Abstract
This article describes the study protocol for an evaluation of an innovative model of care that supports home health nurses (HHN) who serve children with medical complexity (CMC). CMC constitute a small proportion of children, but have very high need for health services, are hospitalized frequently, and account for significant proportion of pediatric healthcare expenditures. High-quality home health nursing services are important for CMC, but models of care of home healthcare, after discharge of CMC from the hospital, have not been tested. Our project aims are to develop, implement, and test a model of care, called ICollab, to improve home healthcare delivery for CMC. The ICollab model consists of collaboration between HHN, primary-care physicians and clinicians of the complex care program of a tertiary-care children's hospital in the care of CMC. In this randomized clinical trial, we will recruit 110 CMC discharged home on home health nursing services. The intervention group (n = 55) will receive the ICollab intervention for 6 months post-discharge from the hospital, in addition to usual care. Children in the control group (n = 55) will receive only usual care. Outcome measures will include healthcare utilization metrics (hospitalization rates, emergency room visit rates, and days to readmission), caregiver burden and caregiver satisfaction with home healthcare, HHN retention, and HHN collaboration with other healthcare providers. We hypothesize that ICollab will reduce healthcare utilization and caregiver burden, and improve caregiver satisfaction with home healthcare, increase HHN retention, and increase HHN collaboration with other healthcare providers. Results of this study have the potential to provide a critically needed evidence-base for interventions to improve the quality of healthcare delivery for CMC. This study is registered on clinicaltrials.gov (NCT03978468) and is ongoing.
Keywords: Children, Medical complexity, Home health nursing, Collaborative healthcare model, Clinical trial
Abbreviations: ACO, Accountable Care Organizations; BCH, Brenner Children's Hospital; CAPHONQ, Caregiver Assessment of Pediatric Home Health Nursing Quality; CMC, Children with Medical Complexity; EMR, Electronic Medical Record; ER, Emergency Room; HHN, Home Health Nurses; ICC, Intraclass Correlation; PCP, Primary Care Physician; IRB, Institutional Review Board; PDN, Private Duty Nursing; PECP, Pediatric Enhanced Care Program; RCT, Randomized Controlled Trial
Highlights
-
•
The quality of home health nursing services for children with medical complexity in the U.S. is not optimal.
-
•
Models of care that optimize collaboration between home health nurses and other providers have not been previously tested.
-
•
This RCT will evaluate the effect of an innovative care model on children-, caregiver-, and home-health-nurse-level outcomes.
1. Introduction
Children with medical complexity (CMC) are a subgroup of children with high need for health services [1]. Also referred to as children with complex chronic conditions, technology-dependent children, or medically fragile children, CMC have conditions that involve multiple organ systems and encompass conditions such as genetic disorders, extreme prematurity, perinatal ischemic encephalopathy, trauma, infection, degenerative or autoimmune disorders, and malignancy. Although CMC are at risk of early death, due to advances in medical care and technology, CMC overall are living longer [[2], [3], [4]]. CMC constitute <1% of all children, and yet account for 33% of healthcare expenditures for children [5]. CMC account for more hospitalizations and hospital days of all children compared to a decade ago [6], and make up a very large proportion of readmissions to children's hospitals in the U.S [7].
The numbers of CMC receiving complex medical care at home has steadily increased [8] and more CMC are being discharged to home care [9]. Some CMC receive home health nursing as part of home care services, either intermittently (nursing visits) or continuously (private-duty nursing (PDN)) by a licensed home health nurse (HHN) at the recipient's home. Parents/caregivers of CMC have reported that the quality of home healthcare delivered to CMC at home by HHN is variable and not always of high quality [10]. HHN may not always have the skills and clinical support necessary to provide good-quality care for CMC at home [[10], [11], [12], [13]]. Poor-quality home healthcare has negative consequences for CMC and contributes to caregiver burden [10].
Fragmentation of care is particularly problematic when CMC transition from hospital to home healthcare, and contributes to higher readmissions for this population [14,15]. Different models of comprehensive care for CMC have been evaluated in clinical trials before [[16], [17], [18]]. Post-discharge interventions in pediatrics have also been described [[18], [19], [20]]. However, studies focused on transitioning CMC from hospital to home healthcare are limited. To address the gaps in care delivery for CMC at home after they transition from the hospital, we developed an innovative, collaborative model of care involving HHN, primary-care physicians (PCP), and hospital-based providers.
