Supplemental Digital Content is available in the text.
Keywords: adult, coronavirus disease 2019, critically ill, family-centered care, pediatric intensive care unit, staffing
Abstract
We describe the process converting half of our 40-bed PICU into a negative-pressure biocontainment ICU dedicated to adult coronavirus disease 2019 patients within a 1,003-bed academic quaternary hospital. We outline the construction, logistics, supplies, provider education, staffing, and operations. We share lessons learned of working with a predominantly pediatric staff blended with adult expertise staff while maintaining elements of family-centered care typical of pediatric critical care medicine. Critically ill coronavirus disease 2019 adult patients may be cared for in a PICU and care may be augmented by implementing elements of holistic, family-centered PICU practice.
To the Editor:
Coronavirus disease 2019 (COVID-19) has overrun healthcare systems worldwide. The projected need for ICU beds in the United States was three times the existing number (1–6). As the pandemic spread in the Baltimore, DC region, pediatric needs declined because elective surgeries were halted and COVID-19 has a low pediatric disease burden (7–10). The Johns Hopkins Hospital (JHH), a 1,003-bed facility with embedded 203-bed children’s center, is a National Emerging Special Pathogens Treatment Center with a dedicated biocontainment unit that quickly reached capacity with critically ill COVID-19 patients (11). JHH was able to fulfill its pediatric mission as consequence of a lower patient volume but needed to expand adult ICU capacity to support a surge of patients (12, 13). We describe the conversion of half of our PICU into an adult negative-pressure COVID-19 ICU.
LAUNCHING THE UNIT
JHH successfully “launched” multiple novel biocontainment ICUs to meet the needs of COVID-19 patients using a multidepartment and multidisciplinary Incident Command Center. Leaders from the Departments of Medicine and Anesthesiology and Critical Care Medicine formed a centralized multidisciplinary “launch team” to standardize physical plant changes, staffing, equipment/supplies, and training for new converted COVID-19 ICUs. At the time of PICU conversion, JHH had increased ICU beds from 118 to 172 in both converted subspecialty ICUs and repurposed adult acute care spaces. Yet, rising cases locally and transfers from affiliate hospitals necessitated additional capacity. With a PICU census less than half of the available beds, the PICU was the next unit for conversion. Transformation of the PICU into two units occurred over 10 days (Fig. 1).
Figure 1.
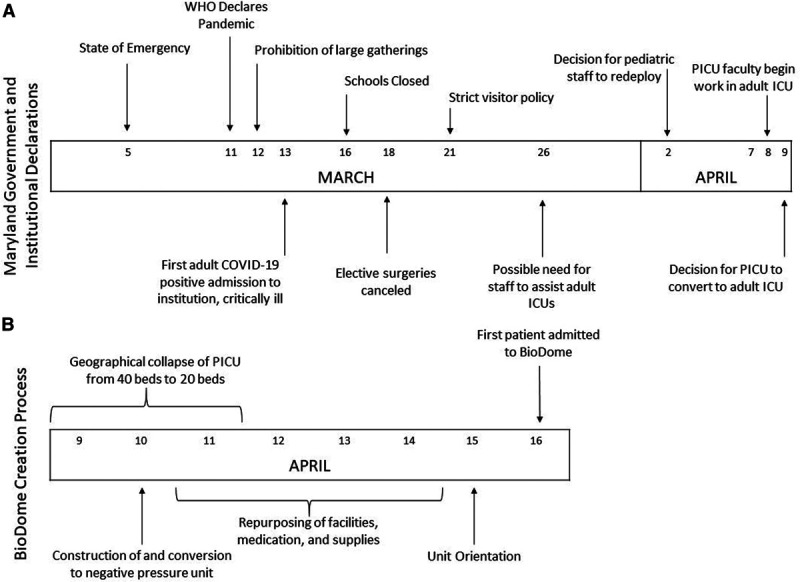
Timeline of events leading to the opening of an adult coronavirus disease 2019 (COVID-19) ICU in repurposed PICU space in March 2020 and April 2020. A, Maryland state and institutional responses to the developing local outbreak by day of month. B, Dates of steps taken to convert the physical space of the PICU and ready staff for opening of the negative-pressure adult COVID-19 ICU. WHO = World Health Organization.
Physical Plant
JHH Facilities, Epidemiology and Infection Control, and PICU leaders identified a natural divide for the 40-bed PICU into a 20-bed neo-PICU and 20-bed negative-pressure adult ICU, colloquially known as the “BioDome.” Construction included building a separation wall, sealing of pneumatic tube stations and doorways, and creation of one donning and two doffing anterooms, one accommodating patient transport. The main ventilation system was converted, so patient rooms were negative pressure to the hall and portable high efficiency particulate air fans made the donning and doffing anterooms positive pressure to the unit and outside corridors. Pressure monitors were installed ensuring donning and doffing areas sustained a positive pressure relationship to adjacent spaces.
