Supplemental Digital Content is available in the text.
Keywords: acute respiratory distress syndrome, coagulation, coronavirus disease 2019, microvascular thrombosis, thrombolysis
Abstract
Objectives:
Microvascular thrombosis contributes to acute respiratory distress syndrome pathophysiology and has been demonstrated in coronavirus disease 2019-associated acute respiratory distress syndrome. Clinical laboratory measurements of coagulation and disseminated intravascular coagulation, such as coagulation factor function, platelet count, and fibrinogen, may not fully reflect the extent of microvascular thrombosis present in these patients. We investigated thromboelastography in patients with coronavirus disease 2019-associated acute respiratory distress syndrome with the objective of characterizing suspected coagulopathy and impaired fibrinolysis.
Design:
Retrospective observational cohort study.
Setting:
Single-center academic medical center.
Patients:
Ten patients with polymerase chain reaction-confirmed coronavirus disease 2019 disease complicated by acute respiratory distress syndrome.
Interventions:
Measurement of thromboelastography (n = 10) and thrombolysis with alteplase (n = 4).
Measurements and Main Results:
Hypercoagulability and decreased or absent fibrinolysis were demonstrated by thromboelastography. Thrombocytopenia and hypofibrinogenemia were not observed, while seven of 10 patients had elevated d-dimer values. For patients who received thrombolytic therapy, repeat thromboelastography demonstrated improvements in coagulation index and lysis at 30 minutes reflecting reduced hypercoagulability and increased fibrinolysis. One major bleeding complication was detected following thrombolysis. Eight of 10 patients survived and were successfully extubated, and six of 10 have since been discharged.
Conclusions:
In coronavirus disease 2019 patients with acute respiratory distress syndrome in whom thromboelastography was performed, hypercoagulability and impaired fibrinolysis were observed. In the context of autopsy studies demonstrating pulmonary microvascular thromboses in coronavirus disease 2019 patients, noninvasive detection of hypercoagulability and deficient fibrinolysis in coronavirus disease 2019 acute respiratory distress syndrome using thromboelastography could improve understanding and management of coronavirus disease 2019.
Patients with severe coronavirus disease 2019 (COVID-19) infection manifested by acute respiratory distress syndrome (ARDS) demonstrate extensive pulmonary microvascular thromboses and fibrin deposition in available postmortem pathologic specimens (1, 2). These findings have generated the hypothesis that coagulopathy is a central mechanism of hypoxia in COVID-19-associated ARDS (3–5). Microvascular thrombosis may promote hypoxia through increased dead space leading to ventilation/perfusion ratio (V/Q) mismatch or by promoting hypoxic vasoconstriction. Hypercoagulability in COVID-19 patients correlates with increased mortality, motivating multiple clinical trials of anticoagulation or systemic thrombolysis (6–8). Although d-dimer is prominently elevated and associated with mortality in COVID-19 patients, other indices of disseminated intravascular coagulation are variable in this population (6). Thus, detection of microvascular thrombosis before overt thrombotic phenomena or clinical decompensations occur, and determining indications for coagulopathy-directed treatment constitute a substantial clinical challenge.
Thromboelastography measures platelet function, clot strength, and fibrinolysis in addition to coagulation factor function. Despite known derangements in fibrinolysis and coagulopathy in ARDS patients, thromboelastography has only been previously reported in ARDS patients following trauma or extracorporeal membrane oxygenation (ECMO), in which mechanisms of coagulopathy likely differ from COVID-19 ARDS patients. Due to prominent clotting abnormalities (3–5) and proposed use of anticoagulation and lytic therapy (7–9), we hypothesized that comprehensive evaluation of coagulopathy with thromboelastography might guide understanding and treatment in COVID-19 infection. We herein describe our experience using thromboelastography in critically ill COVID-19 ARDS patients, including those receiving thrombolysis.