1.1. Conceptual framework for the intervention model
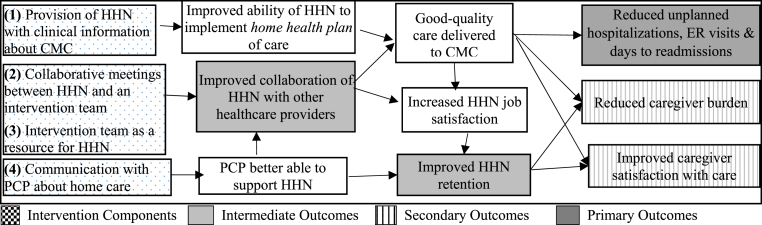
Based on data from our research [10,21,22] and that of others [[23], [24], [25]] we developed the Inter-agency Collaboration (ICollab) intervention model (Fig. 1) to improve home healthcare for CMC after their discharge from the hospital. The ICollab intervention is administered by an intervention team that includes a nurse clinician (ICollab Nurse) and a pediatrician (ICollab Physician) from the complex care program of the academic tertiary-care children's hospital. There are 4 complementary components to the model: (1) The nurse clinician provides HHN with relevant clinical information related to the child (recommendations from clinic and emergency room (ER) visits, and discharge summaries), (2) the entire intervention team engages with HHN in collaborative meetings, (3) the ICollab Nurse assists HHN with their clinical problem-solving; and (4) team members provide clinical information to PCPs, so they too can be a resource for HHN. Together these components are hypothesized to improve care through two pathways: (1) ensuring that HHN have the clinical information that is needed to provide care for CMC, and (2) fostering collaboration between HHN and other clinicians in clinical problem-solving.
Fig. 1.
Conceptual Framework of the ICollab model.
1.2. Specific aims and hypotheses
The Specific Aims of this project, developed based on the conceptual framework in Fig. 1, are to: (1) Implement ICollab for CMC for 6 months after discharge from the hospital. (2) To compare the effectiveness of ICollab plus usual care vs. usual care in reducing healthcare utilization – hospitalization and ER visit rates, and days to readmission. (3) To compare the effectiveness of ICollab plus usual care vs. usual care in reducing caregiver burden, improving caregiver satisfaction in home healthcare, improving HHN retention, and fostering better HHN collaboration with other providers caring for CMC.
Hypotheses
ICollab plus usual care, compared to usual care, will reduce hospitalizations and ER visit rates, increase time to readmission, reduce caregiver burden, improve caregiver satisfaction in home healthcare, improve HHN retention, and foster better collaboration among providers caring for CMC.
2. Methods
2.1. Intervention trial
2.1.1. Study design
We are using a randomized controlled trial (RCT) trial design to study the effectiveness of ICollab. The intervention group (n = 55) will receive ICollab plus usual care; the control group (n = 55) will receive usual care only. This clinical trial is registered in clinicaltrials.gov (NCT03978468).
2.1.2. Setting
This study is being conducted in the inpatient and outpatient settings of Brenner Children's Hospital (BCH), a tertiary care children's hospital within the Wake Forest Baptist Health system in Winston-Salem, North Carolina. Recruitment began on November 4, 2019.
2.1.3. Inclusion and exclusion criteria
Only CMC who are discharged home with PDN are included. CMC are defined as: (1) child <18 years of age; and (2) presence of a chronic condition, defined as a health condition expected to last ≥ 12 months; and (3) complexity of the condition, defined as needing ongoing care with ≥5 sub-specialists (e.g. gastroenterologist, neurologist etc.) or services (e.g. physical therapy, psychology etc.) or dependent on ≥ 1 medical technology (e.g. gastrostomy, oxygen, tracheostomy, ventilator, etc.). Children who will turn 18 during the intervention period are excluded to avoid having to re-consent with adult informed consent forms. Children who do not have at least 3 sub-specialists within the Wake Forest Baptist Health system, receive skilled nursing visits or personal care services only, are discharged to a long-term care facility or to a foster home, or whose caregivers do not speak English/Spanish, are excluded.
2.1.4. Usual care
At BCH, hospital-based physicians write home health orders that are communicated to the home health agency. Home health agencies employ HHNs and the clinical managers who supervise HHNs. The clinical manager uses the home health orders to develop the federally-mandated Home Health Certification and Plan of Care (Form CMS-485) [26] and communicates the plan to the agency's HHNs. Similar to many other tertiary care children's hospitals, BCH has a complex care program for children called the Pediatric Enhanced Care Program (PECP). PECP's staff prepare caregivers for home care, coordinate follow-ups appointments with community providers, and address the practical needs of children (e.g. transportation). Direct communication with HHN is not part of usual care.
2.1.5. Intervention (ICollab)
ICollab is administered for 6 months after discharge of the child from the hospital, by an intervention team of a nurse (ICollab Nurse) and a physician (ICollab Physician). The intervention period covers only the time when the child is at home. Thus for children who are readmitted during the intervention period, the total “home care period” will be longer than 6 months. In those cases, the intervention will be administered up to a maximum of 9 months of home care period. The 4 components of ICollab are:
2.1.5.1. Component 1: communication with HHN about clinical information
The ICollab Nurse identifies and contacts the child's HHN, and tracks the child's clinic and ER visits at BCH whenever a visit occurs (or at least twice monthly) using information in the electronic medical record (EMR). The ICollab Nurse reviews the clinic and ER visit notes for clinicians' recommendations, and develops a Clinical Summary in a structured format.
