2b trial in overweight subjects with T2DM. It showed superior reduction in body weight and serum aminotransferases levels compared with liraglutide (NCT03235050).31
SGLT2 inhibitors
Sodium/glucose transport protein 2 (SGLT2) inhibitors are a class of antidiabetic agents that exert their glucose-lowering effects by inhibition of SGLT2, which accounts for ~90% of the glucose reabsorbed by the kidney. SGLT2 inhibitors induce a moderate weight loss of approximately 3%–4% and have consistently demonstrated reduced risk of cardiovascular events in patients with T2DM in large randomised clinical trials32 including the EMPA-REG OUTCOME trial for empagliflozin,33 the CANVAS Program for canagliflozin34 and the DECLARE-TIMI 58 trial for dapagliflozin.35 In addition, SGLT2 inhibitors have shown robust effects in reducing the progression of renal disease.32 Recently, results from the DAPA-HF study showed a significant risk reduction of worsening heart failure or death due to cardiovascular disease among patients with heart failure with or without T2DM.36 SGLT2 inhibitors induce multiple beneficial metabolic changes including a chronic shift in metabolic substrate utilisation, ketogenesis in the liver and increased utilisation of hepatic non-esterified fatty acids.37 Clinical studies have reported a reduction in plasma ALT levels driven by weight loss and glycaemic control.38–41 Randomised controlled trials have reported a decrease in hepatic fat content with empagliflozin,42 dapagliflozin40 and licogliflozin.43 Due to their beneficial effect on cardiovascular and kidney diseases, and glucose homeostasis, SGLT2 inhibitors may provide collateral benefits if these agents show improvement in resolution of NASH and fibrosis in future trials.
Chemokine inhibitors
C-C motif chemokine receptor (CCR) type 2 plays a role in the recruitment, migration and infiltration of proinflammatory monocytes and macrophages at the site of liver injury, and CCR5 in the activation and proliferation of collagen-producing activated hepatic stellate cells/myofibroblasts. Cenicriviroc is an oral, dual CCR2/CCR5 receptor inhibitor. In the phase 2b CENTAUR trial, cenicriviroc showed no effect on resolution of NASH, but an improvement in fibrosis stage after 1 year, although this effect was not significant after 2 years; however, patients with a decrease in fibrosis at year 1 maintained this benefit at year 2 (NCT02217475).44 The efficacy and safety of cenicriviroc are currently being tested in patients with NASH in a phase 3 AURORA clinical trial (NCT03028740).
Treatment combinations for NASH
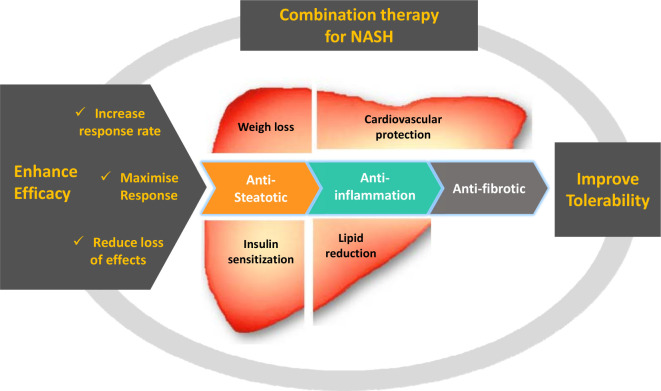
There are several reasons for treating patients with NASH with a combination of drugs, as shown in figure 2.
Figure 2.
Rationale for combination therapy to treat non-alcoholic steatohepatitis (NASH). Drugs with different mechanisms of action targeting hepatic steatosis, inflammation and fibrosis could be combined. Ideally, such combinations should be safe and have positive effects beyond the liver such as weight loss, cardiovascular protection, insulin sensitisation and lipid reduction.
Increasing response rate with combination therapy
Trials of drugs as monotherapy for the treatment of NASH have reported response rates <32% in comparison with placebo. Combination of two or more therapies may increase these response rates, meaning that the proportion of patients improving is larger with the combination than with a monotherapy. This strategy aims to convert non-responders or partial responders to monotherapy into responders. Given the heterogeneity in the drivers of fibrosis and NASH among the spectrum of patients with NASH, it is likely that multiple mechanistic pathways may need to be targeted to achieve an optimal histological response. In order to enhance the response rates for either one-stage improvement in fibrosis or resolution of NASH, one can speculate that two or three distinct pathways would need to be targeted to optimise response, for example, by combining drugs with metabolic activity along with predominantly anti-inflammatory activity may further enhance the likelihood of a histological response.
