Abstract
Contemporary humans are living very different lives from those of their ancestors, and some of the changes have had serious consequences for health. Multiple chronic “diseases of civilization,” such as cardiovascular problems, cancers, ADHD, and dementias are prevalent, increasing morbidity rates. Stress, including the disruption of traditional sleep patterns by modern lifestyles, plays a prominent role in the etiology of these diseases, including obstructive sleep apnea. Surprisingly, jaw shrinkage since the agricultural revolution, leading to an epidemic of crooked teeth, a lack of adequate space for the last molars (wisdom teeth), and constricted airways, is a major cause of sleep-related stress. Despite claims that the cause of this jaw epidemic is somehow genetic, the speed with which human jaws have changed, especially in the last few centuries, is much too fast to be evolutionary. Correlation in time and space strongly suggests the symptoms are phenotypic responses to a vast natural experiment—rapid and dramatic modifications of human physical and cultural environments. The agricultural and industrial revolutions have produced smaller jaws and less-toned muscles of the face and oropharynx, which contribute to the serious health problems mentioned above. The mechanism of change, research and clinical trials suggest, lies in orofacial posture, the way people now hold their jaws when not voluntarily moving them in speaking or eating and especially when sleeping. The critical resting oral posture has been disrupted in societies no longer hunting and gathering. Virtually all aspects of how modern people function and rest are radically different from those of our ancestors. We also briefly discuss treatment of jaw symptoms and possible clinical cures for individuals, as well as changes in society that might lead to better care and, ultimately, prevention.
Keywords: jaw, epidemic, evolution, orthodontics, cultural environment
“What are the causes and consequences of the growing prevalence of crooked teeth?” is a much-neglected question in public health. The much-neglected answer is the same as for other “diseases of civilization”: that industrialized humanity has developed an unprecedented lifestyle. Among many other things, that lifestyle has dramatically changed the environments in which human beings develop and has led to serious health problems (Ehrlich and Blumstein 2018), including the largely hidden ones connected with human jaws. One branch of dentistry, orthodontics, has become big business, and many children are now wearing braces and then retainers to manage malocclusion. The prevalence of orthodontic treatment, largely for cosmetic reasons, during a lifetime may be reaching 20% in the United States with the “need” much higher (Brunelle et al. 1996, Christopherson et al. 2009). Furthermore, increasing numbers of people are suffering facial pain connected to their jaws, specifically where they join the rest of the skull at the temporomandibular joint (Sessle 2015). In some populations, up to 10% of people are sufferers (LeResche 1997), and a branch of medicine has developed that specializes in treating craniofacial pain. Unhappily, rampant malocclusion and facial pain are actually only the tip of the iceberg—symptoms of a more serious underlying pandemic. Children are increasingly walking around and sleeping with their mouths open, snoring, and, along with adults, suffering obstructive sleep apnea and upper airway resistance syndrome (UARS). The increase in these problems can be only roughly estimated because of various forms of detection bias. Nonetheless, unbiased sampling of skulls of industrialized and hunter-gatherer populations shows unambiguously that the former suffer a higher incidence of jaw problems.”
Obstructive sleep apnea refers to having repeated stressful episodes of interrupted sleep from a temporary cessation of breathing, tracing often to jaws too small to house the tongue adequately. UARS is sleep fragmentation, often accompanied by snoring, without apnea, often traceable to narrowed jaws (Guilleminault and De Los Reyes 2011) The prevalence of obstructive sleep apnea appears to be perhaps 2%–7% or more in children (Lumeng and Chervin 2008), about 5%–20% in adults in general (Finkel et al. 2009), and over 80% in some elderly populations (Senaratna et al. 2017). The available data have many shortcomings, but a reasonably conservative estimate is that obstructive sleep apnea afflicts at least 1 in 20 people worldwide (Punjabi 2008), which is one indicator of the global extent of the jaw epidemic. We have found no data on the frequency of UARS, but it seems reasonable to assume that it is higher than the frequency of obstructive sleep apnea.
In children of normal weight, obstructive sleep apnea “is a disorder of oral-facial growth” (Huang and Guilleminault 2013, Stupak and Park 2018). The stress caused by obstructive sleep apnea or lesser degrees of sleep disturbance, such as UARS, is associated with a wide range of diseases including heart disease (e.g., Peker et al. 2006, Gottlieb et al. 2010, Taylor et al. 2017, Lopes et al. 2018), cancer (Campos-Rodriguez et al. 2013), ADHD (Montgomery and Wiggs 2015), and possibly Alzheimers disease (Walker 2017a, Fultz et al. 2019), as well as with deaths from errors caused by fatigue on the highway (Tregear et al. 2009) and in hospitals, where interns often get inadequate sleep (Walker 2017b). One of the potentially nasty consequences for individuals with obstructive sleep apnea is that the stress of disturbed sleep results in more or less constant sympathetic arousal. Virend Somers and his colleagues at the Cardiovascular Center at the University of Iowa College of Medicine concluded “that patients with obstructive sleep apnea have high sympathetic activity when awake, with further increases in blood pressure and sympathetic activity during sleep” (Somers et al. 1995, Usui et al. 2005, Abboud and Kumar 2014). Men with obstructive sleep apnea, if they also have insomnia that involves high sympathetic activity (Nunn et al. 2016), are also at greater risk for depression or hypertension than those with either condition alone (Gupta and Knapp 2014, Lang et al. 2017). Moreover, the disruption of sleep that is a typical consequence of obstructive sleep apnea increases the risk of cardiovascular disease (Palma et al. 2013, Li et al. 2018), most probably arising at least in part from the increased sympathetic tone (Bisogni et al. 2016). Complicating the whole picture is that stress itself is a cause of disturbed sleep, a dangerous positive feedback system (Han et al. 2012).
During the 2009 swine flu “epidemic,” about 0.5%–2% of Americans developed flu symptoms (Reed et al. 2009). It therefore seems reasonable to call the array of orofacial (and related airway) problems now afflicting people in the industrialized world a jaw epidemic, of which malocclusion is but one symptom. The oral and facial alignment and developmental issues in the childhood population can be traced specifically to poorly developed jaws. Nonetheless shrunken jaws are not being viewed as a medical issue of major consequence but rather as one of cosmetic concern.
Origins: Evolutionary and environmental causes of the epidemic
The root causes of our jaw problems go back several hundred thousand years as the crania of archaic hominids evolved into those of modern Homo sapiens. Major features of that transition included moving to a more globular brain case with a shrunken face tucked under it, dramatic shortening of the human jaw, and backward movement of the tongue. These may have been accompanied by a tendency for mouth breathing as our ancestors moved onto savannahs and needed greater airflow to lungs to increase endurance for pursuit hunting. If endurance running was important (Bortz II 1985, Bramble and Lieberman 2004, Lieberman DE et al. 2009), the shrinkage of the face may have helped to stabilize the head (Lieberman DE 2008). “Human distance runners are obligatory mouth breathers (but not panting).” Significantly lower levels of general fitness in modern societies may reveal why so many people are overbreathing (hyperventilation) orally, becauase relatively nonstrenuous tasks are provoking mouth breathing because of reduced respiratory efficiency (Tomkinson et al. 2012, 2019).
Oral overbreathing alters oral rest posture, thereby the developmental growth of the jaws. Dentists are familiar with what they call “long face syndrome” or “hyperdivergent growth”; it results from hanging the mouth open and produces a face with augmented downward facial development and restricted airway development. The cause is changes in habitual posture related to narrowed airways and weak chewing muscles. It leads to overeruption—the teeth becoming too long (Buschang et al. 2013).
Keeping the teeth apart at rest alters jaw structure, causing, among other things, a downward and backward rotation of the mandible. Together with increased malocclusion and other changes that accompany recent jaw shrinkage, this has made the airway more susceptible to blockage or collapse and children more susceptible to choking if they try to talk and eat (swallow) simultaneously. But preceding evolutionary changes toward smaller jaws also (Harari et al. 2010) provided presumed advantages, such as allowing the evolution of speech with syntax. As all the structures shortened and descended, the physical structure for such speech became possible (Lieberman P 2007).
The selection pressures causing these changes as archaic Homo sapiens genomes evolved into modern Homo sapiens genomes over thousands of generations have been speculated on (Lieberman DE 2008) but not identified with any certainty. The original reduction in jaw size that occurred millions of years ago as hominins evolved from ape-like ancestors has resumed over bib85the last tens of generations, moving much too rapidly to be attributed to genetic evolution. Comparisons of Medieval and modern skulls demonstrate this dramatically, with tooth crowding considerably less frequent in the Middle Ages (Moore et al. 1968, Helm and Prydsö 1979, Luther 1993), and there has been rapid change in jaw morphology in that brief period (Goose 1981). With very bib85rare exceptions, hunter-gatherers had roomy jaws. Malocclusion and noneruption of third molars (wisdom teeth) and crowding of the tongue were close to nonexistent; preindustrial jaws were simply roomier than those of people exposed to modern lifestyles (e.g., Price 1939, Proffit 1975, Helm and Prydsö 1979, Gibson and Calcagno 1993, Luther 1993, Kaifu 1997, 2000, Evensen and Øgaard 2007, Rose and Roblee 2009, Lieberman DE 2013, Kahn and Ehrlich 2018). The jaw epidemic is therefore a recent phenomenon and temporal and geographic correlation strongly suggests that it can be traced to changes in environmental factors due to agriculture and industrialization, but exactly what those factors are and how they operate remain uncertain. Indeed, environmental influences on skeletal growth are largely ignored by the orthodontic profession, which often accepts jaw skeletal development as genetic in nature, although the teeth themselves are recognized as subject to environmental influences (Proffit 1978, Tulloch et al. 1998, 2004, Dolce et al. 2007, Siara-Olds et al. 2010, Ehsani et al. 2015).