Conference rooms and workrooms were repurposed in the neo-PICU to accommodate six-foot distance between staff. With significant visitor restrictions, unused family kitchens and waiting areas were repurposed for staff respite areas. Offices were moved outside the PICU.
Staffing
Early in the pandemic, a subset of PICU attending physicians, nurses, and respiratory therapists (RTs) were deployed to adult COVID-19 ICUs to support increased demand. There they received rapid bedside experience in caring for critically ill adult COVID-19 patients, becoming familiar with common treatments and complications, and building familiarity with adult critical care leadership staff. Deployed PICU attending physicians had dual training in internal medicine or anesthesia or were biocontainment unit faculty. All deployed physicians received hospital approved emergency credentialing for the care of adult patients. Additionally, pediatric critical care fellows with internal medicine training who had completed clinical fellowship training requirements received fast-tracked credentialing as attending physicians. Many PICU nurses and RTs had previous adult experience prior to working in the PICU, and JHH expanded RT capacity by training anesthesia providers as RT adjuncts.
PICU providers were recalled to the BioDome from deployments and blended with additional staff. The BioDome staffing was with PICU attendings, fellows, nurses, and RTs. Housestaff was intentionally augmented with senior residents from Medicine/Pediatrics, Anesthesiology, and Emergency Medicine to strategically blend in providers with adult experience. The primary PICU BioDome team was supported with a daytime adult intensivist from the launch team, and an adult ICU resource fellow and nurse were on site 24/7 for a week. A standing JHH resource is the central intensivist (CI), a 24/7 roving adult intensivist supporting the hospital in ICU bed management and crisis care. After the first week, we relied on the CI with either phone consultation or could immediately be present in the unit if needed. These adult colleagues provided patient management support, especially in patients with complications unable to be managed with published resources or those with advanced disease (14). All staff were cleared by hospital epidemiology and infection control to work in both COVID-19 units and non-COVID-19 units. Physician, fellow, and resident scheduling allowed for dedicated around-the-clock BioDome staff separate from the PICU, whereas nursing and RT staff were assigned on a shift by shift as needed basis to not only our BioDome but multiple COVID-19 units throughout the institution.
A PICU social worker with adult medical ICU experience, adult critical care pharmacists, physical and occupational therapists (PTs/OTs), pediatric palliative care nurse practitioner, and dietician participated in virtual rounds with occasional in-person support. All consults were made to adult subspecialists.
Centralized COVID-19 teams were available for additional support: an anesthesia airway team performed intubations; the CI-led emergency response team assisted in emergencies; an ICU nurse, RT, and PT/OT assisted with prone positioning; and a transport team ensured safe transports. A procedure team was available, but PICU fellows completed all procedures. All patients were transferred to a specific ICU for extracorporeal support if needed, with streamlined consultation and activation.
Equipment/Supply/Medication Preparation
The physical separation of the neo-PICU and BioDome required substantially different supply stocks. Pediatric supplies were moved to the neo-PICU. The launch team provided standard supplies, equipment, and medication lists, and PICU staff ordered and stocked the BioDome during construction. Adult code carts, emergency resuscitation medication boxes, IV and feeding pumps, and sequential compression devices were brought to the units. Ultrasound machines with point-of-care capability and minimal surfaces to clean were obtained. Workflows for medication hand-delivery to the BioDome and batched laboratory specimen transport were created. Monitors were converted to adult variables, a separate bank of wireless telephones was linked to these monitors, and emergency alarms were separated by unit. Rooms were outfitted with an iPad and speaker to facilitate communication with families and virtual interpreters, and dry erase boards and markers were added to facilitate provider communication.
Personal Protective Equipment
Each staff member was fit-tested for at least two appropriate airborne respirators (Supplemental Material, http://links.lww.com/CCX/A326) (15, 16). Dedicated safety officers stationed in the anterooms ensured standardized donning and doffing.
Electronic Medical Records
Staff used adult physician and nursing documentation templates, flow sheets, and medication and laboratory order sets designed for COVID-19 in our electronic medical records. We relied on provider-guided titration of sedation and vasoactive medications to continue safe practices familiar to our PICU staff. PICU attendings were educated on documentation, billing, and state guidance for declaration of deaths from COVID-19.
OPENING THE UNIT
Education
Pre-launch, all BioDome staff received standard JHH-wide electronic education on COVID-19 disease and role-specific training (Supplemental Material, http://links.lww.com/CCX/A326). All staff learned safe personal protective equipment (PPE) donning and doffing procedures. A half-day multidisciplinary orientation was held 1 day before the first patient admission and recorded for future review (Supplemental Material, http://links.lww.com/CCX/A326).
