Introduction
Temporary external pacemakers are frequently used in critically ill patients who are not candidates for a permanent device.1,2 While patients with cardiac implantable electronic devices (CIEDs) meeting specific criteria have been approved by the Food and Drug Administration to undergo magnetic resonance imaging (MRI) studies, patients with temporary external devices may be denied the opportunity for MRI given the limited data regarding the safety profile of these devices.3, 4, 5
We present a case of a patient with an MRI-compatible temporary active-fixation right ventricular pacing lead with externalized pacemaker generator, who underwent successful MRI of the brain to guide his critical care management.
Case report
A 61-year-old man with history of non-Hodgkin’s lymphoma with prior radiation therapy and coronary artery disease status post coronary artery bypass graft at time of mechanical aortic valve replacement for severe bicuspid aortic valve stenosis presented to an outside hospital with fever, malaise, and respiratory distress. He was treated with broad-spectrum intravenous antibiotics for sepsis and intubated for respiratory failure. Initial blood cultures grew methicillin-sensitive Staphylococcus aureus. A transesophageal echocardiogram demonstrated a vegetation on the mechanical aortic valve suggestive of prosthetic endocarditis. His antibiotic therapy was narrowed to intravenous oxacillin, gentamicin, and rifampin. On hospital day 6, his course was complicated by pulseless electrical activity cardiac arrest with new complete heart block, for which an external MRI-compatible pacemaker (Accolade MRI L310; Boston Scientific, Marlborough, MA) and a right ventricle MRI-compatible active-fixation lead (Ingevity MRI 7742-59 cm; Boston Scientific, Marlborough, MA) were placed via a left subclavian approach owing to stenosis of the internal jugular veins. Following the cardiac arrest, a computed tomography (CT) of the head demonstrated multifocal bilateral infarcts with small areas of adjacent parenchymal and subarachnoid hemorrhage. Subsequent hospital course was notable for persistent ventilator requirement, left pneumothorax requiring chest tube placement, and progressive renal injury secondary to acute tubular necrosis.
He was transferred to our institution on hospital day 12. On initial examination, he was intubated and sedated; corneal and gag reflexes were present, he grimaced in response to upper extremity noxious stimuli without withdrawal, and there was no response to lower extremity noxious stimuli. Laboratory studies were notable for white blood count of 22,700/μL, hemoglobin 9.4 g/dL, platelets 402,000/μL, and creatinine 3.2 mg/dL. A limited transthoracic echocardiogram was obtained that redemonstrated aortic valve vegetation and trace aortic regurgitation (Video 1).
A brain MRI was requested on hospital day 13 to best evaluate the extent of cerebral infarction and for septic emboli or developing brain abscess. Repeat contrast CT imaging was contraindicated owing to renal insufficiency and noncontrast CT was felt to be insufficiently sensitive to answer the clinical question. In consultation with the radiology department Magnetic Resonance (MR) Safety Officer and MR Medical Director, the MRI was approved for scanning on a 1.5 T MR scanner (Achieva; Philips, Amsterdam, Netherlands) with the following conditions: (1) use of a transmit-receive head coil rather than the bore transmit-only and head receive-only coils, (2) imaging in normal mode, (3) repositioning of the generator from the neck to the upper left chest to maximize distance from the scanning area, and (4) insulating the generator from direct skin contact (Figure 1). For insulation, one pack of 4 × 4-inch gauze pads was inserted between the generator and exposed skin and covered with a transparent film dressing. These conditions were specified to minimize radiofrequency (RF) exposure to the generator and lead, prevent susceptibility artifact from the generator interfering with the imaging, and prevent skin injury from possible heat generation. The patient’s underlying rhythm was complete heart block without a ventricular escape. Pre-MRI impedance (773 ohms) and threshold values (0.3 V at 0.4 ms) were in normal range; sensing could not be determined owing to lack of an escape rhythm. Pacemaker MRI mode was activated (VOO at 80 beats per minute with pacing output of 5.0 V at 1.0 ms). Transcutaneous pacing pads connected to an external defibrillator were placed and the patient was monitored by an intensive care nurse via continuous telemetry and pulse oximetry during 35 minutes of scanning. Imaging was completed uneventfully and post-MRI impedance, thresholds, and battery capacity were unchanged. Chest roentgenograph demonstrated no evidence of lead migration (Supplemental Figure 1). Brain MRI images demonstrated bilateral multifocal infarcts consistent with septic emboli without evidence of brain abscess (Figure 2).
