Abstract
OBJECTIVES:
(1) To assess prognostic factors for patient-reported outcome measures (PROMs) and physical activity two to ten years after anterior cruciate ligament reconstruction (ACLR) or injury, and (2) to assess differences in prognostic factors between patients treated with ACLR and with rehabilitation alone.
DESIGN:
Prognosis systematic review.
LITERATURE SEARCH:
Systematic searches in PubMed, Web of Science and SPORTDiscus.
STUDY SELECTION CRITERIA:
We selected prospective cohort studies and randomised clinical trials that included adults/adolescents undergoing either ACLR or rehabilitation alone after ACL rupture. Studies had to assess for a statistical association between potential prognostic factors (factors related to patient characteristics, injury or knee symptoms/function measured at baseline or within one year) and outcomes (PROMS and physical activity).
DATA SYNTHESIS:
Our search yielded 997 references. Twenty studies met inclusion criteria. Seven studies with low or moderate risk of bias remained for data synthesis.
RESULTS:
There was moderate certainty evidence that concomitant meniscus and cartilage injuries were prognostic factors for worse PROMs two to ten years after ACLR. There was very low certainty evidence that BMI, smoking and baseline PROMs were prognostic factors for worse outcome. There was very low certainty evidence that female sex and worse baseline Marx Activity Rating Scale (Marx) were prognostic factors for worse Marx two to ten years after ACLR. There was a lack of studies on prognostic factors after rehabilitation alone.
CONCLUSION:
Concomitant meniscus and cartilage injuries were prognostic factors for worse long-term PROMs after ACLR. The certainty was very low for other prognostic factors.
Keywords: Prognosis, Ligament, Knee surgery, Sporting injuries
INTRODUCTION
Anterior cruciate ligament (ACL) injuries have serious negative long-term consequences such as lower extremity dysfunction, low levels of physical activity, poor quality of life, and early development of knee osteoarthritis (OA) (1-7). Resolving impairments and returning to sport are often the main short-term goals for patients (1, 8). Clinicians must consider the long-term consequences of ACL injury when providing patient education, and when making decisions about interventions early after injury or reconstruction (9). Hence, high quality studies on prognostic factors for important long-term outcomes such as patient reported outcome measures (PROMs), levels of physical activity and OA are valuable.
A prognosis study can aim to predict the total individual risk given all available information in a prediction model, or to estimate a population average causal effect of an exposure or treatment on an outcome given adjustment for relevant confounders. Both approaches may provide important information on prognostic factors, as a prognostic factor can be either causally or non-causally related to an outcome variable (10-12). Many systematic reviews have evaluated prognostic factors for developing knee OA after ACL injury (5, 13-17). A few systematic reviews have reported prognostic factors for long-term PROMs and level of physical activity (15, 16, 18-21), but most of them are of poor quality due to lack of risk of bias assessments (15, 16, 18). Also, patients treated with rehabilitation alone have not been included in previous systematic reviews.
Consequently, we need a high-quality systematic review on prognostic factors for PROMs and level of physical activity two to ten years after ACL reconstruction (ACLR) or injury, with an appropriate and thorough risk of bias assessment. Such a study may provide information about prognostic factors that can be targeted with early treatment, and can thereby help to improve outcomes for patients with ACL injury.
Current evidence suggests similar clinical courses following rehabilitation alone and ACLR (3, 22-26), but we do not know if prognostic factors differ in the two treatment groups. There is great clinical interest to identify early prognostic factors associated with better outcome after both ACLR and rehabilitation alone. This knowledge can help inform treatment choices. No systematic review has previously addressed this topic.
Therefore, the aims of our systematic review were (1) to assess prognostic factors for PROMs and physical activity two to ten years after ACL injury or ACLR, and (2) to assess differences in prognostic factors between patients treated with ACLR and with rehabilitation alone.
METHODS
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (27). Our study protocol was published in the International Prospective Register of Systematic Reviews (PROSPERO: CRD42018095602) on June 7th 2018.
Eligibility criteria
Studies were included using the following criteria: (1) Prospective cohort studies and randomised clinical trials (RCT), that (2) reported prognostic factors for PROMs or level of physical activity, at (3) a mean of ≥ two and <ten years, in (4) adults and adolescents (mean age > 13 years), (5) undergoing either ACLR or rehabilitation alone after complete ACL rupture. (6) Studies had to assess the association between exposure and outcome with regression analyses. Studies only on revision ACLR, knee dislocations, partial tears or bilateral injury were excluded. We included studies where a subset of patients had these conditions. Prognostic factors were defined as either patient characteristics (all factors that describes a patient (e.g. age, sex, psychological factors), factors related to the injury (e.g. concomitant injury) or knee symptoms and function (e.g. functional performance, patient reported outcome measures) that were assessed within one year after injury or ACLR.
The following PROMs were selected; Knee injury and Osteoarthritis Outcome Score (KOOS), International Knee Documentation Committee Subjective Knee Form (IKDC-SKF) and Knee Outcome Survey Activities of Daily Living Scale (KOS-ADLS). These PROMs were chosen based on their frequent use as stand-alone PROMs for long-term outcomes during the last decade and because they have good measurement properties (28-34). The KOOS consists of five subscales: pain, other symptoms, function in daily living (ADL), function in sport and recreation (S/R), and knee-related quality of life (QoL) (32). KOOS can be reported as individual subscales or as KOOS4 which is an average score of four subscales (ADL excluded). The IKDC-SKF measures symptoms, function and sports activity in patients with different types of knee problems (34). The KOS-ADLS assesses the impact of symptoms on patients’ ability to perform daily activities (28). All three questionnaires are scored from 0 (worst) to 100 (best).
We included all outcomes that reflect type and level of physical activity, including the three components defining physical activity: frequency, intensity and duration (35) (eg objective measures such as accelerometers, patient-reported physical activity questionnaires and return to sports). An example of a patient-reported outcome measure of physical activity for ACL injured individuals is the Marx Activity Rating Scale (Marx). Marx is a brief survey on the frequency of participation in sports involving running, pivoting, cutting, and deceleration (36).
Data sources and searches
We systematically searched PubMed, Web of Science and SPORTDiscus for articles published from database inception to 20th September 2018. See search strategy for PubMed in TABLE 1. Filters on “Humans” and “English language” were used and all free text words/terms were searched on "Title/abstract". Relevant systematic reviews were identified with the same search terms in PubMed. Reference lists from systematic reviews and included studies were hand searched for relevant material to supplement electronic database searches. To identify additional literature, the following simplified search was performed in Google Scholar: "Anterior cruciate ligament"∣ACL Prognosis∣"Prognostic factors"∣Predict∣Associations "Return to sports"∣Participation∣"Activity level"∣"Physical activity"∣Tegner∣Marx∣KOOS ∣IKDC∣KOS "Prospective study"∣"Observational study"∣"Cohort study"∣RCT”. The 100 first (and most relevant) results from Google Scholar were screened. The searches were performed with assistance from and reviewed by librarians at the Norwegian School of Sport Sciences and the University of Oslo.
Table 1.
