Abstract
Background:
As resources are overwhelmed with the coronavirus disease 2019 pandemic, multiple approaches to produce individualized split-ventilator designs have emerged. These designs attempt to address the significant limitations and safety concerns of coventilation practices by allowing practitioners to adjust pressure settings for individual patients connected with specialized circuits to a single ventilator. The critical component in virtually all individualized circuit designs is the adjustable inline positive end-expiratory pressure valve.
Methods:
We reviewed the literature on the mechanics of inline positive end-expiratory pressure valve function, the implications and considerations for advanced application of inline positive end-expiratory pressure valves in individualized circuits, available methods of adapting commercial positive end-expiratory pressure valves in the resource-restricted setting, and major caveats of the use of inline positive end-expiratory pressure valves.
Results and Conclusions:
The function of adjustable inline positive end-expiratory pressure valves in advanced individualized ventilator circuits has not been described. Adjustable inline positive end-expiratory pressure valves are critical to individualized circuit reliability and patient safety when attempting to extend ventilator capacity in the setting of extreme ventilator shortages. Adjustable inline positive end-expiratory pressure valves provide a means to reduce delivered peak inspiratory pressure to an individual patient circuit, a method to increase positive end-expiratory pressure for an individual patient circuit, and act as an one-way valve to ensure unidirectional gas flow through the divided circuit. Adjustable inline positive end-expiratory pressure valves can be adapted from commercial valves or printed de novo when commercial options are unavailable. Noncommercial sourcing of ventilator components should only be considered in the setting of extreme ventilator shortages under the supervision of a knowledgeable anesthesiologist or intensivist.
Keywords: artificial respiration, coronavirus disease 2019, mechanical ventilation, positive end-expiratory pressure, ventilator
As resources are overwhelmed with the coronavirus disease 2019 pandemic and ventilator shortages occur or are envisioned, health systems have been scrambling for methods of increasing ventilator capacity. One solution that has been proposed is to share ventilators between multiple patients. Although so-called “co-ventilation” strategies have been used in New York (1) and have received crisis approval by Health and Human Services and the Federal Drug Administration (2, 3), there are major potential risks with such approaches, and major medical organizations have made statements against their use (4). To address these limitations, several international working groups have designed modified ventilator circuits which permit individualized settings for patients sharing a ventilator (5–7). These modified systems, also known as differential multiventilation (DMV), use flow restrictors and sensors to allow discrete adjustment and monitoring of inspiratory and expiratory variables (an example system is shown in Fig. 1)
Figure 1.
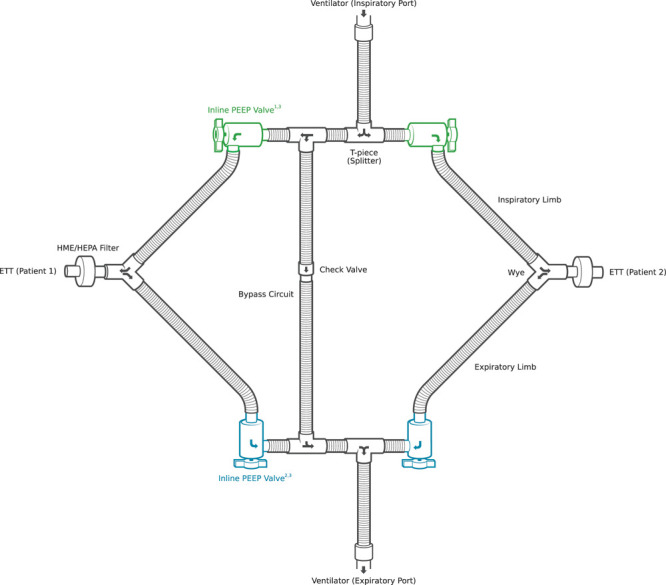
Differential multiventilation (DMV). An example of a simplified DMV circuit with the four inline positive end-expiratory pressure (PEEP) valves highlighted. The most fundamental component for these improved multiventilation systems is the inline PEEP valve. In DMV setups, inline PEEP valves serve the following three key functions: 1) reduce delivered inspiratory pressure to an individual patient circuit, 2) increase end-expiratory pressure for an individual patient circuit, and 3) act as an one-way valve to ensure unidirectional gas flow through the divided circuit. While the monitoring components have been omitted for visual clarity in the figure, DMV systems should use individual sensors and monitoring equipment whenever possible to ensure patients are receiving adequate oxygenation and ventilation. Appropriate monitoring options include pressure manometry, flow sensors, end-tidal Co2 monitors, and noninvasive cardiac output monitors (6). ETT = endotracheal tube, HEPA = high-efficiency particulate air filter, HME = heat and moisture exchanger.