Several drugs are currently being tested in combination with FXR agonists (table 1). The results of 20 patients with NASH who received cilofexor 30 mg plus firsocostat 20 mg once daily in combination for 12 weeks in a ‘proof-of-concept’ study have been reported (NCT02781584): 74% of patients had >30% decrease in liver fat, as determined by MRI-PDFF, and serum ALT and GGT were significantly improved. ATLAS, a phase 2, randomised, double-blind, placebo-controlled study (NCT03449446), evaluated the safety and efficacy of monotherapy and dual combination regimens of cilofexor 30 mg, firsocostat 20 mg and selonsertib 18 mg in patients with advanced fibrosis, including bridging fibrosis and cirrhosis due to NASH. The selonsertib monotherapy arm was discontinued in the ATLAS trial following the negative results of selonsertib monotherapy in the STELLAR trials. In 392 treated patients, of whom 56% had compensated cirrhosis, a ≥1-stage improvement in fibrosis without worsening of NASH after 48 weeks of treatment was numerically higher in the combination therapy group (cilofexor and firsocostat) compared with placebo (20.9% vs 10.5%, p=0.17), respectively.45 Although the trial did not meet its primary endpoint, probably due to a small sample size, the numerical results were higher in the combination therapy group compared with cilofexor or firsocostat monotherapy. Furthermore, the combination therapy group (cilofexor plus firsocostat) was statistically significant for decreases in ≥2-points improvement in NAS, serum ALT and serum based non-invasive fibrosis markers compared with placebo. These results are to be interpreted with caution given the small sample size.
The ATLAS trial provides an example of efforts to use a lower dose of an FXR agonist with an ACC inhibitor with the aim of reducing side effects related to FXR, namely pruritus and LDL cholesterol increase, but still retaining efficacy in showing fibrosis improvements in patients with advanced fibrosis due to NASH (NCT03449446). Another study will test the combination of cilofexor and firsocostat with semaglutide (NCT03987074). Other trials that are planned include a trial of the FXR agonist tropifexor combined with the SGLT1/2 inhibitor licogliflozin (NCT04065841), and a trial combining tropifexor with the leukotriene A4 hydrolase inhibitor, LYS006 (NCT04147195). PF-05221304 and PF-06865571 are also being investigated in combination in a randomised, double-blind, placebo-controlled, phase 2 study to assess their pharmacodynamics, safety and tolerability for 6 weeks in adults with NAFLD (NCT03776175).
Maximising response with combination therapy
Primary endpoints of phase 3 trials of patients with NASH are either improvement of fibrosis without worsening of NASH or resolution of NASH without worsening of fibrosis. Maximising the response with combination therapy means that for a given patient the response is bigger with the combination than with monotherapy. The optimal response would be to improve fibrosis and have resolution of NASH. Fibrosis is not part of the definition of NASH but it is a consequence of the chronic metabolic overload and inflammation. Fibrosis is a relevant therapeutic endpoint since it dictates the prognosis of the disease. It is logical from a clinical perspective to combine drugs to improve the fibrosis and to decrease the metabolic stress and inflammation that drives the fibrotic process. The phase 2 TANDEM trial assesses the combination of cenicriviroc with two doses of the FXR agonist tropifexor over 48 weeks (NCT03517540).
Combination with antidiabetic drugs
Patients with T2DM have a high prevalence of NAFLD, 60%–80% depending on diagnostic methods used46–52; 30%–40% are estimated to have NASH53 54 and 7%–20% to have advanced fibrosis.52 55 56 Several studies have demonstrated that the coexistence of T2DM and NAFLD worsen the course of either disease. Indeed, T2DM is an independent risk factor for the progression of NAFLD to NASH and advanced fibrosis, which increases the risk of progression to cirrhosis, liver-related mortality and hepatocellular carcinoma.57–60 Also, the presence of NAFLD in patients with T2DM hampers maintenance of optimal glycaemic control as it increases hepatic and peripheral insulin resistance.61 Moreover, an increased risk of both macrovascular and microvascular complications of T2DM has been reported when NAFLD is present.62–65 Combination of antidiabetic drugs with anti-NASH drugs may help improve both liver-related and diabetes-related outcomes while improving glucose homeostasis. The addition of vitamin E to pioglitazone was tested over 18 months in a randomised trial in patients with T2DM. Pioglitazone alone resulted in significantly more frequent resolution of NASH and improvement of fibrosis than placebo; the addition of vitamin E resulted in a numerically greater response, although this was not significantly different from pioglitazone alone.66 Of particular interest are antidiabetic drugs that lead to weight loss, such as GLP-1 agonist and SGLT2 inhibitors. The FXR agonist, tropifexor, is being investigated in combination with the SGLT1/2 inhibitor, licogliflozin, for a duration of 48 weeks as a treatment for adults with fibrotic NASH; this study will assess a histological endpoint (NCT04065841). The GLP-1 agonist, semaglutide, is being investigated as monotherapy and in combination with the FXR agonist, cilofexor, and in combination with the ACC inhibitor, firsocostat, in a phase 2 proof-of-concept trial (NCT03987074).
