Abstract
Objective
This observational cross-sectional multicenter study aimed to evaluate the longitudinal impact of the coronavirus disease 2019 (COVID-19) pandemic on neurosurgical practice.
Methods
We included 29 participating neurosurgeons in centers from all geographical regions in the Kingdom of Saudi Arabia. The study period, which was between March 5, 2020 and May 20, 2020, was divided into three equal periods to determine the longitudinal effect of COVID-19 measures on neurosurgical practice over time.
Results
During the 11-week study period, 474 neurosurgical interventions were performed. The median number of neurosurgical procedures per day was 5.5 (interquartile range [IQR]: 3.5–8). The number of cases declined from 72 in the first week and plateaued at the 30′s range in subsequent weeks. The most and least number of performed procedures were oncology (129 [27.2 %]) and functional procedures (6 [1.3 %]), respectively. Emergency (Priority 1) cases were more frequent than non-urgent (Priority 4) cases (178 [37.6 %] vs. 74 [15.6 %], respectively). In our series, there were three positive COVID-19 cases. There was a significant among-period difference in the length of hospital stay, which dropped from a median stay of 7 days (IQR: 4–18) to 6 (IQR: 3–13) to 5 days (IQR: 2–8). There was no significant among-period difference with respect to institution type, complications, or mortality.
Conclusion
Our study demonstrated that the COVID-19 pandemic decreased the number of procedures performed in neurosurgery practice. The load of emergency neurosurgery procedures did not change throughout the three periods, which reflects the need to designate ample resources to cover emergencies. Notably, with strict screening for COVID -19 infections, neurosurgical procedures could be safely performed during the early pandemic phase. We recommend to restart performing neurosurgical procedures once the pandemic gets stabilized to avoid possible post pandemic health-care system intolerable overload.
Abbreviation: COVID-19, Coronavirus disease 2019
Keywords: Neurosurgery, COVID-19, Pandemic, Impact, Neurosurgical practice
1. Introduction
In December 2019, the novel coronavirus was first reported in the Wuhan region of China. The number of people infected with the novel respiratory viral illness has rapidly increased in all continents as it continues to globally spread. On March 11, 2020, the World Health Organization declared COVID-19 a pandemic [1]. By May 31, 2020, the number of confirmed cases globally exceeded 6 million with >300,000 confirmed deaths [2].
In the Kingdom of Saudi Arabia, the first case of COVID-19 was reported on March 2, 2020 [3]. Subsequently, the Saudi government took proactive measures for controlling the virus spread and keeping the public safe [4,5]. These measures included halting air travel, border closures, suspension of religious pilgrimages, suspension of in-person schooling, and switching all educational activities to online platforms [4,5]. By March 14, the number of locally confirmed COVID-19 cases exceeded 100 [3]. In collaboration with multiple government stakeholders, the Saudi Ministry of Health devised plans for flattening the curve and minimizing the spread of the virus among the population and healthcare workers [4]. The Saudi Center for Disease Prevention and Control and the Saudi Patient Safety Center (SPSC) developed and monitored hospital policies to ensure safety during the pandemic [6,7]. Multiple measures were taken to reduce transmission among healthcare providers, such as ensuring proper personal protective equipment (PPE), training on PPE donning and doffing, and surge preparation. Hospitals and neurosurgical services followed patient triaging protocols and screening guidelines promoted by the SPSC to ensure the safety of both patients and providers [8].
Recently, we published a quantitative study evaluating the early pandemic phase and its effect on the distribution of neurosurgical cases compared to the pre-pandemic periods [9]. This previous study reported no change in the absolute number of acute neurosurgery emergencies. Notably, there were no significant changes in the distribution of treated pathologies. By May 22nd, the number of confirmed cases in Saudi Arabia had exceeded 70,000 [3]. The majority of the literature discussing the effects of the outbreak on neurosurgical practice is based on surgeon-completed surveys and questionnaires, which are prone to recall bias and may give an inaccurate representation of the actual status. This study aimed to objectively evaluate the longitudinal impact of COVID-19 on neurosurgical practice in Saudi Arabia during the pandemic.
2. Materials and methods
2.1. Study design and setting
We performed an observational cross-sectional multicenter study to assess the longitudinal impact of COVID-19 on neurosurgical practice in Saudi Arabia. Data were collected from March 5, 2020 through May 20, 2020. The centers were included from all major cities and geographical regions in the Kingdom. We included both private and public hospitals providing full neurosurgical services. Public hospitals were from all healthcare sectors, including the academic sector, military, and ministry of health.
The study was approved by the Institutional Review Board (IRB) at King Saud University Medical City, Riyadh, Saudi Arabia (IRB no. 20/0341/IRB).