MATERIALS AND METHODS
We performed a retrospective observational cohort study of 10 critically ill patients admitted to the medical ICU at our academic medical center for ARDS with polymerase chain reaction-confirmed COVID-19 disease who underwent thromboelastography assessment. Initial thromboelastography evaluation was performed for laboratory and clinical evidence of coagulopathy. Ventilatory and laboratory data reported in Supplemental Table 1 (http://links.lww.com/CCX/A293) is at time of first thromboelastography evaluation unless stated otherwise. Initiation of thrombolytic therapy was performed at the intensivists’ clinical decision following multidisciplinary consultation with a senior hematologist and pharmacist.
Patient Characteristics and Disease Course
Comorbidities and laboratory characteristics are reported in Supplemental Table 1 (http://links.lww.com/CCX/A293). All patients met Berlin criteria for ARDS with median Pao2:Fio2 (P:F) at intubation 169.5 (interquartile range, 138–204); oxygen saturation:Fio2 (S:F) was used when P:F was not available. All patients received lung-protective ventilation, four of 10 received neuromuscular blockade (NMB) and none underwent prone positioning. Shock and multisystem organ dysfunction were common (Supplemental Table 1, http://links.lww.com/CCX/A293). COVID-19-directed therapies are summarized in Supplemental Table 1 (http://links.lww.com/CCX/A293). At the time of this article, two of 10 patients died, while eight of 10 were successfully extubated and transferred to the floor. Of those, five have since been discharged home, while one was discharged to acute rehabilitation.
Thromboelastography Characteristics
Thromboelastography was performed a median of 2.5 days (1–6 d) after ICU admission (Supplemental Table 2, http://links.lww.com/CCX/A294). Initial use of rapid thromboelastography (15-min protocol) was replaced by 20-minute extended studies to better evaluate clotting and lysis abnormalities. Seven of 10 patients were receiving heparin (six prophylactic, one treatment dosing); thromboelastograms in these patients were reviewed with and without heparinase. Common observed abnormalities included short r time, median time: 4.45 minutes (3.6–5.8 min), rapid fibrin cross-linking and strong platelet-fibrin interaction (median alpha angle, 78.25° [75.1–78.7°] and median maximum amplitude was 71.95 mm [68.5–74.5 mm]), and absence of rapid fibrinolysis (median percent lysis at 30 min [LY30%] 0.75% [0–2.6%]). Several patients exhibited profoundly depressed LY30% values. Median coagulation index was elevated (2.8, 1.8–3.6). Overall, these changes reflect hypercoagulability with profoundly impaired fibrinolysis.
Outcomes of Treatment With Lytic Therapy
Patients received off-label alteplase for thrombolysis (n = 4) for clinical evidence or suspicion of microvascular or macrovascular thrombosis, including acute kidney injury (AKI), sinoatrial node dysfunction, clotting continuous renal replacement therapy (CRRT) circuit, worsening hypoxemia as defined by declining P:F or S:F or increasing positive end-expiratory pressure (PEEP) requirement, or elevated dead space fraction, in conjunction with laboratory markers such as thromboelastography, C-reactive protein, and d-dimer (Fig. 1). Acute pulmonary embolism was suspected in one patient based on hemodynamic instability correlating with right ventricular strain on bedside ultrasonography. Multiple organ dysfunction, NMB, vasopressor support, and CRRT requirement were common (Supplemental Table 1, http://links.lww.com/CCX/A293). Median admission P:F was 152.5 (76–201) with pre-lysis median P:F 107.5 (73.5–131.8). Pretreatment thromboelastography exhibited elevated alpha angle (3/4) and maximum amplitude (3/4) and absent LY30% (3/4). Alteplase was administered as 25 mg over 120 minutes with remaining 25 mg infused over 22 hours. Cases are summarized in further detail as follows:
Figure 1.