Most DMV systems use variations on a fundamental approach to solving the challenges associated with split-ventilators: First, because patient triggering of the ventilator could lead to over-ventilation of one or both patients and potentially dangerous patient-patient-ventilator interactions, all patients must be passively ventilated. Adequate sedation and, if necessary, paralytics are used to prevent one or more patients from triggering breaths. Second, the ventilator must be in a pressure control mode. Using a pressure-regulated ventilator mode prevents the situation where a single patient receives the tidal volume intended for two or more patients if a circuit or patient obstructs. As a secondary benefit, pressure-based modes also facilitate the individualization process since pressure is easier to mechanically regulate than volume. Third, patient ventilation variables are individually monitored using digital or mechanical pressure manometry, flow sensors, end-tidal Co2 monitors, and/or noninvasive cardiac output monitors (6). Finally, valves and flow restrictors are used in each patient’s circuit to individualize ventilator variables. Although many flow restrictors have been described, most DMV systems use adjustable inline positive end-expiratory pressure (PEEP) valves in at least some part of the system (Fig. 1). Inline PEEP valves serve three key functions in DMV systems: 1) reducing delivered peak inspiratory pressure (PIP) to an individual patient circuit (flow restrictor), 2) increasing PEEP for an individual patient circuit (pressure release valve), 3) acting as one-way valves to ensure unidirectional gas flow through the divided circuit (check valve).
BASIC FUNCTION OF THE ADJUSTABLE PEEP VALVE
PEEP valves are adjustable pressure release valves. They are commonly used in conjunction with bag valve masks (BVMs) and normally vent exhaled gases to the atmosphere. When the prevalve pressure exceeds the valve setpoint, a diaphragm opens and allows flow. When prevalve pressure drops below the valve setpoint, the diaphragm closes and flow across the valve stops. Inline PEEP valves additionally function as one-way or check valves in that backward flow is prevented by the closed diaphragm.
Typical PEEP valve function depends on a valve that is closed by a spring (illustrated in Fig. 2). The spring can be manually tensioned to apply a set amount of pressure (e.g. 5 cm H2O). At atmospheric pressures, the valve stays closed, and pressure accumulates below the valve when the prevalve pressure is less than the pressure exerted by the tensioned spring. When the prevalve pressure accumulates to the point of greater pressure than the tensioned spring exerts, the valve opens, and gas is vented until the prevalve gas pressure is again below the setpoint (Fig. 2A).
Figure 2.