PubMed search
| 1) | Anterior cruciate ligament[mesh terms] OR Anterior cruciate ligament injury[mesh terms] OR Anterior cruciate ligament reconstruction[mesh terms] |
| 2) | Anterior cruciate ligament Or ACL |
| 3) | Prognosis[mesh terms] |
| 4) | Prognosis OR Prognostic factors OR Prognostic factor OR Predictor OR Predictors OR Predict OR Prediction OR Predictive OR Effect modifiers OR Effect modifier OR Risk factors OR Risk factor OR Factor OR Factors OR Associated OR Association OR Associations |
| 5) | Return to sport[mesh terms] |
| 6) | Return to sport OR Return to sports OR Participation OR Activity level OR Physical activity OR "Tegner activity scale" OR "Marx activity rating scale" OR Return to play OR KOOS OR "Knee injury and Osteoarthritis Outcome score" OR "International Knee Documentation Committee subjective knee form" OR "IKDC-SKF 2000" OR IKDC-SKF2000 OR "International Knee Documentation Committee Subjective Knee Evaluation Form" OR "IKDC-SKF" OR "Knee Outcome Survey" OR KOS |
| 7) | Prospective studies[mesh terms] |
| 8) | Prospective studies OR Prospective study OR Observational study OR Cohort study OR Randomized controlled trial OR Randomized clinical trial OR Randomised controlled trial OR Randomised clinical trial OR RCT OR Randomised trial OR Randomized trial |
| 9) | 1 OR 2 |
| 10) | 3 OR 4 |
| 11) | 5 OR 6 |
| 12) | 7 OR 8 |
| 13) | 9 AND 10 AND 11 AND 12 |
Study selection and data extraction
Two independent researchers (MP and JLJ) screened for eligibility and extracted data with customized data extraction forms. Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia, available at www.covidence.org) was used to assist this process. Calibration exercises were performed to ensure consistency between reviewers, but without testing agreement. Discrepancies were resolved by discussion or a third reviewer (HG or MAR). We contacted study authors to resolve uncertainties when necessary. Titles and abstracts were screened to identify potentially relevant studies for full text eligibility assessment. The reasons for exclusion were recorded. When several exclusion criteria were fulfilled, the first reason on a predefined list was chosen.
Risk of bias assessment
Risk of bias was assessed with the Quality in Prognosis Study (QUIPS) risk of bias tool (37). We chose this tool because it was developed specifically for the methodological assessment of prognostic studies. QUIPS is a reliable tool for systematically assessing risk of bias in the following six domains: study participation, study attrition, prognostic factor measurement, outcome measurement, study confounding and statistical analysis and reporting (37). Three independent reviewers (MP, JLJ and KM) performed the scoring of the different domains. Our operationalization of the QUIPS items is described in APPENDIX 1. For studies where the objective was prediction and not etiology, the confounding domain was classified as irrelevant (because the goal of a prediction model is to predict the total individual risk given all information, for example independent of the covariates’ influence on each other) (11, 12).
The overall risk of bias for each study was classified: (1) low, if there was low risk of bias in all domains, (2) moderate, if there was moderate risk of bias for ≥one domain and (3) high, if there was high risk of bias for ≥one domain (38). For all domains, high risk of bias was defined as a level where the results of the study should not be trusted, and/or it was impossible to interpret due to research methodology and/or inadequate description of methodology. This was an overall assessment and decision, and hence, no study was classified as high risk of bias in any domain based on only one question.
Data synthesis and analysis
Results from all included studies (n=20) are presented in APPENDIX 2 and 3. We included only studies with low or moderate risk of bias in the data synthesis. The purpose was to ensure that conclusions and recommendations to clinicians and patients were robust, and to make the results easier to interpret and easier to translate into practice. When data from the same patients were used in publications on the same prognostic factors and outcomes at different time points, we included the most recent publication. Results were presented separately for the outcomes PROMs and level of physical activity and for patients undergoing ACLR and rehabilitation alone. When possible, results from studies on each treatment group were extracted separately. Results from adjusted analyses were preferred. It was not possible to perform a meta-analysis due to methodological diversity in outcome measures and follow-up time.
Quality of evidence for each prognostic factor was judged as high, moderate, low or very low according to the “Grading of Recommendations Assessment, Development and Evaluation” (GRADE) approach (39, 40). We used GRADEpro (41) to help generate evidence summaries.
RESULTS
Search results
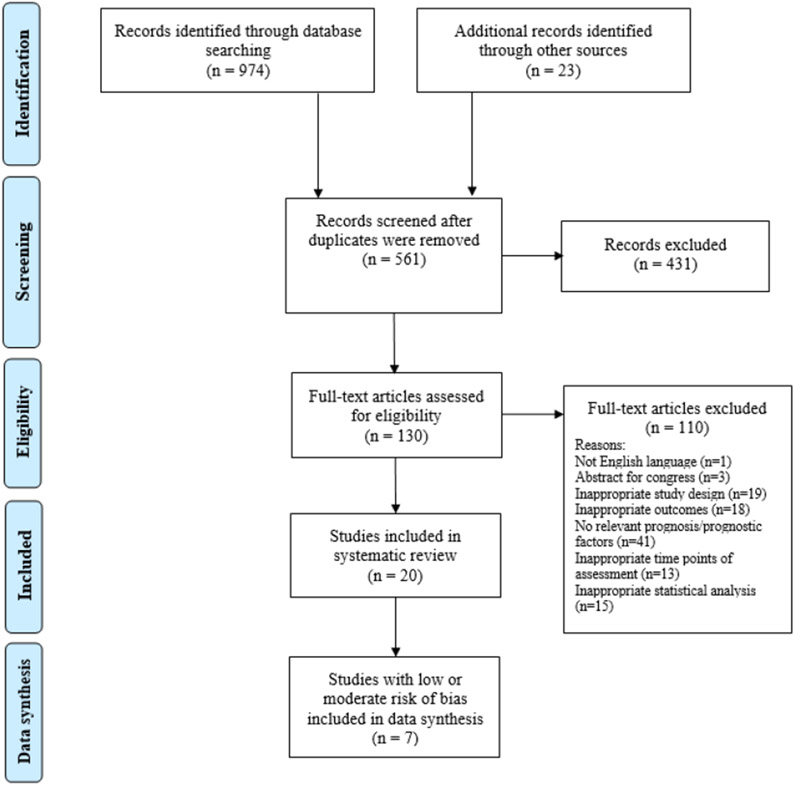
Database searches identified 974 references, and 23 additional references were identified through bibliographies (n=2), Google Scholar (n=3) and reference lists (n=18). After removing duplicates, 561 references remained. All were screened for eligibility and 431 were ineligible due to objectives, outcome or follow-up time. The remaining 130 articles were read in full text and 20 met all eligibility criteria (FIGURE 1). Seventeen of the included studies were identified through the systematic search, while three were identified through other sources. Due to more recent publications on the same prognostic factors and outcomes, we excluded the results on concomitant cartilage lesions, but not meniscus lesions from Røtterud et al. (42) and all results from Magnussen et al. (43) from 2016. Seven studies with low or moderate risk of bias remained for data synthesis (42, 44-49).
FIGURE 1.
Flow chart
Study characteristics
Characteristics of the included studies (n=20) are presented in TABLE 2. Most of the cohort studies were based on data from the Multicenter Orthopedic Outcomes Network (MOON) cohort (n= 8) (43, 47, 48, 50-54) and the Swedish and/or Norwegian Knee Ligament Registries (SKLR/NKLR) (n= 5) (42, 44, 46, 49, 55). In the included RCTs, both treatment groups were treated as one cohort for the assessment of prognostic factors (45, 56-58). Three of the RCT publications were based on the Knee Anterior Cruciate Ligament, Nonsurgical versus Surgical Treatment (KANON) trial (45, 57, 58). The studies included median (Q1-Q3) 495 (121-2333) patients. Due to several publications on the same patients in the large registry studies, it was challenging to estimate the total number of unique patients included in this systematic review. Most studies included patients undergoing primary ACLR only, and no study included only patients treated with rehabilitation alone. Patients with substantial concomitant injuries (43, 45-47, 51, 53, 55-61) and/or contralateral ACL injury (42, 46, 48, 49, 51-54, 56) were frequently excluded from the included studies. The median age at inclusion was 26 years (range 18-27). The median percentage of females was 44% (range 26-77%). Preinjury activity level was reported in seven studies, where four (52, 59-61) included patients active in pivoting sports preinjury and three (45, 57, 58) included patients with Tegner Activity Scale between 6 and 9 (6=recreational pivoting sports, 9=competitive sports).
