Highlights
-
•
The CDC is prioritizing HPV catch-up vaccination; college students are ideal targets.
-
•
Risk perception can drive HPV vaccination behavior, but it is a complex construct.
-
•
Affective and cognitive risk are components of HPV vaccine decision making.
Keywords: Perceived risk, HPV vaccine intentions, Cancer prevention, College students
Abstract
The HPV vaccine is recommended for all adolescents starting at age 11, but coverage is low, especially in the young adult population. The CDC is prioritizing catch-up vaccination and has expanded recommendations for all young adults to age 26. College students may be ideal targets for HPV vaccine interventions as they typically have on-site clinics that offer prevention services and students are in the position to make decisions about their own healthcare. We examined the risk perceptions of 101 HPV vaccine-naïve college students, both in terms of risk cognition (beliefs about susceptibility to HPV-related cancers and genital warts) and affect (worry and fear regarding HPV-related health outcomes) as they relate to HPV vaccine intentions. Participants completed an online survey, reporting absolute and comparative risk perceptions for HPV-related cancers/genital warts, fear and worry related to getting HPV-related cancer and/or genital warts, desire for positive emotions, affective associations with the HPV vaccine, and intentions to get the HPV vaccine. More fear/worry about vaccination was directly associated with increased vaccine intentions. The perceived risk to intentions relation included an indirect effect via fear/worry. Desire for positive affect strengthened this relation. Positive affective associations with the HPV vaccine were also related to increased vaccine intentions. Given the public health impact of increasing HPV vaccine coverage for young adults, educational strategies framing the HPV vaccine positively while decreasing fear/worry related to negative health outcomes might increase interest in on-campus catch-up vaccination.
1. Introduction
In the United States, human papillomavirus (HPV) is the most commonly diagnosed sexually transmitted infection (Satterwhite et al., 2013). The HPV vaccine, which has been recommended for adolescent and young adult women since 2006 and adolescent and young adult men since 2009 (CDC, 2016), is expected to significantly reduce incidence of HPV, with the overarching goal of reducing morbidities related to the virus. Since the introduction of the HPV vaccine, population coverage has remained low. While Healthy People 2020 goals include 80% coverage of the two dose nanovalent vaccine for adolescents ages 13–15 (ODPHP, 2020), only 49% of 13–17 year-olds in the United States received all recommended doses in 2017 (CDC, 2018). Data from the same survey showed that over 80% of same age adolescents had received Tetanus, Diphtheria, Pertussis, and Meningococcal vaccines, which are recommended to be given concomitantly with the HPV vaccine. While squamous cell cervical cancer rates have slightly decreased due to secondary prevention pap screening, rates of HPV-attributable oropharyngeal cancers are on the rise (Mourad et al., 2017). Thus, it is important to increase HPV vaccine coverage for both young women and men as a key primary prevention tool.
College students are a key population to prioritize in terms of HPV vaccine uptake and coverage. HPV vaccination policies have recently shifted to target pre and early-pubertal adolescents prior to age 13 (Bernstein et al., 2017a, Bernstein et al., 2017b, Meites et al., 2016). Evidence suggests adolescents ages 13 and older are less likely to complete the HPV vaccine series. Currently, 23 million young adults ages 19–26 are unvaccinated (Williams et al., 2017). In 2016, only 16% of unvaccinated 13 to 17-year olds received both doses. Additionally, adolescents were less likely to initiate the HPV vaccine as age increased, with only 7% initiation after age 15 (Bednarczyk et al., 2019). Such low vaccination rates highlight the need for effective catch-up vaccination strategies targeting young adult populations outside of the recommended vaccination schedule. In fact, the CDC Advisory Committee on Immunization practices recently recommended an expansion of the age range for vaccination to 26 years for both men and women, and for clinicians to engage in shared decision making with older patients (ages 27–45) who might benefit from its use (CDC, 2019).
Students on a college campus may be ideal targets for HPV vaccine decision-making interventions as most American four-year university campuses have on-site health services that offer the vaccine at free or low cost to students (Barnard et al., 2017), alleviating some of the common structural barriers associated with low vaccination rates in other contexts (Fisher et al., 2016). Unlike younger adolescent populations who rely on parents and pediatricians to make vaccination decisions, college students make their own decision about healthcare. In addition, college health centers are accustomed to providing prevention services and sexual healthcare to emerging adults (Eisenberg et al., 2012, Coor et al., 2018). As increasing HPV vaccine coverage is a national priority (ODPHP, 2020), it is important to understand factors that impact college students’ HPV vaccine decision making.