2.1.5.2. Component 2: collaborative meetings
The intervention team meets with HHNs to discuss each child's case monthly. As such, each child is scheduled for discussion 6 times during the intervention period. These meetings are in the form of “collaborative rounds” by phone. The ICollab Nurse coordinates meeting times with HHNs whose clients are being discussed. Prior to the meeting, the ICollab Nurse solicits HHNs' concerns about the case. Approximately 2 days prior to the meeting, the ICollab Nurse sends the Clinical Summary to the ICollab Physician for review. The ICollab Physician generates discussion questions based on the review of the Clinical Summary and prior meeting notes. During the meetings, clinical issues that arise are discussed and HHN concerns about the care of the child are addressed. If HHNs have concerns or need additional resources (e.g. input from the PCP, subspecialists, equipment provider, etc.), a plan for addressing these is developed. The ICollab Physician develops detailed meeting notes that includes specific action items. This is reviewed by the ICollab Nurse. The ICollab Physician documents the finalized Clinical Summary and meeting notes in the child's EMR, and shares them with the PCP by routing the note through the EMR or faxing the note. The Clinical Summary and meeting notes are sent to the child's residence for child's HHNs to review. Each HHN is given a $20 incentive for participating in a meeting.
2.1.5.3. Component 3: Intervention team as a resource for HHN
The ICollab Nurse is available as a resource for the HHN during regular work hours by cell phone or email for clinical problem solving. The ICollab Nurse addresses the concerns of the HHN, discusses with the ICollab Physician, or contacts other clinicians if needed and provides guidance to HHNs.
2.1.5.4. Component 4: communication with PCP
The ICollab Physician contacts the child's PCP, introduces the study, and offers her contact information for clinical problem solving about the child. The ICollab Physician communicates with the PCP about the plan developed in the ICollab meetings. The ICollab Nurse communicates any changes to the plan of care after clinic or ER visits, and whenever there is information about the child to be shared. The ICollab Physician is available for the PCP to problem-solve about care of CMC.
2.1.6. Recruitment and enrollment
We plan to enroll 110 CMC in the study: approximately 55 each into the intervention and control arms over an 18-month period.
Flyers about the study were developed in English and Spanish, and are placed in inpatient neonatal and pediatric and intensive care, and pediatric acute care units. The ICollab Nurse screens children for eligibility from 2 sources: (1) reviewing a list in the EMR of hospitalized children who are enrolled in PECP, (2) attending interdisciplinary meetings in the neonatal intensive care and inpatient units approximately 2–3 times/week.
Once deemed eligible, the ICollab Nurse approaches the child's primary caregiver, explains the study, and obtains written informed consent. Spanish-speaking caregivers are enrolled by one of the bilingual PECP staff.
2.1.7. Randomization
Random assignments are made by the biostatistician (EI). A block randomization is created to ensure equal accrual to each arm. We will stratify each block to try to achieve an approximate balance within each block across the intervention and control groups based on the status of home health nursing services (new vs. established). No accurate prevalence data are available on the proportion of CMC discharged home with home health nursing services for the first time vs. already established services. Hence, we will use a sequentially adjusted randomization scheme for each block to achieve approximate balance [27]. By starting with an estimate of prevalence of new vs. established home health from the previous wave of children enrolled, the scheme will adjust the probability of assignment of a newly enrolled child to the control or intervention group based on the home health nursing status. To ensure that randomization is unpredictable to the intervention team, the process will employ differing block sizes.
2.2. Outcomes evaluation
2.2.1. Observation period
The beginning of the observation period is 30 days after discharge from the index hospitalization. For some CMC, especially who are new to home health nursing, it takes a few weeks to establish home health nursing services. This results, in some cases, not being able to start the intervention immediately after discharge from the hospital. The end of the observation period is after 6 months of “home care period” up to a maximum of 9 months after discharge from the hospital.
2.2.2. Outcome measures (Table 1)
Table 1.
Study measures.
| Measures | Data Source | |
|---|---|---|
| Primary Outcomes | ||
| Hospitalization rate | Total number of hospitalizations/100 child-years | TDW data supplemented with hospitalization and ER visit data in Caregiver Month 1–5 & Final surveys |
| ER visit rate | Total number of ER visits/100-child years | |
| Days to readmission | Number of days between date of discharge from index and first unplanned hospitalization | |
| Secondary Outcomes | ||
| Caregiver burden | Change in Impact on Family Scale | Part of Caregiver Month 1 & Final survey |
| Satisfaction with home healthcare | Change in Caregiver Assessment of Pediatric Home Health Nursing Quality | Part of Caregiver Month 1–5 & Final survey |
| Intermediate Outcomes | ||
| HHN retention | HHN turnover rate (number of monthly HHN separations/number of HHN assigned) | Questions in Caregiver Month 1–5 & Final survey |
| HHN collaboration | Improvement in rating of “excellent”/“very good” vs. others | Question in Caregiver Month 1–5 & Final survey |
| Covariates – Child-level Characteristics | ||
| Age | Years | Questions in baseline Caregiver survey |
| Household residence | Rural vs. urban | |
| Race/ethnicity | Race/ethnicity categories | |
| Propensity Score – Home health agency Characteristics | ||
| Number of children served, ratio of pediatric clients to total number of clients, number of HHN trained in pediatrics, length of agency's existence | Questions in Home health agency survey (baseline) | |
| Measurement of Dose of Implementation | ||
| Dose Score | Number of HHN and PCP encounters with the intervention team | Encounter logs, Meeting Record Form |
ER: emergency room; HHN: home health nurse; PDN: private-duty nursing; TDW: Transitional Data Warehouse – Wake Forest Health Sciences' electronic tool to query child's healthcare utilization data
2.2.2.1. Primary outcome measures - healthcare utilization metrics
2.2.2.1.1. Rate of hospitalizations/100-child years
We will compare the rate of hospitalizations/100-child years between the intervention and control groups. Number of hospitalizations during the observation period will be counted and the hospitalization rate will be calculated as:
This measure is similar to that used by Mosquera et al. in the RCT of care coordination program versus usual care [16]. Using data from the institution's data warehouse (Section 2.4.1) and that from monthly caregiver surveys (Section 2.4.2), total number of hospitalizations will be calculated for each child. Planned admissions will be excluded.