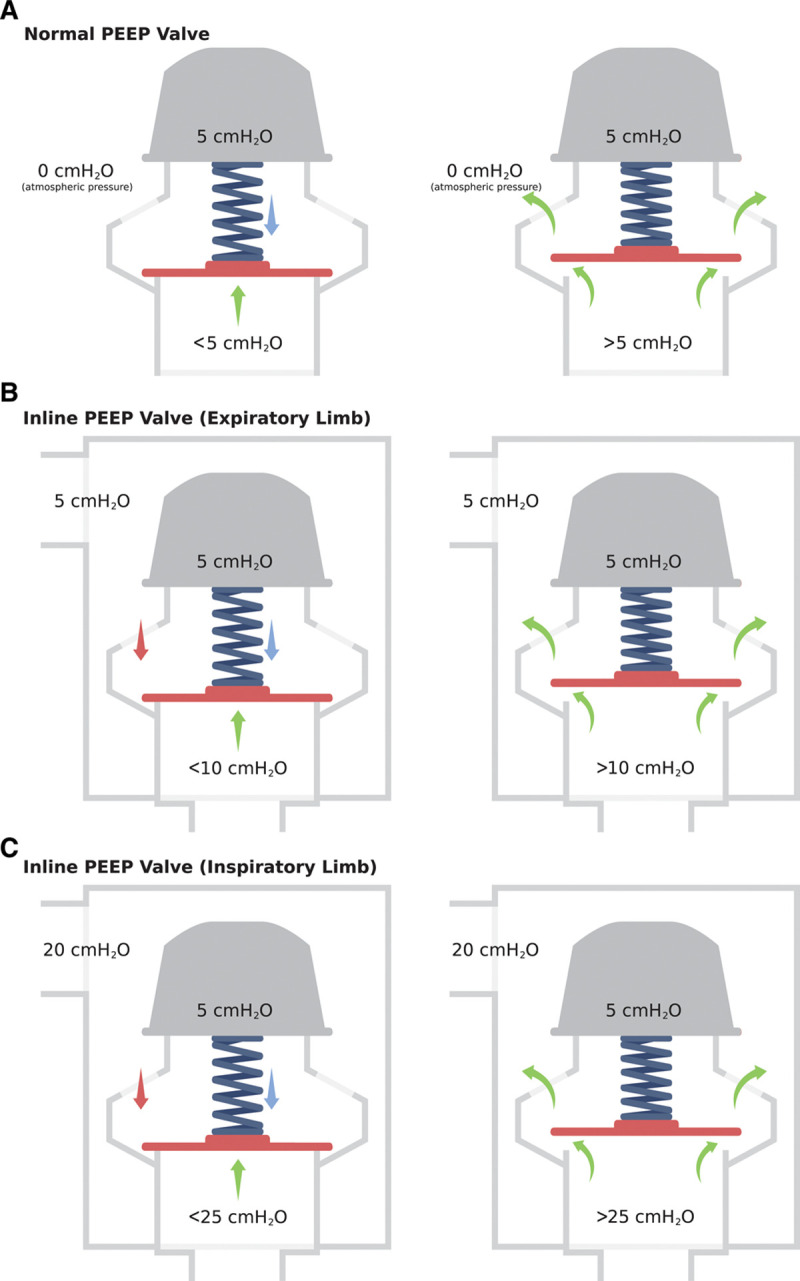
Function and behavior of positive end-expiratory pressure (PEEP) valves in different settings. In situation (A), prevalve gas is vented to the environment when the prevalve pressure exceeds the PEEP valve setpoint. In the case of an inline PEEP valve (B and C), prevalve gas is vented to the postvalve circuit when the prevalve pressure exceeds the combined resistance of the spring tension, and the postvalve gas pressure. When used in the expiratory circuit (situation B), inline PEEP valve pressure is additive to ventilator PEEP (PEEPvent) (PEEPpatient = PEEPvent + valve setpoint). When used in the inspiratory circuit (situation C), the inline “PEEP” valve setting is subtractive to the delivered ventilator pressure (PIPpatient = PIPvent – valve setpoint). PIP = peak inspiratory pressure, PIPvent = ventilator PIP.
When PEEP valves are placed in an inline enclosure (Fig. 2, B and C), the valve may now function at pressures other than local atmospheric pressure. In this setting, the setpoint of the PEEP valve becomes the sum of the pressure exerted by the spring and the pressure exerted by the gas pressure in the postvalve compartment of the enclosure. The valve will now open only when the prevalve pressure is greater than the sum of both the pressure the spring is tensioned to and the postvalve gas pressure.
ADJUSTABLE INLINE PEEP VALVES AS PRESSURE RELEASE VALVES
When an inline PEEP valve is placed into the expiratory limb of a DMV circuit (Fig. 2B), the gas entering the enclosure is expiratory flow from the patient, and postvalve gas pressure is regulated by the ventilator. Since postvalve gas pressure reflects the PEEP set on the ventilator, the additional resistance to flow out of the individual expiratory circuit by the spring represents additional PEEP above the PEEP set by the ventilator. Therefore, the inline PEEP valve setting in the expiratory circuit is additive to the ventilator PEEP (i.e. total PEEP is 10 cm H2O in a circuit when the inline PEEP valve is set to 5 cm H2O and the ventilator is set to maintain a PEEP of 5 cm H2O).
