Introduction
Despite several proposed algorithms to facilitate the differential diagnosis of wide QRS tachycardia, discriminating ventricular tachycardia (VT) from supraventricular tachycardia with aberrancy or pre-excited supraventricular tachycardia remains clinically challenging in certain cases. In this report, we present a case with initial manifestation of incessant wide QRS tachycardia with different right bundle branch block (RBBB) morphologies caused by dual atrioventricular (AV) nodal conduction that could be misinterpreted as ventricular arrhythmia (VA).
Case report
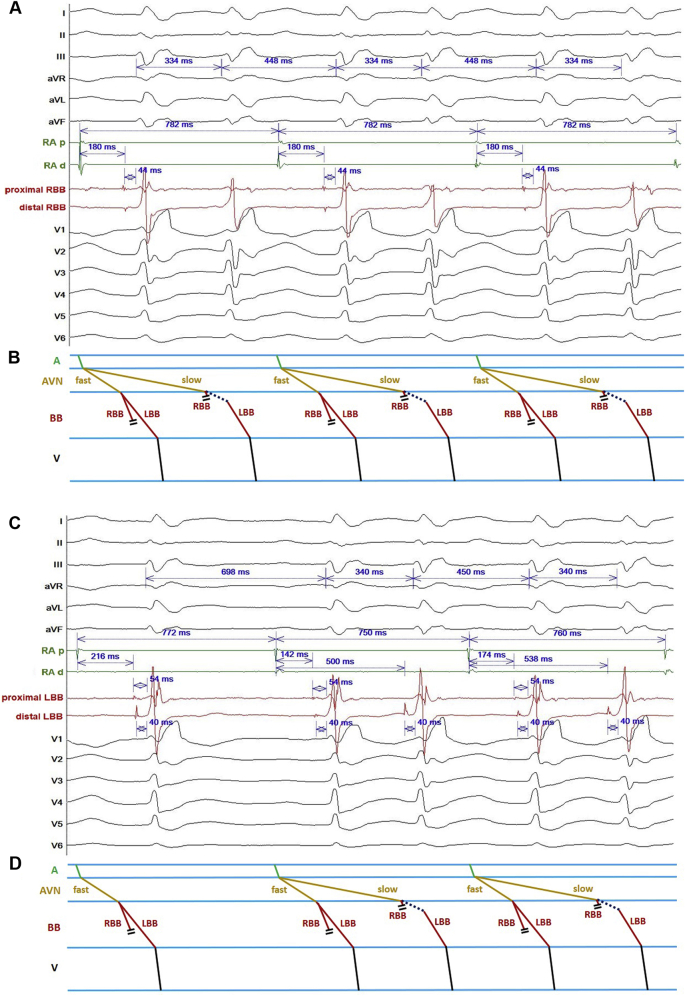
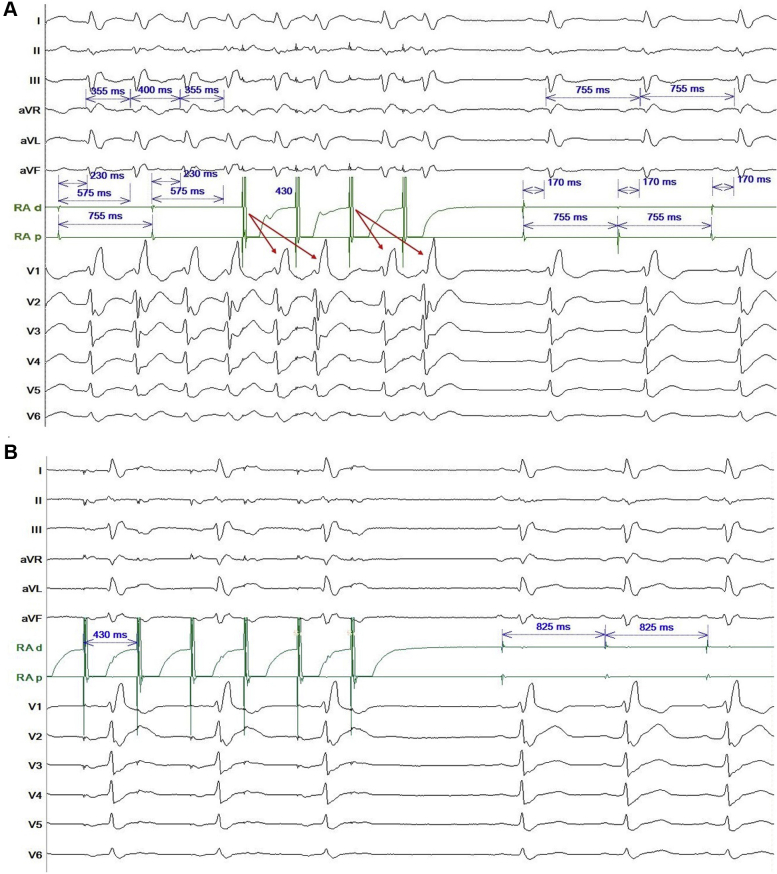
A 52-year-old man presented with palpitations for 10 years and was referred owing to a suspicion of incessant VA. Transthoracic echocardiography showed global hypokinesia and reduced left ventricular systolic function with ejection fraction of 41%, while coronary angiography excluded the possibility of ischemic cardiomyopathy. The 12-lead electrocardiogram showed wide complex tachycardia with alternation of different RBBB morphologies (Figure 1). An electrophysiologic study showed sinus activity with His-proximal right bundle branch (RBB) potential for 1 QRS complex with RBBB pattern (A-RBB: 180 ms and RBB-V: 44 ms) and the absence of His-proximal RBB signal for the other QRS complex with different RBBB morphology (Figure 2A). The differential diagnoses of second QRS complex with different RBBB morphology were (1) junctional escape beats with retrograde conduction block, (2) VA originating from the His/left bundle branch (LBB) region, or (3) dual AV nodal non-reentrant tachycardia (DAVNNT) with different extent of RBBB. Junctional escape beats were less likely owing to the absence of His-RBB potential. Mapping of the proximal LBB demonstrated the earliest activation site with the presence of LBB potential preceding the onset of the second RBBB wide QRS complex by 54 ms (Figure 2B). Of note, the proximal LBB potential was recorded during the sinus beats with the same LBB-V interval, which made the VA originating from the proximal LBB likely. The absence of proximal LBB potential in the second QRS complex with different RBBB morphology implied that VA originating from distal LBB cannot be completely excluded. However, right atrial pacing reproducibly induced “1P to 2QRS” with fixed coupling interval of slow pathway (Figure 3), which provided indirect evidence of “double fire” of DAVNNT and potentially variable linking of the fast and slow pathways to the LBB. Given the risk of complete AV block, cryoablation was applied to the traditional low Koch region and the tachycardia was successfully eliminated, which confirmed the final diagnosis.
Figure 1.
Surface electrocardiogram shows a wide complex tachycardia with 2 different right bundle branch block morphologies.
Figure 2.