Table 2.
Characteristics of included studies (n=20)
| Study characteristics | Patients' characteristics |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Study | n | Treatment | FU Years |
Prognostic factors assessed |
Outcome | Included in data synthesis |
Sex % female |
Median/ mean age Years |
|
| Ageberg et al. (2010) (44) | SKLR | 10164 | Primary ACLR | 2 | Age | KOOS | ✓ | 42% | 27 |
| Barenius et al. (2013) (55) | SKLR | 8584 | Primary ACLR | 2 | Sex, age, baseline PROMs, concomitant meniscus/ cartilage, knee laxity, previous knee surgery | KOOS | 49% | NR | |
| Brophy et al. (2016) (50) | MOON | 2198 | Primary or revision ACLR | 2 | Diabetes | IKDC-SKF KOOS Level of PA | 44% | 24 | |
| Cox et al. (2014) (51) | MOON | 1512 | Primary or revision ACLR | 6 | Sex, age, BMI, smoking, education, ethnicity, type of sport, competition level, baseline PROM, concomitant meniscus/cartilage | IKDC-SKF KOOS Level of PA | 44% | 23 | |
| Dunn et al. (2010) (52) | MOON | 446 | Primary or revision ACLR | 2 | Sex, age, BMI, smoking, education, marital status, ethnicity, type of sport, competition level, baseline PROM, concomitant meniscus/ cartilage, hearing a pop at injury | Level of PA | 44% | 23 | |
| Ericsson et al. (2013) (57) | KANON | 121 | ACLR or non-surgical | 2 + 5 | Early physical performance | KOOS | 26% | 26 | |
| Filbay et al. (2017) (45) | KANON | 121 | ACLR or non-surgical | 5 | Baseline PROM, concomitant meniscus/cartilage, knee extension deficit | KOOS | ✓ | 26% | 26 |
| Hamrin Senorski et al. (2018) (46) | SKLR | 15204 | Primary ACLR | 2 | Concomitant MCL/LCL/meniscus/ cartilage | KOOS | ✓ | 50% | NR |
| Ithurburn et al. (2017) (59) | Cohort | 48 | Primary ACLR | 2 | Early physical performance | KOOS | 77% | 18 | |
| Magnussen et al. (2016) (43) | MOON | 2333 | Primary ACLR | 2 | Knee laxity | IKDC-SKF KOOS | 44% | 27 | |
| Magnussen et al. (2018) (47) | MOON | 2333 | Primary ACLR | 6 | Knee laxity | IKDC-SKF KOOS Level of PA | ✓ | 44% | 27 |
| Nawasreh et al. (2018) (60) | Cohort | 107 | Primary ACLR | 2 | Sex, age, baseline PROM, early physical performance | Level of PA | 34% | 27 | |
| Roessler et al. (2015) (58) | KANON | 121 | ACLR or non-surgical | 2 | Psychological factors | KOOS | 26% | 26 | |
| Rotterud et al. (2013) (42) | S/N KLR | 15783 | Primary ACLR | 2 | Concomitant meniscus/ cartilage | KOOS | ✓ | 42% | 26 |
| Sasaki et al. (2016) (56) | RCT | 150 | Primary ACLR | 2 | Sex, age, BMI, baseline PROM, concomitant meniscus | KOOS | 58% | 26 | |
| Sonnery-Cottet et al. (2017) (61) | Cohort | 541 | Primary ACLR | 3 | Sex, age, type of sport, concomitant meniscus | Level of PA | 27% | 22 | |
| Spindler et al. (2005) (53) | MOON | 314 | Primary ACLR | 5 | Sex, age, type of sport, concomitant meniscus/cartilage, hearing a pop at injury, onset of swelling after injury | IKDC-SKF KOOS | 45% | 27 | |
| Spindler et al. (2011) (48) | MOON | 448 | Primary or revision ACLR | 6 | Sex, age, BMI, smoking, ethnicity, marital status, type of sport, baseline PROM, concomitant MCL/LCL/ meniscus/ cartilage, hearing a pop at injury | IKDC-SKF KOOS Level of PA | ✓ | 43% | 23 |
| Ulstein et al. (2018) (49) | S/N KLR | 15783 | Primary ACLR | 5 | Concomitant cartilage | KOOS | ✓ | 42% | 27 |
| Wasserstein (2015) (54) | MOON | 1761 | Primary ACLR | 2 + 6 | Sex, age, BMI, smoking, education, baseline PROM, concomitant meniscus/ cartilage, previous knee pathology | KOOS | 44% | 23 | |
FU, follow-up; NR, not reported; SKLR/NKLR, Swedish/Norwegian Knee Ligament Registry; MOON, Multicenter Orthopedic Outcomes Network; KANON, Knee Anterior Cruciate Ligament, Nonsurgical versus Surgical Treatment
Sixteen studies were etiological (42-47, 49-53, 56-59, 61) and four were predictive (48, 54, 55, 60). Among the studies included in our data synthesis, only Spindler et al. (48) was a predictive study.
Risk of bias
Risk of bias for the six QUIPS-domains and an overall rating is shown in TABLE 3. Studies generally performed poorly on the domains “Study confounding” and “Analysis and reporting” because they did not explicitly state what covariates were adjusted for and why, did not separate between confounders, mediators and colliders (and subsequently did not treat these covariates in accordance with existing rules for adjustment), or had mixed predictive and etiological statistical approaches, which led to uninterpretable results (10, 12, 62).
Table 3:
Risk of bias assessment (n=20)
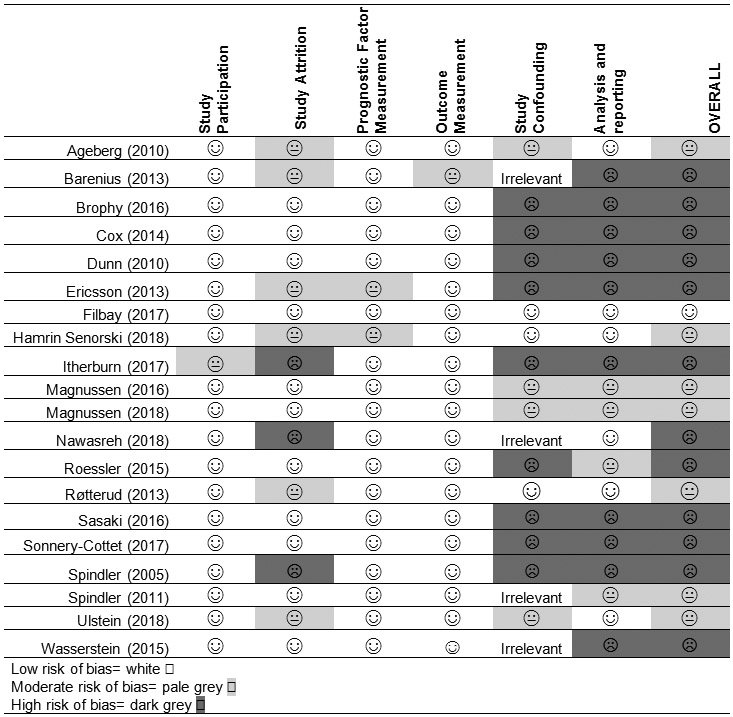 |
Data synthesis of studies with low or moderate risk of bias (n=7)
Prognostic factors for PROMs in patients treated with ACLR
Prognostic factors for PROMs in patients treated with ACLR were assessed in seven studies from four cohorts. The IKDC-SKF was an outcome in two studies (47, 48) and the KOOS was an outcome in seven studies (42, 44-49). The following 13 factors were assessed by ≥1 study with low or moderate risk of bias: sex, age, body mass index (BMI), smoking, ethnicity, type of sport, concomitant injury on medial or lateral concomitant ligaments (MCL/LCL), meniscus or cartilage, hearing a pop at injury, knee laxity, extension range of motion deficit and baseline PROMs. These factors were measured at baseline, preoperatively or during ACLR.