2.2. Data source and variables
We collected data from 29 neurosurgeons. The participants were fully privileged consultants at their institution with a practice of ≥2 years. To study the longitudinal effect of COVID-19 measures on neurosurgical practice over time, the study timeline was divided into three equal periods as follows: Period 1 (March 5-March 30), Period 2 (March 31-April 25), and Period 3 (April 26-May 20). We included neurosurgical procedures performed on both adult and pediatric patients and collected the following data: demographic information; e.g., age, gender, and institution type (public or private). Additionally, we collected information regarding surgical interventions, including diagnosis, surgical intervention category, case priority, general and craniospinal complications, length of hospital stay, and 30-day mortality. Surgical interventions were categorized into the following nine major subcategories: trauma, oncology, spine, vascular, congenital, hydrocephalus, peripheral nerves, functional, and infection. Intervention priorities were set according to the previously published Saudi Association of Neurological Surgery priority list consensus statement [8]. We define the four major priority levels as follows. Priority 1 (immediate) indicates cases requiring immediate intervention. Priority 1 (1–24 h) is for urgent cases that can be performed within 24 h of presentation. Priority 2 is for cases requiring intervention within one week. Priority 3 is for cases requiring intervention between one and four weeks. Priority 4 is for cases that can be delayed for >4 weeks. We collected information regarding COVID-19 testing, timing of testing, and COVID-19 related complications. At the end of the study period, the participating surgeons received a simple survey questionnaire for evaluating the reasons underlying the decreasing number of surgical procedures in their practice during the study period.
2.3. Statistical analysis
The study duration was divided into three distinct periods. Normally distributed demographic and surgical intervention characteristics during the three study periods were compared using a two-way T-test. Non-normally distributed and cross-tabulation data were compared using the Mann-Whitney and Pearson's chi-squared test, respectively. Statistical significance was set at P-value < 0.05. Statistical analyses were performed using Stata 14 statistical software (StataCorp, College Station, Texas).
3. Results
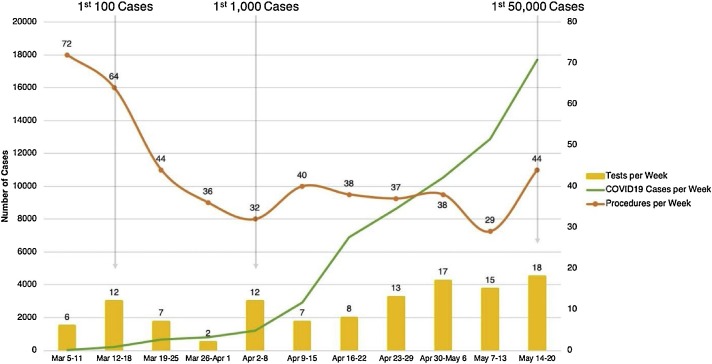
We included 474 neurosurgical interventions performed during the 11-week study period (Table 1 ). The mean age was 35 years (±22.4), with 293 (61.8 %) patients being male. The median number of performed procedures per day was 5.5 cases (interquartile range [IQR]: 3.5–8). Most cases were performed at public hospitals (332 [70 %] vs. 142 [30 %] performed in private hospitals). The number of procedures per week declined from 72 and 64 cases in the first 2 weeks, respectively, to 29 and 44 cases in the last 2 weeks, respectively (Fig. 1 ). With regard to the case categories, oncology cases were the highest (129 [27.2 %]), followed by spinal (89 [18.8 %]) and vascular interventions (83 [17.5 %]). With regard to the distribution of priority levels, Priority 1 cases were the most common (178 [37.6 %]), followed by Priority 2 (146 [30.8 %]), Priority 3 (76 [16 %]), and Priority 4 (74 [15.6 %]) cases.
Table 1.
Patients characteristics.
| Variable | n = 474 |
|---|---|
| Age, mean by year (SD) | 35 (22.4) |
| Gender | |
| Male, n (%) | 293 (61.8) |
| Female, n (%) | 181 (38.2) |
| Procedures per day, median (IQR) | 5.5 (3.5–8) |
| Institution type | |
| Public, n (%) | 332 (70) |
| Private, n (%) | 142 (30) |
| Diagnosis category | |
| Trauma, n (%) | 42 (8.9) |
| Oncology, n (%) | 129 (27.2) |
| Spine, n (%) | 89 (18.8) |
| Vascular, n (%) | 83 (17.5) |
| Congenital, n (%) | 19 (4) |
| Hydrocephalus, n (%) | 65 (13.7) |
| Peripheral Nerve, n (%) | 12 (2.5) |
| Functional, n (%) | 6 (1.3) |
| Infections, n (%) | 29 (6.1) |
| Priority of the case | |
| Priority 1 (Immediate), n (%) | 89 (18.8) |
| Priority 1 (1−24 h), n (%) | 89 (18.8) |
| Priority 2 (1−7 d), n (%) | 146 (30.8) |
| Priority 3 (1−4 w), n (%) | 76 (16) |
| Priority 4 (>4 w), n (%) | 74 (15.6) |
| Complication | |
| General, n (%) | 17 (3.6) |
| Craniospinal, n (%) | 45 (9.5) |
| Length of hospital stay, median (IQR) | 6 (3–14) |
| 30-day mortality, n (%) | 8 (1.7) |
SD: standard deviation; IQR: interquartile range; n: number.