A: Intracardiac electrogram at the right paraseptal region. Fixed right bundle branch (RBB) to V interval (44 ms) was only recorded in the first conducted beat via the fast pathway while RBB signal was not observed in the following conducted beat via the slow pathway. B: Corresponding ladder diagram of the right paraseptal recording. C: Intracardiac electrogram at the left paraseptal region. Fixed left bundle branch (LBB) to V interval (54 ms) was observed during the anterograde conduction via the fast and slow pathways. The conduction of slow pathway to LBB was different from fast pathway, which resulted in different activation patterns of proximal LBB and bipolar electrogram characteristics. D: Corresponding ladder diagram of left paraseptal recording.
Figure 3.
Right atrial pacing during preablation and postablation. A: Preablation atrial stimulation at 430 ms terminated the tachycardia without changing the sinus rate. Right atrial pacing reproducibly induced “1P 2QRS” (red arrows) with fixed coupling interval of slow pathway. B: Postablation atrial pacing at 430 ms showed 2:1 AV conduction. The QRS complexes during pacing are similar to the QRS complexes during sinus rhythm. This is consistent with the QRS complexes conducted via the fast pathway, and a confirmation that the slow pathway was eliminated.
Discussion
Twelve-lead electrocardiogram has been regarded as the gold standard for the diagnosis of DAVNNT with “1 P and 2 QRS” manifestation.1 However, in patients with intraventricular conduction disturbances or bundle branch block as presented in our case, the wide QRS complex tachycardia may confuse the exact diagnosis.2 The presence of VA dissociation and rate criteria for ventricular activation greater than atrial activation may be misinterpreted as VT, especially when wide QRS complex with variable morphologies are present.3, 4, 5 Previous reports showed that patients with DAVNNT and wide QRS tachycardia were misdiagnosed as VT and received inappropriate intracardiac defibrillator device therapy. The misdiagnoses were based upon interpretation of atrial and ventricular device electrograms that satisfied both rate and V>A criteria for ventricular tachycardia.4,5
A DAVNNT is defined by a fixed relationship between His, bundle branch, and ventricular activation. The effective refractory periods of the His-Purkinje system usually are shorter than the difference of conduction properties between fast and slow pathways.3,6,7 Consequently, the constant RBB and LBB potentials should be demonstrated during both fast and slow pathway conductions. In this patient, the nonuniform conduction in fast and slow pathways to the RBB and LBB could be ascribed by the infra-His conduction as a form of gap phenomenon or refractoriness of the RBB compared with the LBB. The activation conducted preferentially to the LBB with 1:1 conduction and to the proximal RBB with 2:1 conduction, which might be caused by the diseased RBB given the presence of RBBB pattern during sinus beats. Of note, the slow pathway preferentially conducted to the distal LBB with the conduction block to the proximal LBB, reflecting the heterogeneous conduction surrounding the perinodal/infranodal region (Figure 2). Despite the fixed LBB-V internal between the fast and slow pathway conductions, proximal activation of RBB via the fast pathway may contribute to the difference of RBBB morphologies when compared to those via the slow pathway.