One component of health decision making is a feeling state or emotion associated with a specific prevention behavior, or an affective association. These affective associations have been shown to directly relate to preventive health behaviors, including cancer screening (Brown-Kramer and Kiviniemi, 2015, Kiviniemi et al., 2014, Klasko-Foster et al., 2018), fruit and vegetable consumption (Kiviniemi and Duangdao, 2009), and physical activity (Kiviniemi et al., 2007). In the context of prevention behavior, changing the way individuals feel about a behavior has been shown to improve a desired health behavior. For instance, an experimental study randomly priming participants with positive, negative, and neutral affective associations with condom use prior to a condom selection task resulted in greater number of condoms taken for individuals receiving the positive affect manipulation (Ellis et al., 2015). As such, a better understanding of how young adults feel about both the HPV vaccine and HPV-related health outcomes may inform communication strategies and educational initiatives to increase catch-up HPV vaccination for college students.
1.1. The role of risk perceptions in predicting HPV vaccine behavior
Risk perceptions, which are comprised of both beliefs about the likelihood of acquiring a disease (cognitions) and emotions associated with a disease outcome (affect), have been studied in the context of HPV in young adult populations, however; they have typically been modeled as two distinct main effects (Reiter et al., 2010, Bennett et al., 2012, Gilbert et al., 2011). Previous research focused on cognitive aspects of risk perception in a college student population shows that increased perceived risk of an HPV-related disease outcome was positively associated with self-efficacy to get vaccinated, which in turn influenced vaccine intentions (Christy et al., 2019). Male college students who believed they were susceptible to the HPV virus were more likely to talk to a provider about getting the HPV vaccine (Katz et al., 2012) and had greater intentions to get the vaccine (Gerund and Barley, 2009). By understanding the relative importance and interplay between cognitive and affective components of risk in this population, we can tailor interventions to maximize HPV vaccine uptake for young adults utilizing college campus health services.
When affective components of perceived risk for HPV-related health outcomes have been examined, constructs such as fear and worry have been modeled in separate studies from cognitive risk perceptions or as two independent main effects. Among young adult men who have sex with men, increased worry about getting HPV predicted increased vaccine intentions (Cummings et al., 2015). Vaccinated college students reported in a qualitative study that getting the HPV vaccine attenuated worry about getting an STI in the future (Pitts et al., 2017). Research assessing the separate effects of both affective and cognitive risk components on HPV vaccine intentions in college students has shown mixed results. One experimental study manipulating the level of perceived vulnerability (both affective and cognitive) of acquiring HPV-related cancer and genital warts through message framing found both affective and cognitive components to be separate predictors of HPV vaccine intentions in college students, with larger effect sizes for affective predictors (Richards, 2016). Other work modeling HPV-related worry and perceived susceptibility of the HPV virus separately on HPV vaccine intentions among male college students found that worry, but not cognitively-based risk perceptions predicted intentions (Grace-Leitch and Shneyderman, 2016). Research including main effects of both cognitively-based risk perception and anticipated emotions on HPV vaccine intentions in male and female college students found that when both types of risk components were included in the same model, only the emotional component (anticipated regret about not getting vaccinated and subsequently acquiring an HPV-related health issue) significantly predicted vaccine intentions for men (Christy et al., 2016). Although past work has identified both affective and cognitive components of risk perceptions as predictors of HPV vaccine intentions, the relationship between these variables and the resulting impact on HPV vaccine intentions has not been explored. Given the evidence for the effects of both affective and cognitively-based risk perceptions in predicting HPV vaccine intentions, it is important to understand the interplay between these two components. This study provides an initial examination of a key theory-driven hypothesis – that while both affective and cognitive components of perceived risk are related to HPV vaccine intentions, cognitively-based risk perceptions will indirectly influence vaccination intentions through the path of affective components of perceived risk (Kiviniemi et al., 2018).
1.2. The behavioral affective associations model
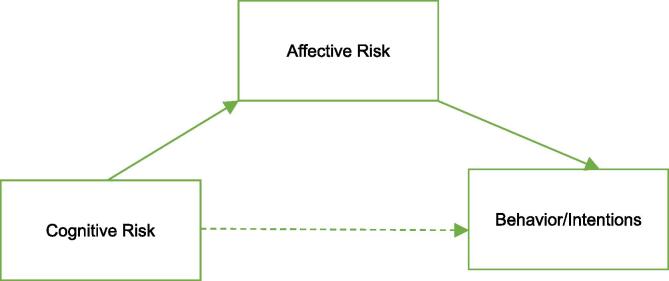
The behavioral affective associations model has been used as a framework to explain how the interplay between affect and cognitions associated with a behavior drive behavioral engagement (Kiviniemi et al., 2007). This model of health decision making posits that both cognitions and affect are related to decisions to engage in or avoid a behavior; however, affective associations mediate the relation between cognitions and behavioral practice (Kiviniemi et al., 2007, Kiviniemi and Klasko-Foster, 2018). Fig. 1 presents the hypothesized relation between variables in the behavioral affective associations model. Past work using the behavioral affective associations model has found that affective components of risk (worry about getting a disease) tend to be more proximal influences on behavioral engagement than cognitive components, such as beliefs about personal susceptibility to a disease (Kiviniemi and Ellis, 2014, Zhao, 2016, Klasko-Foster et al., 2019). Thus, it is important to measure both affective and cognitive components of perceived risk in order to account for more variability in behavior/intentions.