Decreasing side effects with combination therapy
Drug combination may decrease side effects in two ways. First, drugs may have dose-dependent side effects and their use in combination may allow using lower doses to increase tolerability without compromising efficacy. Second, addition of a drug may be prescribed to mitigate the side effect of the first drug. There are currently two examples of this strategy. FXR agonists, including obeticholic acid, increase LDL cholesterol; combination with a statin may decrease this side effect. This was tested in the randomised, placebo-controlled, double-blind CONTROL phase 2 study. After 4 weeks of obeticholic acid, LDL cholesterol increased; addition of atorvastatin subsequently decreased LDL cholesterol below baseline values (NCT02633956).67 In the second example, ACC inhibition may be associated with hypertriglyceridaemia; combination with fenofibrate may decrease this side effect. In a phase 2 randomised study, fenofibrate was prescribed 2 weeks before the addition of firsocostat in patients with advanced fibrosis due to NASH. Not only did the combination prevent increase in triglycerides, but it also improved hepatic fat and liver biochemistry (NCT02781584).68
Addressing loss of effects
A drug with a narrow mechanism of action may lose its effects over time due to adaptive mechanisms. Combinations may reduce the rate of escape to a monotherapy. There is currently no combination trial designed with this rationale.
Challenges of combination therapies for NASH
Selection of drugs for combination
Only considering drugs which have shown an effect in clinical trials as monotherapy, the number of combinations is so high that many of them will never be tested. Besides, focusing only on drugs with demonstrated effects is not correct: a drug without individual effects as monotherapy such as, for example, selonsertib should not necessarily be discarded as it may display synergistic effects in a combination. One way to select combination partners may be based on different and complementary mechanisms of action. Development strategy to test combinations in phase 3 clinical trials may include drugs which have not been tested in a phase 3, but in a phase 2 trial as monotherapy; whether such acceleration in drug development is acceptable is debatable.
Chronology
Possible sequences for when to introduce each component drug of a combination therapy for NASH can be outlined as follows:
Overlapping. The combination is given from the start to the end of the treatment.
Outlasting. The combination is given from the start and one drug is stopped as it reaches a specific endpoint whereas the second drug is given longer as a maintenance therapy.
Addition. One drug is prescribed, with a second drug introduced when the effect of the first drug declines or is insufficient.
All current trials follow an overlapping combination sequence, except for addition of a statin to obeticholic acid.
Safety and side effects
Side effects are a major concern in a population of patients with chronic liver disease. Combination approaches need to have no more side effects or safety signals than monotherapies. As combination trials are ongoing, particular attention has to be paid to safety and side effects and these protocols should capture information on quality of life and patient-related outcomes.
Selecting a target population
Given the complexity of the pathophysiology of NASH and patient heterogeneity, it is essential to select adequate populations for a specific combination. This requires the development of predictive biomarkers of response. Determination of genetic polymorphisms could provide relevant information regarding response to treatment. Kawaguchi-Suzuki et al reported that a single nucleotide polymorphism rs903361 in the ADORA1 gene was associated with resolution of NASH in patients treated with pioglitazone.69 Recently, a genome-wide analysis study identified several loci associated with response to obeticholic acid in patients with NASH.70 More research in this field is needed before we see the introduction of predictive biomarkers in NASH.
Trial design
Variability of the reponse rate due to unaccountable changes in lifestyles may lead to uncontrolled improvement and jeopardise the outcome of a trial also in case of combination. Another difficulty with combination trials is the number of arms necessary to demonstrate an advantage of the combination. Ideally, four arms with placebo should be considered, where each drug would be tested as monotherapy and in combination. With numerous combinations of interest, the number of patients to be included in trials will increase as well as the costs of clinical development.