Fig. 1.
Weekly timeline showing the number of procedures (orange line) and COVID-19 swabs performed for our patients (yellow bar), in comparison with the number of COVID-19 cases diagnosed in Saudi Arabia (green line). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article).
Complications were reported as two separate categories: general and craniospinal. General and craniospinal complications were reported in 17 (3.6 %) and 45 (9.5 %) patients, respectively. Further, 30-day mortality was reported in 8 patients (1.7 %) and the median number of days for the length of hospital stay was 6 days (IQR 3–14).
During the study period, 117 (24.7 %) patients underwent COVID-19 testing using nasopharyngeal swabs. Only three patients who underwent surgical intervention tested positive for COVID-19 swab while the remaining patients were either negative or did not exhibit clinical signs associated with COVID-19 in the perioperative period.
The number of procedures in the three consecutive periods was 209, 133, and 132, respectively. The median number of cases per day were significantly lesser in the latter two periods than in the first period (7; IQR: 4–13), (5; IQR: 3–6), and (5; IQR: 4–7), respectively (Table 2 ).
Table 2.
Comparison between study periods.
| Variable | Period 1 n = 209 |
Period 2 n = 133 |
Period 3 n = 132 |
P - Value |
|---|---|---|---|---|
| Procedures per day, median (IQR) | 7 (4–13) | 5 (3–6) | 5 (4–7) | 0.1 |
| Institution type | ||||
| Public, n (%) | 141 (67.5) | 90 (67.7) | 101 (76.5) | 0.16 |
| Private, n (%) | 68 (32.5) | 43 (32.3) | 31 (23.5) | |
| Diagnosis category | ||||
| Trauma, n (%) | 19 (9.1) | 16 (12) | 7 (5.3) | 0.15 |
| Oncology, n (%) | 53 (25.4) | 39 (29.3) | 37 (28) | 0.7 |
| Spine, n (%) | 41 (19.6) | 24 (18.1) | 24 (18.2) | 0.92 |
| Vascular, n (%) | 35 (16.8) | 16 (12) | 32 (24.2) | 0.03 |
| Congenital, n (%) | 11 (5.3) | 5 (3.8) | 3 (2.3) | 0.39 |
| Hydrocephalus, n (%) | 22 (10.53) | 24 (18.1) | 19 (14.4) | 0.14 |
| Peripheral Nerve, n (%) | 10 (4.8) | 1 (0.7) | 1 (0.7) | 0.02 |
| Functional, n (%) | 5 (2.4) | 0 | 1 (0.76) | 0.13 |
| Infections, n (%) | 13 (6.2) | 8 (6) | 8 (6) | 0.99 |
| Priority of the case | ||||
| Priority 1 (Immediate), n (%) | 31 (14.8) | 32 (24.1) | 26 (19.7) | 0.09 |
| Priority 1 (1−24 h), n (%) | 29 (13.9) | 30 (22.6) | 30 (22.7) | 0.05 |
| Priority 2 (1−7 d), n (%) | 62 (29.7) | 40 (30.1) | 44 (33.3) | 0.76 |
| Priority 3 (1−4 w), n (%) | 38 (18.2) | 18 (13.5) | 20 (15.2) | 0.5 |
| Priority 4 (>4 w), n (%) | 49 (23.4) | 13 (9.8) | 12 (9.1) | <0.001 |
| Complication | ||||
| General, n (%) | 8 (3.8) | 5 (3.8) | 4 (3) | 0.92 |
| Craniospinal, n (%) | 21 (10.1) | 15 (11.3) | 9 (6.8) | 0.43 |
| Length of hospital stay, median (IQR) | 7 (4–18) | 6 (3–13) | 5 (2–8) | 0.02 |
| 30-day mortality, n (%) | 2 (1) | 4 (3) | 2 (1.5) | 0.35 |
IQR: interquartile range; n: number.