2.2.2.1.2. Rate of ER visits/100 child years
Rate of ER visits will be calculated for the intervention and control groups as follows:
This measure is similar to that used in the study by Mosquera et al. [16] The data source, observation period, and comparisons will be similar to those in Section 2.2.2.1.1 above.
2.2.2.1.3. Days to first readmission
Days to first readmission will be calculated as the duration between the start of the observation period and the date of admission for the subsequent hospitalization.
2.2.2.2. Secondary outcome measures
2.2.2.2.1. Caregiver burden
Change in caregiver burden will be measured using the Impact on Family Scale-Revised, which has 15 items and 4 domains – financial, family/social, personal strain, and mastery [28]. Scores range from 15 to 60; the lower the score, the greater the impact. The Impact on Family Scale is a validated measure and used extensively in pediatric health-services research.
2.2.2.2.2. Caregiver satisfaction with home healthcare
Caregiver satisfaction with home healthcare will be compared between the 2 groups. Measures of satisfaction with home healthcare are limited and pediatric-specific measures are lacking. Hence, we developed a new survey called the Caregiver Assessment of Pediatric Home Health Nursing Quality (CAPHONQ). CAPHONQ is a 22-item measure with scores ranging from 1 (worst) to 10 (best) rating of health nurse quality. We evaluated the content validity and the test-retest reliability of CAPHONQ with caregivers of 22 CMC receiving PDN. We will use CAPHONQ in this clinical trial to assess caregiver satisfaction with home healthcare.
2.2.2.3. Intermediate outcome measures
2.2.2.3.1. HHN retention
Staff retention will be measured as turnover rate during the observation period using data from monthly and final caregiver surveys. High HHN turnover indicates low retention, and vice versa:
We pilot tested the caregiver survey in 10 caregivers of CMC who receive PDN. This survey included questions about HHN assigned and separated. CMC had a median of 3 HHN assigned; in 2 cases one HHN each was dismissed by the caregiver. The median turnover rate was 6% (range: 0%–33%). We will use a similar strategy to calculate HHN turnover in the 2 groups.
2.2.2.3.2. HHN-healthcare provider collaborations
Improvement in caregiver perception of collaboration between HHN and other healthcare providers during the study period will be compared for the 2 groups. There is no validated instrument to measure collaboration. We adapted the question about collaboration that we used in a previous study [29] for caregiver use and pilot tested it (Section 2.2.2.3.1). HHN collaboration with other healthcare providers was reported as “excellent” or “very good” by 5 out of 10 caregivers (50%). We will use this question in this clinical trial to assess caregiver perception of collaboration between HHN and other healthcare providers.
2.2.3. Outcome analysis
2.2.3.1. Power calculations
For power calculation, rate of hospitalizations will be the primary outcome. The baseline for CMC in our institution for this metric is 135/100 child-years. A power analysis was conducted based on the following assumptions: significance level of two-sided test α = 0.05; and number of children = 110 (55 in the intervention and control groups). The study by Mosquera et al. showed that comprehensive care resulted in a 50% reduction in rate of hospitalizations from 131 to 69/100 child-years compared to usual care [16]. The standard deviation for the control group (usual care) in this study was approximately 17 so the effect size was approximately (131–69)/17 = 3.65, a substantially large effect by Cohen's criterion. Since several children may be served by the same home health agency, clustering of participants within agencies is a possibility. There is no literature on the extent of clustering of CMC within a home health agency. The intraclass correlation (ICC) is often used to quantify the extent of clustering and the following values were used for power calculation for a two-level cluster randomized trial (level 1 = child, level 2 = agency): 0.0, 0.01, 0.05, and 0.1. The detectable effect sizes at 80% power are respectively 0.97, 1.08, 1.20, and 1.35. In the calculation we assumed that for each arm, there are 9 families within an agency, and a total of 6 agencies. Thus, the study should have power to detect an effect size less than half of that found in the study by Mosquera et al. Estimates of power calculations were done using the program Optimal Design v3.01 [30]. Since 3 primary outcomes will be reported, we will use the Benjamini & Hochberg (BH) procedure [31] according to the guideline described previously for adjustment for multiplicity [32]. The BH procedure is less conservative than the commonly used Bonferonni adjustment and retains statistical power [33].
2.2.3.2. Statistical analysis
We will use intention-to-treat analysis. Data analysis will include (1) descriptive statistics and visualization, and (2) multi-level modeling. Descriptive statistics and visualization for outcome variables include means, standard deviations, and ranges for continuous dependent variables (rate of hospitalizations and ER visits, and days to readmission). Two-sample t-tests for continuous variables and chi-squared tests for categorical variables will be used in bivariate analyses for evaluating the effect of intervention. Descriptive analyses are intended for both quality checking and for achieving a broad, intuitive understanding of the data.