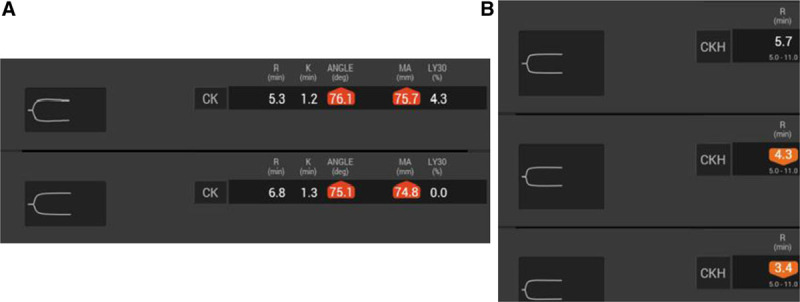
Thromboelastography tracings from representative patients. A, Patient A: Bottom precedes thrombolytic treatment with top performed after alteplase. B, Patient B: Progression from bottom to top demonstrating worsening fibrinolysis in the clinical context of bradycardia, ventricular tachycardia, and asystole. ANGLE = alpha angle (slope between R and K, measure of clot strengthening), CK = citrated kaolin, CKH = citrated kaolin with heparinase, K = kinetics, LY30 = lysis at 30 minutes, MA = maximum amplitude, R = reaction time.
Patient 3, a 39-year-old man with psoriasis on immune modulator therapy, was admitted from the emergency department (ED) with moderate ARDS requiring immediate ICU admission, intubation, and NMB. AKI developed requiring CRRT. He received alteplase followed by therapeutic heparin for 4.5 days. In the time after completion of thrombolysis, ventilatory ratio improved from 2.77 to 2.09, P:F improved from 186 to 262.5, and Fio2 requirement decreased from 0.5 to 0.4. No major bleeding complications were observed. He was extubated on ICU day number 6 to high-flow nasal cannula (HFNC) and has since been discharged home.
Patient 7, a 47-year-old man with morbid obesity, was transferred from an outside institution for ARDS requiring intubation. Following transfer, severe ARDS, multifactorial shock, and AKI requiring CRRT were noted. He received NMB and inhaled epoprostenol; proning was deferred secondary to habitus. Bedside echocardiogram performed for refractory hypoxia demonstrated right ventricular strain. Therapeutic anticoagulation was initiated but CRRT circuit clotting persisted, motivating treatment with systemic thrombolysis. Over the following 24 hours, S:F ratio increased from 134 to 184, Fio2 requirement decreased from 0.7 to 0.5, and PEEP decreased from 20 to 18 cm H2O. Given the patient’s prior wishes to avoid prolonged hospitalization, comfort measures were ultimately pursued.
Patient 9, a 43-year-old man with morbid obesity, was admitted from the ED with moderate ARDS requiring immediate intubation and NMB. He was treated with systemic thrombolysis followed by heparin infusion. Over the following 24 hours, Fio2 requirement decreased from 0.7 to 0.4, PEEP from 16 to 14 cm H2O, and P:F remained stable from 192 to 200, but right forearm and neck hematoma were noted. Compartment syndrome was confirmed with Stryker compartment measurement, and bedside right volar fasciotomy was performed. He suffered an aspiration event during endotracheal tube exchange with clinical worsening 5 days after ICU admission but was ultimately extubated to HFNC and has since been transferred to a general hospital floor.
Patient 10, a 54-year-old woman with diabetes mellitus and morbid obesity, was initially admitted from the ED to the ICU with moderate ARDS requiring intubation. She was extubated to HFNC on hospital day number 4. On day number 7, she was emergently reintubated for severe hypoxia and hemodynamic instability, including sinus bradycardia, prompting systemic thrombolysis followed by therapeutic anticoagulation. No major bleeding complications were observed. Due to her clinical instability prior to thrombolysis, arterial blood gas and ventilatory ratio are not available pre-thrombolysis. Post-intubation and thrombolysis, P:F was 140. During the treatment period, S:F ratio improved from 123 to 240, Fio2 was weaned from 0.8 to 0.4, and PEEP from 14 to 12 cm H2O. She was extubated 24 hours after completion of thrombolysis. Prior to discharge, CT angiography revealed segmental pulmonary emboli, and apixaban was started. She has been discharged home.