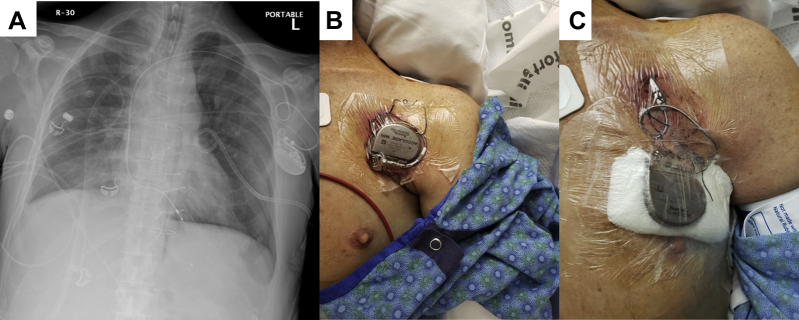
Figure 1.
Device implant site and positioning. A: Chest roentgenograph demonstrating the left subclavian location of the device and positioning of the active fixation right ventricular lead. B,C: External location of the implanted device on the chest wall at time of initial examination (B) and after repositioning and placement of gauze to insulate against thermal injury (C).
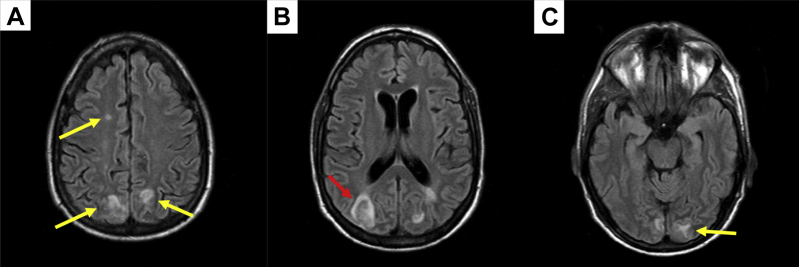
Figure 2.
Brain magnetic resonance imaging. Multifocal bi-hemispheric signal abnormalities with adjacent sulcal effacement (yellow arrows) and mild hemorrhagic conversion (red arrow) are present in the frontal (A), parietal (B), and occipital lobes (C), consistent with an embolic origin. No discrete abscesses visualized.
A cardiac CT was then performed to evaluate for aortic root abscess given the patient’s complete heart block. The patient was over-breathing the ventilator and he was therefore administered a bolus of benzodiazepine and then neuromuscular blockade to ensure breath-holding during image acquisition. Prior to the scan, the device was reprogrammed to VOO at 70 beats per minute to minimize motion artifact. The CT demonstrated a large hypoattenuated mass associated with the mechanical aortic valve, consistent with a vegetation; and thickening of the mitral-aortic intervalvular fibrosa, suggestive of perivalvular involvement, without abscess (Figure 3, Video 2). Post-MRI position of the lead tip within the right ventricular apex was further demonstrated on the CT images (Figure 3).
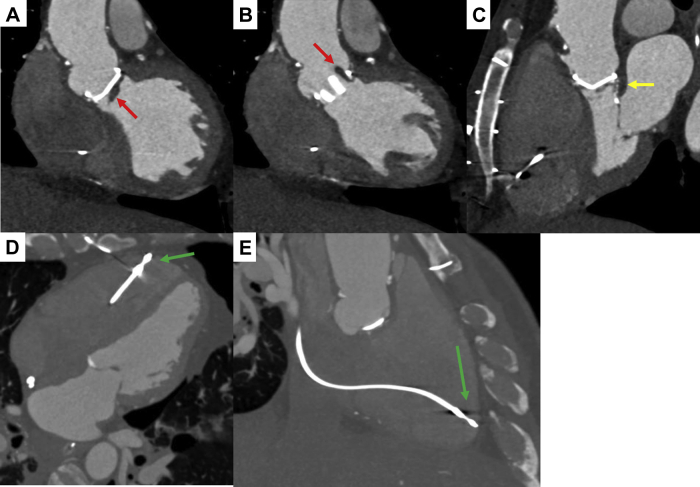
Figure 3.