The strong correlations in time and space with the course of the jaw epidemic and the agricultural and industrial revolutions has naturally called attention to softening diets and a reduction in the amount of chewing required for adequate nutrition (Lieberman DE et al. 2004, Buschang et al. 2013, Kahn and Ehrlich 2018). In the course of dealing with the genetic explanation of the epidemic, we now think too much emphasis has been put on the chewing function and not enough on oral posture. Current evidence suggests that alteration of oral postural influences on skeletal growth is the main cause of malocclusion. It results from changes in the persistent but gentle forces that appear to influence phenotypic skeletal development—soft tissue positioning molding bone shape and size (Sankey et al. 2000, Mew 2004, 2015a, Buschang et al. 2013, Buschang and Jacob 2014, Pisani et al. 2016). Bones grow (and change shape) under light but persistent pressures. Those created by oral posture—the positions of the jaws and tongue in relation to each other when a child is not eating or speaking—constitute signals that, among other signals, guide the growth of the jaws. What Mew (2004) postulated and more recently Engelke and his colleagues (Engelke et al. 2011, Knösel et al. 2016) have demonstrated as “correct” oral posture is holding the teeth lightly together, with the tongue positioned against the palate; clinical studies show that this posture results in an adequately roomy jaw (Wong 2018).
The Engelke team began to elucidate experimentally the details of pressure differences within functional “compartments” (formed by the positions of the lips tongue and soft palate) of the closed mouth, especially the way that, at the end of a proper swallow, there remains a self-sustaining negative pressure in the key compartment. They concluded (Engelke et al. 2011) that subjects (largely free of malocclusion) who swallow using the actions of fully closing their mouths prior to an upward tongue pump generate a negative intraoral pressure system. This, in turn, is shown to develop a natural biomechanical equilibrium of forces surrounding the dental arches as well as to reduce the upper airway resistance to nasal breathing. Importantly, once this negative pressure is created, little if any further muscular input is required to sustain this closed posture, thereby providing what could well be the biologically optimal therapeutic rest position.
This basically says actions just before and after swallowing caused by environmental changes produced aberrant swallowing that may hold the keys to the etiology of the jaw epidemic. The problem is not a function of chewing itself but, rather, of maintaining the necessary negative pressure for long periods after a swallow, which is only possible in a closed compartment with that correct oral posture. The critical area seems to be the rear of the tongue, which is parasympathetically innervated, meaning the posture can be sustained without voluntary muscle action through passive light suction.
In any case, the importance of muscle posture and function in skeletal morphogenesis is well established (Henderson and Carter 2002), although full understanding of the complex mechanical and biochemical processes influencing how bones develop remains elusive (Ornitz and Marie 2015, Wu et al. 2016). The preponderance of evidence suggests the epidemic is caused by environmental modification of the pattern of gentle and persistent pressures that signal the normal development of the bones of the maxilla and the mandible—the upper and lower jaws (Woodside et al. 1983). That is seen in animal studies (such as blocking a monkey's nose or using a device to change the pressures its tongue applies to its palate; Harvold 1968) where changing the environment disrupts normal jaw development. Also, when the teeth are not kept in contact during rest, the tongue spills out over the teeth (as it does when the jaw is hung open) so the whole pressure system fails. Jaws shrink, but the tongue does not; indeed, it may grow larger in an obese individual (Nashi et al. 2007). The tongue may flow back into the throat, especially when an overweight individual is supine, partially blocking the airway (channel for air in the throat) and contributing to snoring or, if blockage is complete, obstructive sleep apnea. Reshaping of bones by persistent gentle pressures is also demonstrated by the fate of toe bones in Chinese women subjected to foot binding (Zhang et al. 2014) and changes in skull shape from head binding (Bridges et al. 2002; see also https://bit.ly/2LRiBwN).
The most obvious results of disruption of normal information flow between developing soft tissues and developing jawbones in modern people have been the shrinkage of the human jaws, their backward movement accompanied by crowding and misalignment of teeth. That leads to a reduction of space for the tongue, mouth breathing, and loss of tone in orofacial muscles (Harari et al. 2010), as well as other changes in facial morphology (Bresolin et al. 1983).
A big requirement in understanding the epidemic and treating its victims is to uncover exactly which of a number of possible factors disrupt correct oral posture and by how much? One obvious candidate that has received much attention is the effects on jaw musculature on switching to a diet that requires less chewing (Sakashita et al. 1996, Hall 2010, Limme 2010, Le Révérend et al. 2014, Sella-Tunis et al. 2018). That environmental transition had an “impact on the human speech apparatus (and) spoken language” (Blasi et al. 2019); that is, our occlusion changed from edge-to-edge to overbite and overjet over the last 6000–8000 years. That switch also appears to foster an incorrect (or reverse) swallow. Incorrect swallowing can result in open compartment resting postures, which, in turn, distorts the developing jaw shape, whereas correct adult swallowing results in the necessary physiological posture held by negative pressure and that can be maintained during sleep when maximum growth occurs.
Hunter-gatherers usually did not gorge on massive soft meals or on calorie-laden, nutrition-free liquids, like soft drinks. We suspect cultural traditions of thorough mastication, deliberate complete swallows, and pauses developed in circumstances where food was not normally superabundant (“chew your food thirty times, kids”). A connection of muscle use and mouth breathing to jaw development (Surtel et al. 2015) has been shown by animal experiments. It appears that a transition to softer diets disrupts the signaling system that determines appropriate orofacial structure. The negative impact on jaw development of that transition has been demonstrated in people and other mammals (Beecher and Corruccini 1981, Hinton 1993, Lieberman DE et al. 2004, Pirttiniemi et al. 2004, Bonin et al. 2007, Kingsmill et al. 2010). Nonhuman animals that had their oral posture disrupted by nose blockage or a dietary manipulation (Harvold 1968, Lieberman DE et al. 2004) showed changes in their jaws analogous to what is happening to children in industrialized societies today (Grippaudo et al. 2016, Kahn and Ehrlich 2018). Furthermore, studies of jaw size in relation to toughness and abundance of food and clinical studies in which treatment focused on muscle exercise and oral posture (how the jaws are held when not functioning) alters development of the maxilla and mandible (Wong 2018) support the environmental explanation of the jaw epidemic.
It seems that swallowing properly and chewing thoroughly, which are helpful in keeping the resting tongue and jaws in correct posture, prevented hunter-gatherers from developing long-face syndrome (Buschang et al. 2013). The spread of that syndrome may have started early in industrialization with reduction of duration of breastfeeding (Amaral et al. 2017) and weaning to liquid or near-liquid baby foods. There is evidence that extended breastfeeding reduces the chances of children having some types of malocclusion (Peres et al. 2015, Boronat-Catalá et al. 2017, Doğramacı et al. 2017) or suffering obstructive sleep apnea. This suggests that the early complex muscle use associated with breast (as opposed to bottle) feeding may be one factor in achieving the muscle tone (Huang and Guilleminault 2013) and pressures that are critical to proper oral posture and development of the maxilla and mandible.
It was not until agriculture and then, especially, industrialized food processing created the environment in which correct oral posture was often compromised that many human jaws underwent rapid shrinkage (Goose and Parry 1974, Frake and Goose 1977, Kaifu 1997, Rock et al. 2006, Rose and Roblee 2009). Agriculture and industrialization encouraged a more sedentary lifestyle, moving indoors, where ventilation rates are low and allergens are concentrated (Bornehag et al. 2005). Subsequent sending offspring to viral sinks, such as daycare centers, and other factors in civilization resulted in developed countries having 20%–25% of children under 5 suffer blockage of the nasal airway in early life (Jesenak et al. 2011). A stuffy nose automatically leads to mouth breathing and reverse swallowing, altering the shape of the jaws and face during development (Jefferson 2010). Aberrant breathing and swallowing as a consequence of infection (bacterial or viral), gastroesophageal reflux, adenoid hypertrophy (Niu et al. 2018), smoke (Bugova et al. 2018), asthma (Nava et al. 2007) and allergens (Jesenak et al. 2011, Marseglia et al. 2011, Niu et al. 2018) in early childhood affect adult jaw structure. The prevalence of pollution-emitting motor vehicles has also contributed to the worldwide increase in the frequency of allergic rhinitis (Janssen et al. 2003) and mouth breathing, as have changes to more processed and readily available foods in the human diet (Hoff et al. 2005, De Batlle et al. 2008).
Another possible contributor to the epidemic is premature spoon (utensil) feeding before a child's normal developmental system is ready for transition to adult swallowing. Spoons, forks, and chopsticks may not be iPhones, but they are technology and are being used to change the way children are raised (Brace 1986). In most industrialized societies, spoon feeding starts at around 6 months. Weaning is critical to transition from the immature or baby swallow to the adult swallow, and the method of food delivery is important in swallowing (Aytekin et al. 2014, Hernandez et al. 2019). The practice of force feeding children with spoons before they are ready likely disrupts the normal sequence of development. The only way to eat from a spoon is to slurp from it. Spoon feeding too early does not lead to the proper transition to mature swallowing; it teaches a child to suck and swallow. This is not an infantile or adult swallow; instead, it is an aberration. This is why most of the food ends up on the face when spoon feeding a 6-month-old. It seems likely that spoon feeding became common during industrialization, when mothers had to hurry and get back to work and spoon feeding was quick and easy. Even societies that traditionally use chopsticks start children on spoons (Visser 2015).
What other factors might change the way people hold their tongues and jaws at rest? The main time our jaws are at rest is when we are sleeping. If the posture hypothesis is right, function (exercise) will change the shape of the jaw, but only posture will allow for coordinated growth. In theory, a child can have balanced growth with weak muscles if it sleeps with its mouth fully closed. It can have strong muscles and also an undersized jaw if it does lots of hard chewing and breastfeeds for years (function) and if it does not sleep with its mouth fully closed. So a key change in the environment of a world settling down to practice agriculture and then industrializing may have been how people sleep, very differently from the way our primate relatives and hunter-gatherers slept—mostly on the ground (not in beds), on their sides, and without pillows. That had many postural advantages, including encouraging keeping the mouth shut (Tetley 2000). This hypothesis surely deserves more investigation, because human sleep patterns are unique among primates and are thought to have been critical to the development of human beings’ extraordinary cognitive abilities (Nunn et al. 2016). An interesting issue is the different perceptions of nighttime safety between hunter-gatherers and sedentary peoples (Musharbash 2013) and their possible impacts on sleep quality and, therefore, on jaw development.