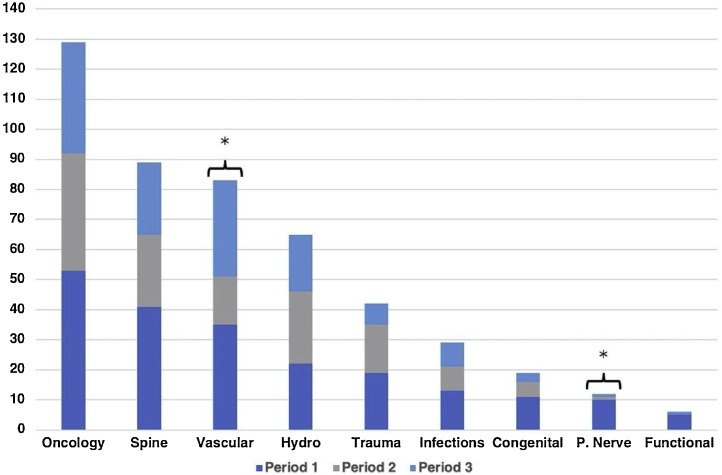
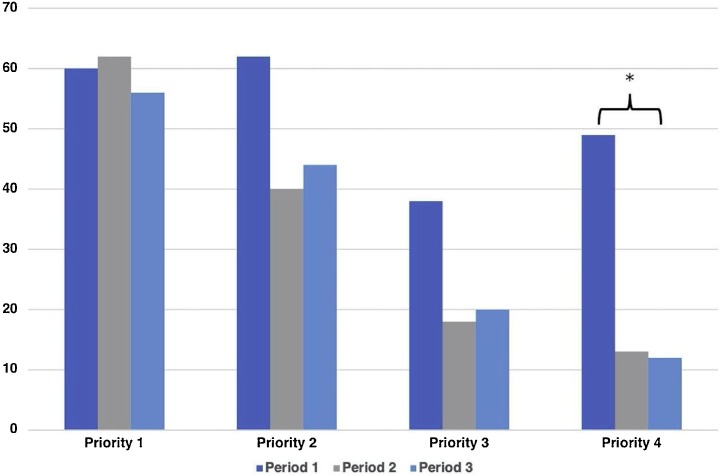
With regard to the category of cases, there were significant among-period differences in only the vascular and peripheral nerve cases (P-values 0.03 and 0.02, respectively) (Fig. 2 ). With regard to the intervention priority, there was a significant among-period difference in Priority 4 interventions, which declined from 49 (23.4 %) to 13 (9.8 %) and 12 (9.1 %) over the three periods (P-value < 0.001) (Fig. 3 ). There was a significant among-period difference in the length of hospital stay, which dropped from a median of 7 days (IQR: 4–18) to 6 (IQR: 3–13) and 5 days (IQR: 2–8). There was no significant among-period difference with respect to the institution type, complications, and mortality.
Fig. 2.
Case distribution according to the category during the three periods.
The asterisks indicate a significant reduction in the number of cases between the three periods.
Fig. 3.
Case distribution according to priority during the three periods.
The asterisks indicate a significant reduction in the number of cases between the three periods.
4. Discussion
The impact of the COVID-19 pandemic on neurosurgical practice in our region was similar to that reported in other regions [[10], [11], [12], [13], [14], [15], [16], [17]]. We recently compared 50 days during the early phase of the COVID-19 pandemic with a similar period in 2019 [9]. We found a 44 % reduction in the number of neurosurgical procedures performed during the COVID-19 pandemic compared to the previous year. Moreover, there was a significantly lower median number of procedures performed per day during the pandemic than during the same period in the previous year. In the previous study, we observed that the proportions of Priority 1 (immediate) and Priority 1 (1–24 h) cases were 82 % and 63 %, respectively, and these cases were more likely to occur during the pandemic period. On the other hand, Priority 4 cases were 72 % less likely to occur during the pandemic period than during the pre-pandemic period. In the present study, we assessed the longitudinal impact of COVID-19 on neurosurgical practice in Saudi Arabia during the early pandemic months. Our findings revealed a decrease in the number of operations performed throughout the study period, which was concomitant with the increased number of COVID-19 cases in Saudi Arabia, as shown in Fig. 1 [3].
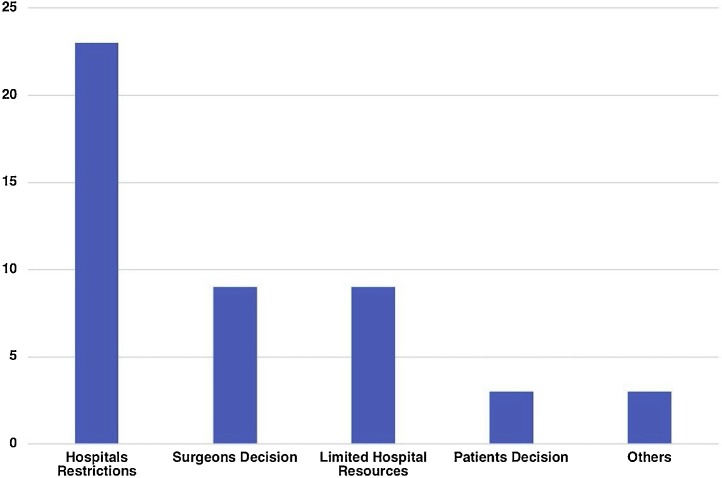
Decreased surgical load could be attributed to several factors. An internal survey sent on June 5, 2020, to participating surgeons for assessing the COVID-19 impact on the surgical workflow indicated that most neurosurgeons considered restrictions by internal hospital policies as the main factor (Fig. 4 ). Other factors that could have played a role included a personal decision to delay elective non-urgent operations to limit the risk of COVID-19 transmission between patients and health care workers. Some patients preferred delaying non-urgent procedures to avoid exposure and contracting the virus from the hospitals. Limited resources in some hospitals, including a decreased capacity of the surgical intensive care unit, which affected other aspects of health care delivery, could have contributed to our findings. However, during the study period, the health care system in Saudi Arabia was not severely affected by the pandemic.