ADJUSTABLE INLINE PEEP VALVES AS FLOW RESTRICTORS
In contrast to the expiratory limb, use of inline “PEEP” valves in the inspiratory limb of DMV circuit results in different behavior (Fig. 2C). The gas entering the inlet of the enclosure is inspiratory flow from the ventilator, and the valve resists this flow with the tension in the spring. Prevalve gas pressure reflects the PIP set on the ventilator, and the inline valve is tensioned with the requisite pressure drop needed to achieve the prescribed PIP for the individual patient (PIPpatient). At the beginning of the inspiratory phase, pressure in the individualized circuit should always be lower than the pressure delivered by the ventilator (PIPvent). Therefore, the valve will permit gas entry until the desired PIPpatient is achieved. At this point, the postvalve gas pressure combined with the spring tension will equal or exceed the prevalve pressure, and the valve will close. In this way, the inline “PEEP” valve setting in the inspiratory circuit is subtractive to the ventilator PIP (i.e., net PIPpatient is 20 cm H2O in a circuit when the inspiratory inline valve is set to 5 cm H2O, and the ventilator is set to deliver a PIPvent of 25 cm H2O).
In contrast to the behavior of inline “PEEP” valves in the inspiratory circuit, most other types of flow restrictors that have been described for use in DMV systems provide much less predictable performance characteristics. For example, flow restrictors such as ball valves or pin valves rely on a variable constriction to create a flow limitation. This approach results in a consistent pressure drop only as long as the inspiratory time (Itime) remains constant. When the inspiration/expiration ratio is changed such that the Itime is prolonged, the pressure in the postvalve circuit has more time to equalize with the prevalve pressure and can increase despite no change in the valve setting. In addition to the Itime-dependant behavior, most valves have nonlinear flow restriction. In ball valves, for example, initial rotation of the control lever results in negligible changes in flow because the threshold constriction size has not been met. As the lever is further rotated and significant constriction occurs, smaller and smaller rotations of the lever result in larger and larger reductions in flow. Finally, ball valves and pin valves lack numerical settings in meaningful units, making reproduction or prediction of a required setting difficult. In contrast, adjustable inline PEEP valves do not suffer from these major drawbacks in DMV systems: PEEP valves demonstrate relatively time-independent behavior, near linear adjustable flow restriction, and do so with predictable numerical settings in the correct units (cm H2O).
CHECK VALVE FUNCTION OF INLINE PEEP VALVES
In its basic construction, the PEEP valve is a spring-loaded disc check valve. As soon as the pressure on the outlet combined with the spring force exceeds the inlet pressure, the membrane will close the valve and the flow will stop. This check valve behavior ensures unidirectional flow in the individual patient circuits preventing rebreathing of expiratory gas. In DMV systems, every limb of a circuit requires a check valve. Therefore, when inline PEEP valves are used in the inspiratory and expiratory limbs of patient circuits, regular check-valves are only required in the bypass circuit (Fig. 1).
EFFECTS OF INLINE PEEP VALVES ON VENTILATOR ALARMS
The use of inline PEEP valves should not significantly affect ventilator alarms in properly configured systems. In fact, the use of adjustable inline PEEP valves together with a bypass circuit specifically allows ventilator alarms to be left intact by ensuring two normal situations continue to occur at the expiratory port of the ventilator: equal net inspiratory and expiratory gas volume and equal gas pressure at the inspiratory and expiratory ventilator ports.
Inline PEEP valves allow the creation of a closed system since, in contrast to traditional PEEP valves, no gas is vented to the atmosphere. Since inline PEEP valves should not introduce leak into the system when constructed with well-sealed materials, the volume of gas leaving the ventilator at the inspiratory circuit port is the same as the volume received at the expiratory port. This situation allows the ventilator to identify leaks when a discrepancy between the inspiratory and expiratory volume is detected and prevents false detection of patient respiratory effort which can result in ventilator autocycling. In general, DMV setups using inline PEEP valves that have passed the ventilator self-check should not trigger “patient disconnect”, “low pressure”, or “low expiratory volume” alarms except when a disconnect event or new leak has occurred.