Retrograde conduction from the ventricle to the atrium is usually absent or poor in patients with DAVNNT, which was different from the retrograde conduction properties in most of the typical slow-fast AV nodal reentrant tachycardia.7 Programmed atrial stimulation terminated tachycardia, which makes isorhythmic AV dissociation with firing from His or proximal LBB less likely (Figure 3).
Slow pathway modification is regarded as the curative treatment for patients with DAVNNT.1 Termination of the tachycardia by ablation of the slow pathway confirmed the diagnosis in this patient.7
Conclusion
DAVNNT with bundle branch block pattern can be misinterpreted as VA. Different conduction patterns between fast and slow atrioventricular nodal to the infranodal region was demonstrated in this case. Subtle QRS changes were observed with fast and slow pathway conduction, which might be explained by variable infra-His conduction. Successful ablation of the slow pathway with termination of tachycardia confirms the diagnosis of DAVNNT.
Key Teaching Points.
-
•
Dual atrioventricular nodal non-reentrant tachycardia (DAVNNT) rarely presents with wide complex tachycardia, which might be misinterpreted as ventricular arrhythmia.
-
•
Alternating right bundle branch morphologies in DAVNNT may represent different conduction patterns between the fast and slow pathways to the infranodal region. A thorough mapping of the conduction system is essential to understand the mechanism.
-
•
Termination of tachycardia with slow pathway ablation is the key to diagnosis of DAVNNT.
Footnotes
This work was supported by the Ministry of Science and Technology of Taiwan (MOST 107-2314-B-010-061-MY2, MOST 106-2314-B-010-046-MY3), Grant of TVGH (V108C-032, V109D48-001-MY2-1, C17-095), Research Foundation of Cardiovascular Medicine (107-02-036), and Szu-Yuan Research Foundation of Internal Medicine (No. 109015). All authors have no conflict of interest to disclose.
References
- 1.Peiker C., Pott C., Eckardt C. Dual atrioventricular nodal non-re-entrant tachycardia. Europace. 2016;18:332–339. doi: 10.1093/europace/euv056. [DOI] [PubMed] [Google Scholar]
- 2.Ozcan E., Szeplaki G., Merkely B., Geller L. Non-reentrant atrioventricular nodal tachycardia. Clin Res Cardiol. 2013;102:383–386. doi: 10.1007/s00392-013-0537-6. [DOI] [PubMed] [Google Scholar]
- 3.Neuss H., Buss J., Schlepper M., Mitrovíc V. Double ventricular response in dual AV nodal pathways mimicking supraventricular as well as ventricular tachycardia. Eur Heart J. 1982;3:146–154. doi: 10.1093/oxfordjournals.eurheartj.a061277. [DOI] [PubMed] [Google Scholar]
- 4.Karnik A., Hematpour K., Bhatt A., Mazzini M. Dual nodal nonreentrant tachycardia resulting in inappropriate ICD therapy in a patient with cardiac sarcoidosis. Indian Pacing Electrophysiol J. 2014;14:44–48. doi: 10.1016/s0972-6292(16)30715-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kirmanoglou K., Peiker C., Clasen L., Shin D., Kelm M., Meyer C. Duale AV-nodale nicht-reentry-tachykardie. Herzschrittmacherther Elektrophysiol. 2014;25:109–115. doi: 10.1007/s00399-014-0310-1. [DOI] [PubMed] [Google Scholar]
- 6.Francis J., Krishnan M. Dual ventricular response or 1:2 atrioventricular conduction in dual atrioventricular nodal physiology. Indian Pacing Electrophysiol J. 2008;8:77. [PMC free article] [PubMed] [Google Scholar]
- 7.Wang N. Dual atrioventricular nodal nonreentrant tachycardia: a systematic review. Pacing Clin Electrophysiol. 2011;34:1671–1681. doi: 10.1111/j.1540-8159.2011.03218.x. [DOI] [PubMed] [Google Scholar]