Cardiac computed tomography. A large hypoattenuated mass consistent with a vegetation (red arrows) is associated with the mechanical aortic valve (A) and protrudes through the valve in systole (B). There is thickening of the mitral-aortic intervalvular fibrosa (yellow arrow), suggestive of perivalvular involvement (C). No abscess was identified. Lead position within the right ventricular apex (green arrows) following magnetic resonance imaging is demonstrated in 4-chamber (D) and modified 2-chamber views (E).
With the imaging results of the brain MRI and cardiac CT, cardiac surgery evaluated the patient and estimated an approximately 40% operative mortality risk and determined that surgical intervention could not be safely offered.6 After discussions with palliative care, the patient’s family decided to transition to comfort-oriented care. The patient subsequently died on hospital day 14.
Discussion
Here we report the case of a patient with prosthetic valve endocarditis complicated by complete heart block and dependence on a temporary externalized active-fixation pacemaker who successfully underwent a brain MRI. This study and the subsequent cardiac CT demonstrating bilateral cerebral infarcts and perivalvular involvement assisted the surgical team and family in making a joint decision to transition to comfort-oriented care given his high surgical risk and overall poor prognosis.
The potential safety risks for patients with CIEDs undergoing MR procedures relates to exposure of the device and leads to the 3 major electromagnetic fields present in the MR environment. These electromagnetic fields are (1) the static magnetic field, which extends throughout the MRI suite; (2) the RF field, which is generally confined to the volume of tissue being imaged; and (3) the time-varying (gradient) field, which is present within the bore of the scanner.7 Each of these electromagnetic fields has the potential to interact adversely with the CIED and leads, resulting in numerous safety concerns: atrial or ventricular arrhythmias owing to induced currents from the time-varying gradient field; oversensing or undersensing of native electrical signals owing to electromagnetic interference from interaction of all 3 fields; activation of the reed switch (mimicking the effect of an external magnet) or displacement of the leads or device, both owing to effects of the static magnetic field; damage to the generator or lead circuitry from the time-varying gradient and RF fields; and, finally, thermal injury from the RF field if the device and leads are within the imaged tissue volume.8
In this patient’s case, compared with a typical fully implanted CIED system, the externalization of the generator and proximal lead presented a theoretical increased risk of thermal injury to the adjacent skin, and greater risk of electromagnetic interference and damage to the generator or lead circuitry. The conditions specified by the MR Safety Officer and MR Medical Director in this case were focused on minimizing these safety concerns: (1) 1.5 T rather than 3.0 T imaging to reduce the static magnetic field imaging exposure, (2) Normal mode imaging to limit RF energy absorption to physiologic limits of <2 W/kg, (3) transmit receive only head coil to further isolate the RF field to the head and upper neck region, and (4) repositioning of the generator to the chest to further separate it from the imaged tissue volume and associated RF energy, with insulation around the generator used to prevent any possible thermal injury to the skin.
Data regarding the safety of MRI in patients with temporary external pacemakers is limited to case reports. Brain MRI demonstrating new temporal lobe neoplasm has been previously performed without incident in a patient requiring temporary external pacemaker implant via a right internal jugular approach for seizure-related asystole events.9 Recently, Chaudhry and colleagues10 described a patient with new complete heart block requiring temporary external pacing via a right subclavian approach who underwent cardiac MRI demonstrating myocarditis. These data, while limited, support the concept that MR imaging can be safely performed from either an internal jugular or subclavian approach with device programming and monitoring in line with the manufacturer recommendations for implanted devices. For patients who require temporary external pacing and in whom the need for future MR imaging is anticipated, implantation of an MRI-compatible system is reasonable and positioning of the lead tip within the right ventricular apex may enhance safety. Further study will be imperative to determine best safety and monitoring practices for patients with temporary external pacemakers undergoing MRI.
Conclusions
MRI was safely performed on a patient with an MRI-compatible temporary external pacemaker and active fixation lead without adverse events. A small body of literature supports the case-by-case use of MRI in selected patients with a temporary pacemaker.
Key Teaching Points.