Sadly, we lack the data to say how blame should be apportioned for the epidemic among the factors discussed above and listed in table 1. But environmentally instigated bad oral posture, we emphasize, appears to disrupt the muscular–postural guidance of facial development, leading to the jaw epidemic as first agriculture (Katz et al. 2017) and sedentariness and then industrialization spread over the world. Eating, not surprisingly, has a great impact on jaw form, as has been long recognized (Ferris 1909). The effect of loading bone with heavier mastication appears directly to affect the density and size of the structures (Lieberman DE et al. 2004, Zink and Lieberman 2016). “Both human and animal studies have reported the effect of food consistency on orofacial development, suggesting that a diet with harder textures enhances bone and muscle growth, which could indirectly lead to better mastication efficiency and potentially reduce the need for orthodontic treatment” (Le Révérend et al. 2014). However, without considering the effect of posture, it is difficult to determine the influence of chewing on the form and balance between the jaws (Kaifu 1997).
Table 1.
Changes in the orofacial-respiratory environment induced by agricultural revolution and industrialization, with possible impacts on oral posture and jaw development and health.
| Hunter-gatherer societies (physical development focus) | Industrialized societies (intellectual development focus) |
| Long breast feeding, specialized muscle use | Insufficient nursing to develop posture or to hold muscle tone |
| No bottle feeding, normal physiological delivery | Strong milk flow in bottle feeding, spoon feeding disrupts normal swallowing, Pacifiers and bottle nipple changing tongue posture |
| Wean to adult diet, baby learns what and how to eat | Baby food, pap, spoon feeding disrupts self-learning |
| “Chewy” diet, and proper swallow, encourages salivation (PH, cleaning, remineralization, first digestion, etc.) | Increasingly liquid diet, bypasses positive nutritional and developmental effects from vigorous chewing, salivation |
| Sparse populations, less viral transmission, fewer stuffy noses | Dense populations, more nasal blockage, lead to hanging mouth open at rest |
| Much time spent outside, less allergen exposure | Little time spent outside more exposure to concentrated allergens |
| Sleeping on the ground, head not pillowed | Sleeping on a mat or bed, head pillowed |
| Sleep relatively exposed to predators or enemies, snoring selected againsta | Sleep securely indoors, snoring less lethal |
| Body, nasal breathing and general posture maintained | Body, nasal breathing and general posture often ignored |
| Active outdoor living, mouth closed, predominantly nose breathers, tongue plastered on palate and teeth lightly together at rest a | Couch potato, cell phone addict, teeth kept mostly apart at rest, nose frequently blocked, mouth often hung open, tongue held low partially resting over teeth kept apart |
Note: Environmental changes possibly influencing jaw development in modern societies. Italic text represents the correct posture to provide an environment for normal jaw development. aSpeculative.
In summary, here are hypothetical evolutionary and then environmental steps to explain the origins of the jaw epidemic: a shift from sleeping in chimp-like tree nests to ground sleeping and a change of sleep posture; mouth breathing for endurance running when hunting on the savanna; a switch to a hunter diet, with reduced chewing and altered swallowing; smoke-induced respiratory distress from the use of fire; a change in mouth resting posture; a change in facial development and a reduction of jaw size; the development of speech; and postagriculture changes in living environment. See table 1.
“Genetic” causation
The overall failure of the dental community to understand the jaw epidemic is partly because “most of the theories accept genetic changes as the main or underlying cause” (Knösel et al. 2016). This persistent error can be seen in this quote on malocclusion in the respected WebMD (www.webmd.com/oral-health/guide/crooked-teeth-misaligned-bites#1): “Most often crooked teeth, overbites, and underbites are inherited traits just as the color of your eyes or size of your hands.”
The US-government-approved MedlinePlus chimes in with roughly the same view (https://medlineplus.gov/ency/article/001058.htm): “Malocclusion is most often hereditary. This means it is passed down through families.”
Orthodontics is a big and successful business, and, in an era of genetic determinism, it is convenient to blame malocclusion on genetics, avoiding the complexities of prevention. As a result, orthodontic techniques tend toward symptom management with temporary relief of aesthetic concerns—teeth straightening for teenagers, with lifelong management strategies (retainers) usually required for permanent success (Little 1999).
Some scholars, although they accept all or some of our narrative, still assert that part of the problem must be genetic or hereditary. They apparently do not realize that, because every attribute of all living organisms must to some degree be traceable to their DNA (or RNA), the statement is nonsensical. Nonetheless, some scientists continue to push partial blame for the epidemic toward genetic evolution (Punjabi 2008) while ignoring the etiology of jaw shrinkage and distortion (Powell 2009). The success of some clinical techniques to normalize jaw growth in young children (Kahn and Wong 2016, Kahn and Ehrlich 2018, Wong 2018) and abundant evidence that jaw shrinkage is a factor in both obstructive sleep apnea and the advancement of maxilla and mandible are key treatments, in addition to other surgical techniques (Sunitha and Kumar 2010, Olszewska et al. 2012). This further makes clear the largely environmental cause of the epidemic.
This confusion over etiology is a possible result of the genetic determinism (Feldman 2014) that is characteristic of much of popular science. For instance, recent genome-wide association studies (GWAS) studies aimed at orofacial issues have been focused on possible genetic factors involved in the variation in the eruption of third molars (wisdom teeth). But they in no way suggest that selection and widespread genomic evolution explain the rarity of impacted third molars in hunter-gatherers compared with their common occurrence in settled or industrialized human populations (Sullivan et al. 2016, Crittenden et al. 2017, Vukelic et al. 2017; see also box 1). Similar problems occur when “racial” differences in the occurrence of jaw-related disease are discussed. For instance, Weinstock and colleagues (2014) found that African-American children were about 20% more susceptible to pediatric obstructive sleep apnea than children of other ethnic groups. But, unhappily, possible key environmental variables such as allergen concentrations at home or the length of nursing were ignored, as were different head shapes in different human groups that could make some more susceptible to the impacts of environmental change. In short, despite the great attention paid to a possible genetic evolutionary cause of the jaw epidemic, precious little evidence of genomic change being a significant factor has been uncovered (e.g., Cruz et al. 2008, Xue et al. 2010, Mossey 2014a, 2014b, Moreno Uribe and Miller 2015, Patel and Ifzah 2016).
Box 1. Some genetic detail.
Recent attempts to find genetic contributions to craniofacial phenotypes have also used GWAS. For example, an analysis of 2329 people of European ancestry using more than 9 million single nucleotide polymorphisms (SNPs) found that 1821 SNPs across 15 genetic loci were associated with quantitatively defined aspects of facial shape (Claes et al. 2018). They found that most of these genes were active in CNCCs, a group of embryonic cells that arise at 3–6 weeks of gestation and are important in formation of the facial plan. Many of the SNPs involved were regulatory variants. It is not unreasonable that such regulatory elements can be profoundly affected by environmental conditions during development. The type of chewing or breathing could well constitute environmental effects on CNCCs that may contribute to phenotypes of the jaw (Askary et al. 2017). It is still the case, however, that the sample sizes of genetic studies of jaw morphology are underpowered relative to corresponding GWAS of such phenotypes as height and body mass index, where sample sizes of half a million are now routine. Genetic studies of malocclusion etiology have identified 4 deleterious mutations in genes, DUSP6, ARHGAP21, FGF23, and ADAMTS1 in familial class III cases. (Weaver et al. 2017). Although some of these variants may have large impacts on class III phenotypic expression, their low frequency (less than 1%) makes them unlikely to explain most class III malocclusions that can be as high as 18% of malocclusion in Chinese population for example (Hardy et al. 2012). This research also may seem to some to confirm the theory that the basic cause of widespread malocclusion lies in “genetic etiology” when, in fact, it cannot. To the contrary it is becoming increasingly clear from studies of height, mental illness, body mass index and most other complex human traits (likely including jaw configuration) that the heritable component is due to hundreds or thousands of genes each with very small effect. That militates against a sudden, near global, genetic change causing a rapid shrinkage of human mandibles and maxillae.
Suffice it to say that if there were selection pressures against big jaws, the limited number of generations (as few as 15) in which shrinkage has been observed in population samples (Luther 1993, Larsen 1995, 2006) would not be long enough for a genetic–evolutionary explanation. Anecdotally, shrinkage has been observed in one generation (Waugh 1937) or within a single individual (see figures 1 and 2). There is also discussion of the possibility that genetic drift is involved in jaw morphology. But drift is random changes in the frequency of structural genes in small populations—hardly an explanation for a unidirectional global trend in populations of millions exposed to similar environmental changes.
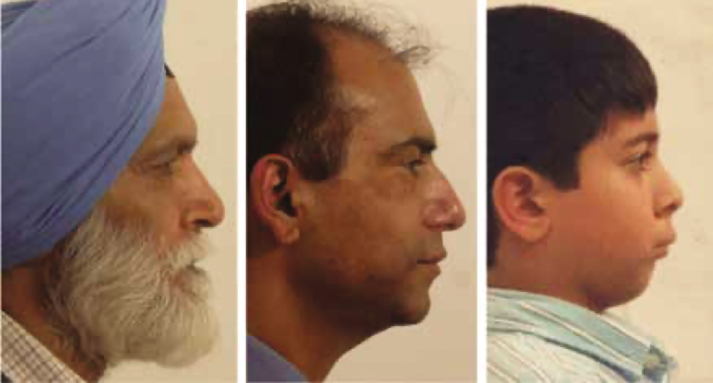
Figure 1.
Indian Grandfather born in village who had come to England as a young man with his children. Son in center. Grandchild (right) was born in industrialized society. You can see a progressive reduction in the forward dentofacial growth in the three generations. Photographs: John Mew.
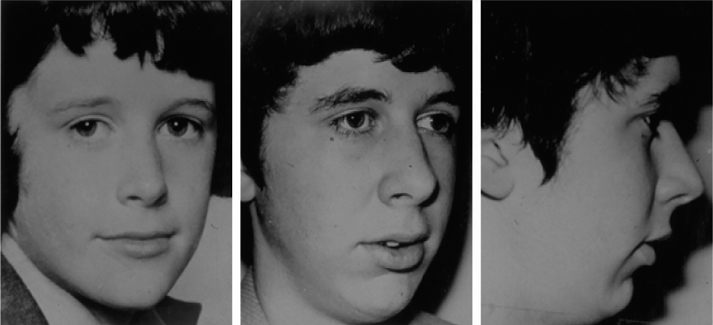
Figure 2.