DISCUSSION
Our findings demonstrate hypercoagulability and impaired fibrinolysis in selected COVID-19-associated ARDS patients. Our findings complement previous observations of poor prognosis associated with elevated d-dimer and pathology from COVID-19 victims demonstrating significant microvascular thrombosis, suggesting that coagulopathy may contribute to hypoxemia in these patients (1, 6, 9). Given the lack of effective treatments and the severity of the current pandemic, further investigation of this potential mechanism is indicated.
Microvascular thrombosis is central to ARDS pathophysiology; endothelial dysfunction, fibrin deposition, and platelet aggregation impair perfusion to ventilated alveoli, leading to dead space ventilation and V/Q mismatch (10). Coagulation abnormalities and microvascular thromboses are associated with ARDS and with ARDS-triggers, particularly impaired fibrinolysis (as measured by biomarkers) (8). Our results suggest COVID-19-associated ARDS shares these features. Despite these findings, coagulopathy is not a routine target of monitoring or treatment in ARDS patients, and thromboelastography has not been used in non-COVID ARDS patients aside from trauma and ECMO patients. Thromboelastography provides more comprehensive assessment of coagulopathy than coagulation factor function studies and may identify subgroups of COVID-19 ARDS patients who are at greater risk of microvascular thrombosis, organ dysfunction, and poor outcomes. Improvements in oxygenation and ventilation observed after systemic thrombolysis in our cohort were likely multifactorial, and whether COVID-19 patients benefit from thrombolysis remains to be answered in the context of ongoing and planned clinical trials (NCT04344756); however, impaired fibrinolysis detected by thromboelastography may provide useful guidance to initiation and monitoring of lytic therapy, particularly in patients without response to therapeutic anticoagulation, should it be found to benefit COVID-19 ARDS patients.
CONCLUSIONS
Our findings, along with other case reports, suggest that impaired fibrinolysis may contribute to pathophysiology, including hypoxia and physiologic dead space in COVID-19 ARDS (7, 8). Use of thromboelastography may provide a noninvasive correlate of microvascular thrombosis that could improve risk stratification and prognostication for COVID-19 ARDS patients. Further investigation into the role of thromboelastography in assessing and treating ARDS should be a priority in the care of these patients as the search for effective therapies continues.
Supplementary Material
Footnotes
Drs. Sadd and Rowe contributed equally to this article.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccejournal).
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Yao XH, Li TY, He ZC, et al. [A pathological report of three COVID-19 cases by minimally invasive autopsies]. Zhonghua Bing Li Xue Za Zhi. 2020; 49:E009. [DOI] [PubMed] [Google Scholar]
- 2.Zhang T, Sun LX, Feng RE. [Comparison of clinical and pathological features between severe acute respiratory syndrome and coronavirus disease 2019]. Zhonghua Jie He He Hu Xi Za Zhi. 2020; 43:E040. [DOI] [PubMed] [Google Scholar]
- 3.Chen G, Wu D, Guo W, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020; 130:2620–2629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020; 323:1061–1069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020; 180:1–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yin S, Huang M, Li D, et al. Difference of coagulation features between severe pneumonia induced by SARS-CoV2 and non-SARS-CoV2. J Thromb Thrombolysis. 2020 Apr 3. [online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang J, Hajizadeh N, Moore EE, et al. Tissue plasminogen activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): A case series. J Thromb Haemost. 2020; 18:1752–1755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MacLaren R, Stringer KA. Emerging role of anticoagulants and fibrinolytics in the treatment of acute respiratory distress syndrome. Pharmacotherapy. 2007; 27:860–873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tang N, Bai H, Chen X, et al. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020; 18:1094–1099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Idell S. Coagulation, fibrinolysis, and fibrin deposition in acute lung injury. Crit Care Med. 2003; 314 SupplS213–S220 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