When inline PEEP valves are used in conjunction with a bypass circuit, the gas pressure at the expiratory port of the ventilator will be equal to PIPvent during inspiration and the ventilator-set PEEP during end-expiration. This situation is required to prevent “tube obstruction” and “high airway pressure” alarms whereby the ventilator detects inline PEEP valves as an obstruction. The bypass circuit is necessary when using inline PEEP valves with most ventilators not only to avoid triggering these alarms but also to maintain predictable behavior of the ventilator, which is discussed in detail later.
OBTAINING INLINE VALVES IN A PANDEMIC
Inline adjustable PEEP valves are only commercially available in a limited number of countries and are not commonly stocked by hospitals. Fixed-pressure inline valves are more prevalent, but their application in DMV systems is limited since physical replacement of valves as a means for adjusting ventilator settings is impractical. For these reasons, most DMV systems rely on the conversion of commercial BVM PEEP valves, which are readily available in most healthcare systems worldwide. Alternatively, when even standard commercial PEEP valves are not available, inline PEEP valves can be 3D printed (Fig. 3A) (8).
Figure 3.
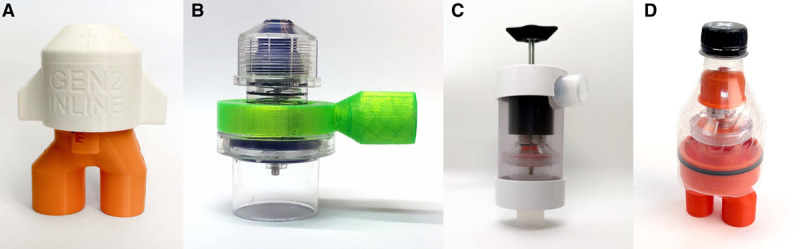
Adjustable inline positive end-expiratory pressure (PEEP) valve examples. From left to right: A, 3D printed PEEP valve (inline PANDApeep Gen2 inline) (8), B, PEEP valve collar (collar adapter) (9), C, PEEP valve enclosure (simple polyvinyl chloride enclosure) (10), D, 3D printed enclosure (PANDAcase bottle) (11).
Standard PEEP valves can be converted to inline valves by collecting vented gas with additional components. Currently proposed methods for converting a standard PEEP valve to an inline version include collar designs or enclosure designs (a comparison of the benefits and weaknesses of each approach is provided in Table 1). Collar designs encase the exhaust ports but leave the adjustment knob external (Fig. 3B) (9). In contrast, enclosure designs encase the entire valve to collect exhaled gases. Enclosures can be 3D printed, assembled from modified commercial parts, or use a combination of commercial and 3D-printed components. Enclosure designs use various methods for adjusting the enclosed PEEP valve’s pressure setpoint including replacements of the built-in adjustment cap (Fig. 3C) or knob extenders that leave the cap intact (Fig. 3D) (10, 11).
Table 1.
A Comparison of Inline Positive End-Expiratory PressureValves Options for Differential multiventilation Systems
| Types | Adjustable Inline PEEP Valve | Modified PEEP Valve With Collar | Inline PEEP Valve Enclosure With Commercial PEEP Valve | ||
|---|---|---|---|---|---|
| Construction | Commercial | 3D-printed components | 3D-printed components | Commercial Components | 3D-printed components |
| Pros | Made for purpose | Requires minimal sourcing of supplies | Requires minimal sourcing of supplies | Uses commercial PEEP valves | Requires minimal sourcing of supplies |
| Food and Drug Administration approved | |||||
| Valves are easily serviced and replaced | |||||
| Does not require an intact supply chain | Manufacturer PEEP settings/indicators intact | Uses commercial PEEP valves | |||
| Manufacturer PEEP setting/indicators can be kept intact (transparent enclosures only) | |||||
| Manufacturer PEEP setting/indicators can be kept intact (transparent enclosures only) | |||||
| Convenient form-factor | |||||
| Cons | Not available in most countries | No indicated PEEP settings (must be measured) | Leaks at higher postvalve pressures (due to manufacturer-provided cap design) | Requires sourcing of multiple parts | Fully 3D printed designs do not permit simple visualization of PEEP valve setting. |
| Rarely stocked in hospitals | Printed spring strength may decrease over time at high settings | Requires epoxy and/or sealant | Nonprinted enclosures often involve more complicated assembly | Function of bottle-based design dependant on matching local bottle shape (varies by country) to 3D printed base | |
| Requires intact supply chain at time of surge | |||||
| Expensive | Requires permanent modification of commercial valves | ||||
PEEP = positive end-expiratory pressure.