Allergy can block a young person's nostrils as thoroughly as plastic plugs can block those of a rhesus monkey. Look at the consequences in the present figure for an attractive youth (left) getting a gerbil for a pet. He was allergic to the gerbil, and the resulting nasal congestion and mouth breathing redirected the growth of his jaw with sad results (center and right). Photographs: John Mew.
Treatment of individuals
Prevention is the ideal solution for parents of children with jaw development problems. The best course is probably to seek help from an orthodontist or other practitioner who works with the postural factors and have her help them to change their child's jaw resting posture. The aim is to redirect the trend in growth from the age of 3 or 4 so the jaws remain balanced by fostering a correct swallowing or resting environment. To date, there are almost no treatment approaches that aim for the prevention of jaw development problems. There are no definitive evidence-based interceptive approaches. No early intervention approaches have been proven to change skeletal growth patterns to any clinically significant degree. The focus on functional appliances (devices that attempt to change the shape of the mandible) and the correction of dysfunction have not been successful means to correct skeletal malocclusion. Schulz and colleagues (2005) and Siara-Olds and colleagues (2010) revealed that these methodologies provided a predominance of only dentoalveolar changes (altering the parts of the maxilla and mandible that evolved to hold teeth), whereas Tulloch and colleagues (1998, 2004), Flores-Mir and Major (2006a, 2006b), O’Brien and colleagues (2009), and Batista and colleagues (2018) have confirmed the elusiveness of any form of definitive methods for modification of the basal bone.
However, almost none is not the same as none. Sankey and colleagues (2000) and Mew (2004, 2015a, 2015b) showed treatment effects of clinically significant growth direction changes of basal bone.
Addressing oral posture is the common thread for each of these studies and a sound reason to direct attention and funding to testing and developing postural approaches (rather than the historical and current attention to functional approaches) for the correction of malocclusion and sleep disordered breathing.
But as we have said, for patients already suffering the stress that accompanies this epidemic through sleep disruption (of which the worst is obstructive sleep apnea), symptomatic treatments include oral appliances, the use of CPAP (continuous positive airway pressure) machines, and surgery (Liu et al. 2016, 2019).
As the role of poor oral posture as a cultural–etiological factor for malocclusion and sleep disordered breathing, is confirmed, programs such as Forwardontics and GOPex (short for good oral posture exercise; Ehrlich and Levin 2005) specifically designed to restore norms (such as table manners and linguistic patterns; MacLarnon and Hewitt 1999) that provide a natural oral environment and cure or significantly improve aberrant swallowing and other ailments can be employed in treatment of individuals (Ehrlich and Levin 2005, Ehrlich 2009).
These protocols encourage closed mouth resting posture by creating a new jaw architecture (expansion) as well as the correct breathing and, especially, swallowing patterns. The exercises focus on changing the start and end of the swallowing routine to produce the proper pressures during long rest periods. This should accompany the array of therapies being implemented to address the symptoms of the jaw epidemic. The results of treatment and posture training can be seen in figures 3 and 4.
Figure 3.
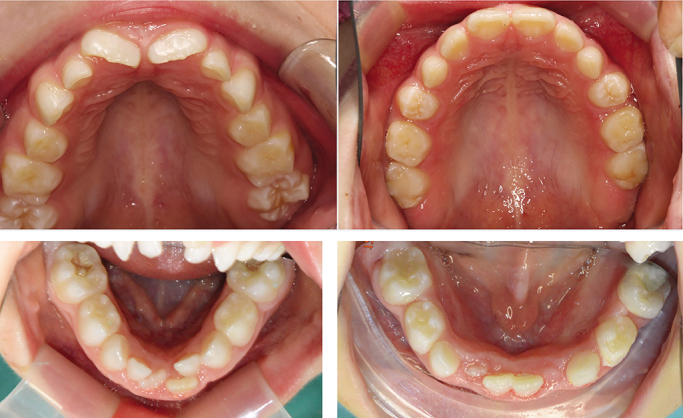
Treating children with baby dentition can help develop the jaws and improve their breathing. Note high palate on the top left (upper jaw before) and top right much flatter (after) forwardontic expansion and postural treatment. In the lower left (lower jaw before) and right (after), note there is much more space for the tongue after 3 months of treatment. Photographs: Sandra Kahn and María Jóse Muñoz.
Figure 4.
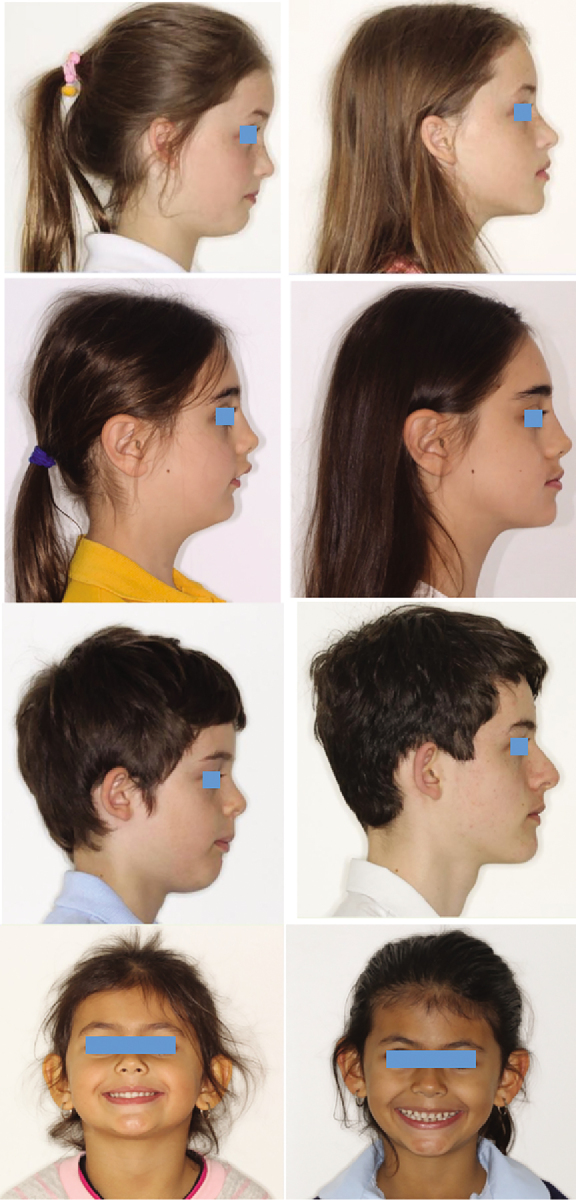
Profiles of children being treated by postural techniques. Left before, right after. Note on the bottom left child, holding chin high to keep airway open, on right normal posture, wide smile and gaps between baby teeth visible. Photographs: Simon Wong.
Poor sleep quantity or quality is stressful, and indices of activation of the physiological stress response can be induced by truncated sleep, disrupted sleep, and even the anticipation when going to sleep that it would be unpredictably disrupted (Born et al. 1999). Consonant with that, obstructive sleep apnea is fairly consistently associated with increased tone of the sympathetic nervous system (SNS; arising from increased stimulation of the SNS or decreased renal clearance of circulating catecholamines), and well as activation of the adrenocortical axis (for a review, see Meerlo et al. 2008, Bisogni et al. 2016). Moreover, the bulk of studies show that when obstructive sleep apnea is significantly countered by CPAP treatment, there are decreases in circulating catecholamine levels, blood pressure, and heart rate (for a review, see Bisogni et al. 2016). These findings constitute further evidence of the adverse downstream health consequences of the jaw epidemic.
Societal response
Problems such as the impact of premature spoon feeding on jaw development would best be dealt with by trying to change social norms. Feeding practices need to change. Utensil use needs to be timed with proper development. Spoons and pureed baby food, should not be used at 6 months when the child's first teeth are erupting but delayed to 12–18 months, when its molars come in. That time also coincides with the beginning of speech. It should become the norm to respect that timeline, and the dental community should be at the frontlines of promoting it. Other social strategies that could help reduce the impact of the jaw epidemic would be to train health professionals to reemphasize posture and table manners, encourage children not to talk while they are eating—mealtime discussions should be an important source of education. But only encourage discussion after they are 6 years old and in an appropriate place. It's been done in the past; perhaps it could be done in the future.
Promoting good eating and speaking manners may be a social animal's antidote to bad jaw growth and development. But as clinical studies show, that requires discipline to counter the social pressures of industrial society. Sadly, the cure may continue to elude society if people continue to ignore adult responsibility in this and related areas (Kahn and Wong 2016, Lustig 2017). Until such extensive social change can be entrained, there is a possible chain of action for both the avoidance of jaw shrinkage as well as mitigation of the consequences when it has occurred. Sadly, the latter may involve surgical correction of poorly developed skeletal structures. Permanent solutions invariably necessitate the modification or elimination of the habits, postural and functional, that resulted in less than optimal size and configuration for orofacial structures. The jaws, tongue, all the 32 adult teeth, including the third (wisdom) molars, and the airway develop in coordination and need to be treated as an integrated complex (as in a sense, should the entire body, including the mind) if modern environments are to be prevented from causing serious noncommunicable diseases. Early intervention (starting, ideally, in infancy) with targeted growth programs has was shown in limited clinical trials that jaw shrinkage can be avoided (Wong 2018).
This brings us to a social–institutional question: How do we increase the supply or availability of orthodontists and other practitioners who fully understand the jaw epidemic? Orthodontic professionals are the clinical facial growth experts, basing their practical techniques on the ideas of pioneers such as Angle (1907), Moss (1997), and Enlow and Hans (1996). The need to move orthodontics from symptomatic treatment of misaligned jaws and teeth to prevention has long been recognized, but nonetheless, the emphasis has remained on the symptoms rather than the etiology of disrupted oral posture, especially causes in early childhood. A sign of this misplaced emphasis is the widespread opinion among orthodontists that early treatment does not work, when their view of “early” is starting around 7 years old—about at the end of a key growth period of the human face (Scott 1954).