Conclusion
A strategy of combining therapies to treat NASH seems like a natural progression and several combinations are already being tested in phase 2 trials. Further studies are needed to improve our understanding for better identifying patients who would have a higher likelihood of treatment response with a specific combination therapy. This would only be possible if credible non-invasive biomarkers can be developed to reliably predict histological and clinical responses to facilitate efficient screening of suitable individual therapies that provide synergistic effects when combined.
Footnotes
Twitter: @dufour_jf
Correction notice: This article has been corrected since it published Online First. The title has been corrected.
Contributors: All authors: drafting of the manuscript, critical revision of the manuscript, approved final submission.
Funding: RL receives funding support from NIEHS (5P42ES010337), NCATS (5UL1TR001442), NIDDK (R01DK106419, P30DK120515) and DOD PRCRP (CA170674P2). J-FD receives funding from the Swiss National Foundation (310030_185219) and CC receives no relevant for this publication
Competing interests: CC received consultant fees from NovoNordisk, AstraZeneca, Gilead. J-FD Advisory committees: Bayer, BMS, Falk, Genfit, Genkyotex, Gilead Science, HepaRegenix, Intercept, Eli Lilly, Merck, Novartis; Speaking and teaching: Bayer, BristolMyers Squibb, Intercept, Genfit, Gilead Science, Novartis. RL serves as a consultant or advisory board member for Arrowhead Pharmaceuticals, AstraZeneca, Bird Rock Bio, Boehringer Ingelheim, Bristol-Myer Squibb, Celgene, Cirius, CohBar, Conatus, Eli Lilly, Galmed, Gemphire, Gilead, Glympse bio, GNI, GRI Bio, Intercept, Ionis, Janssen, Merck, Metacrine, NGM Biopharmaceuticals, Novartis, Novo Nordisk, Pfizer, Prometheus, Sanofi, Siemens, and Viking Therapeutics. In addition, his institution has received grant support from Allergan, Boehringer-Ingelheim, Bristol-Myers Squibb, Cirius, Eli Lilly and Company, Galectin Therapeutics, Galmed Pharmaceuticals, GE, Genfit, Gilead, Intercept, Grail, Janssen, Madrigal Pharmaceuticals, Merck, NGM Biopharmaceuticals, NuSirt, Pfizer, pH Pharma, Prometheus, and Siemens. He is also cofounder of Liponexus.
Patient consent for publication: Not required.
Provenance and peer review: Commissioned; externally peer reviewed.
References
- 1. Younossi ZM, Ratziu V, Loomba R, et al. Obeticholic acid for the treatment of non-alcoholic steatohepatitis: interim analysis from a multicentre, randomised, placebo-controlled phase 3 trial. Lancet 2019;394:2184–96. 10.1016/S0140-6736(19)33041-7 [DOI] [PubMed] [Google Scholar]
- 2. Sanyal AJ, Ratziu V, Loomba R, et al. Obeticholic acid treatment in patients with non alcoholic steatohepatitis: a secondary analysis of the regenerate study across fibrosis stages. Hepatology 2019:23A. [Google Scholar]
- 3. Tropifexor SA. A highly potent FXR agonist, produces robust and dose-dependent reductions in hepatic fat and serum alanine aminotransferase in patients with fibrotic NASH after 12 weeks of therapy: FLIGH-FXR part C interim results. Hepatology 2019;70. [Google Scholar]
- 4. Neuschwander-Tetri BA, Loomba R, Sanyal AJ, et al. Farnesoid X nuclear receptor ligand obeticholic acid for non-cirrhotic, non-alcoholic steatohepatitis (FLINT): a multicentre, randomised, placebo-controlled trial. Lancet 2015;385:956–65. 10.1016/S0140-6736(14)61933-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Traussnigg S, Schattenberg JM, Demir M, et al. Norursodeoxycholic acid versus placebo in the treatment of non-alcoholic fatty liver disease: a double-blind, randomised, placebo-controlled, phase 2 dose-finding trial. Lancet Gastroenterol Hepatol 2019;4:781–93. 10.1016/S2468-1253(19)30184-0 [DOI] [PubMed] [Google Scholar]