CAVEATS OF INLINE PEEP VALVES IN DMV
The safest DMV designs use a bypass circuit which ensures predictable behavior of the ventilator and individualized circuit adjustments by preventing obstruction of the normal bias flow. When the ventilator is set to a pressure control mode and this bypass circuit is not used, the use of inline PEEP valves results in a number of predictable, but unintuitive effects to the inspiratory and expiratory limbs of the ventilator circuit. For example, when in a two-patient DMV system lacking a bypass circuit, two scenarios can occur. In the first scenario, one patient receives ventilator PIP and PEEP without any individualized adjustment, whereas the other patient has both PIP decreased and PEEP increased. In this scenario, the ventilator will generally behave as expected as bias flow is preserved (via the first patient’s circuit). In the second scenario, both patients have at least one individualized setting. When this occurs, the expiratory port of the ventilator may sense lower pressure than expected and automatically increase the PIP above the set pressure to compensate for the obstruction. This effect is highly undesirable because it results in a potentially confusing situation whereby a provider changes one setting (e.g., PEEPinline), but this change results in the ventilator changing a seemingly unrelated variable (e.g., PIPvent). Even if this effect is anticipated, the ventilator compensation behavior still results in more difficult prediction of required settings in addition to triggering obstruction alarms on the ventilator. For this reason, use of a bypass circuit is required when inline PEEP valves (or other flow restrictors) are used in a DMV system.
Another caveat of the use of adapted or improvised inline valves is the possibility of device failure. Failure potential exists whenever commercial or improvised devices are used in a manner that produces considerable wear or stress on equipment. DMV methods are new, and data on the useable lifetime of printed and adapted PEEP valves are lacking. Given the risks of unanticipated device failure, DMV circuits should be closely monitored for performance changes or failure. Enclosure and collar-type adapters have the potential to develop leaks over time and should be replaced when this occurs. PEEP valve springs, particularly low-quality and nonmetal springs, can lose strength over time especially when more compressed at the higher PEEP settings. Whenever possible, the ventilator should be used to provide the majority of the PEEP which lowers the required individual PEEP valve settings and reduces stress and wear on individual springs. Furthermore, continuous pressure manometry should be used to identify failing valves, facilitating early replacement. Individual inline PEEP valves designs should be subjected to formal evaluation to determine failure points and quantify the useable life of adjustable inline PEEP valves.
When adjustable valves are used in a DMV system to decrease PIP and/or increase PEEP, the driving pressure is reduced. As a consequence, the possibility exists of situations where driving pressure may be inadequate for one or more patients when valves settings are high. Inadequately low driving pressure is dangerous to the patient as it can result in severe hypoventilation. In the worst case scenario, driving pressure is close to zero resulting in complete apnea. Continuous individual patient and circuit monitoring are essential to avoid critical hypoventilation of patients connected to DMV systems.
Finally, although the effects of individualized inline PEEP valves are relatively predictable when incorporated into a well-designed DMV system, these effects are still more complex than usual ventilator use, require some mental calculations, and involve unfamiliar steps for the uninitiated. For these reasons, safe use of inline valves requires continuous monitoring with pressure sensors or dial manometers to allow real-time measurement of delivered individual PIP and PEEP. Although measuring these values in real-time helps reduce the risk of error, the use of inline valves to individualize settings in a DMV system involves high-level knowledge of ventilator function, DMV systems, and potential effects on covented patients. These DMV-specific challenges also further complicate sometimes already challenging aspects of traditional single-patient mechanical ventilation such as weaning patients and patient-ventilator interactions. Therefore, DMV methods constitute advanced ventilator management and should always be supervised by a knowledgeable intensivist or anesthesiologist.