Fig. 1.
The behavioral affective associations model. *Solid lines represent indirect effects of affective risk on the relation between cognitive risk and behavior, dashed lines represent the absence of a direct effect between cognitive risk and behavior when affective risk is added to the model.
1.3. Ideal affect and affective associations with the HPV vaccine
Ideal affect is a construct that evaluates not how a person actually feels, but how someone would ideally like to feel. While people may have attitudes about many types of affect, they may only want to feel specific affective states (Tsai, 2007). As such, while most people value positive affective states over negative, they differ in valuation of arousal both individually and cross-culturally. Ideal affect differs from social norms in that ideal affect is the way people want to feel, which is not always the same as what people think they should feel; however, there are cultural differences in valuation of arousal. High arousal positive affect (excitement) has been shown to be more desirable among people from Western cultures, while low arousal positive affect (serenity) has been shown to be more desirable among people from Eastern cultures (Tsai, 2007, Tsai et al., 2006, Sims and Tsai, 2015). Differences between actual affect and ideal affect motivate behavior that will get an individual closer to their ideal affective state (Tsai, 2007). Worry and fear are both high arousal negative affective states. Given previous work showing that disparities between actual and ideal affect can motivate behavior (Tsai, 2017), the relation between affectively-based perceived risk may be strengthened when individuals have more high arousal negative affect associated with genital warts and cancer, the two primary morbidities of HPV infection, but value low arousal positive affect. As such, we are interested in the extent that a discrepancy between actual and ideal affect moderates the relation between perceived risk of HPV-related health outcomes and HPV vaccine intentions.
Finally, we are interested in how affective associations with the HPV vaccine itself influences HPV vaccine intentions. Across behavioral domains, affect is a strong predictor of behavioral engagement (Kiviniemi and Klasko-Foster, 2018). Evidence for the effects of affective associations on health decision making can be found in recent research on eating behaviors (Kiviniemi and Duangdao, 2009, Walsh and Kiviniemi, 2014, Jun and Arendt, 2016), smoking (Lawton et al., 2007), physical activity (Kiviniemi et al., 2007, Lawton et al., 2009, Helfer et al., 2015), cancer screening (Brown-Kramer and Kiviniemi, 2015, Kiviniemi et al., 2014, Klasko-Foster et al., 2019, Zhao and Nan, 2016), sunscreen use (Kiviniemi and Ellis, 2014), and donating biospecimens for research (Kiviniemi et al., 2013). To our knowledge, the relations between positive and negative affective associations with the HPV vaccine and behavioral intentions has not been tested
1.4. Current study
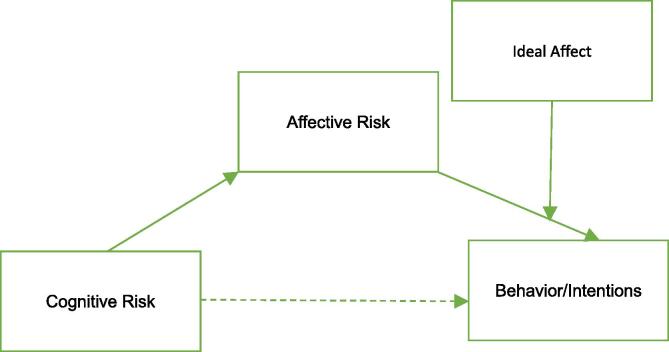
We are interested in whether affect and cognitions associated with risk for two HPV-related disease outcomes (genital warts and cancer), are associated with vaccination intentions. Based on the behavioral affective associations model, we hypothesize that both cognitive and affective components of perceived risk for genital warts and HPV-related cancer will have significant effects on future HPV intentions (hypothesis 1). According to the behavioral affective associations model, affective components will mediate the relation between cognitive components and future vaccine intentions and affective components will be associated with HPV vaccine behavior even after accounting for the influence of cognitive components (hypothesis 2). When ideal affect is added to this model, (Fig. 2) we hypothesize that high arousal positive ideal affect will increase the strength of the relation between affective components of perceived risk and intentions to get the HPV vaccine (hypothesis 3). Finally, we hypothesize that stronger positive affective associations and weaker negative affective associations with the HPV vaccine itself will encourage individuals to engage in HPV vaccination behavior (hypothesis 4).
Fig. 2.
A conceptual model, including ideal affect.