Multi-level linear regression analysis will test the primary hypothesis that ICollab is effective in reducing hospitalization rates, ER visits, and days to readmission. Relative risk of hospitalization between the intervention and control groups will be the quantity of interest. To account for the clustering effects due to participants being recruited from same home health agencies, outcomes will be analyzed using 2-level linear model, in which CMC characteristics form the first level and the agency characteristics form the second level. The 2-level model is similar to standard regression models except that it accounts for possible clustering effects of CMC within the same agency.
Although the intervention is randomized, bias due to imbalance across the groups is a possibility. To account for confounding due to imbalance based on child characteristics, child-level variables - child's age, race/ethnicity, and residence, will be used as first level covariates in the model. To account for confounding due to imbalance at the agency level, propensity scores will be created using agency characteristics – numbers of pediatric patients who are clientele, number of pediatric HHNs, ratio of pediatric PDN clients to overall clientele, and how long the agency has existed (in years). Propensity scores will then be included as weights in the analyses of outcomes in the multilevel model [34]. Besides the main effects analysis, we will perform subgroup analysis of the effects of the intervention on the outcomes for categories of the following variables: home health status (new versus established), dose of intervention (Dose Score as described in Section 2.3.1, race/ethnicity categories, and residence (rural vs. urban). We will use two-sided test at the level of α = 0.05 for all statistical hypothesis testing.
2.2.4. Attrition from death and loss to follow-up
Our experience shows that attrition rates from loss to follow-up are minimal. Deaths of children do pose a threat to study validity; however when deceased children are included in the analyses, outcomes will be calculated up to the point of death. Deceased children may have more frequent hospitalizations before death, thus biasing the results. We will therefore analyze the data both including and excluding deceased children. In the case of excluding deceased children, we expect power to be reduced. At ICC = 0, and 0.1, and a death rate of 20%, power at the above specified detectable effect size at 80% would decrease to approximately 70%.
2.3. Process evaluation
Process evaluation has 3 distinct purposes: 1) to evaluate the fidelity with which the ICollab model has been implemented; 2) to measure the “dose” of intervention (Dose Score) that each child receives; and 3) to improve the design and implementation of the ICollab model based on the experiences and recommendations of those who are implementing the model. Of these 3, only the measure of Dose Score is discussed further in Section 2.3.1 because it relates to outcome evaluation testing.
2.3.1. Measuring dose of intervention (Dose Score)
We focus primarily on the overall degree to which the ICollab intervention was carried out according to design (i.e., across all 55 patients), on a child-by-child basis. Some HHNs may be less inclined to contact the intervention team, or participate at the collaborative meetings. If so, children cared for by those HHNs will be receiving less of the ICollab intervention. We will incorporate this variability into the outcome evaluation by treating dose as a predictor variable (Dose Score) in the analysis of healthcare utilization, caregiver burden, and caregiver satisfaction. Patients who receive a higher dose of the ICollab intervention would be expected to show a greater effect.
Dose of intervention will be assessed using the following 2 indicators: (1) Number of encounters of HHN with the intervention team: This is the total number of encounters all HHN assigned to the child's case have with the intervention team. This includes attendance in meetings and phone calls to/from HHN to the intervention team. (2) Number of encounters of PCP: It is possible that PCPs may contact the intervention team members for assistance with coordination of care or the intervention team may contact PCPs. These encounters will be captured in the logs maintained by the intervention team. We will measure dose of intervention for each participant in the intervention group. We will transform the data into z-scores and aggregate across the different indicators to create an overall Dose Score for each child. Depending on the distribution of the dose variable, we will either treat it as a continuous or as a categorical measure with low vs high implementation categories.
2.4. Data collection (Table 1)
2.4.1. Healthcare utilization data
We will obtain healthcare utilization data from enrollment through the observation period from the institution's research data warehouse. Data collected will include date of birth, dates of admission and discharge for each hospitalization, and dates of ER visits. We will use these data to calculate healthcare utilization outcomes. To capture hospitalizations and ER visits outside of BCH, we will add data about hospitalizations and ER visits from monthly and final caregiver surveys.
2.4.2. Caregiver surveys
A baseline survey is administered to caregivers of CMC using an in-person/phone interview after enrollment. Demographic information of the child and primary caregiver are obtained. The Impact on Family Scale-Revised [28] is administered at baseline and Month 1. Brief monthly surveys are administered inquiring about hospitalizations and ER visits outside of BCH, HHN turnover, and number of hours per week of receipt of PDN in the month prior to the survey. The CAPHONQ survey is administered as part of the monthly and final surveys.
The final caregiver surveys will be administered at the completion of the observation period (6 months of home care or 9 months after discharge from the index hospitalization, whichever comes first). The survey will inquire about the burden of coordinating care, satisfaction with home healthcare, and perceived collaboration between HHNs and other healthcare providers caring for CMC. To assess caregiver burden and satisfaction with home healthcare, the Impact on Family Scale-Revised and CAPHONQ respectively will be repeated. Items to measure perceived HHN collaboration with healthcare providers will be included. Caregivers will receive $20 and $10 incentives for completed baseline or final surveys and monthly surveys, respectively. For Spanish-speaking families, surveys will be conducted in Spanish.