Fig. 4.
Perceptions of participating surgeons about the causes underlying the decreased surgical load.
As shown in Fig. 1, the number of cases during the early weeks was higher than that during the subsequent weeks. Initially, there were 72 and 64 cases during the first two weeks, which subsequently dropped and plateaued to 30–40 during the following weeks. This occurred concomitantly with an increase in the number of COVID-19 confirmed cases in the country. During the study period, predominantly during and after period 2, we saw an increase in the number of screening tests to detect possible COVID-19 infections in patients scheduled for elective or emergency surgeries; 24.7 % of our cohort was tested for COVID-19 infection. Per the protocol, tested patients must meet the minimum risk assessment score instituted by the Ministry of Health guidelines [6] (e.g. shortness of breath, fever, cough, history of direct contact with a confirmed COVID-19 case), and patients who meet the criteria receive a nasopharyngeal swab test using real-time reverse transcription-polymerase chain reaction (RT-PCR) for the detection of COVID-19. In our series, three patients tested positive for COVID-19. A patient was transferred from a secondary hospital as a positive COVID-19 case requiring neurosurgical intervention. Two subsequent tests at a 3-day interval yielded negative results without showing any COVID-19 related symptoms. The second patient presented to the emergency department and underwent emergency decompressive craniectomy. Despite having no COVID-19-related symptoms, her preoperative screening test showed positive results. Postoperatively, she developed asymptomatic pulmonary embolism with no subsequent sequelae. The third patient, who underwent a Priority 2 spinal procedure, was swabbed after his procedure because of exposure to a COVID-19-positive case. The patient did not exhibit any clinical symptoms related to COVID-19, and he was discharged home after subsequent swabs yielded negative results. None of our participating neurosurgeons or treating team members contracted the disease from the positive cases.
Several measures have been proposed to limit the spread of COVID-19 infections during surgery [[18], [19], [20]]. All patients undergoing emergency procedures should be considered positive until proven otherwise, with development of a dedicated route from the emergency department to the operating room (OR) and the use of separate designated ORs. Use of negative pressure ORs is highly encouraged, particularly for aerosol-generating procedures such as intubation, extubation, and transnasal procedures. Limiting unnecessary staff and unnecessary movements in and out of ORs, along with ensuring that all staff wear proper PPE, including N95 masks, and appropriately dispose all PPE and OR attire, is mandatory. In addition, good communication between hospital teams is crucial for better safety control and risk minimization during any outbreak.
We found that oncology procedures were the most commonly performed throughout the three periods (Fig. 2). The majority of oncological procedures were performed for Priority 2 (61 [47.3 %]) cases, followed by Priority 3 (34 [26.4 %]), Priority 1 (24 [18.6 %]), and Priority 4 (10 [7.7 %]) cases. We observed that with progression of time, between periods, there was a decrease in priority 4 procedures and a shift towards more critical and urgent cases, priority 1 and 2, which reflects the high patients’ selection among surgeons as we advanced through the pandemic. The oncological procedures varied, although the majority were performed for tumors compressing the brain and causing acute focal neurological deficits, tumors causing hydrocephalus, or tumors causing high intracranial pressure. Vascular procedures were the third most common, which could be attributed to their urgency, including ruptured aneurysms, hemorrhagic strokes, or malignant vascular strokes, which cause a mass effect. There was a decreased number of vascular procedures during the second study period, which was mainly attributed to more hospital restrictions in accepting referred cases among leading vascular centers due to increased COVID-19 cases. Khalafallah et al. [16] assessed the COVID-19 impact on their neurosurgery department. With regard to the impact on operative workflow, there was a decrease in operative volumes from 360 cases in April 2019 to 112 projected total cases in April 2020. Cancellation of operative cases varied by subspecialty with spine procedures being the most affected, followed by tumor, vascular, functional, and pediatric surgeries. Contrastingly, there was a non-significant trend of a decrease in trauma cases.