2. Materials and methods
2.1. Participants and procedures
Participants, ages 18–26, were recruited from a college campus via posted flyers in common areas of buildings and emailed flyers sent through student interest groups (e.g. the Asian American Student Union) with a link inviting interested participants to complete an online questionnaire. Recruitment occurred in two waves; the first wave of recruitment occurred during fall semester 2017 and the second wave occurred during fall semester 2018. Eligibility criteria included young adults age-eligible for the HPV vaccine who had not been exposed to the HPV vaccine prior to study enrollment and felt comfortable reading and answering survey questions in English. Individuals who screened eligible were consented to participate online. Participants who completed the cross-sectional survey (average time to completion was 45 min) were offered $10 in credits added to their university identification cards (wave 1) or $10 electronic Amazon gift cards (wave 2). To estimate the necessary sample size, we followed Fritz and Mackinnon’s guidelines to detect a small to moderate effect (b’s between 0.14 and 0.25) for both indirect paths in a mediation model utilizing bias-corrected bootstrapping (Fritz and MacKinnon, 2007). The study protocol was approved by the Institutional Review Board at xxxx (omitted for blind review).
2.2. Measures
2.2.1. HPV knowledge and awareness
Items were selected from previous studies (Reiter et al., 2010, Licht et al., 2010). To gauge awareness, participants were asked, “Have you heard of the HPV vaccine before today?” with response options: yes, no, and don’t know. Fourteen questions were asked to measure knowledge, each with response options: yes, no, don’t know. A total knowledge score was computed by summing all correct answers (range 0–14). Participants were asked questions regarding whether HPV causes problems for women and men, modes of transmission, HPV-related negative health outcomes, HPV prevalence, risk behaviors.
2.2.2. Cognitively-based perceived risk
Participants responded to items assessing absolute risk and comparative risk for multiple HPV-related morbidities, including genital warts, cervical cancer, anal cancer, and oral cancer; adapted from previous work (Reiter et al., 2009, Moser et al., 2007). For each morbidity, participants who had no previous exposure to the HPV vaccine were asked the following to measure absolute risk, “What is the chance that you will ever get____?” on a 5-point Likert scale, with endpoints of 1 = no chance and 5 = high chance. Comparative risk was assessed with the following question: “Compared to others of your age and gender, how likely are you to get ____?” with response options of less likely, equally likely, and more likely.
2.2.3. Affectively-based perceived risk
Participants responded to single items assessing worry and fear about a) cancer and b) genital warts: “How worried are you about getting ____?” and “How afraid are you of getting ____?” (Moser et al., 2007). Response options were on a 5-point scale with endpoints 1 = not at all and 5 = extremely.
2.2.4. Ideal affect
Ideal affect was measured using 25 items adapted from Tsai and Knutson (2005). For this analysis, only the 6 items that measured high arousal and low arousal positive affect were included. For each type of affective state, participants were asked to report how often he/she would ideally like to feel that affective state on a 5-point Likert scale with endpoints 1 = not at all and 5 = all of the time. High arousal positive ideal affect included three affective states (enthusiastic, excited, elated) and low arousal positive ideal affect included three affective states (calm, relaxed, serene). Mean measures for each subscale were computed for analysis. Reliability for the high arousal positive ideal affect was α = 0.72 and low arousal positive ideal affect was α = 0.66, which is consistent with other literature measuring ideal affect (Tsai et al., 2006).
2.2.5. Affective associations with the HPV vaccine
Affective associations were assessed by asking respondents to think about the HPV vaccine and then report agreement with four positive affective states (e.g. “Do you feel relaxed?), and five negative affective states (“Do you feel sad?”) on a 5-point scale with endpoints 1 = not at all and 5 = extremely using a modified measure of affective attitude components (Crites et al., 1994). Modifications were made to separate positive and negative affective states and mean scores were created (Kiviniemi, 2018). Reliability for the positive and negative affective association scales were α = 0.94 and α = 0.92, respectively. Both individual items and aggregate scales were used in analyses.
2.2.6. Outcome measures
Key outcomes for this study were HPV vaccination intentions (Reiter et al., 2010, Gerend et al., 2008). Past vaccine behavior was measured by asking how many shots of the HPV vaccine each participant had received. “Don’t know” responses were not included in this analysis. Intentions were analyzed for HPV vaccine naïve individuals only (participants reported 0 shots received). Participants were asked on a 5-point Likert scale how likely they were to get the HPV vaccine in the next twelve months. Responses were on a 5-point Likert scale with endpoints of 1 = not at all likely to 5 = extremely likely.
2.3. Analysis plan
All analyses were conducted using SPSS 24. Descriptive analyses, including percentages, means and standard deviations, were performed on the demographic characteristics of the participants (age, gender, race, country of origin) and on the outcome and predictor variables. Linear regression was used to test models of each component of risk separately on HPV vaccine intentions. We estimated mediation models using bootstrap estimation via the SPSS PROCESS macro (Hayes, 2012). Next, ideal affect was added to the mediation models to assess any interaction with affective risk perceptions. We tested associations between individual and the aggregate positive and negative affective associations with the HPV vaccine and HPV vaccination intentions using linear regression. Parallel models were assessed and compared, both including and excluding age, gender, and race. There were no differences in significance, magnitude and direction of effects between models. As such, results reported below are the most parsimonious models and do not include demographic controls. As male HPV vaccine completion rates lag behind those for women, we used analysis of variance to determine differences in each risk perception variable by sex. No significant differences were present (Table 1).