2.4.3. Home health agency survey
Each home health agency has an organizational structure with multiple offices serving a small geographic area. Each office serves as a clinical unit with its own set of HHNs and clientele. When a child is enrolled, the research associate will query the relevant agency office about its duration of existence; geographic area covered; and number of HHNs employed, clients served, pediatric clients, and children receiving PDN.
2.4.4. Encounter logs
The ICollab Nurse and the ICollab Physician document all encounters with HHNs and PCPs of all children enrolled in the study. This encounter log will include dates and descriptions of intervention team members’ contact with HHNs, and vice versa. Data in the encounter log is used to calculate the Dose Score.
2.4.5. Meeting records
Using a meeting record form, data about HHNs’ participation in ICollab meetings are collected. This data will be used to calculate the Dose Score (Section 2.3.1).
2.5. Human subject research
The Institutional Review Board (IRB) of Wake Forest Health Sciences approved this study. Written informed consent is obtained from caregivers using the IRB-approved Informed Consent Forms prior to enrollment. Spanish consent forms are used for Spanish-speaking caregivers. Assent is obtained from children 7 years or older and can understand the assent process. For recruiting HHN and PCP to participate in the intervention, verbal consent is obtained.
3. Discussion
3.1. Study limitations and alternate strategies
3.1.1. Recruitment
We are using the strategies that were successful in our prior research studies (e.g. incentives, leveraging relationships) to recruit caregivers and HHN. Individuals participate in research studies that are meaningful to them [21]. Caregivers and HHN told us that interventions such as the one proposed are needed to improve the care of CMC.
3.1.2. Attrition
In our care coordination programs, attrition is very low since caregivers value the intervention. Although children in the control group will not receive the intervention, they will receive care coordination services (usual care) throughout the intervention period that is likely to reduce attrition. The ICollab model depends on participation of HHN in ICollab activities. Home health agencies were enthusiastic about participating in the study. We are providing incentives for HHN participating in ICollab meetings and scheduling ICollab meetings at times convenient to them. These strategies are likely to help maintain HHN participation throughout the intervention period.
3.1.3. Survey response
To enhance survey responses of participants, we are using our previously successful strategies, such as incentivizing and administering surveys by staff who built relationships with the caregiver/HHN/PCP. In our community program, the response rate for caregiver survey was 92% without incentives.
3.1.4. Contamination
Children enrolled in the study will receive services of the complex care program as part of usual care. This could potentially contribute to contamination. However, none of the intervention components is part of usual care offered by the complex care program. HHN of a child enrolled in the control group may have had a prior interaction with the ICollab Nurse which may contribute to contamination. We will use intention-to-treat analysis to evaluate outcome measures.
3.1.5. Intervention
Since this is a complex intervention and its success may depend on the intervention team, we will standardize procedures by developing and refining the ICollab manual and conducting a systematic process evaluation.
3.1.6. Bias
The nature of the intervention requires interaction of study participants with the intervention team. Hence, it is not possible to blind caregivers, HHNs, PCPs, and survey data collectors to the intervention. However, the primary outcome, hospitalization rate, is unlikely to be affected by caregivers' and data collector's knowledge about the intervention.
3.1.7. Generalizability
ICollab was designed and implemented based on our clinical and research experience. The model will have to be adapted when replicating in new settings. CMC are a heterogeneous group, but all children in this study receive PDN. Hence, the study findings are generalizable to CMC discharged with PDN in other locations, but not generalizable to those who do not receive PDN. There is considerable state and regional variability in organization of home healthcare. Hence, the study needs replication in other centers, especially in other states or regions.
3.1.8. Real-world application
We provide incentives to HHN to attend collaborative meetings. Existing policies do not reimburse HHN for their participation in collaborative clinical activities with other clinicians (i.e. participating in meetings, clinic visits etc.), limiting the application of study findings to actual clinical settings. However, study results will provide an evidence base for a collaborative model of care. If results demonstrate effectiveness of ICollab, we will disseminate study results to healthcare policy makers to effect policy changes for home healthcare services.
3.1.9. Impact due to the coronavirus pandemic
All research activities at Wake Forest Baptist Health were paused due to the coronavirus pandemic. As a result, children in the intervention arm did not receive ICollab as of March 13, 2020. We anticipate that these children may have different healthcare experiences compared to children enrolled during the coronavirus pandemic. When analyzing results of this trial, we will do a sub-group analysis of children enrolled before/during the coronavirus pandemic.
3.2. Impact
Improving the healthcare of people with multiple chronic conditions is a strategy to improve the U.S healthcare system [35]. Creating evidence-based programs that offer high-quality and integrated care is one of the recommendations to improve care of people with multiple comorbidities. Our study has the potential to provide the evidence-base for an integrated model of care and the results will improve the health infrastructure and system of care for a subgroup of children [36]. The Affordable Care Act dedicated several demonstration programs to improve care delivery through development of Accountable Care Organizations (ACO). The Partnership for Patients program is a program specifically designed to better coordinate patients’ transitions from the hospital to other settings [36]. Results of the proposed study will (1) support development of an intervention model that can be used to create a component of an ACO model of care in the future; and (2) provide strategies for reduction of readmissions and other healthcare utilization metrics as a means to reduce healthcare costs, a recent focus for policy makers in the U.S. Additionally, our study has the potential to improve the healthcare of CMC, reduce caregiver burden, and improve the system of care for children.
