Glossitis is an inflammation of the tongue. The inflammation can cause swelling, change of color (usually red or purple) and develop variable appearances on the surface of the tongue.
The causes include allergies (to food, medications, and oral care products), infection (Herpes simplex, bacteria, or yeast), injuries (from dentures or burns), irritants (tobacco, alcohol, and spices), immunologic disorders (such as Sjogren's syndrome, lichen planus), vitamin B deficiency (B2, B3, B6, and folate), and other miscellaneous disorders (glucagonoma, Whipple's disease, carcinoid syndrome, acquired immunodeficiency syndrome, sprue, and celiac disease).
There are various kinds of glossitis, including:
Atrophic glossitis (a smooth glossy tongue surface, caused by loss of papillae)
Median rhomboid glossitis (a depapillated region in the central area of tongue) caused by oral candidiasis
Geographic tongue due to patchy depapillation. This can appear to move, giving a changing map picture
Geometric glossitis in which there is a deep fissure in the middle of the tongue, with branches; this condition is usually seen in immunocompromised people (e.g., patients with leukemia
Strawberry tongue caused by hyperplastic fungiform papillae, associated with bacterial infections.
A review showed prevalence ranges of 0.1%–14.3% for geographic tongue, 1.3%–9.0% for atrophic glossitis, and 0.0%–3.35% for median rhomboid glossitis.1
Modern biomedical treatment involves oral hygiene; avoidance of spicy food, alcohol, tobacco and other irritants; treating the underlying causes; diet changes; and addressing nutritional and vitamin deficiencies.
Steroid ointments—such as Kenalog® in Orabase®—are effective for producing short-term benefits.
Glossitis in Chinese Medicine
In Chinese Medicine, the tongue is a window of the internal environment, and the pathology of the internal organs are usually reflected on the tongue. In a patient with glossitis, the tongue is usually red and can be swollen. The representations of internal organs on the surface of the tongue are shown in Figure 1; the usual areas of color change according to the pathology of internal organs are shown in Figure 2.
FIG. 1.
Internal organ representation on the tongue.
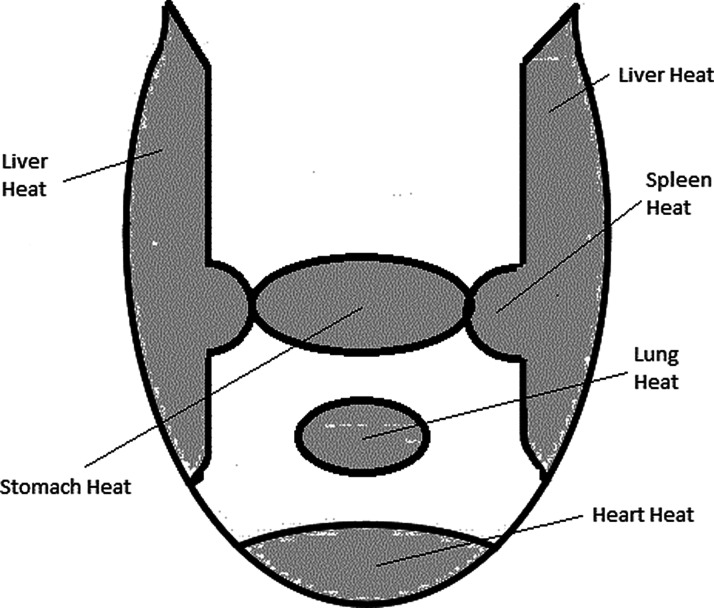
FIG. 2.
Specific areas of the tongue that indicate organ Heat.
A red tongue almost always indicates Heat/Fire (Fire is extreme Heat); if the whole tongue is red and the tip is more red, this is generalized Heat and severe Heart Heat. Red sides along the edges of the tongue indicate Liver Heat. Redness confined to the central section of the edge of the tongue indicates Spleen Heat. Redness just proximal to the tip of the tongue is Lung Heat. Redness in the middle section of the tongue indicates Stomach Heat. Red points on the tongue indicate severe Heat. A Purple tongue almost always indicates Blood Stasis. It takes a long time for the Stasis to give the tongue a purple color, and, hence, this is more common in the elderly. The commonest area where purple discoloration occurs is in the Liver area, which indicates Blood Stasis in any organ affected by the Liver Meridian. Hence, Stasis in the Ovary/Uterus, is usually reflected in the Liver area. Blood Stasis in the Breast, Lung, and Heart is usually seen in the chest area behind the tip of the tongue.
Swelling of the tongue is caused by Stagnation of fluid transport, which is Dampness. As internal fluid transport is a function of the Spleen, swelling of the tongue is caused by Spleen Deficiency. As the fluid Stagnation becomes chronic, the fluid condenses to form Phlegm. In both of these conditions the tongue is swollen. The differentiation is determined according to the appearance of the tongue coating. In Dampness, the coating is smooth and slippery; in Phlegm, the coating is rough and sticky.