-
•
Magnetic resonance imaging (MRI) may be safely performed in selected patients with MRI-compatible temporary external pacemakers and appropriate precautions.
-
•
Choice of vascular site for lead implant; positioning, dressing, and programming of the device; and close monitoring with a backup pacing option are essential to success.
-
•
A multidisciplinary approach involving cardiac electrophysiologists, radiologists, and cardiac imaging specialists is key to appropriate patient selection and safe image acquisition.
Footnotes
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. All authors declare no conflicts of interest.
Supplementary data associated with this article can be found in the online version at https://doi.org/10.1016/j.hrcr.2020.06.012.
Appendix. Supplementary data
Post-MRI chest roentgenograph. Chest roentgenograph demonstrating unchanged lead position following successful MRI.
Transthoracic echocardiogram.
Cardiac CT.
References
- 1.Kornberger A., Schmid E., Kalender G. Bridge to recovery or permanent system implantation: an eight-year single-center experience in transvenous semipermanent pacing. Pacing Clin Electrophysiol. 2013;36:1096–1103. doi: 10.1111/pace.12175. [DOI] [PubMed] [Google Scholar]
- 2.Kawata H., Pretorius V., Phan H. Utility and safety of temporary pacing using active fixation leads and externalized re-usable permanent pacemakers after lead extraction. Europace. 2013;15:1287–1291. doi: 10.1093/europace/eut045. [DOI] [PubMed] [Google Scholar]
- 3.Indik J.H., Gimbel J.R., Abe H. 2017 HRS expert consensus statement on magnetic resonance imaging and radiation exposure in patients with cardiovascular implantable electronic devices. Heart Rhythm. 2017;14:e97–e153. doi: 10.1016/j.hrthm.2017.04.025. [DOI] [PubMed] [Google Scholar]
- 4.Gimbel J.R., Bello D., Schmitt M. Randomized trial of pacemaker and lead system for safe scanning at 1.5 Tesla. Heart Rhythm. 2013;10:685–691. doi: 10.1016/j.hrthm.2013.01.022. [DOI] [PubMed] [Google Scholar]
- 5.Williamson B.D., Gohn D.C., Ramza B.M. Real-world evaluation of magnetic resonance imaging in patients with a magnetic resonance imaging conditional pacemaker system: results of 4-year prospective follow-up in 2,629 patients. JACC Clin Electrophysiol. 2017;3:1231–1239. doi: 10.1016/j.jacep.2017.05.011. [DOI] [PubMed] [Google Scholar]
- 6.Navia J.L., Elgharably H., Hakim A.H. Long-term outcomes of surgery for invasive valvular endocarditis involving the aortomitral fibrosa. Ann Thorac Surg. 2019;108:1314–1323. doi: 10.1016/j.athoracsur.2019.04.119. [DOI] [PubMed] [Google Scholar]
- 7.Tsai L.L., Grant A.K., Mortele K.J., Kung J.W., Smith M.P. A practical guide to MR imaging safety: what radiologists need to know. Radiographics. 2015;35:1722–1737. doi: 10.1148/rg.2015150108. [DOI] [PubMed] [Google Scholar]
- 8.Blissett S., Chetrit M., Kovacina B., Mardigyan V., Afilalo J. Performing cardiac magnetic resonance imaging in patients with cardiac implantable electronic devices: a contemporary review. Can J Cardiol. 2018;34:1682–1686. doi: 10.1016/j.cjca.2018.09.009. [DOI] [PubMed] [Google Scholar]
- 9.McGuinn E.M., Bhatia N., O'Leary J.M., Crossley G.H., Rottman J.N. Emergent use of an MRI-conditional external pacemaker in a patient with sinus arrest facilitating diagnosis of a temporal lobe neoplasm. HeartRhythm Case Rep. 2016;2:296–299. doi: 10.1016/j.hrcr.2016.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chaudhry U., Svensson J., Mosen H., Mortsell D. Cardiac magnetic resonance imaging in a patient with temporary external pacemaker: a case report. Eur Heart J Case Rep. 2019;3:1–4. doi: 10.1093/ehjcr/ytz228. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Post-MRI chest roentgenograph. Chest roentgenograph demonstrating unchanged lead position following successful MRI.
Transthoracic echocardiogram.
Cardiac CT.