- 6. Chalasani NP, Sanyal AJ, Kowdley KV, et al. Pioglitazone versus vitamin E versus placebo for the treatment of non-diabetic patients with non-alcoholic steatohepatitis: PIVENS trial design. Contemp Clin Trials 2009;30:88–96. 10.1016/j.cct.2008.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cusi K, Orsak B, Bril F, et al. Long-Term pioglitazone treatment for patients with nonalcoholic steatohepatitis and prediabetes or type 2 diabetes mellitus: a randomized trial. Ann Intern Med 2016;165:305–15. 10.7326/M15-1774 [DOI] [PubMed] [Google Scholar]
- 8. Musso G, Cassader M, Paschetta E, et al. Thiazolidinediones and advanced liver fibrosis in nonalcoholic steatohepatitis: a meta-analysis. JAMA Intern Med 2017;177:633–40. 10.1001/jamainternmed.2016.9607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American association for the study of liver diseases. Hepatology 2018;67:328–57. 10.1002/hep.29367 [DOI] [PubMed] [Google Scholar]
- 10. European Association for the Study of the Liver Electronic address eee, European association for the study of D, European association for the study of O. EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 2016;64:1388–402. [DOI] [PubMed] [Google Scholar]
- 11. Ratziu V, Harrison SA, Francque S, et al. Elafibranor, an Agonist of the Peroxisome Proliferator-Activated Receptor-α and -δ, Induces Resolution of Nonalcoholic Steatohepatitis Without Fibrosis Worsening. Gastroenterology 2016;150:1147–59. 10.1053/j.gastro.2016.01.038 [DOI] [PubMed] [Google Scholar]
- 12. Gawrieh S. A phase 2, prospective, multicenter, double-blind, randomized study of sarogliazar magnesium 1 mg, 2 mg or 4 mg versus placebo in patients with NAFLD and/or NASH (evidence IV). Hepatology 2019;70. [Google Scholar]
- 13. Ratziu V, de Guevara L, Safadi R, et al. One-year results of the globalphase 2brandomized placebo-controlled arrest trial of aramchol, a stearyl CoA desaturase modulator in 247 NASH patients. Hepatology 2018;68. [Google Scholar]
- 14. Loomba R, Kayali Z, Noureddin M, et al. GS-0976 reduces hepatic steatosis and fibrosis markers in patients with nonalcoholic fatty liver disease. Gastroenterology 2018;155:1463–73. 10.1053/j.gastro.2018.07.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Amin N, Carvajal-Gonzalez S, Arggawal N, et al. PF-05221304 (PF’1304), a liver-targeted acetyl-CoA carboxylase inhibitor (ACCI), in afults with non-alcoholic fatty liver disease demonstrates robust reductions in liver fat and ALT - phase 2a, dose ranging study. Hepatology 2019;70 Suppl:21. [Google Scholar]
- 16. Calle R, Bergman A, Somayaji V, et al. PS-110-Ketohexokinase inhibitor PF-06835919 administered for 6 weeks reduces whole liver fat as measured by magnetic resonance imaging-proton density fat fraction in subjects with non-alcoholic fatty liver disease. J Hepatol 2019;70:e69–70. 10.1016/S0618-8278(19)30122-7 [DOI] [Google Scholar]
- 17. Loomba R, Neutel J, Mohseni R, et al. LBP-20-VK2809, a novel liver-directed thyroid receptor beta agonist, significantly reduces liver fat with both low and high doses in patients with non-alcoholic fatty liver disease: a phase 2 randomized, placebo-controlled trial. J Hepatol 2019;70:e150–1. 10.1016/S0618-8278(19)30266-X [DOI] [Google Scholar]
- 18. Harrison SA, Bashir MR, Guy CD, et al. Resmetirom (MGL-3196) for the treatment of non-alcoholic steatohepatitis: a multicentre, randomised, double-blind, placebo-controlled, phase 2 trial. Lancet 2019;394:2012–24. 10.1016/S0140-6736(19)32517-6 [DOI] [PubMed] [Google Scholar]
- 19. Harrison SA, Alkhouri N, Davison BA, et al. Insulin sensitizer MSDC-0602K in non-alcoholic steatohepatitis: a randomized, double-blind, placebo-controlled phase IIb study. J Hepatol 2020;72:613–26. 10.1016/j.jhep.2019.10.023 [DOI] [PubMed] [Google Scholar]
- 20. Sanyal A, Charles ED, Neuschwander-Tetri BA, et al. Pegbelfermin (BMS-986036), a PEGylated fibroblast growth factor 21 analogue, in patients with non-alcoholic steatohepatitis: a randomised, double-blind, placebo-controlled, phase 2A trial. Lancet 2019;392:2705–17. 10.1016/S0140-6736(18)31785-9 [DOI] [PubMed] [Google Scholar]