With regard to the trauma cases, there was a decreased number of cases performed throughout the three periods. This is consistent with previous reports, which could be explained by reduced road traffic accidents from the strict curfew imposed by the governments [16,21]. Priority 1 (immediate and 1−24 h) cases were persistently high throughout periods 1, 2, and 3 (28.7 %, 46.7 %, and 42.4 %, respectively) (Fig. 3). On the other hand, Priority 4 cases decreased significantly during the three periods, which is consistent with the decrease in the absolute number of cases performed during the period and the increase in the COVID-19 cases, leading to more restrictions in healthcare facilities. Manusubroto et al. divided the COVID-19 pandemic into four phases, and they were in phase 2 at the time of publication of their report. Consistent with our findings, they reported a decrease in elective procedures in their center from an average of 16 elective operations per week during phase 1, when there were confirmed cases in Indonesia but none in Yogyakarta, to an average of 9 cases per week during phase 2, which is the period between the time of initial detection of the outbreak in Yogyakarta and the time when their government relaxed the strict outbreak-related regulations. This was associated with hospital restrictions regarding intensive care unit beds for postoperative neurosurgical patients and reduced the availability of personal protective equipment in their hospital [21].
We saw a persistently high number of Priority 1 (immediate and 1–24 h) cases during the study period. A few factors may have contributed to this finding, including the establishment of a new emergency hotline by the Ministry of Health, with allocation of medical staff and physicians to receive calls from patients and their families. Patients either received medical advice over the phone or received further medical evaluations after getting permits through a phone application during the curfew hours, which allowed them to reach the hospitals efficiently. Such factors may have played a role in maintaining the number of emergency procedures during the pandemic.
With regard to complication rates, 13.1 % of our patients presented with either general or craniospinal complications. This rate is close to the 14.3 % complication rate reported by an analysis of a large database from the American College of Surgeons, which included >38,000 procedures from hundreds of US hospitals [22]. However, the complication rate could be higher for COVID-19 positive patients undergoing surgical procedures. A retrospective analysis of 34 COVID-19 positive cases who underwent elective surgical procedures during the disease incubation period reported that all patients developed COVID-19 pneumonia soon after surgery, 15 (44.1 %) required ICU admission, and 7 (20.5 %) patients died. These data suggest that surgical procedures could exacerbate COVID-19 disease progression [23]. We found that the median length of hospital stay decreased from 7 days in period 1–5 days in period 3 (p = 0.02). This finding could be attributed to enhanced efficiency in assessing in-hospital patients for discharge planning to allow better resource utilization during the pandemic period.
Another important issue is the burden of patients on waiting lists for elective procedures, as well as difficulty in accessing emergency departments and outpatient visits. A previous study [24] reported that 3 patients admitted to an emergency department in 1 week presented with complications associated with delayed seeking of healthcare advice or misinterpretation of the complaint as being COVID-19 related. Delaying early interventions could negatively affect patients and exert long-term consequences, especially in patients with cancer. Several measures have been suggested to guide cancer treatment, including designating cancer surgeries as essential and of high priority surgeries, transferring patients with cancer to less overwhelmed institutions, high-level guidance for prioritizing cancer surgeries if delaying is essential, and concrete planning for performing delayed surgeries in a reasonable time period [25]. Our study demonstrated no change in the safety profile for both patients and healthcare workers throughout the study period. Therefore, we suggest that optimal resource utilization and continuation of essential neurosurgical procedures could benefit patients requiring time-sensitive intervention for certain pathologies before the healthcare system is overwhelmed and “life-or-limb” procedures dominate the practice. In a study published in the United States, an algorithmic approach based on institutional and local community volume surges of COVID-19 cases was set, aiming for better resource distribution to meet the outbreak need as well as provision of care for neurosurgical patients [26]. The surge levels were categorized into four types according to the cases in the community, positive inpatients, and staff shortage; “green” reflected a light load of COVID-19 infections in the community and institutes, while “black” represented the highest level warranting postponement of all elective cases and outpatients visits until settlement of the surge. This, along with individualized patient selection procedures, could be an acceptable and dynamic approach for institutes providing neurosurgical services during the pandemic.
This study has several limitations. First, we did not evaluate the impact of the COVID-19 pandemic on other neurosurgical services, including outpatient clinic care, inpatient care, or the effects on the workforce. Second, we did not assess the COVID-19 pandemic impact on neurosurgical patients on waiting lists for elective or semi-elective procedures, which could improve further strategic planning for optimal patient care. Lastly, our cohort is not representative of patients with COVID-19. Further studies are needed to address these issues.