Patient characteristics
One predictive study reported higher baseline BMI as a prognostic factor for worse six-year IKDC-SKF and KOOS S/R outcomes and smoking for worse IKDC-SKF (48). The same study found no association between higher BMI and KOOS QoL, or between smoking and KOOS QoL and KOOS S/R.
There were no statistically significant association between the factors sex, age, ethnicity and type of sport and the outcomes two- and six-year IKDC-SKF and KOOS (44, 48).
Factors related to the injury
Concomitant meniscus injury was reported as a prognostic factor in some studies, but not in others. Three studies (two etiological and one predictive) of three different cohorts, found a statistically significant negative association between concomitant meniscus injury and two-year patient-reported success (KOOS4 ≥80th percentile) (46) and five- and six-year KOOS S/R and QoL outcomes (45, 48). The mean difference between those with and without concomitant meniscus injury was 10-14.4 points for KOOS S/R (45, 48) and 8.9 points for KOOS QoL (48). The same studies found, however, no statistically significant associations between meniscus injury and the other KOOS subscales and IKDC-SKF (45, 48). In one etiological study, concomitant meniscus injury was not a prognostic factor for any two-year KOOS subscale (42).
Concomitant cartilage injury was assessed in four studies from four different cohorts (45, 46, 48, 49). In two etiological studies, there was a statistically significant association between concomitant cartilage lesions and five-year KOOS (all subscales), particularly for the full-thickness lesions (45, 49). The mean difference between those with and without concomitant cartilage injury was 8.1 points for KOOS S/R (49) and 8-2.3 points for KOOS QoL (45, 49). The results of Filbay et al. (45) applied only for the five-year KOOS QoL in patients with early (not delayed) ACLR. In a third etiological study, the absence of concomitant cartilage injury predicted two-year patient-reported success (as previously defined) while having a concomitant cartilage injury predicted failure (KOOS4 ≤ 20th percentile) (46). One predictive study found no association between concomitant cartilage injury and six-year KOOS S/R and QoL and IKDC-SKF (48).
There were no statistically significant associations between concomitant MCL/LCL injury or hearing a pop at injury and the outcomes two-year patient-reported success or failure (46) and six-year IKDC-SKF, KOOS QoL and KOOS S/R (48).
Knee symptoms/function
In one etiological study, baseline KOOS4 predicted five-year KOOS Symptoms, KOOS S/R and KOOS QoL, but not KOOS pain, in patients with early ACLR (45). In those with delayed ACLR, KOOS4 did not predict any of the five-year KOOS subscales (45). A predictive study found conflicting results for the association between baseline and five-year KOOS scores (48).
Preoperative knee laxity, defined as severely abnormal either Lachman, anterior drawer or pivot-shift test, was assessed in one etiological study (47). There was a small statistically significant association between preoperative knee laxity and six-year IKDC-SKF and KOOS QoL (mean difference between those with and without preoperative laxity of 2.3 and 2.7 points, respectively) that was not considered as clinically relevant (47).
There were no statistically significant associations between baseline Short-Form 36 and knee extension deficit >10 degrees and five-year KOOS outcomes (45).
GRADE evaluation for prognostic factors for PROMs in patients treated with ACLR
The evidence for concomitant meniscus and cartilage injuries was moderate, while for the other factors it was low or very low (TABLE 4). Our conclusions did not differ when all 20 eligible studies were included in a GRADE evaluation (APPENDIX 4).
Table 4.
GRADEa evidence profile: potential prognostic factors for 2- to 10-year PROMs in ACL b reconstructed patients. Studies with low- and moderate risk of bias (n=7).
| GRADE factors | Summary of findings | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Potential prognostic factors (№ of studies) |
№ of
patients |
Study limitations |
Inconsistency | Indirectness | Imprecision | Publication bias |
Moderate/large effect size |
Dose effect | Univariable analysis |
Multivariable Analysisg |
Certainty | ||||
| + | 0 | − | + | 0 | − | ||||||||||
| Sex (1) | 448 | ✕ c | ✓ | ✓ | ✕ | ✕ h | ✕ | ✕ | 1 | ⊕◯◯◯ VERY LOW |
|||||
| Age (2) | 10612 | ✕ d | ✓ | ✓ | ✕ | ✕ h | ✕ | ✕ | 1 | 1 | ⊕⊕◯◯LOW | ||||
| Higher BMI (1) | 448 | ✕ c | ✓ | ✓ | ✕c | ✕ h | ✕ | ✕ | 1 | ⊕◯◯◯ VERY LOW |
|||||
| Smoking (1) | 448 | ✕ c | ✕ e | ✓ | ✕ | ✕ h | ✕ | ✕ | 1 | ⊕◯◯◯ VERY LOW |
|||||
| Ethnicity (1) | 448 | ✕ c | ✓ | ✓ | ✕ | ✕ h | ✕ | ✕ | 1 | ⊕◯◯◯ VERY LOW |
|||||
| Type of sport (1) | 448 | ✕ c | ✓ | ✓ | ✕ | ✕ h | ✕ | ✕ | 1 | ⊕◯◯◯ VERY LOW |
|||||
| Concomitant MCL or LCL injuries (2) | 15652 | ✕ d | ✓ | ✓ | ✕ | ✕ h | ✕ | ✕ | 2 | ⊕⊕◯◯LOW | |||||
| Concomitant meniscus injuries (4) | 31556 | ✓ | ✕ e | ✓ | ✓ | ✕ h | ✓ | ✕ | 1 | 3 | ⊕⊕⊕◯MODERATE | ||||
| Concomitant cartilage injuries (4) | 31556 | ✓ | ✕ e | ✓ | ✓ | ✕ h | ✓ | ✓ | 1 | 4 | ⊕⊕⊕◯MODERATE | ||||
| Hearing pop at injury (1) | 448 | ✕ c | ✓ | ✓ | ✕ | ✕ h | ✕ | ✕ | 1 | ⊕◯◯◯ VERY LOW |
|||||
| Preoperative knee laxity (1) | 2333 | ✕ c | ✓ | ✓ | ✕ | ✕ h | ✕ | ✕ | 1 | ⊕◯◯◯ VERY LOW |
|||||
| Preoperative extension deficit (1) | 121 | ✕ f | ✓ | ✓ | ✕ | ✕ h | ✕ | ✕ | 1 | ⊕◯◯◯ VERY LOW |
|||||
| Higher baseline PROMs (2) | 569 | ✕ d | ✕ e | ✓ | ✕ | ✕ h | ✕ | ✕ | 2 | ⊕◯◯◯ VERY LOW |
|||||
For uni− and multivariable analyses: +, number of significant effects with a positive value; 0, number of non-significant effects; −, number of significant effects with a negative value.