- 21. Petit J-M, Cercueil J-P, Loffroy R, et al. Effect of liraglutide therapy on liver fat content in patients with inadequately controlled type 2 diabetes: the Lira-NAFLD study. J Clin Endocrinol Metab 2017;102:407–15. 10.1210/jc.2016-2775 [DOI] [PubMed] [Google Scholar]
- 22. Armstrong MJ, Houlihan DD, Rowe IA, et al. Safety and efficacy of liraglutide in patients with type 2 diabetes and elevated liver enzymes: individual patient data meta-analysis of the lead program. Aliment Pharmacol Ther 2013;37:234–42. 10.1111/apt.12149 [DOI] [PubMed] [Google Scholar]
- 23. Armstrong MJ, Gaunt P, Aithal GP, et al. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (lean): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet 2016;387:679–90. 10.1016/S0140-6736(15)00803-X [DOI] [PubMed] [Google Scholar]
- 24. Pieber TR, Bode B, Mertens A, et al. Efficacy and safety of oral semaglutide with flexible dose adjustment versus sitagliptin in type 2 diabetes (pioneer 7): a multicentre, open-label, randomised, phase 3A trial. Lancet Diabetes Endocrinol 2019;7:528–39. 10.1016/S2213-8587(19)30194-9 [DOI] [PubMed] [Google Scholar]
- 25. Davies M, Pieber TR, Hartoft-Nielsen M-L, et al. Effect of oral Semaglutide compared with placebo and subcutaneous Semaglutide on glycemic control in patients with type 2 diabetes: a randomized clinical trial. JAMA 2017;318:1460–70. 10.1001/jama.2017.14752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pfeffer MA, Claggett B, Diaz R, et al. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med 2015;373:2247–57. 10.1056/NEJMoa1509225 [DOI] [PubMed] [Google Scholar]
- 27. Hernandez AF, Green JB, Janmohamed S, et al. Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (harmony outcomes): a double-blind, randomised placebo-controlled trial. Lancet 2018;392:1519–29. 10.1016/S0140-6736(18)32261-X [DOI] [PubMed] [Google Scholar]
- 28. Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2016;375:311–22. 10.1056/NEJMoa1603827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2016;375:1834–44. 10.1056/NEJMoa1607141 [DOI] [PubMed] [Google Scholar]
- 30. Frias JP, Nauck MA, Van J, et al. Efficacy and safety of LY3298176, a novel dual GIP and GLP-1 receptor agonist, in patients with type 2 diabetes: a randomised, placebo-controlled and active comparator-controlled phase 2 trial. Lancet 2018;392:2180–93. 10.1016/S0140-6736(18)32260-8 [DOI] [PubMed] [Google Scholar]
- 31. Nahra r, Wang T, Oscarsson J, et al. Effects of cotadutide (MEDI0382) on biomarkers of non-alcoholic steatohepatitis in overweight or obese subjects with type 2 diabetes mellitus: a 26-week analysis of a randomized phase 2B study. Hepatology 2019;70:24A. [Google Scholar]
- 32. Zelniker TA, Wiviott SD, Raz I, et al. SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet 2019;393:31–9. 10.1016/S0140-6736(18)32590-X [DOI] [PubMed] [Google Scholar]
- 33. Zinman B, Lachin JM, Inzucchi SE. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 2016;374:1094. 10.1056/NEJMc1600827 [DOI] [PubMed] [Google Scholar]
- 34. Neal B, Perkovic V, Matthews DR. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med 2017;377:377. 10.1056/NEJMc1712572 [DOI] [PubMed] [Google Scholar]
- 35. Wiviott SD, Raz I, Sabatine MS. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. reply. N Engl J Med 2019;380:347–57. 10.1056/NEJMoa1812389 [DOI] [PubMed] [Google Scholar]
- 36. McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med 2019;381:1995–2008. 10.1056/NEJMoa1911303 [DOI] [PubMed] [Google Scholar]
- 37. Thomas MC, Cherney DZI. The actions of SGLT2 inhibitors on metabolism, renal function and blood pressure. Diabetologia 2018;61:2098–107. 10.1007/s00125-018-4669-0 [DOI] [PubMed] [Google Scholar]
- 38. Seko Y, Sumida Y, Sasaki K, et al. Effects of canagliflozin, an SGLT2 inhibitor, on hepatic function in Japanese patients with type 2 diabetes mellitus: pooled and subgroup analyses of clinical trials. J Gastroenterol 2018;53:140–51. 10.1007/s00535-017-1364-8 [DOI] [PubMed] [Google Scholar]