5. Conclusion
This study evaluated the longitudinal effect of COVID-19 pandemic on neurosurgery practice. The number of neurosurgical procedures per week decreased in the early pandemic period and then plateaued. Although our health care system was not significantly affected, the pandemic impact on the neurosurgical practice is apparent. The load of emergency neurosurgery procedures remained unchanged throughout the three periods while that of unurgent elective cases significantly declined. This reflects the need to designate ample resources to cater for emergencies. Our findings could contribute toward developing a long-term strategy for surgical services during pandemics. We recommend to restart performing neurosurgical procedures once the pandemic gets stabilized to avoid a possible post-pandemic intolerable overload on the healthcare system.
Funding sources
This work was supported by the Deanship of Scientific Research at King Saud University, Riyadh, Saudi Arabia through Researchers Supporting Project number (RSP-2020/245).
CRediT authorship contribution statement
Khalid Bajunaid: Conceptualization, Methodology, Formal analysis, Resources, Data curation, Writing - original draft, Writing - review & editing, Visualization, Project administration. Abdullah Alatar: Methodology, Resources, Data curation, Writing - original draft, Writing - review & editing, Visualization, Project administration. Ashwag Alqurashi: Methodology, Validation, Resources, Data curation, Writing - original draft, Writing - review & editing, Visualization, Project administration. Mohammad Alkutbi: Validation, Resources, Data curation, Writing - review & editing. Anas H. Alzahrani: Formal analysis, Data curation, Writing - original draft, Writing - review & editing. Abdulrahman J. Sabbagh: Conceptualization, Data curation, Writing - review & editing. Abdullah Alobaid: Conceptualization, Data curation, Writing - review & editing. Abdulwahed Barnawi: Conceptualization, Data curation, Writing - review & editing. Ahmed A. Alferayan: Data curation, Writing - review & editing. Ahmed M. Alkhani: Conceptualization, Data curation, Writing - review & editing. Ali Bin Salamah: Conceptualization, Data curation, Writing - review & editing. Bassem Y. Sheikh: Data curation, Writing - review & editing. Fahad E. Alotaibi: Data curation, Writing - review & editing. Faisal Alabbas: Data curation, Writing - review & editing. Faisal Farrash: Data curation, Writing - review & editing. Hosam M. Al-Jehani: Conceptualization, Data curation, Writing - review & editing. Husam Alhabib: Conceptualization, Data curation, Writing - review & editing. Ibrahim Alnaami: Conceptualization, Data curation, Writing - review & editing. Ikhlass Altweijri: Data curation, Writing - review & editing. Isam Khoja: Data curation, Writing - review & editing. Mahmoud Taha: Data curation, Writing - review & editing. Moajeb Alzahrani: Data curation, Writing - review & editing. Mohammed S Bafaquh: Conceptualization, Data curation, Writing - review & editing. Mohammed Binmahfoodh: Conceptualization, Data curation, Writing - review & editing. Mubarak A. Algahtany: Data curation, Writing - review & editing. Sabah Al-Rashed: Data curation, Writing - review & editing. Syed M. Raza: Data curation, Writing - review & editing. Sherif Elwatidy: Data curation, Writing - review & editing. Soha A. Alomar: Data curation, Writing - review & editing. Wisam Al-Issawi: Data curation, Writing - review & editing. Yahya H. Khormi: Conceptualization, Data curation, Writing - review & editing. Ahmad Ammar: Supervision, Data curation, Writing - review & editing. Amro Al-Habib: Supervision, Conceptualization, Data curation, Writing - review & editing. Saleh S. Baeesa: Supervision, Conceptualization, Data curation, Writing - review & editing. Abdulrazag Ajlan: Conceptualization, Methodology, Resources, Data curation, Writing - original draft, Writing - review & editing, Visualization, Supervision, Project administration.
Declaration of Competing Interest
The authors report no declarations of interest.
Acknowledgements
The authors extend their appreciation to the Deanship of Scientific Research at King Saud University, Riyadh, Saudi Arabia for funding this work through Researchers Supporting Project number (RSP-2020/245).