Table 1.
Mean risk perceptions and significant differences by gender (n = 101).
| Construct | Men (n = 39) | Women (n = 62) | F-Ratio | p-value |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | |||
| Absolute risk: genital warts | 2.23 (0.68) | 2.10 (0.81) | 0.60 | 0.44 |
| Absolute risk: HPV-related cancer | 2.14 (0.64) | 2.13 (0.81) | 0.004 | 0.95 |
| Comparative risk: genital warts | 1.35 (0.63) | 1.36 (0.64) | 0.004 | 0.95 |
| Comparative risk: HPV-related cancer | 1.48 (0.72) | 1.35 (0.65) | 0.61 | 0.44 |
| Worry: genital warts | 2.16 (0.95) | 2.18 (1.28) | 0.01 | 0.92 |
| Worry: HPV-related cancer | 2.21 (1.02) | 2.37 (1.23) | 0.45 | 0.51 |
| Fear: genital warts | 2.11 (0.86) | 2.37 (1.26) | 1.26 | 0.27 |
| Fear: HPV-related cancer | 2.32 (0.99) | 2.51 (1.42) | 0.53 | 0.47 |
3. Results
3.1. Participant characteristics
Of the 423 individuals who clicked on the electronic survey link, 288 completed the questionnaire. Observations were excluded from this analysis if they had already been exposed to the HPV vaccine or reported “don’t know” for past vaccination behavior (n = 174), if they did not pass three of the seven attention control tests throughout the survey (n = 5), or if they were not current University students (n = 8). Demographic characteristics of participants are shown in Table 2. Study participants ranged in age from 18 to 26 (mean age = 21). Almost two thirds of the sample identified as female, 45% self-reported white race, and 26% were international students.
Table 2.
Participant Characteristics (n = 101).
| N | M (SD) or % | ||
|---|---|---|---|
| Age | 101 | 21.0 (2.2) | |
| Sex | Male | 39 | 38.6 |
| Female | 62 | 61.4 | |
| Race | White | 45 | 44.6 |
| Asian | 39 | 38.6 | |
| Black/African American | 10 | 9.9 | |
| American Indian /Alaska Native | 1 | 1.0 | |
| Other | 6 | 5.9 | |
| Type of student | International | 26 | 25.7 |
| Domestic | 75 | 74.3 | |
| Highest education level completed | High school | 5 | 5.0 |
| College 1st year | 12 | 11.9 | |
| College 2nd year | 25 | 24.8 | |
| College 3rd year | 26 | 25.7 | |
| College 4th year | 16 | 15.8 | |
| Graduate school 1st year | 10 | 9.9 | |
| Graduate school 2nd year | 5 | 5.0 | |
| Graduate school 4th year | 2 | 1.9 | |
While 85% of participants were aware of HPV and 78% were aware that an HPV vaccine was available to them, neither type of awareness measure was associated with behavioral intentions to get the vaccine. Similarly, HPV knowledge was not associated with vaccine intentions. Mean scores on the 14-point knowledge measure were 6.5 (SD = 3.8).
3.2. Do both cognitive and affective risk perceptions influence HPV vaccine intentions?
The direct effects of each cognitive (absolute and comparative risk) and affective (worry and fear) risk variable for both genital warts and HPV-related cancer were estimated using separate linear regression models (Table 3). Greater absolute and comparative risk for genital warts was associated with greater vaccine intentions. Greater fear and worry about getting genital warts was also positively associated with HPV vaccine intentions. For HPV-related cancer risk perceptions, greater absolute risk, cancer worry, and cancer fear were associated with greater vaccine intentions. Comparative risk for HPV-related cancer was not significantly associated with HPV vaccine intentions.
Table 3.
Direct effects of perceived risk variables on intentions to get the HPV Vaccine in the next 12 months, classified by health outcome (n = 101).
| Risk variable | Genital warts | HPV-related cancer* |
|---|---|---|
| Absolute risk | b = 0.39, p < 0.001 | b = 0.26, p < 0.05 |
| Comparative risk | b = 0.25, p < 0.05 | b = 0.15, p = 0.21 |
| Worry | b = 0.42, p < 0.001 | b = 0.29, p < 0.01 |
| Fear | b = 0.43, p < 0.001 | b = 0.23, p < 0.05 |
*HPV-related cancer includes questions about HPV-related anal, oral, and cervical cancers. For male respondents, only HPV-related anal and oral cancer questions were presented.