Funding
This project is supported by the Health Resources & Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under R40MC32754 MCH FIRST Program (PI: Nageswaran). This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
Declaration of competing interest
We confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
Acknowledgement
We thank Ms. Vanessa Ortiz and Ms. Aura Rosado for obtaining informed consents and administering caregiver surveys for Spanish speaking families. We thank Dr. Megyn Sebesta, DO, Ms. Andrea Radulovic RN BSN MPH, Ms. Krista Ennis, RN BSN, Ms. Aura Rosado, MSW and Ms. Vanessa Ortiz for providing care for children enrolled in the study.
References
- 1.Cohen E., Kuo D.Z., Agrawal R. Children with medical complexity: an emerging population for clinical and research initiatives. Pediatrics. 2011;127(3):529–538. doi: 10.1542/peds.2010-0910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murphy S.L., Mathews T.J., Martin J.A., Minkovitz C.S., Strobino D.M. Annual summary of vital statistics: 2013-2014. Pediatrics. 2017;139(6) doi: 10.1542/peds.2016-3239. [DOI] [PubMed] [Google Scholar]
- 3.Feudtner C., Hays R.M., Haynes G., Geyer J.R., Neff J.M., Koepsell T.D. Deaths attributed to pediatric complex chronic conditions: national trends and implications for supportive care services. Pediatrics. 2001;107(6):E99. doi: 10.1542/peds.107.6.e99. [DOI] [PubMed] [Google Scholar]
- 4.Feudtner C., Christakis D.A., Zimmerman F.J., Muldoon J.H., Neff J.M., Koepsell T.D. Characteristics of deaths occurring in children's hospitals: implications for supportive care services. Pediatrics. 2002;109(5):887–893. doi: 10.1542/peds.109.5.887. [DOI] [PubMed] [Google Scholar]
- 5.Cohen E., Berry J.G., Camacho X., Anderson G., Wodchis W., Guttmann A. Patterns and costs of health care use of children with medical complexity. Pediatrics. 2012;130(6):e1463–1470. doi: 10.1542/peds.2012-0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simon TD, Berry J, Feudtner C, et al. Children with complex chronic conditions in inpatient hospital settings in the United States. Pediatrics.126(4):647–655. [DOI] [PMC free article] [PubMed]
- 7.Berry J.G., Hall D.E., Kuo D.Z. Hospital utilization and characteristics of patients experiencing recurrent readmissions within children's hospitals. J. Am. Med. Assoc. 2011;305(7):682–690. doi: 10.1001/jama.2011.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnson C.P., Kastner T.A. Helping families raise children with special health care needs at home. Pediatrics. 2005;115(2):507–511. doi: 10.1542/peds.2004-2520. [DOI] [PubMed] [Google Scholar]
- 9.Elias E.R., Murphy N.A. Home care of children and youth with complex health care needs and technology dependencies. Pediatrics. 2012;129(5):996–1005. doi: 10.1542/peds.2012-0606. [DOI] [PubMed] [Google Scholar]
- 10.Nageswaran S., Golden S.L. Improving the quality of home health care for children with medical complexity. Acad Pediatr. 2017;17(6):665–671. doi: 10.1016/j.acap.2017.04.019. [DOI] [PubMed] [Google Scholar]
- 11.OB I., Duffy A. The developing role of children's nurses in community palliative care. Br. J. Nurs. 2010;19(15):977–981. doi: 10.12968/bjon.2010.19.15.77694. [DOI] [PubMed] [Google Scholar]
- 12.Kun S.S., Beas V.N., Keens T.G., Ward S.S., Gold J.I. Examining pediatric emergency home ventilation practices in home health nurses: opportunities for improved care. Pediatr. Pulmonol. 2015;50(7):691–697. doi: 10.1002/ppul.23040. [DOI] [PubMed] [Google Scholar]
- 13.Law J., McCann D., O'May F. Managing change in the care of children with complex needs: healthcare providers' perspectives. J. Adv. Nurs. 2011;67(12):2551–2560. doi: 10.1111/j.1365-2648.2011.05761.x. [DOI] [PubMed] [Google Scholar]
- 14.Nageswaran S., Radulovic A., Anania A. Transitions to and from the acute inpatient care setting for children with life-threatening illness. Pediatr. Clin. 2014;61(4):761–783. doi: 10.1016/j.pcl.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 15.Berry J.G., Toomey S.L., Zaslavsky A.M. Pediatric readmission prevalence and variability across hospitals. J. Am. Med. Assoc. 2013;309(4):372–380. doi: 10.1001/jama.2012.188351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mosquera R.A., Avritscher E.B., Samuels C.L. Effect of an enhanced medical home on serious illness and cost of care among high-risk children with chronic illness: a randomized clinical trial. J. Am. Med. Assoc. 2014;312(24):2640–2648. doi: 10.1001/jama.2014.16419. [DOI] [PubMed] [Google Scholar]