For GRADE factors: ✓, no serious limitations; ✕, serious limitations (or not present for moderate/large effect size, dose effect)
Grading of Recommendations Assessment, Development and Evaluation
Anterior Cruciate Ligament
Evidence is based on only one study with moderate risk of bias
Evidence is based on only two studies with moderate risk of bias
Inconsistency within/between study/studies
Evidence is based on only one study with low risk of bias
Summary of authors conclusions when several outcomes for each factor were assessed
Due to a small number of included studies, we could not assess small study biases with a funnel plot. We therefore cannot rule out publication bias
Prognostic factors for Physical Activity in patients treated with ACLR
Prognostic factors for level of physical activity in patients treated with ACLR was assessed in two studies from the same cohort, both using the Marx questionnaire as the outcome (47, 48). The following 13 factors were assessed by ≥1 study with moderate risk of bias: sex, age, BMI, smoking, marital status, ethnicity, type of preinjury sport, baseline PROMs, concomitant injury to the LCL/ MCL, meniscus or cartilage, knee laxity and hearing a pop at injury (TABLE 2).
Patient characteristics
One predictive study assessed several demographic factors as possible prognostic factors for six-year Marx (48). Female sex and worse baseline Marx were prognostic factors for worse six-year Marx, while age, BMI, smoking, marital status, ethnicity and type of preinjury sport were not (48).
Factors related to the injury
None of the following factors were prognostic factors for six-year Marx score: concomitant MCL/LCL, meniscus or cartilage injuries and hearing a pop at injury (48). One etiological study found a statistically significant association between preoperative laxity (as previously defined) and six-year Marx (47). The mean difference between those with and without preoperative laxity was small (0.5 points) and not clinically relevant (47).
GRADE evaluation for prognostic factors for level of physical activity in patients treated with ACLR
Quality of evidence was judged as very low for all the prognostic factors for level of physical activity in patients treated with ACLR. Serious limitations in several GRADE domains occurred because evidence for all factors was based on only one study with moderate risk of bias.
Prognostic factors for PROMs and physical activity in patients treated with rehabilitation alone
One etiological study assessed prognostic factors for five-year KOOS4 for a group of patients treated with rehabilitation alone separately (45). None of the following factors were prognostic factors: baseline cartilage defect, meniscus damage, osteochondral lesion, extension deficit, SF-36 and KOOS4 (45). Quality of evidence was judged as very low due to few studies. No study assessed prognostic factors for physical activity in this patient group.
Differences in prognostic factors between treatment groups
One etiological study with low risk of bias assessed differences in prognostic factors between those treated with rehabilitation alone and with ACLR (45). Based on differences in prognostic factors for five-year KOOS4 between the treatment groups, the authors suggested that patients with concomitant meniscus injury and those with worse KOOS symptoms, S/R and QoL in the early phase may benefit most from exercise therapy before choosing treatment (45).
DISCUSSION
Concomitant meniscus and cartilage injuries were, with moderate certainty, prognostic factors for worse PROMs two to ten years after ACLR. Smoking, BMI and baseline PROMs were prognostic factors for two to ten-year PROMs with very low certainty. For level of physical activity two to ten years after ACLR, we concluded with very low certainty that female sex and worse baseline Marx were prognostic factors for worse long-term Marx. The other factors assessed in this systematic review were not associated with the outcomes. No studies included only patients treated with rehabilitation alone. One study assessed differences in prognostic factors between patients treated with rehabilitation alone and with ACLR (45). Patients with concomitant meniscal and cartilage injuries and lower KOOS scores in the acute phase may benefit most from an initial non-surgical treatment choice, but further research on the topic is needed to draw conclusions. Hence, we could not answer the second aim of this systematic review.
For the prognostic factors BMI, smoking, baseline PROMs, sex and baseline Marx, the impact on outcomes was small (see appendix 2 and 3) and probably not clinically relevant. The impact of concomitant meniscus injury as a prognostic factor was larger, as the mean difference between those with and without meniscus injury was 10-14.4 points for KOOS S/R (45, 48) and 8.9 points for KOOS QoL (48). For KOOS S/R, but not KOOS QoL, the impact of having a concomitant meniscus injury was clinically relevant as the minimal important change (MIC) (95% CI) are 12.1 (9.3 to 14.8) points for KOOS S/R and 18.3 (16.0 to 20.6) points for KOOS QoL (63). The impact of having a concomitant cartilage injury on KOOS S/R (8.1 points) and QoL (8-12.3 points) outcomes also seemed important, but the mean difference between those with and without concomitant cartilage was below the MIC for the instruments (45, 49).
Comparison with other studies
The high methodological quality of this systematic review makes an important contribution to this field. Our high-quality search strategy, rigorous risk of bias assessment and data synthesis ensured robust conclusions and recommendations for clinicians and patients. Due to these methodological factors, we could not replicate the findings of previous systematic reviews, such as that male sex, younger age and psychological factors are positive prognostic factors and that quadriceps weakness and range of motion deficits are negative factors (19, 64).
To our knowledge, ours is the first systematic review to assess prognostic factors for PROMs and level of physical activity after ACL injury both in patients treated with ACLR and with rehabilitation alone. Although the paucity of studies on patients treated with rehabilitation alone made it impossible to answer our review questions regarding prognostic factors for PROMs and level of physical activity for this treatment group, or to assess differences in prognostic factors between treatment groups.
Our results highlighted the importance of risk of bias assessments in systematic reviews as 12 of 20 included studies (60%) were rated as having high risk of bias. Bias was suspected especially in the domains “Study confounding” and “Statistical analysis and reporting”. Lack of clarity in aims and methods about whether studies were predictive or etiological was a recurring limitation. Effect estimates calculated from one model, often a prediction model, which is presented in one table may mislead because the underlying associations between covariates are not accounted for (10). In many papers with etiological aims, but statistically driven rather than theoretically driven approaches, it was unclear if the estimates were adjusted for all relevant confounders, and whether they should have been interpreted as total or direct effects (11). Epidemiological research methodology has developed over time, and the distinction between explanatory and predictive aims was less clear at the time when the included studies were performed.
Limitations
An important limitation in the literature in this field was the likely between-study overlap of patients within the different publications from the MOON cohort and the SKLR/NKLR. This overlap may have led to a correlation between study results that we could not account for. To minimize this problem, we only included the most recent publication of data from the same patients and on the same prognostic factors. Further, our strict inclusion criteria might have led us to miss high quality research where other PROMs than IKDC-SKF, KOOS and KOS-ADLS were used, such as Lysholm, ACL Return to Sport after Injury scale (ACL-RSI) and Short Form-36 (SF-36). The included studies did not differentiate between types of meniscus injuries, and we therefore lack knowledge on the prognosis after different injury types (eg. dislocated bucket-handle tears versus stable, horizontal tears).
Our results apply to individuals with first time complete unilateral ACL-injury, not including knee dislocations. The prognostic factors are also only applicable to the outcomes PROMs and level of physical activity ≥ two and <ten years after ACLR. We did not consider psychological, overall health or quality of life outcomes.