3.3. Do affective components of perceived risk mediate the relation between cognitive components and intentions?
We took a three-step approach to determine whether the effects of cognitively-based risk perceptions were indirectly associated with HPV vaccine intentions through the path of affective components of perceived risk. First, we estimated regression models with cognitive risk variables predicting each affective risk component independently. We found significant, positive associations for each relation (Table 4). Next, we used bootstrap estimation to model the indirect effects of each affective risk component as independent mediators of the relation between cognitively-based perceived risk and HPV vaccine intentions. Results of mediation analyses are shown in Table 5. The association between absolute risk of genital warts and HPV vaccine intentions was partially mediated by fear, but not worry. Affective components of risk (fear/worry) did not mediate the relation between absolute risk of HPV-related cancer and HPV vaccine intentions. The association between comparative risk of genital warts and vaccine intentions was fully mediated by both worry and fear. The relation between comparative risk of HPV-related cancer and HPV vaccine intentions was fully mediated by worry, but not fear. Last, we examined the independent influences of affective components on each significant mediation model. The residual score representing the portion of variance of each affective variable not related to cognitive risk in each model was calculated. HPV vaccine intentions were regressed on each residual score. The residual slopes were significant for fear of genital warts in both cognitive risk models (absolute risk: b = 0.25, p < 0.05; comparative risk: b = 0.37, p < 0.01). Residual slopes were also significant for all mediation models including comparative risk and worry (comparative risk for genital warts: b = 0.34, p < 0.01; comparative risk for HPV-related cancer: b = 0.24, p < 0.05). These significant relations indicate an independent effect of affectively-based perceived risk on vaccine intentions.
Table 4.
Univariable relations between cognitively-based risk perceptions and affectively-based risk perceptions (n = 101).
| Risk variable | Worry | Fear |
|---|---|---|
| Absolute risk: genital warts | b = 0.38, p < 0.01 | b = 0.30, p < 0.01 |
| Absolute risk: HPV-related cancer | b = 0.55, p < 0.001 | b = 0.39, p < 0.001 |
| Comparative risk: genital warts | b = 0.35, p < 0.01 | b = 0.28, p < 0.05 |
| Comparative risk: HPV-related cancer | b = 0.39, p < 0.01 | b = 0.27, p < 0.05 |
Table 5.
Affectively-based Perceived Risk as a Mediator of the Relation between Cognitively-based Risk Perceptions and HPV Vaccine Intentions in the Next 12 Months (n = 101).
| Cognitive Risk | Affectively-based Perceived Risk |
|||
|---|---|---|---|---|
| Worry (cancer or genital warts) |
Fear (Cancer or genital warts) |
|||
| Direct | Indirect | Direct | Indirect | |
| Absolute risk genital warts |
0.40 (0.12, 0.69) |
0.09 (−0.01, 0.27) |
0.40 (0.13, 0.27) |
0.10 (0.01, 0.30) |
| Absolute risk cancer | 0.24 (−0.10, 0.58) |
0.14 (−0.05, 0.35) |
0.32 (0.01, 0.63) |
0.01 (−0.03, 0.24) |
| Comparative risk warts | 0.20 (−0.18, 0.58) |
0.20 (0.05, 0.43) |
0.23 (−0.13, 0.59) |
0.17 (0.04, 0.39) |
| Comparative risk cancer | 0.07 (−0.28, 0.44) |
0.15 (0.01, 0.40) |
0.15 (−0.20, 0.50) |
0.07 (−0.002, 0.23) |
3.4. Does positive ideal affect strengthen the relation between affectively-based risk perceptions and HPV vaccine intentions?
We completed the moderated mediation analysis using the PROCESS macro to obtain bootstrapped confidence intervals for the aforementioned mediation models at different levels of positive ideal affect. Moderation was assessed on the path between the mediator and outcome variable. It was expected that people who valued high arousal positive emotions, such as excitement, relatively more than others would have stronger associations between affective components of perceived risk and HPV vaccine intentions. Moderated mediation was present in models in which both fear and worry about genital warts mediated the relation between cognitive risk components and HPV vaccine intentions. For all models, interactions were assessed by testing the conditional indirect effects of affective risk at three levels of either high arousal or low arousal positive ideal affect: the mean, one standard deviation above the mean, and one standard deviation below the mean.
Both high and low arousal positive ideal affect significantly moderated the relation between perceived risk and HPV vaccine intentions such that when individuals had moderate to high positive ideal affect, the relation between affective components of risk and HPV vaccine intentions was stronger compared to those with lower positive ideal affect. In all models with significant indices of moderated mediation, indirect effects of affectively-based risk perceptions were strongest and significant at higher levels of positive ideal affect. When the relation between absolute risk for genital warts and HPV vaccine intentions was mediated by worry, the index of moderated mediation was significant for high arousal positive ideal affect (index = 0.12; 95% CI, 0.01–0.30; R2 = 0.26). The indirect effects of worry were significant for participants with moderate (b = 0.11; 95% CI, 0.02 to 0.27) and high (b = 0.21; 95% CI, 0.05–0.44), but not low (b = 0.01; 95% CI, −0.13 to 0.14) levels of high arousal ideal affect. The index of moderated mediation was also significant for low arousal positive ideal affect (index = 0.12; 95% CI, 0.02–0.29; R2 = 0.23). The indirect effects of worry were significant for participants with moderate (b = 0.13; 95% CI, 0.02–0.34) and high (b = 0.22; 95% CI, 0.05–0.50), but not low (b = 0.04; 95% CI, −0.06 to 0.22) levels of low arousal ideal affect.