“As the technology of tooth movement has improved, the smaller has been the interest in the developmental aspects of the malocclusions” (Varrela and Alanen 1995). Indeed, Varrela and dental anthropologist Robert Corruccini (1984) correctly stated, “From the clinical point of view the most important element of the new perspective is that most of the malocclusions orthodontists are treating today are environmentally induced and, at least in theory, preventable. Prevention can therefore be considered as a potential alternative for active treatment.” In practice, the only “prevention” done (functional orthopedics; Fränkel and Fränkel 1983) is to use appliances in attempts to correct jaw shrinkage in 7–8-year-old children, when we believe it is already too late. We, in contrast, suggest guiding jaw growth in children as young as 2 years old,
Now is surely the time for a broad revision of dental and orthodontic training. The orthodontic profession is in trouble. As orthodontist Bill Hang quoted, “Smile Direct within 5 years will do more orthodontics than all the orthodontists in the United States combined.… Every practice will be devastated (https://vimeo.com/295502729).” Smile Direct Club is a commercial enterprise that, using techniques developed by Align Technology for straightening teeth with a series of plastic disposable devices, straightens teeth with no direct contact with a dental professional involved (https://bit.ly/2BPKKzH). One danger of this is that just moving teeth around and then necessarily holding them in place with a plastic or wire retainer may not solve problems of airway restriction that a forwardontist (an orthodontist with enhanced training when needed) could correct. Indeed, they may disguise the malocclusion symptoms of the much more serious consequences of jaw shrinkage that, as we’ve noted, include heart attacks, malignancies, learning difficulties, dementia, and death on the highway or in hospitals.
During a pandemic, less active treatments, changing habits early, and the use of remote online consultations will lower the risks to families and healthcare personal. This involves using removable appliances and minimizing personal contact and aerosol production to help to prevent contamination within the orthodontic settings. Prioritizing treatments that retrain nasal breathing and resting with mouth fully closed will very likely enhance the antiviral response against SARS-CoV-2 by engaging the filtering effect of the nose and by increasing antiviral NO levels in the airways (Martel et al. 2020).
One of the basic educational problems the jaw epidemic highlights is the lack of training in evolutionary theory, not just in medical schools but in elementary, secondary school, and college education. Not only does this lead to absurdities such as that crooked teeth are caused by genetics and the resultant expense and suffering but, more dramatically, in the miserable societal response to pesticide and antibiotic resistance. Added to this is the isolation of dentistry (at least in the United States) from medicine in general. One consequence of this isolation is the lack of orofacial data; that is, there is no equivalent of the Framingham studies (e.g., Meigs et al. 2003), and too few studies that were focused on prevention (e.g., of malocclusion incidence, braces use, sleeping positions, table manners and use of utensils in eating, environmental allergen exposure, overall posture, in relation to oral posture).
We see the future of dentistry as a respected and integral healthcare profession becoming tied to medicine and science based. Efforts must be made to increase substantive training experience in general internal medicine and biological sciences (especially evolutionary theory) for dental students. Eventually, they should play key roles in orthorhinopediatric teams that will help guard the health of young Homo sapiens.
Conclusions
Humanity is facing a series of gigantic environmental problems (Ehrlich and Ehrlich 2013), but this is one where people can do something significant individually—in particular, to help protect their children. Not enough attention is paid to the mismatch (Ehrlich and Blumstein 2018) between human genetic endowments and modern environments. Unfortunately, stunningly little attention is paid in the medical community to cause, cure, and prevention. Updating orthodontic training and dealing clinically more effectively with the jaw epidemic could be an ideal place to start changing that.
Acknowledgments
We thank Mark Cruz and two anonymous reviewers for many helpful comments. Larry Bond gave us great logistic support.
Author Biographical
Sandra Kahn is an orthodontist in private practice, Paul Ehrlich, Marcus Feldman, and Robert Sapolsky are in the Department of Biology, Stanford University, and Simon Wong is a dentist in private practice.
References cited
- Abboud F, Kumar R.. 2014. Obstructive sleep apnea and insight into mechanisms of sympathetic overactivity. The Journal of Clinical Investigation 124: 1454–1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amaral CC, da Costa VPP, Azevedo MS, Pinheiro RT, Demarco FF, Goettems ML. 2017. Perinatal health and malocclusions in preschool children: Findings from a cohort of adolescent mothers in Southern Brazil. American Journal of Orthodontics and Dentofacial Orthopedics 152: 613–621. [DOI] [PubMed] [Google Scholar]
- Angle EH. 1907. Treatment of Malocclusion of the Teeth: Angle's System. Greatly Enl. and Entirely Rewritten, with Six Hundred and Forty-One Illustrations. SS White Dental Manufacturing Company.
- Askary A, Xu P, Barske L, Bay M, Bump P, Balczerski B, Bonaguidi MA, Crump JG. 2017. Genome-wide analysis of facial skeletal regionalization in zebrafish. Development 144: 2994–3005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aytekin A, Albayrak EB, Küçükoğlu S, İ Caner. 2014. The effect of feeding with spoon and bottle on the time of switching to full breastfeeding and sucking success in preterm babies. Turkish Archives of Pediatrics 49: 307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Batista KB, Thiruvenkatachari B, Harrison JE, D O’Brien K. 2018. Orthodontic treatment for prominent upper front teeth (class II malocclusion) in children and adolescents. Cochrane Database of Systematic Reviews 3 (CD003452). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beecher RM, Corruccini RS.. 1981. Effects of dietary consistency on craniofacial and occlusal development in the rat. Angle Orthodontist 51: 61–69. [DOI] [PubMed] [Google Scholar]
- Bisogni V, Pengo MF, Maiolino G, Rossi GP. 2016. The sympathetic nervous system and catecholamines metabolism in obstructive sleep apnoea. Journal of Thoracic Disease 8: 243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blasi DE, Moran S, Moisik SR, Widmer P, Dediu D, Bickel B. 2019. Human sound systems are shaped by post-Neolithic changes in bite configuration. Science 363: eaav3218. [DOI] [PubMed] [Google Scholar]
- Bonin S, Clayton H, Lanovaz J, Johnston T. 2007. Comparison of mandibular motion in horses chewing hay and pellets. Equine Veterinary Journal 39: 258–262. [DOI] [PubMed] [Google Scholar]
- Born J, Hansen K, Marshall L, Mölle M, Fehm HL. 1999. Timing the end of nocturnal sleep. Nature 397: 29–30. [DOI] [PubMed] [Google Scholar]
- Bornehag C-G, Sundell J, Hägerhed‐Engman L, Sigsgaard T. 2005. Association between ventilation rates in 390 Swedish homes and allergic symptoms in children. Indoor Air 15: 275–280. [DOI] [PubMed] [Google Scholar]
- Boronat-Catalá M, Bellot-Arcís C, Almerich-Silla JM, Catalá-Pizarro M. 2017. Association between duration of breastfeeding and malocclusions in primary and mixed dentition: A systematic review and meta-analysis. Scientific Reports 7: 5048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bortz WM., II 1985. Physical exercise as an evolutionary force. Journal of Human Evolution 14: 145–155. [Google Scholar]
- Boyle EA, Li YI, Pritchard JK. 2017. An expanded view of complex traits: From polygenic to omnigenic. Cell 169: 1177–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brace CL. 1986. Egg on the face, f in the mouth, and the overbite. A Mericxn Anthropologist 88: 695–697. [Google Scholar]
- Bramble DM, Lieberman DE.. 2004. Endurance running and the evolution of Homo. Nature 432: 345–352. [DOI] [PubMed] [Google Scholar]
- Bresolin D, Shapiro PA, Shapiro GG, Chapko MK, Dassel S. 1983. Mouth breathing in allergic children: Its relationship to dentofacial development. American Journal of Orthodontics 83: 334–340. [DOI] [PubMed] [Google Scholar]
- Bridges S, Chambers T, Pople I. 2002. Plagiocephaly and head binding. Archives of Disease in Childhood 86: 144–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunelle J, Bhat M, Lipton J. 1996. Prevalence and distribution of selected occlusal characteristics in the US population 1988–1991. Journal of Dental Research 75: 706–713. [DOI] [PubMed] [Google Scholar]
- Bugova G, Janickova M, Uhliarova B, Babela R, Jesenak M. 2018. The effect of passive smoking on bacterial colonisation of the upper airways and selected laboratory parameters in children. Acta Otorhinolaryngologica Italica 38: 431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buschang PH, Jacob H, Carrillo R. 2013. The morphological characteristics, growth, and etiology of the hyperdivergent phenotype. Seminars in Orthodontics 19: 212–226. [Google Scholar]
- Buschang PH, Jacob HB.. 2014. Mandibular rotation revisited: What makes it so important? Seminars in Orthodontics 20: 299–315. [Google Scholar]
- Campos-Rodriguez F, Martinez-Garcia MA, Martinez M, Duran-Cantolla J, Mdl Peña, Masdeu MJ, Gonzalez M, Fd Campo, Gallego I, Marin JM. 2013. Association between obstructive sleep apnea and cancer incidence in a large multicenter Spanish cohort. American Journal of Respiratory and Critical Care Medicine 187: 99–105. [DOI] [PubMed] [Google Scholar]