References
- 1.(WHO) WHO . World Health Organization; 2020. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19 - 11 March 2020. [Google Scholar]
- 2.(WHO) WHO . 2020. Coronavirus Disease (COVID-19) Situation Report – 133. [Google Scholar]
- 3.(MOH) MoH . 2020. COVID 19 Dashboard: Saudi Arabia. [Google Scholar]
- 4.Algaissi A.A., Alharbi N.K., Hassanain M., Hashem A.M. Preparedness and response to COVID-19 in Saudi Arabia: building on MERS experience. J. Infect. Public Health. 2020;13(6):834–838. doi: 10.1016/j.jiph.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meo S.A. COVID-19 pandemic: Saudi Arabia’s role at national and international levels. J. Diabetes Sci. Technol. 2020 doi: 10.1177/1932296820930068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.(MOH) MoH . 2020. COVID-19 Coronavirus Guidelines. [Google Scholar]
- 7.(SPSC) SPSC . 2020. COVID-19 Safety Guide for Healthcare Professionals. [Google Scholar]
- 8.Bajunaid K., Sabbagh A.J., Ajlan A., et al. Consensus statement of the Saudi association of neurological surgery (SANS) on triage of neurosurgery patients during COVID-19 pandemic in Saudi Arabia. Neurosciences (Riyadh). 2020;25(2):148–151. doi: 10.17712/nsj.2020.2.20200054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bajunaid K., Alqurashi A., Alatar A., et al. Neurosurgical procedures and safety during the COVID-19 pandemic: a case-control multi-center study. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.07.093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bernucci C., Brembilla C., Veiceschi P. Effects of the COVID-19 outbreak in Northern Italy: perspectives from the bergamo neurosurgery department. World Neurosurg. 2020;137:465–468. doi: 10.1016/j.wneu.2020.03.179. e461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jose Antonio S.S., Tito P., Marcelo Z., et al. Early report on the impact of Covid-19 outbreak in neurosurgical practice among members of the Latin American federation of neurosurgical societies. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.04.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jean W.C., Ironside N.T., Sack K.D., Felbaum D.R., Syed H.R. The impact of COVID-19 on neurosurgeons and the strategy for triaging non-emergent operations: a global neurosurgery study. Acta Neurochir (Wien). 2020;162(6):1229–1240. doi: 10.1007/s00701-020-04342-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fontanella M.M., De Maria L., Zanin L., et al. Neurosurgical practice during the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic: a worldwide survey. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.04.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.El-Ghandour N.M.F., Elsebaie E.H., Salem A.A., et al. Letter: the impact of the coronavirus (COVID-19) pandemic on neurosurgeons worldwide. Neurosurgery. 2020 doi: 10.1093/neuros/nyaa212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Antony J., James W.T., Neriamparambil A.J., Barot D.D., Withers T. An Australian response to the COVID-19 pandemic and its implications on the practice of neurosurgery. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.05.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khalafallah A.M., Jimenez A.E., Lee R.P., et al. Impact of COVID-19 on an academic neurosurgery department: the johns Hopkins experience. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.05.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Manusubroto W., Wicaksono A.S., Tamba D.A., et al. Neurosurgery services in Dr. Sardjito General Hospital, Yogyakarta, Indonesia, during COVID-19 pandemic: an experience from a developing country. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.05.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moletta L., Pierobon E.S., Capovilla G., et al. International guidelines and recommendations for surgery during Covid-19 pandemic: a systematic review. Int. J. Surg. 2020;79:180–188. doi: 10.1016/j.ijsu.2020.05.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Heffernan D.S., Evans H.L., Huston J.M., et al. Surgical infection society guidance for operative and peri-operative care of adult patients infected by the severe acute respiratory syndrome Coronavirus-2 (SARS-CoV-2) Surg Infect (Larchmt). 2020;21(4):301–308. doi: 10.1089/sur.2020.101. [DOI] [PubMed] [Google Scholar]
- 20.Reed L.K., Wen J., Liang B., Wang X., Feng D., Huang J.H. Safely performing neurosurgical procedures during COVID-19 pandemic. Neurol. Res. 2020:1–7. doi: 10.1080/01616412.2020.1781455. [DOI] [PubMed] [Google Scholar]
- 21.Manusubroto W., Wicaksono A.S., Tamba D.A., et al. Neurosurgery Services in Dr. Sardjito General Hospital, Yogyakarta, Indonesia, During the COVID-19 Pandemic: Experience from a Developing Country. World Neurosurg. 2020 doi: 10.1016/j.wneu.2020.05.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rolston J.D., Han S.J., Lau C.Y., Berger M.S., Parsa A.T. Frequency and predictors of complications in neurological surgery: national trends from 2006 to 2011. J. Neurosurg. 2014;120(3):736–745. doi: 10.3171/2013.10.JNS122419. [DOI] [PubMed] [Google Scholar]
- 23.Lei S., Jiang F., Su W., et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine. 2020 doi: 10.1016/j.eclinm.2020.100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tartara F., Cofano F., Zenga F., Boeris D., Garbossa D., Cenzato M. Are we forgetting non-COVID-19-related diseases during lockdown? Acta Neurochir (Wien). 2020;162(7):1501. doi: 10.1007/s00701-020-04385-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Finley C., Prashad A., Camuso N., et al. Guidance for management of cancer surgery during the COVID-19 pandemic. Can. J. Surg. 2020;63(22):S2–S4. doi: 10.1503/cjs.005620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burke J.F., Chan A.K., Mummaneni V., et al. Letter: The Coronavirus Disease 2019 Global Pandemic: A Neurosurgical Treatment Algorithm. Neurosurgery. 2020;87(1):E50–E56. doi: 10.1093/neuros/nyaa116. [DOI] [PMC free article] [PubMed] [Google Scholar]