Implications for clinical practice
When planning future physical activities and discussing patient expectations, it is useful for patients, physical therapists, orthopaedic surgeons and athletic trainers to be aware that concomitant meniscus or cartilage injuries may lead to worse knee function two to ten years after ACLR. As concomitant meniscus injuries are also the most frequently reported prognostic factor for knee OA after ACL injury (5, 13), patients should be informed about preventive interventions for knee OA such as knee extensor muscle strength training and maintaining a healthy body weight (65-71). Although with very low certainty, higher BMI was a prognostic factor for worse PROMs after ACLR. Due to the relation to both knee function and development of knee OA, BMI as a prognostic factor is important and needs to be incorporated in the early patient education. We also found that smoking is a negative prognostic factor for PROMs. As this factor is modifiable, patients should be informed that avoiding smoking might contribute to better long-term outcomes.
Implications for future research on prognostic factors after ACL injury and ACLR
Future studies should be clear whether their aims and methods are aimed at prediction or etiology. If the aim is etiological, authors should carefully state their hypothesis with background and run an informed causal effect analysis, ensuring that rules for adjustment for different types of covariates (confounders, mediators and colliders) are followed (11, 72). If the aim is predictive, studies should systematically build a prediction model based on all available predictors and study the model’s discriminative ability and calibration and subsequently internally and externally validate findings (73, 74). Pre-registration of study protocols for observational studies on prognostic factors might enable researchers to assess if selective reporting and publication bias occur within this field.
Future high-quality prognosis studies should include patients treated with rehabilitation alone. This patient group is important as it represents between 26% and 77% of the ACL-injured population (75-77). New studies should also compare prognostic factors between patients treated with rehabilitation alone and with ACLR in order to help clinicians identify who might have the best prognosis with ACLR and who might succeed with rehabilitation alone. Future studies should also assess modifiable prognostic factors which can be targeted in early rehabilitation, such as muscle strength, range of motion and hop performance.
Our systematic review also uncovered a lack of studies on level of physical activity long-term after ACL injury. Most studies were at high risk of bias and the study outcomes were only activity rating scale (Marx) and the prevalence of return to sport, neither of which align with the most common definition of level of physical activity (35) as they only measure participation in specific types of sports. Future studies should therefore include more general level of physical activity as outcomes (eg accelerometery, International Physical Activity Questionnaire).
CONCLUSION
Concomitant meniscus and cartilage injuries were prognostic factors for worse PROMs two to ten years after ACLR. There was very low certainty evidence that BMI, smoking and worse baseline PROMs were prognostic factors for worse PROMs, and that female sex and worse baseline Marx score were prognostic factors for worse Marx score two to ten years after ACLR.
Supplementary Material
KEY POINTS.
FINDINGS: We have moderate confidence that concomitant meniscus and cartilage injuries are prognostic factors for worse long-term PROMs after ACLR. The certainty is low/very low for other prognostic factors.
IMPLICATIONS: When planning future activities and discussing patient expectations, it is useful for patients, physical therapists, orthopaedic surgeons and athletic trainers to consider that concomitant meniscus or cartilage injuries may lead to worse knee function two to ten years after ACLR.
CAUTION: A large proportion (60%) of included studies in this systematic review were at high risk of bias, and there is a lack of studies on prognostic factors in patients treated with rehabilitation alone.
STUDY DETAILS.
Data sharing: All data relevant to the study are included in the article or are available as supplementary files.
Patient and public involvement: There was no patient or public involvement in this research.
AKNOWLEDGEMENTS
We would like to acknowledge librarians Anne Grethe Gabrielsen, Karianne Hasledalen and Elin Hecker at the Norwegian School of Sport Sciences and Marte Ødegaard at the University of Oslo for assistance and reviewing of systematic searches.
Funding: The project is funded by the National Institutes of Health through grant R37HD37985.
Footnotes
Public trials registry: Our study protocol was published in the International Prospective Register of Systematic Reviews (PROSPERO: CRD42018095602) on June 7th 2018.
Statement of financial disclosure and conflict of interest: I affirm that I have no financial affiliation (including research funding) or involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript.
REFERENCES
- 1.Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–52. [DOI] [PubMed] [Google Scholar]
- 2.Filbay SR, Ackerman IN, Russell TG, Macri EM, Crossley KM. Health-related quality of life after anterior cruciate ligament reconstruction: a systematic review. Am J Sports Med. 2014;42(5):1247–55. [DOI] [PubMed] [Google Scholar]
- 3.Grindem H, Eitzen I, Engebretsen L, Snyder-Mackler L, Risberg MA. Nonsurgical or Surgical Treatment of ACL Injuries: Knee Function, Sports Participation, and Knee Reinjury: The Delaware-Oslo ACL Cohort Study. J Bone Joint Surg Am. 2014;96(15):1233–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moksnes H, Risberg MA. Performance-based functional evaluation of non-operative and operative treatment after anterior cruciate ligament injury. Scand J Med Sci Sports. 2009;19(3):345–55. [DOI] [PubMed] [Google Scholar]
- 5.Oiestad BE, Engebretsen L, Storheim K, Risberg MA. Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med. 2009;37(7):1434–43. [DOI] [PubMed] [Google Scholar]
- 6.Culvenor AG, Collins NJ, Guermazi A, Cook JL, Vicenzino B, Khan KM, et al. Early knee osteoarthritis is evident one year following anterior cruciate ligament reconstruction: a magnetic resonance imaging evaluation. Arthritis Rheumatol. 2015;67(4):946–55. [DOI] [PubMed] [Google Scholar]
- 7.Ajuied A, Wong F, Smith C, Norris M, Earnshaw P, Back D, et al. Anterior cruciate ligament injury and radiologic progression of knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med. 2014;42(9):2242–52. [DOI] [PubMed] [Google Scholar]
- 8.Ardern CL, Osterberg A, Sonesson S, Gauffin H, Webster KE, Kvist J. Satisfaction With Knee Function After Primary Anterior Cruciate Ligament Reconstruction Is Associated With Self-Efficacy, Quality of Life, and Returning to the Preinjury Physical Activity. Arthroscopy. 2016;32(8):1631–8.e3. [DOI] [PubMed] [Google Scholar]
- 9.Risberg MA, Grindem H, Oiestad BE. We Need to Implement Current Evidence in Early Rehabilitation Programs to Improve Long-Term Outcome After Anterior Cruciate Ligament Injury. J Orthop Sports Phys Ther. 2016;46(9):710–3. [DOI] [PubMed] [Google Scholar]
- 10.Westreich D, Greenland S. The table 2 fallacy: presenting and interpreting confounder and modifier coefficients. Am J Epidemiol. 2013;177(4):292–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hernan MA, Robins JM. Estimating causal effects from epidemiological data. J Epidemiol Community Health. 2006;60(7):578–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shmueli G To Explain or To Predict? Statistical Science. 2010;25(3):289–310. [Google Scholar]