Treatment
A popular textbook of clinical acupuncture recommended that the following points be used to treat patients who have glossitis: GV 20; GV 28; Jinjin; Yuye Extra Points; LI 4; LI 11; GV 14; and SP 10.2 The current author has used these points and found them effective for treating acute glossitis. In chronic glossitis due to the pathology of the internal organs, these points provide temporary relief but the problem returns. This is similar to the temporary relief obtained from steroid ointments. To achieve lasting benefit, the underlying pathology has to be targeted and the details for this are given in Table 1.
Table 1.
Signs, Symptoms, & Treatment of Disorders Manifesting with Glossitis
| Pathology | Signs/symptoms | Tongue | Pulse | Treatment |
|---|---|---|---|---|
| Heart Heat/Fire |
Palpitations, thirst, red tongue with ulcers | Red tip, yellow coating, midline crack reaching to the tip | Full rapid mainly in left front position, can be irregular | LI 11 (clears Heat in general). HT 7, HT 8, HT 9 (clears Heart Heat). All points reduced; reinforce SP 6 & KI 6 to lift Yin. Chinese herbs: Xie Xin Tang, Draining the Heart Decoction. |
| Heart Blood Stasis |
Stabbing pain in the chest, palpitations, cyanosis of lips | Purple all over or only in the chest area | Choppy, knotted, can be wiry | PC 6, PC 4, HT 7, CV 17 (Front Mu point of Pericardium), BL 14 (Back Shu point of Heart), BL 17 (Influential point for Blood), SP 10 (Moves Blood), KI 25 (Moves Blood in the chest); all points reduced. Chinese herbs: Xue Fu Zhu Yu Tang (Blood Mansion Eliminating Stasis decoction). |
| Liver Fire |
Headache, irritability, red face, red eyes | Red tongue with redder sides, dry yellow coating | Full wiry, rapid | LI 11 (clears Heat), LR 1, LR 2, LR 3 (clear Liver Heat); GB 20, GB 13, GB 1, GB 8, GB 9, Taiyang, GB 6 (clear headache); all points reduced. Chinese herbs: Long Dan Xie Gan Tang (Gentiana Draining the Liver Decoction) |
| Liver Blood Stasis | Hypochondrial stabbing pain, menstrual blood dark & clotted, purple dark complexion, petechiae | Purple, generally or only on the sides, purple spots | Wiry | SP 4 + PC 6, in that order, opens the Penetrating Vessel, which is the Sea of Blood, to eliminate Blood Stasis; GB 34, LR 3, BL 18 (Back Shu point of the Liver), LR 5, LR 6 (move Blood & reduce Stagnation), BL 17 (Gathering point for Blood), SP 10 + BL 17 (Move the Blood); all points reduced. Chinese herbs: Ge Xia Zhu Yu Tang (Eliminating the Stasis Below the Diaphragm Decoction. |
| Damp Heat in the Liver | Fullness in the hypochondrium, nausea, bitter sticky taste | Red with redder sides, sticky yellow coating | Slippery, rapid | LI 11 (resolves Heat in general), LR 2 (clears Liver Heat), GB 34, LR 14, BL 18 (Back Shu point of the Liver), CV 12, SP 9, SP 6 (resolve Dampness in the Liver); all points reduced except CV 12, which is reinforced. Chinese herbs: Long Dan Xie Gan Tang (Gentiana Draining the Liver Decoction) |
| Lung Heat | Cough with feeling of heat, red face, thirst | Red with yellow coating | Rapid | LI 11 (clears Heat in general), LU 5, LU 10, LU 7, LU 1 + BL 13 (Back Shu point of the Lung); all clear Lung Heat; all points reduced. Chinese herbs: Ma Xing Shi Gan Tang (Ephedra Prunus Gypsum Glycyrrhiza Decoction. |
| Damp Heat Invading the Spleen | Fullness in epigastrium, feeling of heaviness, loose stools, scanty dark urine, bitter taste | Red with sticky yellow coating | Slippery, rapid | SP 6, SP 9, GV 9, LI 11, GB 34, CV 9, CV11, ST 22, ST 28, BL 22 (Back Shu point of the Triple Burner channel); all reduce Damp Heat; BL 20 (Back Shu point of Spleen); all points reduced, except BL 20, which is reinforced. Chinese herbs: Lian Po Yin (Captis Magnolia Decoction). |
| Stomach Fire | Burning pain in epigastrium, thirst with desire to drink cold liquids, dry mouth, mouth ulcers, bleeding gums | Red in the center with thick yellow coating | Rapid | ST 44, ST 34, ST 21, LI 4, CV 12, CV 13, CV 11; all clear Stomach Heat; LI 11 clears general Heat; all points reduced, except CV 12, CV 13, where even method is used. Chinese herbs: Qing Wei San (Clearing the Stomach Powder) |
| Damp Heat in the Stomach | Epigastric fullness, feeling of heaviness in epigastrium, sticky taste, thirst without desire to drink water, facial pain, sinusitis | Red with sticky yellow coating | Slippery, rapid | Same points as in Stomach Fire with addition of ST 40, SP 9, CV 9, which are reduced. These points reduce dampness. Chinese herbs: Lian Po Yin (Captis Magnolia Decoction). |