- 39. Sattar N, Fitchett D, Hantel S, et al. Empagliflozin is associated with improvements in liver enzymes potentially consistent with reductions in liver fat: results from randomised trials including the EMPA-REG OUTCOME® trial. Diabetologia 2018;61:2155–63. 10.1007/s00125-018-4702-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Latva-Rasku A, Honka M-J, Kullberg J, et al. The SGLT2 inhibitor dapagliflozin reduces liver fat but does not affect tissue insulin sensitivity: a randomized, double-blind, placebo-controlled study with 8-Week treatment in type 2 diabetes patients. Diabetes Care 2019;42:931–7. 10.2337/dc18-1569 [DOI] [PubMed] [Google Scholar]
- 41. Eriksson JW, Lundkvist P, Jansson P-A, et al. Effects of dapagliflozin and n-3 carboxylic acids on non-alcoholic fatty liver disease in people with type 2 diabetes: a double-blind randomised placebo-controlled study. Diabetologia 2018;61:1923–34. 10.1007/s00125-018-4675-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Kuchay MS, Krishan S, Mishra SK, et al. Effect of Empagliflozin on liver fat in patients with type 2 diabetes and nonalcoholic fatty liver disease: a randomized controlled trial (E-LIFT trial). Diabetes Care 2018;41:1801–8. 10.2337/dc18-0165 [DOI] [PubMed] [Google Scholar]
- 43. Harisson S, Manghi F, Smith WB, et al. LIK066 (licogliflozin), an SGLT1/2 inhibitor, robustly decreases ALT and improves markers of hepatic and metabolic health in patients witn non-alcoholic fatty liver disease: interim analysis of a 12-week, randomized, placebo controlled, phase 2A study. Hepatology 2019;70. [Google Scholar]
- 44. Ratziu V, Sanyal A, Francque S, et al. Cenicriviroc treatment for adults with non-alcoholic steatohepatitis: year 2 analysis of the phase 2B CENTAUR study. J Hepatol 2018;68:S1–2. 10.1016/S0168-8278(18)30221-6 [DOI] [PubMed] [Google Scholar]
- 45. Press release: Gilead Announces Topline results from phase 2 atlas study in patients with bridging fibrosis (F3) and compensated cirrhosis (F4) due to nonalcoholic steatohepatitis (NASH) 2019.
- 46. Williams CD, Stengel J, Asike MI, et al. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology 2011;140:124–31. 10.1053/j.gastro.2010.09.038 [DOI] [PubMed] [Google Scholar]
- 47. Targher G, Bertolini L, Padovani R, et al. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care 2007;30:1212–8. 10.2337/dc06-2247 [DOI] [PubMed] [Google Scholar]
- 48. Williamson RM, Price JF, Hayes PC, et al. Prevalence and markers of advanced liver disease in type 2 diabetes. QJM 2012;105:425–32. 10.1093/qjmed/hcr233 [DOI] [PubMed] [Google Scholar]
- 49. Portillo-Sanchez P, Bril F, Maximos M, et al. High prevalence of nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus and normal plasma aminotransferase levels. J Clin Endocrinol Metab 2015;100:2231–8. 10.1210/jc.2015-1966 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Leite NC, Villela-Nogueira CA, Pannain VLN, et al. Histopathological stages of nonalcoholic fatty liver disease in type 2 diabetes: prevalences and correlated factors. Liver Int 2011;31:700–6. 10.1111/j.1478-3231.2011.02482.x [DOI] [PubMed] [Google Scholar]
- 51. Byrne CD, Olufadi R, Bruce KD, et al. Metabolic disturbances in non-alcoholic fatty liver disease. Clin Sci 2009;116:539–64. 10.1042/CS20080253 [DOI] [PubMed] [Google Scholar]
- 52. Doycheva I, Cui J, Nguyen P, et al. Non-invasive screening of diabetics in primary care for NAFLD and advanced fibrosis by MRI and MRE. Aliment Pharmacol Ther 2016;43:83–95. 10.1111/apt.13405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Lomonaco R, Ortiz-Lopez C, Orsak B, et al. Role of ethnicity in overweight and obese patients with nonalcoholic steatohepatitis. Hepatology 2011;54:837–45. 10.1002/hep.24483 [DOI] [PubMed] [Google Scholar]
- 54. Lomonaco R, Bril F, Portillo-Sanchez P, et al. Metabolic impact of nonalcoholic steatohepatitis in obese patients with type 2 diabetes. Diabetes Care 2016;39:632–8. 10.2337/dc15-1876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Arab JP, Barrera F, Gallego C, et al. High prevalence of undiagnosed liver cirrhosis and advanced fibrosis in type 2 diabetic patients. Ann Hepatol 2016;15:721–8. 10.5604/16652681.1212434 [DOI] [PubMed] [Google Scholar]