When fear was modeled as a mediator in the relation between absolute risk for genital warts and HPV vaccine intentions, patterns were similar for both high arousal ideal affect (index = 0.09; 95% CI, 0.004–0.30; R2 = 0.28) and low arousal ideal affect (index = 0.10; 95% CI, 0.01–0.29; R2 = 0.26). The indirect effects of fear were significant for participants with moderate (b = 0.12; 95% CI, 0.03–0.28) and high (b = 0.20; 95% CI, 0.03–0.43), but not low (b = 0.05; 95% CI, −0.07 to 0.18) levels of high arousal ideal affect. The indirect effects of fear were significant for participants with moderate (b = 0.12; 95% CI, 0.03–0.28) and high (b = 0.19; 95% CI, 0.04–0.41), but not low (b = 0.04; 95% CI, −0.07 to 0.18) levels of low arousal ideal affect. Neither high nor low arousal positive ideal affect changed the relations between any of the variables in models estimating comparative risk for genital warts and absolute and comparative risk for HPV-related cancers.
3.5. Do affective associations with the HPV vaccine itself predict vaccine intentions?
We used linear regression to estimate associations between aggregate responses for positive and negative affective associations, and individual affective associations as predictors of HPV vaccine intentions. Positive affective associations were associated with increased HPV vaccine intentions (b = 0.33, p < 0.01). In addition, each of the positive individual affective associations with the HPV vaccine were significantly related to greater vaccine intentions (happy: b = 0.29, p < 0.01; delighted: b = 0.35, p < 0.01; satisfied: b = 0.30, p < 0.01; relaxed: b = 0.36, p < 0.001). Neither aggregate (b = −0.03, p = 0.78) nor individual negative affective associations (disgusted: 0.02, p = 0.83; angry: b = −0.01, p = 0.96; annoyed: b = 0.004, p = 0.97; sad: b = 0.04, p = 0.71; afraid: b = 0.02, p = 0.85) were significantly related to HPV vaccine intentions.
4. Discussion
Although awareness of the HPV vaccine was high in this population, accurate knowledge about HPV was low. On average, participants correctly answered fewer than half of the HPV knowledge questions. This is consistent with other work assessing HPV knowledge/vaccine awareness among college students (Albright and Allen, 2018, Cooper et al., 2018, Fisher et al., 2014, Thompson et al., 2016). As such educational intervention may be necessary to persuade unvaccinated students of the worthiness of this preventive health behavior, especially as accurate HPV knowledge is related to increased intentions for college students to obtain the vaccine in other work (Cooper et al., 2018).
Affect, whether it is associated with risk perceptions about a disease state or with a vaccine, or valued as an ideal state, is important to understanding HPV vaccine intentions in a college student population. Worry and fear were associated with HPV vaccine intentions and both worry and fear mediated relations between cognitively-based perceived risk and behavioral intentions. Furthermore, worry and fear were related to HPV vaccine intentions over and above cognitions about risk, as established through an independent pathway analysis. These findings are consistent with the behavioral affective associations model and indicate that affective components of risk may play a central role in primary prevention decision making.
4.1. Implications
The mediated relation between cognitive and affectively-based risk perceptions as influencers of HPV vaccine intentions has implications for understanding how risk informs decision making for primary prevention behaviors. This work underscores that the measurement of risk perceptions should include assessments of both affective and cognitive components. By only assessing cognitive components, we are unable to assess the possible connection between risk perceptions and worry/fear about HPV-related health outcomes, which may drive behavioral intentions. Relatedly, interventions that only work to change cognitive risk perceptions may exclude affective risk perceptions that are critical to decision making and thus, the effectiveness of the intervention.
Evidence exists for the effect of anticipatory emotions in vaccination decision making (Christy et al., 2016, Chapman and Coups, 2006, Weinstein et al., 2007). In this study, both valuing high and low arousal positive affect moderated the mediated relation between risk components and intentions, by strengthening the association between affective components of perceived risk and HPV vaccine intentions. Our findings show that cognitive and affectively-based perceived risk for both genital warts and HPV-related cancers had significant main effects and indirect effects on HPV intentions, but ideal affect only moderated the relation for fear and worry about genital warts, not HPV-related cancers. It could be the case that genital warts are associated with more negative affect than cancer; thus, more positive ideal affect is associated with a more immediate response. Finding that any positive ideal affect increases the strength of the relation between worry/fear and vaccine intentions paired with the knowledge that positive affective associations with the vaccine are behavior motivating has implications for health communication interventions. As worry/fear increases the likelihood that someone may get the vaccine, and that effect is intensified by wanting to feel more positive affect of any type, communication strategies could highlight the positive affect experienced after getting the vaccine, such as feeling peace of mind with the knowledge that the vaccine prevents lifetime risk of genital warts and HPV-related cancers.