- 13.van Meer BL, Meuffels DE, van Eijsden WA, Verhaar JA, Bierma-Zeinstra SM, Reijman M. Which determinants predict tibiofemoral and patellofemoral osteoarthritis after anterior cruciate ligament injury? A systematic review. Br J Sports Med. 2015;49(15):975–83. [DOI] [PubMed] [Google Scholar]
- 14.Magnussen RA, Mansour AA, Carey JL, Spindler KP. Meniscus status at anterior cruciate ligament reconstruction associated with radiographic signs of osteoarthritis at 5- to 10-year follow-up: a systematic review. J Knee Surg. 2009;22(4):347–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tan SH, Lau BP, Khin LW, Lingaraj K. The Importance of Patient Sex in the Outcomes of Anterior Cruciate Ligament Reconstructions: A Systematic Review and Meta-analysis. Am J Sports Med. 2016;44(1):242–54. [DOI] [PubMed] [Google Scholar]
- 16.Magnussen RA, Spindler KP. The effect of patient and injury factors on long-term outcome after anterior cruciate ligament reconstruction. Curr Orthop Pract. 2011;22(1):90–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van Ginckel A, Verdonk P, Witvrouw E. Cartilage adaptation after anterior cruciate ligament injury and reconstruction: implications for clinical management and research? A systematic review of longitudinal MRI studies. Osteoarthritis Cartilage. 2013;21(8):1009–24. [DOI] [PubMed] [Google Scholar]
- 18.Magnussen RA, Verlage M, Flanigan DC, Kaeding CC, Spindler KP. Patient-Reported Outcomes and Their Predictors at Minimum 10 Years After Anterior Cruciate Ligament Reconstruction: A Systematic Review of Prospectively Collected Data. Orthop J Sports Med. 2015;3(3):2325967115573706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Valk EJ, Moen MH, Winters M, Bakker EW, Tamminga R, van der Hoeven H. Preoperative patient and injury factors of successful rehabilitation after anterior cruciate ligament reconstruction with single-bundle techniques. Arthroscopy. 2013;29(11):1879–95. [DOI] [PubMed] [Google Scholar]
- 20.An VV, Scholes C, Mhaskar VA, Hadden W, Parker D. Limitations in predicting outcome following primary ACL reconstruction with single-bundle hamstring autograft - A systematic review. Knee. 2017;24(2):170–8. [DOI] [PubMed] [Google Scholar]
- 21.Everhart JS, Best TM, Flanigan DC. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):752–62. [DOI] [PubMed] [Google Scholar]
- 22.Grindem H, Eitzen I, Moksnes H, Snyder-Mackler L, Risberg MA. A pair-matched comparison of return to pivoting sports at 1 year in anterior cruciate ligament-injured patients after a nonoperative versus an operative treatment course. Am J Sports Med. 2012;40(11):2509–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. Br J Sports Med. 2015;49(10):700. [DOI] [PubMed] [Google Scholar]
- 24.Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010;363(4):331–42. [DOI] [PubMed] [Google Scholar]
- 25.Meuffels DE, Favejee MM, Vissers MM, Heijboer MP, Reijman M, Verhaar JA. Ten year follow-up study comparing conservative versus operative treatment of anterior cruciate ligament ruptures. A matched-pair analysis of high level athletes. Br J Sports Med. 2009;43(5):347–51. [DOI] [PubMed] [Google Scholar]
- 26.Ageberg E, Thomee R, Neeter C, Silbernagel KG, Roos EM. Muscle strength and functional performance in patients with anterior cruciate ligament injury treated with training and surgical reconstruction or training only: a two to five-year followup. Arthritis Rheum. 2008;59(12):1773–9. [DOI] [PubMed] [Google Scholar]
- 27.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Bmj. 2009;339:b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Irrgang JJ, Snyder-Mackler L, Wainner RS, Fu FH, Harner CD. Development of a patient-reported measure of function of the knee. J Bone Joint Surg Am. 1998;80(8):1132–45. [DOI] [PubMed] [Google Scholar]
- 29.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Neyret P, Richmond JC, et al. Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am J Sports Med. 2006;34(10):1567–73. [DOI] [PubMed] [Google Scholar]
- 30.van Meer BL, Meuffels DE, Vissers MM, Bierma-Zeinstra SM, Verhaar JA, Terwee CB, et al. Knee injury and Osteoarthritis Outcome Score or International Knee Documentation Committee Subjective Knee Form: which questionnaire is most useful to monitor patients with an anterior cruciate ligament rupture in the short term? Arthroscopy. 2013;29(4):701–15. [DOI] [PubMed] [Google Scholar]
- 31.Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ. The International Knee Documentation Committee Subjective Knee Evaluation Form: normative data. Am J Sports Med. 2006;34(1):128–35. [DOI] [PubMed] [Google Scholar]
- 32.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. [DOI] [PubMed] [Google Scholar]
- 33.Collins NJ, Misra D, Felson DT, Crossley KM, Roos EM. Measures of knee function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care & Research. 2011;63(S11):S208–S28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Irrgang JJ, Anderson AF, Boland AL, Harner CD, Kurosaka M, Neyret P, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29(5):600–13. [DOI] [PubMed] [Google Scholar]
- 35.Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100(2):126–31. [PMC free article] [PubMed] [Google Scholar]
- 36.Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213–8. [DOI] [PubMed] [Google Scholar]
- 37.Hayden JA, van der Windt DA, Cartwright JL, Cote P, Bombardier C. Assessing bias in studies of prognostic factors. Ann Intern Med. 2013;158(4):280–6. [DOI] [PubMed] [Google Scholar]
- 38.Higgins J, Green Se. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Table 8.7.a. 2011 [updated 2018.11.16 Available from: www.handbook.cochrane.org. [Google Scholar]
- 39.Iorio A, Spencer FA, Falavigna M, Alba C, Lang E, Burnand B, et al. Use of GRADE for assessment of evidence about prognosis: rating confidence in estimates of event rates in broad categories of patients. Bmj. 2015;350:h870. [DOI] [PubMed] [Google Scholar]
- 40.Huguet A, Hayden JA, Stinson J, McGrath PJ, Chambers CT, Tougas ME, et al. Judging the quality of evidence in reviews of prognostic factor research: adapting the GRADE framework. Systematic Reviews. 2013;2(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University dbEP, Inc.). Available from gradepro.org. [ [Google Scholar]
- 42.Røtterud JH, Sivertsen EA, Forssblad M, Engebretsen L, Årøen A. Effect of Meniscal and Focal Cartilage Lesions on Patient-Reported Outcome After Anterior Cruciate Ligament Reconstruction: A Nationwide Cohort Study From Norway and Sweden of 8476 Patients With 2-Year Follow-up. American Journal of Sports Medicine. 2013;41(3):535–43. [DOI] [PubMed] [Google Scholar]
- 43.Magnussen RA, Reinke EK, Huston LJ, Hewett TE, Spindler KP. Effect of High-Grade Preoperative Knee Laxity on Anterior Cruciate Ligament Reconstruction Outcomes. Am J Sports Med. 2016;44(12):3077–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ageberg E, Forssblad M, Herbertsson P, Roos EM. Sex differences in patient-reported outcomes after anterior cruciate ligament reconstruction: data from the Swedish knee ligament register. Am J Sports Med. 2010;38(7):1334–42. [DOI] [PubMed] [Google Scholar]