| Stomach Blood Stasis | Stabbing pain in the epigastrium, “coffee ground” vomiting | Purple | Wiry | SP 4 + PC 6 in that order to open Penetrating Vessel which is the Sea of Blood; KI 21 (stimulates Penetrating Vessel further); ST 34, ST 21, ST 19, ST 40 to restore Descending of Stomach Qi; GB 34 + CV 12 to move Qi in the Middle Burner; all points reduced. Chinese herbs: Ge Xia Zhu Yu Tang (Eliminating Stasis Below the Diaphragm). |
| Less common patterns | ||||
| Small Intestine Heat | Abdominal pain; tongue ulcers; scanty, dark painful urination; painful micturition due to axis relationship between the Urinary Bladder and Small Intestine | Tongue is red with redder tip; red tip of the tongue due to Yin/Yang relationship between Small Intestine & Heart | Full, rapid | Reduce SI 2, SI 5 (clear Small Intestine Heat), ST 39 (Lower Sea point of Small Intestine) for abdominal pain, HT 5 + HT 8 to drain Heart Fire. Chinese herbs: Dao Chi Qing Xin Tang (eliminating redness and clearing the Heart Decoction). |
| Damp Heat in Large Intestine | Abdominal pain, diarrhea with mucus & blood | Red tongue | Full, rapid | Reduce ST 25 (Front Mu point of Large Intestine), BL 25 (Back Shu point of Large Intestine), SP 9, SP 6, CV 3, BL 22, CV 6 (resolve Dampness from Lower Burner). Chinese herbs: Bai Tou Weng Tang (Pulsatilla Decoction). |
The fundamental basis of acupuncture treatment for pain and swelling of the tongue was discussed by Sun.3
There are not many studies showing the effectiveness of acupuncture for treating glossitis. Noh et al. reported positive effects of acupuncture in 5 cases of glossitis.4
Illustrative Case
A 77-year-old man presented with glossitis of 3 months' duration. He complained of burning in his epigastrium, excessive hunger, mouth ulcers, and a feeling of heat. There was generalized redness over his tongue, with patches of papillary loss (a geographic tongue) and scattered areas of purple discoloration. The redness and burning sensation were more in the Stomach area of his tongue. The tongue coating was slightly yellow. A diagnosis of Stomach Fire leading to early Blood Stagnation in the Stomach was made.
This patient was treated with acupuncture, only using GV 20, GV 28, Jinjin, Yuye, LI 1, LI 11, GV 14 and SP 10 for symptomatic relief (4 treatments), followed by SP 4 left and PC 6 right to open the Penetrating Vessel to address Blood Stagnation; LI 11 to reduce general Heat; ST 44, ST 21, ST 34, and LI 4 to reduce Stomach Heat, all using the reduction method; and CV 12 and CV 13 were stimulated using the even method to subdue the Rebellious Stomach Qi. These points addressed the pathology of this patient's condition.
Treatment was given on alternate days for 4 weeks, followed by twice per week treatment for 3 weeks. This resulted in significant improvement (80%–85%) reduction of symptoms.
Further improvement was not forthcoming. On further questioning, he reported consuming sizable amounts of cashew nuts every day. This was stopped, and his recovery was near complete.
This case illustrates the fact that the points for symptomatic relief that can be used in all cases often provide only temporary results and the pathology persists. The points addressing the pathology often provide long-term relief, but the ultimate cure is obtained only after the causative factor is removed.
Some cases can be extremely resistant to treatment, especially those associated with lichen planus.
Address correspondence to:
Poovadan Sudhakaran, MBBS, PhD
MastACU, MastTCM
26 Tuckers Road
Templestowe, 3106
Australia
Email: dr.p.sudhakaran@gmail.com
References
- 1. Dombi C, Czegledy A. Incidence of tongue diseases based on epidemiologic studies [review of the literature; in Hungarian]. Fogorv SZ. 1992;85(II):335–341 [PubMed] [Google Scholar]
- 2. Jayasuriya A. Disorders of the gastrointestinal system. In: Clinical Acupuncture, 2nd ed. New Delhi: B. Jain Publishers; 2002:525–540 [Google Scholar]
- 3. Sun P. Tongue pain. In: Management of Postoperative Pain with Acupuncture, 1st ed. London: Churchill Livingstone; 2007:113–117 [Google Scholar]
- 4. Noh MH, Park SG, Park HJ, Jung HM, Kim JW, et al. Glossitis treated with acupuncture. J Korean Med Ophthalmol Otolaryngol Dermatol. 2016;29(3)197–207 [Google Scholar]