- Christopherson EA, Briskie D, Inglehart MR. 2009. Objective, subjective, and self‐assessment of preadolescent orthodontic treatment need: A function of age, gender, and ethnic/racial background? Journal of Public Health Dentistry 69: 9–17. [DOI] [PubMed] [Google Scholar]
- Claes P, Roosenboom J, White JD, Swigut T, Sero D, Li J, Lee MK, Zaidi A, Mattern BC, Liebowitz C. 2018. Genome-wide mapping of global-to-local genetic effects on human facial shape. Nature Genetics 50: 414–423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corruccini RS. 1984. An epidemiologic transition in dental occlusion in world populations. American Journal of Orthodontics 86: 419–426. [DOI] [PubMed] [Google Scholar]
- Crittenden AN, Sorrentino J, Moonie SA, Peterson M, Mabulla A, Ungar PS. 2017. Oral health in transition: The Hadza foragers of Tanzania. PLOS ONE 12: e0172197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cruz RM, Krieger H, Ferreira R, Mah J, Hartsfield Jr J, Oliveira S. 2008. Major gene and multifactorial inheritance of mandibular prognathism. American Journal of Medical Genetics A 146: 71–77. [DOI] [PubMed] [Google Scholar]
- De Batlle J, Garcia‐Aymerich J, Barraza‐Villarreal A, Antó J, Romieu I. 2008. Mediterranean diet is associated with reduced asthma and rhinitis in Mexican children. Allergy 63: 1310–1316. [DOI] [PubMed] [Google Scholar]
- Doğramacı EJ, Rossi-Fedele G, Dreyer CW. 2017. Malocclusions in young children: Does breast-feeding really reduce the risk? A systematic review and meta-analysis. The Journal of the American Dental Association 148: 566–574. [DOI] [PubMed] [Google Scholar]
- Dolce C, McGorray SP, Brazeau L, King GJ, Wheeler TT. 2007. Timing of class II treatment: Skeletal changes comparing 1-phase and 2-phase treatment. American Journal of Orthodontics and Dentofacial Orthopedics 132: 481–489. [DOI] [PubMed] [Google Scholar]
- Ehrlich PR. 2009. Cultural evolution and the human predicament. Trends in Ecology and Evolution 24: 409–412. [DOI] [PubMed] [Google Scholar]
- Ehrlich PR, Blumstein DT.. 2018. The great mismatch. BioScience 68: 844–846. [Google Scholar]
- Ehrlich PR, Ehrlich AH.. 2013. Can a collapse of civilization be avoided? Proceeding of the Royal Society B 280: 20122845 http://rspb.royalsocietypublishing.org/content/280/1754/20122845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrlich PR, Levin SA.. 2005. The evolution of norms. Public Library of Science 3: 943–948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehsani S, Nebbe B, Normando D, Lagravere MO, Flores-Mir C. 2015. Dental and skeletal changes in mild to moderate class II malocclusions treated by either a Twin-block or Xbow appliance followed by full fixed orthodontic treatment. Angle Orthodontist 85: 997–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelke W, Jung K, Knösel M. 2011. Intra-oral compartment pressures: A biofunctional model and experimental measurements under different conditions of posture. Clinical Oral Investigations 15: 165–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Enlow DH, Hans MG.. 1996. Essentials of Facial Growth. Saunders. [Google Scholar]
- Evensen JP, Øgaard B.. 2007. Are malocclusions more prevalent and severe now? A comparative study of medieval skulls from Norway. American Journal of Orthodontics and Dentofacial Orthopedics 131: 710–716. [DOI] [PubMed] [Google Scholar]
- Feldman M. 2014. Echoes of the past: Hereditarianism and a troublesome inheritance. PLOS Genetics 10: e1004817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferris HC. 1909. Is your face beautiful. Western Dental Journal 23: 58–69. [Google Scholar]
- Finkel KJ, Searleman AC, Tymkew H, Tanaka CY, Saager L, Safer-Zadeh E, Bottros M, Selvidge JA, Jacobsohn E, Pulley D. 2009. Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Medicine 10: 753–758. [DOI] [PubMed] [Google Scholar]
- Flores-Mir C, Major PW.. 2006a. Cephalometric facial soft tissue changes with the Twin block appliance in class II division 1 malocclusion patients: A systematic review. Angle Orthodontist 76: 876–881. [DOI] [PubMed] [Google Scholar]
- Flores-Mir C, Major PW.. 2006b. A systematic review of cephalometric facial soft tissue changes with the activator and bionator appliances in class II division 1 subjects. European Journal of Orthodontics 28: 586–593. [DOI] [PubMed] [Google Scholar]
- Frake SE, Goose D.. 1977. A comparison between mediaeval and modern British mandibles. Archives of Oral Biology 22: 55–57. [DOI] [PubMed] [Google Scholar]
- Fränkel R, Fränkel C.. 1983. A functional approach to treatment of skeletal open bite. American Journal of Orthodontics 84: 54–68. [DOI] [PubMed] [Google Scholar]
- Fultz NE, Bonmassar G, Setsompop K, Stickgold RA, Rosen BR, Polimeni JR, Lewis LD. 2019. Coupled electrophysiological, hemodynamic, and cerebrospinal fluid oscillations in human sleep. Science 366: 628–631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson KR, Calcagno JM.. 1993. Brief communication: Possible third molar impactions in the hominid fossil record. American Journal of Physical Anthropology 91: 517–521. [DOI] [PubMed] [Google Scholar]
- Goose D. 1981. Changes in human face breadth since the Mediaeval period in Britain. Archives of Oral Biology 26: 757–758. [DOI] [PubMed] [Google Scholar]
- Goose D, Parry SE.. 1974. Palate width in skulls from a recently excavated English mediaeval site. Archives of Oral Biology 19: 273–274. [DOI] [PubMed] [Google Scholar]
- Gottlieb DJ, Yenokyan G, Newman AB, O’connor GT, Punjabi NM, Quan SF, Redline S, Resnick HE, Tong EK, Diener-West M. 2010. Prospective study of obstructive sleep apnea and incident coronary heart disease and heart failure: The sleep heart health study. Circulation 122: 352–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grippaudo C, Paolantonio EG, Antonini G, Saulle R, La Torre G, Deli R. 2016. Association between oral habits, mouth breathing and malocclusion. Acta Otorhinolaryngologica Italica 36: 386–394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guilleminault C, De Los Reyes V. 2011. Upper-airway resistance syndrome. Handbook of Clinical Neurology 98: 401–409. [DOI] [PubMed] [Google Scholar]
- Gupta MA, Knapp K.. 2014. Cardiovascular and psychiatric morbidity in obstructive sleep apnea (OSA) with insomnia (sleep apnea plus) versus obstructive sleep apnea without insomnia: A case-control study from a Nationally Representative US sample. PLOS ONE 9: e90021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall JG. 2010. Importance of muscle movement for normal craniofacial development. Journal of Craniofacial Surgery 21: 1336–1338. [DOI] [PubMed] [Google Scholar]
- Han KS, Kim L, Shim I. 2012. Stress and sleep disorder. Experimental neurobiology 21: 141–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harari D, Redlich M, Miri S, Hamud T, Gross M. 2010. The effect of mouth breathing versus nasal breathing on dentofacial and craniofacial development in orthodontic patients. The Laryngoscope 120: 2089–2093. [DOI] [PubMed] [Google Scholar]
- Hardy DK, Cubas YP, Orellana MF. 2012. Prevalence of angle class III malocclusion: A systematic review and meta-analysis. Open Journal of Epidemiology 2: 75–82. [Google Scholar]
- Harvold EP. 1968. The role of function in the etiology and treatment of malocclusion. American Journal of Orthodontics 54: 883–896. [DOI] [PubMed] [Google Scholar]
- Helm S, Prydsö U.. 1979. Prevalence of malocclusion in medieval and modern Danes contrasted. European Journal of Oral Sciences 87: 91–97. [DOI] [PubMed] [Google Scholar]
- Henderson J, Carter D.. 2002. Mechanical Induction in Limb Morphogenesis: The Role of Growth-Generated Strains and Pressures. Elsevier. [DOI] [PubMed] [Google Scholar]
- Hernandez EG, Gozdzikowska K, Jones RD, Huckabee M-L. 2019. Pharyngeal swallowing during wake and sleep. Dysphagia 34: 916–921. [DOI] [PubMed] [Google Scholar]
- Hinton R. 1993. Effect of dietary consistency on matrix synthesis and composition in the rat condylar cartilage. Cells Tissues Organs 147: 97–104. [DOI] [PubMed] [Google Scholar]
- Hoff S, Seiler H, Heinrich J, Kompauer I, Nieters A, Becker N, Nagel G, Gedrich K, Karg G, Wolfram G. 2005. Allergic sensitisation and allergic rhinitis are associated with n-3 polyunsaturated fatty acids in the diet and in red blood cell membranes. European Journal of Clinical Nutrition 59: 1071. [DOI] [PubMed] [Google Scholar]
- Huang Y-S, Guilleminault C.. 2013. Pediatric obstructive sleep apnea and the critical role of oral-facial growth: Evidences. Frontiers in neurology 3: 184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janssen NA, Brunekreef B, van Vliet P, Aarts F, Meliefste K, Harssema H, Fischer P. 2003. The relationship between air pollution from heavy traffic and allergic sensitization, bronchial hyperresponsiveness, and respiratory symptoms in Dutch schoolchildren. Environmental Health Perspectives 111: 1512–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jefferson Y. 2010. Mouth breathing: Adverse effects on facial growth, health, academics, and behavior. General Dentistry 58: 18–25. [PubMed] [Google Scholar]
- Jesenak M, Ciljakova M, Rennerova Z, Babusikova E, Banovcin P. 2011. Recurrent respiratory infections in children: Definition, diagnostic approach, treatment, and prevention. IntechOpen doi:10.5772/19422 10.5772/19422 [DOI] [Google Scholar]
- Kahn S, Ehrlich PR.. 2018. Jaws: The Story of a Hidden Epidemic. Stanford University Press. [Google Scholar]
- Kaifu Y. 1997. Changes in mandibular morphology from the Jomon to modern periods in eastern Japan. American Journal of Physical Anthropology 104: 227–243. [DOI] [PubMed] [Google Scholar]