- 45.Filbay SR, Roos EM, Frobell RB, Roemer F, Ranstam J, Lohmander LS. Delaying ACL reconstruction and treating with exercise therapy alone may alter prognostic factors for 5-year outcome: an exploratory analysis of the KANON trial. Br J Sports Med. 2017;51(22):1622–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hamrin Senorski E, Alentorn-Geli E, Musahl V, Fu F, Krupic F, Desai N, et al. Increased odds of patient-reported success at 2 years after anterior cruciate ligament reconstruction in patients without cartilage lesions: a cohort study from the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1086–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Magnussen RA, Reinke EK, Huston LJ, Hewett TE, Spindler KP, Amendola A, et al. Effect of High-Grade Preoperative Knee Laxity on 6-Year Anterior Cruciate Ligament Reconstruction Outcomes. Am J Sports Med. 2018:363546518793881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Spindler KP, Huston LJ, Wright RW, Kaeding CC, Marx RG, Amendola A, et al. The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction: a population cohort study. Am J Sports Med. 2011;39(2):348–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ulstein S, Aroen A, Engebretsen L, Forssblad M, Lygre SHL, Rotterud JH. Effect of Concomitant Cartilage Lesions on Patient-Reported Outcomes After Anterior Cruciate Ligament Reconstruction A Nationwide Cohort Study From Norway and Sweden of 8470 Patients With 5-Year Follow-up. Orthopaedic Journal of Sports Medicine. 2018;6(7). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Brophy RH, Huston LJ, Wright RW, Nwosu SK, Kaeding CC, Parker RD, et al. Outcomes of ACL Reconstruction in Patients with Diabetes. Med Sci Sports Exerc. 2016;48(6):969–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Cox CL, Huston LJ, Dunn WR, Reinke EK, Nwosu SK, Parker RD, et al. Are articular cartilage lesions and meniscus tears predictive of IKDC, KOOS, and Marx activity level outcomes after anterior cruciate ligament reconstruction? A 6-year multicenter cohort study. Am J Sports Med. 2014;42(5):1058–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dunn WR, Spindler KP. Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): a Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38(10):2040–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Spindler KP, Warren TA, Callison JC Jr., Secic M, Fleisch SB, Wright RW. Clinical outcome at a minimum of five years after reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 2005;87(8):1673–9. [DOI] [PubMed] [Google Scholar]
- 54.Wasserstein D, Huston LJ, Nwosu S, Kaeding CC, Parker RD, Wright RW, et al. KOOS pain as a marker for significant knee pain two and six years after primary ACL reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) prospective longitudinal cohort study. Osteoarthritis Cartilage. 2015;23(10):1674–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Barenius B, Forssblad M, Engstrom B, Eriksson K. Functional recovery after anterior cruciate ligament reconstruction, a study of health-related quality of life based on the Swedish National Knee Ligament Register. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):914–27. [DOI] [PubMed] [Google Scholar]
- 56.Sasaki S, Tsuda E, Hiraga Y, Yamamoto Y, Maeda S, Sasaki E, et al. Prospective Randomized Study of Objective and Subjective Clinical Results Between Double-Bundle and Single-Bundle Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2016;44(4):855–64. [DOI] [PubMed] [Google Scholar]
- 57.Ericsson YB, Roos EM, Frobell RB. Lower extremity performance following ACL rehabilitation in the KANON-trial: impact of reconstruction and predictive value at 2 and 5 years. Br J Sports Med. 2013;47(15):980–5. [DOI] [PubMed] [Google Scholar]
- 58.Roessler KK, Andersen TE, Lohmander S, Roos EM. Motives for sports participation as predictions of self-reported outcomes after anterior cruciate ligament injury of the knee. Scandinavian Journal of Medicine & Science in Sports. 2015;25(3):435–40. [DOI] [PubMed] [Google Scholar]
- 59.Ithurburn MP, Paterno MV, Ford KR, Hewett TE, Schmitt LC. Young Athletes After Anterior Cruciate Ligament Reconstruction With Single-Leg Landing Asymmetries at the Time of Return to Sport Demonstrate Decreased Knee Function 2 Years Later. Am J Sports Med. 2017;45(11):2604–13. [DOI] [PubMed] [Google Scholar]
- 60.Nawasreh Z, Logerstedt D, Cummer K, Axe M, Risberg MA, Snyder-Mackler L. Functional performance 6 months after ACL reconstruction can predict return to participation in the same preinjury activity level 12 and 24 months after surgery. Br J Sports Med. 2018;52(6):375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sonnery-Cottet B, Saithna A, Cavalier M, Kajetanek C, Temponi EF, Daggett M, et al. Anterolateral Ligament Reconstruction Is Associated With Significantly Reduced ACL Graft Rupture Rates at a Minimum Follow-up of 2 Years: A Prospective Comparative Study of 502 Patients From the SANTI Study Group. Am J Sports Med. 2017;45(7):1547–57. [DOI] [PubMed] [Google Scholar]
- 62.Hernán M, Robins J. Causal Inference: Boca Raton: Chapman & Hall/CRC, forthcoming; 2019. [Google Scholar]
- 63.Ingelsrud LH, Terwee CB, Terluin B, Granan LP, Engebretsen L, Mills KAG, et al. Meaningful Change Scores in the Knee Injury and Osteoarthritis Outcome Score in Patients Undergoing Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2018;46(5):1120–8. [DOI] [PubMed] [Google Scholar]
- 64.Everhart J, Best T, Flanigan D. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surgery, Sports Traumatology, Arthroscopy. 2015;23(3):752–62. [DOI] [PubMed] [Google Scholar]
- 65.Oiestad BE, Juhl CB, Eitzen I, Thorlund JB. Knee extensor muscle weakness is a risk factor for development of knee osteoarthritis. A systematic review and meta-analysis. Osteoarthritis Cartilage. 2015;23(2):171–7. [DOI] [PubMed] [Google Scholar]
- 66.Roos EM, Arden NK. Strategies for the prevention of knee osteoarthritis. Nat Rev Rheumatol. 2016;12(2):92–101. [DOI] [PubMed] [Google Scholar]
- 67.Hart HF, Barton CJ, Khan KM, Riel H, Crossley KM. Is body mass index associated with patellofemoral pain and patellofemoral osteoarthritis? A systematic review and meta-regression and analysis. Br J Sports Med. 2017;51(10):781–90. [DOI] [PubMed] [Google Scholar]
- 68.Jiang L, Tian W, Wang Y, Rong J, Bao C, Liu Y, et al. Body mass index and susceptibility to knee osteoarthritis: a systematic review and meta-analysis. Joint Bone Spine. 2012;79(3):291–7. [DOI] [PubMed] [Google Scholar]
- 69.Zhou Z-Y, Liu Y-K, Chen H-L, Liu F. Body mass index and knee osteoarthritis risk: A dose-response meta-analysis. Obesity. 2014;22(10):2180–5. [DOI] [PubMed] [Google Scholar]
- 70.Zheng H, Chen C. Body mass index and risk of knee osteoarthritis: systematic review and meta-analysis of prospective studies. BMJ Open. 2015;5(12):e007568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fernandes L, Hagen KB, Bijlsma JW, Andreassen O, Christensen P, Conaghan PG, et al. EULAR recommendations for the non-pharmacological core management of hip and knee osteoarthritis. Ann Rheum Dis. 2013;72(7):1125–35. [DOI] [PubMed] [Google Scholar]
- 72.Hernan MA. A definition of causal effect for epidemiological research. J Epidemiol Community Health. 2004;58(4):265–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Collins GS, Reitsma JB, Altman DG, Moons KG. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. Bmj. 2015;350:g7594. [DOI] [PubMed] [Google Scholar]
- 74.Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N, et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology. 2010;21(1):128–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nordenvall R, Bahmanyar S, Adami J, Stenros C, Wredmark T, Fellander-Tsai L. A population-based nationwide study of cruciate ligament injury in Sweden, 2001–2009: incidence, treatment, and sex differences. Am J Sports Med. 2012;40(8):1808–13. [DOI] [PubMed] [Google Scholar]
- 76.Collins JE, Katz JN, Donnell-Fink LA, Martin SD, Losina E. Cumulative incidence of ACL reconstruction after ACL injury in adults: role of age, sex, and race. Am J Sports Med. 2013;41(3):544–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Sanders TL, Maradit Kremers H, Bryan AJ, Kremers WK, Levy BA, Dahm DL, et al. Incidence of and Factors Associated With the Decision to Undergo Anterior Cruciate Ligament Reconstruction 1 to 10 Years After Injury. Am J Sports Med. 2016;44(6):1558–64. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.