- 56. Yeung M-W, Wong GL-H, Choi KC, et al. Advanced liver fibrosis but not steatosis is independently associated with albuminuria in Chinese patients with type 2 diabetes. J Hepatol 2017. doi: 10.1016/j.jhep.2017.09.020. [Epub ahead of print: 06 Oct 2017]. [DOI] [PubMed] [Google Scholar]
- 57. Neuschwander-Tetri BA, Clark JM, Bass NM, et al. Clinical, laboratory and histological associations in adults with nonalcoholic fatty liver disease. Hepatology 2010;52:913–24. 10.1002/hep.23784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Younossi ZM, Gramlich T, Matteoni CA, et al. Nonalcoholic fatty liver disease in patients with type 2 diabetes. Clin Gastroenterol Hepatol 2004;2:262–5. 10.1016/S1542-3565(04)00014-X [DOI] [PubMed] [Google Scholar]
- 59. McPherson S, Hardy T, Henderson E, et al. Evidence of NAFLD progression from steatosis to fibrosing-steatohepatitis using paired biopsies: implications for prognosis and clinical management. J Hepatol 2015;62:1148–55. 10.1016/j.jhep.2014.11.034 [DOI] [PubMed] [Google Scholar]
- 60. Wang P, Kang D, Cao W, et al. Diabetes mellitus and risk of hepatocellular carcinoma: a systematic review and meta-analysis. Diabetes Metab Res Rev 2012;28:109–22. 10.1002/dmrr.1291 [DOI] [PubMed] [Google Scholar]
- 61. Birkenfeld AL, Shulman GI. Nonalcoholic fatty liver disease, hepatic insulin resistance, and type 2 diabetes. Hepatology 2014;59:713–23. 10.1002/hep.26672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Bril F, Sninsky JJ, Baca AM, et al. Hepatic steatosis and insulin resistance, but not steatohepatitis, promote atherogenic dyslipidemia in NAFLD. J Clin Endocrinol Metab 2016;101:644–52. 10.1210/jc.2015-3111 [DOI] [PubMed] [Google Scholar]
- 63. Targher G, Bertolini L, Rodella S, et al. Non-alcoholic fatty liver disease is independently associated with an increased prevalence of chronic kidney disease and proliferative/laser-treated retinopathy in type 2 diabetic patients. Diabetologia 2008;51:444–50. 10.1007/s00125-007-0897-4 [DOI] [PubMed] [Google Scholar]
- 64. Targher G, Bertolini L, Rodella S, et al. Relationship between kidney function and liver histology in subjects with nonalcoholic steatohepatitis. Clin J Am Soc Nephrol 2010;5:2166–71. 10.2215/CJN.05050610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Li Y, Zhu S, Li B, et al. Association between non-alcoholic fatty liver disease and chronic kidney disease in population with prediabetes or diabetes. Int Urol Nephrol 2014;46:1785–91. 10.1007/s11255-014-0796-9 [DOI] [PubMed] [Google Scholar]
- 66. Bril F, Biernacki DM, Kalavalapalli S, et al. Role of vitamin E for nonalcoholic steatohepatitis in patients with type 2 diabetes: a randomized controlled trial. Diabetes Care 2019;42:1481–8. 10.2337/dc19-0167 [DOI] [PubMed] [Google Scholar]
- 67. Pockros PJ, Fuchs M, Freilich B, et al. Control: a randomized phase 2 study of obeticholic acid and atorvastatin on lipoproteins in nonalcoholic steatohepatitis patients. Liver Int 2019;39:2082–93. 10.1111/liv.14209 [DOI] [PubMed] [Google Scholar]
- 68. Lawitz E, Neff G, Ruane P, et al. Fenofibrate mitigates increases in serum triglycerides due to ACC inhibitor firsocostat in patients with advanced fibrosis due to NASH: a phase 2 randomized trial. Hepatology 2019;70. [Google Scholar]
- 69. Kawaguchi-Suzuki M, Cusi K, Bril F, et al. A genetic score associates with pioglitazone response in patients with non-alcoholic steatohepatitis. Front Pharmacol 2018;9:752. 10.3389/fphar.2018.00752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Gawrieh S, Guo X, Tan J, et al. A pilot genome-wide analysis study identifies loci associated with response to obeticholic acid in patients with NASH. Hepatol Commun 2019;3:1571–84. 10.1002/hep4.1439 [DOI] [PMC free article] [PubMed] [Google Scholar]