Unit Function
A JHH central command staggered all COVID-19 admissions to prevent overrun of one ICU. We admitted our first patients in a controlled manner to test the environment, build staff familiarity with adult care, and promote PICU/launch team collaboration. After the first 2 days of controlled and limited admissions, the converted PICU space entered into the hospital-wide admission queue and equally accepted admissions along with other ICUs. Daily operations in the BioDome closely mimicked those of the PICU but incorporated multidisciplinary team members via invite-only video conferencing. The bedside team used a video stream of the patient and monitor for all to observe.
In addition to nursing, at least one physician and RT were always present inside the BioDome. All staff staggered frequent breaks to respite areas. Physician handoffs were staggered and occurred outside the unit, whereas nursing and RT handoffs occurred on the unit.
We created workflows to limit BioDome traffic, PPE use, and separate movement of staff and patients from the neo-PICU. For example, staff carried supplies in, helped with cleaning, and transported trash to doffing areas. We relied on point-of-care ultrasound to reduce need for portable radiography. Specialists consulted by phone, entering the unit only when physical examination was required. We optimized teleconference rounding utilizing a headset, video camera, and speakers.
Uniquely Pediatric
We continued unique family-centered PICU practices in our BioDome. Our child life specialist supported children of our patients, a practice that spread to all other COVID-19 ICUs. We asked families to tell us about their loved ones and posted “All About Me” signs with patients’ interests, likes and dislikes, and family pictures. Our PICU palliative care nurse practitioner helped establish goals of care and supported end-of-life care with legacy-making activities. JHH made exceptions for visitors at end-of-life, and our social worker and nurse practitioner navigated the process of administration approval, escorting families to the unit, instructing them on PPE use, and facilitating electronic communication with those unable to visit. We conducted our usual PICU tradition of “Honor Guard,” lining the hallways with staff as our deceased patients were escorted to the morgue.
Unit Closure
As the local COVID-19 infections stabilized, the need for increased adult non-COVID-19 medical and surgical ICUs beds began to increase. Additionally, the need for PICU beds steadily increased as delayed procedures became urgent, and we began admitting critically ill pediatric patients with multisystem inflammatory syndrome. The PICU BioDome was open for 3 weeks and was the second converted adult BioDome ICU space to return to pre-COVID-19 functions. Initially, the negative pressure system was turned off, the separation wall and adult supplies/medications remained, and the unit was slated to support adult non-COVID-19 ICU patients to be staffed by our adult colleagues. However, the adult patient ICU census was manageable without our space, so the separating wall was eventually removed. As we look forward to uncertain and likely changing need, our unit is now prepared to adapt to future increased ICU needs, either pediatric or adult. Adult supplies are maintained in a separate storage location, and monitors and message systems are set to pediatric presets, but we now have ready operations to convert back to adult mode. In anticipation of a second wave in the fall of 2020, no other modifications were undone and the BioDome can be rapidly reinstituted.
After BioDome physical closure, PICU attendings, nurses, and RTs continued to support the other institutional adult COVID-19 ICUs as independent staff for an additional 7 weeks.
LESSONS LEARNED
We initially deployed staff with adult experience, but pediatric trained PICU providers quickly gained competence in adult COVID-19 and ICU care. We rapidly established an independent PICU run and led BioDome considered equal to the other institutional COVID-19 ICUs. Working in the BioDome required increased staff to facilitate breaks for hydration and rest, reduce PPE facial pressure injuries, and hand-deliver medications and laboratory specimens.
Our greatest growth was our ability to connect with patients and each other. We used iPads and speakers in each room to link with families. Staff members wore cleanable photo buttons with their picture, name, and title enabling patients to see behind the PPE. We established routines of communication with families thrice daily with an early identified decision-maker.
We experienced growing pains as well. Ascertaining practice styles and reconciling variations while learning COVID-19 medical care took time. Although we appreciated the launch team’s expertise and knowledge, chains of command often blurred between the PICU attending/fellow and the resourcing adult attending/fellow. This required direct, clear, and consistent communication regarding ultimate patient management responsibilities belonging to the PICU attending. Having a dedicated and small PICU BioDome attending cohort assisted in keeping consistency. Additionally, the PICU attending was physically present in the BioDome or the work space more frequently than normal to ensure open and uniform communication. Whereas PICU physician staff was supported with colleagues from the adult divisions of our Department of Anesthesiology and Critical Care Medicine, our nursing colleagues were supported with resources from outside their department. Despite PICU nurses gaining familiarity with adult ICU bedside nursing and personnel from redeployments, there were instances of strain between adult and pediatric nursing practices such as sedation and pressor titration. Our PICU relies heavily on physician-guided protocols rather than nurse-driven, which is common in our institution’s medical ICUs. At times, the physician-driven practices and increased presence were interpreted as overbearing from the adult ICU resource nurses. Once there was an openly stated shared mental model of practice style, tensions eased. Additionally, learning the nuances of working in the adult system, such as extracorporeal membrane oxygenation activation or dialysis initiation, sometimes occurred in real time, as these therapies were needed. After occurring once, lessons learned were shared with the whole team, making the next instance easier. Overall, the pandemic fostered a collaborative and “all-hands-on-deck” spirit throughout JHH with all disciplines assisting each other freely.