- Kaifu Y. 2000. Temporal changes in corpus thickness of the Japanese mandibles. Bulletin of the National Museum of Nature and Science D 26: 39–44. [Google Scholar]
- Katz DC, Grote MN, Weaver TD. 2017. Changes in human skull morphology across the agricultural transition are consistent with softer diets in preindustrial farming groups. Proceedings of the National Academy of Sciences 114: 9050–9055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingsmill V, Boyde A, Davis G, Howell P, Rawlinson S. 2010. Changes in bone mineral and matrix in response to a soft diet. Journal of Dental Research 89: 510–514. [DOI] [PubMed] [Google Scholar]
- Knösel M, Nüser C, Jung K, Helms H-J, Engelke W, Sandoval P. 2016. Interaction between deglutition, tongue posture, and malocclusion: A comparison of intraoral compartment formation in subjects with neutral occlusion or different types of malocclusion. Angle Orthodontist 86: 697–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang CJ, Appleton SL, Vakulin A, McEvoy RD, Wittert GA, Martin SA, Catcheside PG, Antic NA, Lack L, Adams RJ. 2017. Co‐morbid OSA and insomnia increases depression prevalence and severity in men. Respirology 22: 1407–1415. [DOI] [PubMed] [Google Scholar]
- Larsen CS. 1995. Biological changes in human populations with agriculture. Annual Review of Anthropology: 185–213. [Google Scholar]
- Larsen CS. 2006. The agricultural revolution as environmental catastrophe: Implications for health and lifestyle in the Holocene. Quaternary International 150: 12–20. [Google Scholar]
- Le Révérend BJ, Edelson LR, Loret C. 2014. Anatomical, functional, physiological and behavioural aspects of the development of mastication in early childhood. British Journal of Nutrition 111: 403–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LeResche L. 1997. Epidemiology of temporomandibular disorders: Implications for the investigation of etiologic factors. Critical Reviews in Oral Biology and Medicine 8: 291–305. [DOI] [PubMed] [Google Scholar]
- Li X, Ren R, Zhang Y, Zhou J, Tan L, Li T, Tang X. 2018. 0673 Increased Sympathetic and Decreased Parasympathetic Cardiac Tone In Patients With Obstructive Sleep Apnea And Periodic Limb Movements During Sleep. Sleep 41: A249–A250. [Google Scholar]
- Lieberman DE. 2008. Speculations about the selective basis for modern human craniofacial form. Evolutionary Anthropology 17: 55–68. [Google Scholar]
- Lieberman D[E] 2013. The Story of the Human Body: Evolution, Health and Disease. Penguin. [PubMed] [Google Scholar]
- Lieberman DE, Krovitz GE, Yates FW, Devlin M, Claire MS. 2004. Effects of food processing on masticatory strain and craniofacial growth in a retrognathic face. Journal of Human Evolution 46: 655–677. [DOI] [PubMed] [Google Scholar]
- Lieberman DE, Bramble DM, Raichlen DA, Shea JJ. 2009. Brains, brawn, and the evolution of human endurance running capabilities. Pages 77–92 in Grine FE, Fleagle JG, Leakey RE, eds. The First Humans–Origin and Early Evolution of the Genus Homo. Springer. [Google Scholar]
- Lieberman P. 2007. Evolution of human language. Current Anthropology 48: 39–66. [Google Scholar]
- Limme M. 2010. The need of efficient chewing function in young children as prevention of dental malposition and malocclusion. Archives de Pediatrie 17: S213–S219. [DOI] [PubMed] [Google Scholar]
- Little RM. 1999. Stability and relapse of mandibular anterior alignment: University of Washington studies. Seminars in Orthodontics 5: 191–204. [DOI] [PubMed] [Google Scholar]
- Liu SY-C, Awad M, Riley RW. 2019. Maxillomandibular advancement: Contemporary approach at Stanford. Atlas of the Oral and Maxillofacial Surgery Clinics of North America 27: 29–36. [DOI] [PubMed] [Google Scholar]
- Liu SY-C, Huon L-K, Iwasaki T, Yoon A, Riley R, Powell N, Torre C, Capasso R. 2016. Efficacy of maxillomandibular advancement examined with drug-induced sleep endoscopy and computational fluid dynamics airflow modeling. Otolaryngology: Head and Neck Surgery 154: 189–195. [DOI] [PubMed] [Google Scholar]
- Lopes M-C, Spruyt K, Soster L, Da Rosa AC, Guilleminault C. 2018. Reduction in parasympathetic tone during sleep in children with habitual snoring. Frontiers in Neuroscience 12: 997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumeng JC, Chervin RD.. 2008. Epidemiology of pediatric obstructive sleep apnea. Proceedings of the American Thoracic Society 5: 242–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lustig RH. 2017. The hacking of the American mind: The science behind the corporate takeover of our bodies and brains. Penguin. [Google Scholar]
- Luther F. 1993. A cephalometric comparison of medieval skulls with a modern population. The European Journal of Orthodontics 15: 315–325. [DOI] [PubMed] [Google Scholar]
- MacLarnon AM, Hewitt GP.. 1999. The evolution of human speech: The role of enhanced breathing control. American Journal of Physical Anthropology 109: 341–363. [DOI] [PubMed] [Google Scholar]
- Marseglia G, Merli P, Caimmi D, Licari A, Labó E, Marseglia A, Ciprandi G, La Rosa M. 2011. Nasal disease and asthma. International Journal of Immunopathology and Pharmacology 24: 7–12. [DOI] [PubMed] [Google Scholar]
- Martel J, Ko Y-F, Young JD, Ojcius DM. 2020. Could Nitric Oxide Help to Prevent or Treat COVID-19? Elsevier. [Google Scholar]
- Meerlo P, Sgoifo A, Suchecki D. 2008. Restricted and disrupted sleep: Effects on autonomic function, neuroendocrine stress systems and stress responsivity. Sleep Medicine Reviews 12: 197–210. [DOI] [PubMed] [Google Scholar]
- Meigs JB, Wilson PW, Nathan DM, D’Agostino RB, Williams K, Haffner SM. 2003. Prevalence and characteristics of the metabolic syndrome in the San Antonio Heart and Framingham Offspring Studies. Diabetes 52: 2160–2167. [DOI] [PubMed] [Google Scholar]
- Mew JRC. 2004. The postural basis of malocclusion: A philosophical overview. The American Journal of Orthodontics and Dentofacial Orthopedics 126: 729–738. [DOI] [PubMed] [Google Scholar]
- Mew JRC. 2015a. The influence of the tongue on dentofacial growth. Angle Orthodontist 85: 715–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mew JRC. 2015b. Visual Comparison of Excellent Orthodontic Results with Excellent Postural Results?. Kieferorthopädie 29: 1–15. [Google Scholar]
- Montgomery P, Wiggs L.. 2015. Definitions of sleeplessness in children with attention‐deficit hyperactivity disorder (ADHD): Implications for mothers’ mental state, daytime sleepiness and sleep‐related cognitions. Child: Care, Health, and Development 41: 139–146. [DOI] [PubMed] [Google Scholar]
- Moore W, Lavelle C, Spence T. 1968. Changes in the size and shape of the human mandible in Britain. British Dental Journal 125: 163–169. [PubMed] [Google Scholar]
- Moreno Uribe L, Miller S. 2015. Genetics of the dentofacial variation in human malocclusion. Orthodontics and Craniofacial Research 18: 91–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moss ML. 1997. The functional matrix hypothesis revisited. 4. The epigenetic antithesis and the resolving synthesis. American Journal of Orthodontics and Dentofacial Orthopedics 112: 410–417. [DOI] [PubMed] [Google Scholar]
- Mossey P. 2014a. The heritability of malocclusion, part 1: Genetics, principles, and terminology. British Journal of Orthodontics 26: 103–113. [DOI] [PubMed] [Google Scholar]
- Mossey P. 2014b. The heritability of malocclusion, part 2: The influence of genetics in malocclusion. British Journal of Orthodontics 26: 195–203. [DOI] [PubMed] [Google Scholar]
- Musharbash Y. 2013. Night, sight, and feeling safe: An exploration of aspects of W arlpiri and W estern sleep. The Australian Journal of Anthropology 24: 48–63. [Google Scholar]
- Nashi N, Kang S, Barkdull GC, Lucas J, Davidson TM. 2007. Lingual fat at autopsy. Laryngoscope 117: 1467–1473. [DOI] [PubMed] [Google Scholar]
- Nava FV, Vázquez Rodríguez EM, Guevara SR, MdC Barrientos Gómez, Vázquez Rodríguez CF, Saldivar González AH, Martín JP, Ochoa DL, Almeida Arvizu VM. 2007. Effect of allergic rhinitis, asthma and rhinobronchitis on dental malocclusion in adolescents. Revista Alergia de Mexico 54: 169–176. [PubMed] [Google Scholar]
- Niu X, Wu Z-H, Xiao X-Y, Chen X. 2018. The relationship between adenoid hypertrophy and gastroesophageal reflux disease: A meta-analysis. Medicine 97 (art. e12540). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunn CL, Samson DR, Krystal AD. 2016. Shining evolutionary light on human sleep and sleep disorders. Evolution, Medicine, and Public Health 2016: 227–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien K, et al. 2009. Early treatment for Class II Division 1 malocclusion with the Twin-block appliance: A multi-center, randomized, controlled trial. American Journal of Orthodontics and Dentofacial Orthopedics 135: 573–579. [DOI] [PubMed] [Google Scholar]
- Olszewska E, Rutkowska J, Czajkowska A, Rogowski M. 2012. Selected surgical managements in snoring and obstructive sleep apnea patients. Medical Science Monitor 18: CR13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornitz DM, Marie PJ.. 2015. Fibroblast growth factor signaling in skeletal development and disease. Genes and Development 29: 1463–1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palma J-A, Urrestarazu E, Lopez-Azcarate J, Alegre M, Fernandez S, Artieda J, Iriarte J. 2013. Increased sympathetic and decreased parasympathetic cardiac tone in patients with sleep related alveolar hypoventilation. Sleep 36: 933–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel Z, Ifzah HS.. 2016. Genetics in orthodontics: A review. European Journal of Pharmaceutical and Medical Research 3: 539–545. [Google Scholar]