- 17.Simon T.D., Whitlock K.B., Haaland W. Effectiveness of a comprehensive case management service for children with medical complexity. Pediatrics. 2017;140(6) doi: 10.1542/peds.2017-1641. [DOI] [PubMed] [Google Scholar]
- 18.Coller R.J., Klitzner T.S., Lerner C.F. Complex care hospital use and postdischarge coaching: a randomized controlled trial. Pediatrics. 2018;142(2) doi: 10.1542/peds.2017-4278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Auger K.A., Simmons J.M., Tubbs-Cooley H.L. Postdischarge nurse home visits and reuse: the hospital to home outcomes (H2O) trial. Pediatrics. 2018;142(1) doi: 10.1542/peds.2017-3919. [DOI] [PubMed] [Google Scholar]
- 20.Auger K.A., Shah S.S., Tubbs-Cooley H.L. Effects of a 1-time nurse-led telephone call after pediatric discharge: the H2O II randomized clinical trial. JAMA Pediatr. 2018;172(9) doi: 10.1001/jamapediatrics.2018.1482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nageswaran S., Golden S.L. Home health nurse collaboration in the medical neighborhood of children with medical complexity. Home Healthc. Nurse. 2016;34(9):507–518. doi: 10.1097/NHH.0000000000000463. [DOI] [PubMed] [Google Scholar]
- 22.Nageswaran S., Golden S.L. Factors associated with stability of health nursing services for children with medical complexity. Home Healthc. Nurse. 2017;35(8):434–444. doi: 10.1097/NHH.0000000000000583. [DOI] [PubMed] [Google Scholar]
- 23.Cohen E., Lacombe-Duncan A., Spalding K. Integrated complex care coordination for children with medical complexity: a mixed-methods evaluation of tertiary care-community collaboration. BMC Health Serv. Res. 2012;12:366. doi: 10.1186/1472-6963-12-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gordon J.B., Colby H.H., Bartelt T., Jablonski D., Krauthoefer M.L., Havens P. A tertiary care-primary care partnership model for medically complex and fragile children and youth with special health care needs. Arch. Pediatr. Adolesc. Med. 2007;161(10):937–944. doi: 10.1001/archpedi.161.10.937. [DOI] [PubMed] [Google Scholar]
- 25.Smith T. Bringing children home: bridging the gap between inpatient pediatric care and home healthcare. Home Healthc. Nurse. 2011;29(2):108–117. doi: 10.1097/NHH.0b013e3182085e93. [DOI] [PubMed] [Google Scholar]
- are. In.
- 27.Muller M.J., Scheurich A., Wetzel H., Szegedi A., Hautzinger M. Sequentially adjusted randomization to force balance in controlled trials with unknown prevalence of covariates: application to alcoholism research. Alcohol Alcohol. 2005;40(2):124–131. doi: 10.1093/alcalc/agh131. [DOI] [PubMed] [Google Scholar]
- 28.Stein R.E., Jessop D.J. The impact on family scale revisited: further psychometric data. J. Dev. Behav. Pediatr. 2003;24(1):9–16. [PubMed] [Google Scholar]
- 29.Nageswaran S., Ip E.H., Golden S.L., O'Shea T.M., Easterling D. Inter-agency collaboration in the care of children with complex chronic conditions. Acad Pediatr. 2012;12(3):189–197. doi: 10.1016/j.acap.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Optimal Design Software for Multi-Level and Longitudinal Research. 2011. [Software] [computer program] [Google Scholar]
- 31.Benjamini Y., Hochberg Y. Controlling the false discovery rate - a practical and powerful approach to multiple testing. J. Roy. Stat. Soc. B. 1995;57(1):289–300. [Google Scholar]
- 32.Proschan M.A., Waclawiw M.A. Practical guidelines for multiplicity adjustment in clinical trials. Contr. Clin. Trials. 2000;21(6):527–539. doi: 10.1016/s0197-2456(00)00106-9. [DOI] [PubMed] [Google Scholar]
- 33.Olejnik S., Li J.M., Supattathum S., Huberty C.J. Multiple testing and statistical power with modified Bonferroni procedures. J. Educ. Behav. Stat. 1997;22(4):389–406. [Google Scholar]
- 34.D'Agostino R.B., Jr., D'Agostino R.B., Sr. Estimating treatment effects using observational data. J. Am. Med. Assoc. 2007;297(3):314–316. doi: 10.1001/jama.297.3.314. [DOI] [PubMed] [Google Scholar]
- 35.Blumenthal D, Chernof B, Fulmer T, Lumpkin J, Selberg J. Caring for high-need, high-cost patients — an urgent priority. N. Engl. J. Med..0(0):null. [DOI] [PubMed]
- 36.Nutting P.A., Crabtree B.F., Stewart E.E. Effect of facilitation on practice outcomes in the National Demonstration Project model of the patient-centered medical home. Ann. Fam. Med. 2010;8(Suppl 1):S33–S44. doi: 10.1370/afm.1119. S92. [DOI] [PMC free article] [PubMed] [Google Scholar]