CONCLUSIONS
Establishing an adult COVID-19 ICU in a PICU was a challenge requiring coordinated multidisciplinary efforts to convert space, equipment, and teams. Nevertheless, by educating PICU clinicians in COVID-19 medical practices and retaining many elements of pediatric practice, we meet pandemic demands and provided excellent patient care.
Supplementary Material
Footnotes
This work was performed at the Johns Hopkins Children’s Center, The Johns Hopkins Hospital, Baltimore, MD.
Drs. Levin and Bernier contributed equally to this work.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website (http://journals.lww.com/ccejournal).
Dr. Milstone received support from National Institutes of Health K24 (K24AI141580). The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Litton E, Bucci T, Chavan S, et al. Surge capacity of intensive care units in case of acute increase in demand caused by COVID-19 in Australia. Med J Aust. 2020; 212:463–467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moghadas SM, Shoukat A, Fitzpatrick MC, et al. Projecting hospital utilization during the COVID-19 outbreaks in the United States. Proc Natl Acad Sci U S A. 2020; 117:9122–9126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Remuzzi A, Remuzzi G. COVID-19 and Italy: What next?. Lancet. 2020; 395:1225–1228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shoukat A, Wells CR, Langley JM, et al. Projecting demand for critical care beds during COVID-19 outbreaks in Canada. CMAJ. 2020; 192:E489–E496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vincent JL, Creteur J. Ethical aspects of the COVID-19 crisis: How to deal with an overwhelming shortage of acute beds. Eur Heart J Acute Cardiovasc Care. 2020; 9:248–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zangrillo A, Beretta L, Silvani P, et al. Fast reshaping of intensive care unit facilities in a large metropolitan hospital in Milan, Italy: Facing the COVID-19 pandemic emergency. Crit Care Resusc. 2020; 22:91–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hogan L. State of Maryland proclomation: Declaration of state of emergency and existence of catastrophic health emergency - COVID-19. 2020 Available at: https://governor.maryland.gov/wp-content/uploads/2020/03/Proclamation-COVID-19.pdf. Accessed September 11, 2020.
- 8.Office of Governor Larry Hogan: The Baltimore Times. As COVID-19 Crisis Escalates in Capital Region, Governor Hogan Issues Stay at Home Order Effective Tonight. 2020. Available at: https://governor.maryland.gov/2020/03/30/as-covid-19-crisis-escalates-in-capital-region-governor-hogan-issues-stay-at-home-order-effective-tonight/. Accessed March 30, 2020
- 9.Hogan L. Order of the Governor of the State of Maryland Number 20-03-30-01: Amending and Restating the Order of March 23, 2020, Prohibiting Large Gatherings and Events and Closing Senior Centers, and All Non-Essential Businesses and Other Establishments, and Additionally Requiring All Persons to Stay at Home. 2020 Available at: https://governor.maryland.gov/wp-content/uploads/2020/03/Gatherings-FOURTH-AMENDED-3.30.20.pdf. Accessed March 30, 2020.
- 10.Cruz AT, Zeichner SL. COVID-19 in children: Initial characterization of the pediatric disease. Pediatrics. 2020; 145:e20200834. [DOI] [PubMed] [Google Scholar]
- 11.National Emerg ing Special Pathogens Training and Education Center. 2020 Available at: https://netec.org/. Accessed May 11, 2020.
- 12.Philips K, Uong A, Buckenmyer T, et al. Rapid implementation of an adult coronavirus disease 2019 unit in a children’s hospital. J Pediatr. 2020; 222:22–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yager PH, Whalen KA, Cummings BM. Repurposing a pediatric ICU for adults. N Engl J Med. 2020; 382:e80. [DOI] [PubMed] [Google Scholar]
- 14.Remy KE, Verhoef PA, Malone JR, et al. Caring for critically ill adults with coronavirus disease 2019 in a PICU: Recommendations by dual trained intensivists. Pediatr Crit Care Med. 2020; 21:607–619 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