CONCLUSIONS
Adjustable inline PEEP valves are critical to DMV system reliability and safety when attempting to extend ventilator capacity in the setting of extreme ventilator shortages. In DMV systems, inline PEEP valves provide a means to reduce delivered PIP to an individual patient circuit, a method to increase PEEP for an individual patient circuit, and act as an one-way valve to ensure unidirectional gas flow through the divided circuit. Because of its multifunctional role in DMV, inline PEEP valves are an essential component but are uncommonly available in healthcare systems. Adjustable inline PEEP valves can be adapted from commercial valves or printed de novo when commercial options are unavailable. DMV systems and noncommercial sourcing of ventilator components should only be considered in a time of crisis and setting of extreme ventilator shortages. Use of adjustable inline PEEP valves to individualize ventilator setting should only be performed under the supervision of a knowledgeable anesthesiologist or intensivist.
Footnotes
Dr. Roy is involved in the design and commercialization of individualized split-ventilator circuits which potentially includes being named coinventor on patent filings.
The authors have not disclosed any potential conflicts of interest.
REFERENCES
- 1.Beitler JR, Kallet R, Kacmarek R, et al. Ventilator Sharing Protocol: Dual-Patient Ventilation With a Single Mechanical Ventilator for Use During Critical Ventilator Shortages. Available at: https://www.gnyha.org/wp-content/uploads/2020/03/Ventilator-Sharing-Protocol-Dual-Patient-Ventilation-with-a-Single-Mechanical-Ventilator-for-Use-during-Critical-Ventilator-Shortages.pdf. Accessed April 29, 2020.
- 2.U.S. Public Health Service Commissioned Corps: Optimizing Ventilator Use During the COVID-19 Pandemic. 2020 Available at: https://www.hhs.gov/sites/default/files/optimizing-ventilator-use-during-covid19-pandemic.pdf. Accessed April 29, 2020.
- 3.U.S. Food and Drug Administration Appendix B: Authorized Ventilators, Ventilator Tubing Connectors, and Ventilator Accessories. 2020. Available at: https://www.fda.gov/media/136528/download. Accessed April 29, 2020
- 4.Society of Critical Care Medicine, American Association for Respiratory Care, American Society of Anesthesiologists, Anesthesia Patient Safety Foundation, American Association of Critical-Care Nurses, American College of Chest Physicians. 2020 Available at: https://www.sccm.org/getattachment/Disaster/Joint-Statement-on-Multiple-Patients-Per-Ventilato/Joint-Statement-Patients-Single-Ventilator.pdf. Accessed April 29, 2020.
- 5.Raredon MSB, Fisher C, Heerdt P, et al. Pressure-regulated ventilator splitting (PReVentS): A COVID-19 response paradigm from Yale University. medRxiv. 2020.04.03.20052217 [Google Scholar]
- 6.Differential Multiventilation International Working Group. Overview - Differential Multiventilation Guide. Available at: https://www.differentialmultivent.org/. Accessed April 27, 2020
- 7.Han JS, Mashari A, Singh D, et al. Personalized ventilation to multiple patients using a single ventilator: Description and proof of concept. Crit Care Explor. 2020; 2:e0118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Textor D, Stahl S; PANDApeep Gen2 Inline 2020. Available at: https://www.thingiverse.com/thing:4316582. Accessed April 29, 2020
- 9.Koberg J; PEEP Adapter for AMBU Valve—GitHub 2020. Available at: https://github.com/jkoberg/splitvent. Accessed April 29, 2020
- 10.Roy S; In-Line Adjustable PEEP Valves—Differential Multiventilation Guide 2020. Available at: https://www.differentialmultivent.org/in-line-adjustable-peep-valves/. Accessed April 29, 2020
- 11.Stahl S, Textor D; PANDAcase Bottle - PEEP Valve Enclosure 2020. Available at: https://www.thingiverse.com/thing:4314931. Accessed April 29, 2020