- Peker Y, Carlson J, Hedner J. 2006. Increased incidence of coronary artery disease in sleep apnoea: A long-term follow-up. European Respiratory Journal 28: 596–602. [DOI] [PubMed] [Google Scholar]
- Peres KG, Cascaes AM, Peres MA, Demarco FF, Santos IS, Matijasevich A, Barros AJ. 2015. Exclusive Breastfeeding and Risk of Dental Malocclusion. Pediatrics 136: e60–e67. [DOI] [PubMed] [Google Scholar]
- Pirttiniemi P, Kantomaa T, Sorsa T. 2004. Effect of decreased loading on the metabolic activity of the mandibular condylar cartilage in the rat. The European Journal of Orthodontics 26: 1–5. [DOI] [PubMed] [Google Scholar]
- Pisani L, Bonaccorso L, Fastuca R, Spena R, Lombardo L, Caprioglio A. 2016. Systematic review for orthodontic and orthopedic treatments for anterior open bite in the mixed dentition. Progress in Orthodontics 17: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell NB. 2009. Contemporary surgery for obstructive sleep apnea syndrome. Clinical and Experimental Otorhinolaryngology 2: 107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price WA. 1939 (2003). Nutrition and Physical Degeneration. Price-Pottenger Nutrition Foundation. [Google Scholar]
- Proffit WR. 1975. Muscle pressures and tooth position: North American whites and Australian aborigines. The Angle Orthodontist 45: 1–11. [DOI] [PubMed] [Google Scholar]
- Proffit WR. 1978. Equilibrium theory revisited: Factors influencing position of the teeth. The Angle Orthodontist 48: 175–186. [DOI] [PubMed] [Google Scholar]
- Punjabi NM. 2008. The epidemiology of adult obstructive sleep apnea. Proceedings of the American Thoracic Society 5: 136–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed C, Angulo FJ, Swerdlow DL, Lipsitch M, Meltzer MI, Jernigan D, Finelli L. 2009. Estimates of the prevalence of pandemic (H1N1) 2009, United States, April–July 2009. Emerging Infectious Diseases 15: 2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rock W, Sabieha A, Evans R. 2006. A cephalometric comparison of skulls from the fourteenth, sixteenth and twentieth centuries. British Dental Journal 200: 33. [DOI] [PubMed] [Google Scholar]
- Rose JC, Roblee RD.. 2009. Origins of dental crowding and malocclusions: An anthropological perspective. Compendium of Continuing Education in Dentistry 30: 292–300. [PubMed] [Google Scholar]
- Sakashita R, Kamegai T, Inoue N. 1996. Masseter muscle activity in bottle feeding with the chewing type bottle teat: Evidence from electromyographs. Early Human Development 45: 83–92. [DOI] [PubMed] [Google Scholar]
- Sankey WL, Buschang PH, English J, Owen AH III. 2000. Early treatment of vertical skeletal dysplasia: The hyperdivergent phenotype. American Journal of Orthodontics and Dentofacial Orthopedics 118: 317–327. [DOI] [PubMed] [Google Scholar]
- Schulz SO, McNamara Jr JA, Baccetti T, Franchi L. 2005. Treatment effects of bonded RME and vertical-pull chincup followed by fixed appliance in patients with increased vertical dimension. American Journal of Orthodontics and Dentofacial Orthopedics 128: 326–336. [DOI] [PubMed] [Google Scholar]
- Scott JH. 1954. The Growth of the Human Face. Sage. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sella-Tunis T, Pokhojaev A, Sarig R, O’Higgins P, May H. 2018. Human mandibular shape is associated with masticatory muscle force. Scientific Reports 8: 6042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, Hamilton GS, Dharmage SC. 2017. Prevalence of obstructive sleep apnea in the general population: A systematic review. Sleep Medicine Reviews 34: 70–81. [DOI] [PubMed] [Google Scholar]
- Sessle BJ. 2015. Orofacial Pain. Lippincott Williams and Wilkins. [Google Scholar]
- Siara-Olds NJ, Pangrazio-Kulbersh V, Berger J, Bayirli B. 2010. Long-term dentoskeletal changes with the Bionator, Herbst, Twin Block, and MARA functional appliances. Angle Orthodontist 80: 18–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Somers VK, Dyken ME, Clary MP, Abboud FM. 1995. Sympathetic neural mechanisms in obstructive sleep apnea. Journal of Clinical Investigation 96: 1897–1904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stupak HD, Park SY.. 2018. Gravitational forces, negative pressure and facial structure in the genesis of airway dysfunction during sleep: A review of the paradigm. Sleep Medicine 51: 125–132. [DOI] [PubMed] [Google Scholar]
- Sullivan A, Vukelic A, Cohen J, Perry GP. 2016. Extending genome-wide association study (GWAS) results to test classic anthropological hypotheses: Human third molar agenesis and the ‘probable mutation effect. Human Biology 89: 157–169. [DOI] [PubMed] [Google Scholar]
- Sunitha C, Kumar SA.. 2010. Obstructive sleep apnea and its management. Indian Journal of Dental Research 21: 119. [DOI] [PubMed] [Google Scholar]
- Surtel A, Klepacz R, Wysokińska-Miszczuk J. 2015. The influence of breathing mode on the oral cavity. Polski merkuriusz lekarski: Organ Polskiego Towarzystwa Lekarskiego 39: 405–407. [PubMed] [Google Scholar]
- Taylor KS, Millar PJ, Murai H, Haruki N, Kimmerly DS, Bradley TD, Floras JS. 2017. Cortical autonomic network gray matter and sympathetic nerve activity in obstructive sleep apnea. Sleep 41: zsx208. [DOI] [PubMed] [Google Scholar]
- Tetley M. 2000. Instinctive sleeping and resting postures: An anthropological and zoological approach to treatment of low back and joint pain. BMJ 321: 1616–1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomkinson GR, Lang JJ, Tremblay MS. 2019. Temporal trends in the cardiorespiratory fitness of children and adolescents representing 19 high-income and upper middle-income countries between 1981 and 2014. British Journal of Sports Medicine 53: 478–486. [DOI] [PubMed] [Google Scholar]
- Tomkinson GR, Macfarlane D, Noi S, Kim D-Y, Wang Z, Hong R. 2012. Temporal changes in long-distance running performance of Asian children between 1964 and 2009. Sports Medicine 42: 267–279. [DOI] [PubMed] [Google Scholar]
- Tregear S, Reston J, Schoelles K, Phillips B. 2009. Obstructive sleep apnea and risk of motor vehicle crash: Systematic review and meta-analysis. Journal of Clinical Sleep Medicine 5: 573–581. [PMC free article] [PubMed] [Google Scholar]
- Tulloch JC, Phillips C, Proffit WR. 1998. Benefit of early class II treatment: Progress report of a two-phase randomized clinical trial. American Journal of Orthodontics and Dentofacial Orthopedics 113: 62–74. [DOI] [PubMed] [Google Scholar]
- Tulloch JC, Proffit WR, Phillips C. 2004. Outcomes in a 2-phase randomized clinical trial of early class II treatment. American Journal of Orthodontics and Dentofacial Orthopedics 125: 657–667. [DOI] [PubMed] [Google Scholar]
- Usui K, Bradley TD, Spaak J, Ryan CM, Kubo T, Kaneko Y, Floras JS. 2005. Inhibition of awake sympathetic nerve activity of heart failure patients with obstructive sleep apnea by nocturnal continuous positive airway pressure. Journal of the American College of Cardiology 45: 2008–2011. [DOI] [PubMed] [Google Scholar]
- Varrela J, Alanen P.. 1995. Prevention and early treatment in orthodontics: A perspective. Journal of Dental Research 74: 1436–1438. [DOI] [PubMed] [Google Scholar]
- Visser M. 2015. The Rituals of Dinner: The Origins, Evolution, Eccentricities, and Meaning of Table Manners. Open Road Media. [Google Scholar]
- Vukelic A, Cohen JA, Sullivan AP, Perry GH. 2017. Extending genome-wide association study results to test classic anthropological hypotheses: Human third molar agenesis and the “probable mutation effect.” Human Biology 89: 157–169. [DOI] [PubMed] [Google Scholar]
- Walker M. 2017a. Sleep the good sleep: The role of sleep in causing Alzheimer's disease is undeniable; here's how you can protect yourself. New Scientist 236: 30–33. [Google Scholar]
- Walker M. 2017b. Why We Sleep: Unlocking the Power of Sleep and Dreams. Scribner. [Google Scholar]
- Waugh LM. 1937. Influence of diet on the jaws and face of the American Eskimo. Journal of the American Dental Association and Dental Cosmos 24: 1640–1647. [Google Scholar]
- Weaver CA, Miller SF, da Fontoura CS, Wehby GL, Amendt BA, Holton NE, Allareddy V, Southard TE, Uribe LMM. 2017. Candidate gene analyses of 3-dimensional dentoalveolar phenotypes in subjects with malocclusion. American Journal of Orthodontics and Dentofacial Orthopedics 151: 539–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstock TG, Rosen CL, Marcus CL, Garetz S, Mitchell RB, Amin R, Paruthi S, Katz E, Arens R, Weng J. 2014. Predictors of obstructive sleep apnea severity in adenotonsillectomy candidates. Sleep 37: 261–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong S-M. 2018. Craniofacial signs, symptoms and orthodontic objectives of paediatric obstructive sleep apnoea. Pages 24–37 in Liem E, ed. Sleep Disorders in Pediatric Dentistry. Springer. [Google Scholar]
- Woodside D, Altuna G, Harvold E, Herbert M, Metaxas A. 1983. Primate experiments in malocclusion and bone induction. American Journal of Orthodontics 83: 460–468. [PubMed] [Google Scholar]
- Wu M, Chen G, Li Y-P. 2016. TGF-β and BMP signaling in osteoblast, skeletal development, and bone formation, homeostasis and disease. Bone Research 4: 16009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue F, Wong R, Rabie ABM. 2010. Identification of SNP markers on 1p36 and association analysis of EPB41 with mandibular prognathism in a Chinese population. Archives of Oral Biology 55: 867–872. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Li F, Shen W, Li J, Ren X, Gu Y. 2014. Characteristics of the skeletal system of bound foot: A case study. Journal of Biomimetics Biomaterials and Tissue Engineering 19: 120. [Google Scholar]
- Zink KD, Lieberman DE.. 2016. Impact of meat and Lower Palaeolithic food processing techniques on chewing in humans. Nature 531: 500. [DOI] [PubMed] [Google Scholar]