This work shows that college students do have increased risk perceptions about HPV that are predictive of behavioral intentions. These findings may be useful as part of a health communication strategy on college campuses. Student health centers could be an ideal setting for vaccine naïve young adults to obtain preventive vaccinations; specifically, many students utilize these resources for primary care (Turner and Keller, 2015), and over 12 million young adults under age 25 are enrolled in American colleges and universities (NCES, 2018); however; campus health centers may not be providing easily accessible information about HPV vaccine education or availability. A recent analysis of college health center websites at 214 American universities found that only 50% mentioned HPV vaccine and only 32% of those provided any additional information such as costs and availability (Fontenot et al., 2016). Research regarding health communication approaches to increase HPV vaccine suggests a preference for strong, straight-forward recommendations (Malo et al., 2016). University health centers should work to include brief, direct information on their websites about the benefits of HPV vaccine, with particular attention to positive emotions and reduction of worry and fear. Additionally, student health services may consider the importance of increased availability of information using mass media and social media campaigns in general terms (e.g., sexual health programs) as well as specific services (e.g., catch-up vaccinations). Providers at student health centers can help increase student knowledge about HPV, which may help increase risk perceptions.
4.2. Limitations
Some limitations should be considered regarding this work. First, results are cross-sectional and limit our ability to make causal statements about relationships between risk components and subsequent impact on HPV vaccine intentions. This work adds to existing evidence that the behavioral affective associations model may accurately predict that cognitive risk perceptions elicit fear and worry and the latter motivate protective action; however, future longitudinal work is necessary to further understand whether worry and fear are causal mechanisms. Second, a convenience sample was used in this study. As such, this sample may not be representative of the general population of college students.
5. Conclusion
Current college students are a priority population for HPV vaccine intervention as they are age-eligible, likely to be unvaccinated or under-vaccinated, and have the ability to get vaccinated at no or low cost. Our work demonstrates that affective components of perceived risk guide HPV vaccine decision making. First, worry and fear about HPV-related health outcomes mediated the relation between cognitive risk assessment and HPV vaccine intentions. Second, positive ideal affect strengthened the relation between affective components of risk and HPV vaccine intentions. Third, affective associations with the HPV vaccine influenced behavioral intentions when they were positive, and not negative. As such, HPV related communications should focus on positive emotions associated with both the vaccine and the how the resulting protection from vaccination can attenuate worry and fear about deleterious HPV-related outcomes.
CRediT authorship contribution statement
Lynne B. Klasko-Foster: Conceptualization, Writing - original draft, Formal analysis. Sarahmona Przybyla: Supervision, Writing - review & editing. Heather Orom: Writing - review & editing. Elizabeth Gage-Bouchard: Writing - review & editing. Marc T. Kiviniemi: Writing - review & editing, Supervision, Methodology.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
Marc Diamond Research Foundation, University at Buffalo, SUNY.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.pmedr.2020.101195.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Albright A.E., Allen R.S. HPV misconceptions among college students: The role of health literacy. J. Commun. Health. 2018;43(6):1192–1200. doi: 10.1007/s10900-018-0539-4. [DOI] [PubMed] [Google Scholar]
- Barnard M., George P., Perryman M.L., Wolff L.A. Human papillomavirus (HPV) vaccine knowledge, attitudes, and uptake in college students: Implications from the Precaution Adoption Process Model. PLoS ONE. 2017;12(8) doi: 10.1371/journal.pone.0182266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bednarczyk R.A., Ellingson M.K., Omer S.B. Human papillomavirus vaccination before 13 and 15 years of age: analysis of national immunization survey teen data. J. Infect. Dis. 2019 doi: 10.1093/infdis/jiy682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett K.K., Buchanan J.A., Adams A.D. Social-cognitive predictors of intention to vaccinate against the human papillomavirus in college-age women. J. Soc. Psychol. 2012;152(4):480–492. doi: 10.1080/00224545.2011.639408. [DOI] [PubMed] [Google Scholar]
- Bernstein H.H., Bocchini J.A., Jr., Committee on Infectious D Practical approaches to optimize adolescent immunization. Pediatrics. 2017;139(3) doi: 10.1542/peds.2016-4187. [DOI] [PubMed] [Google Scholar]
- Bernstein H.H., Bocchini J.A., Jr., Committee on Infectious D The need to optimize adolescent immunization. Pediatrics. 2017;139(3) doi: 10.1542/peds.2016-4186. [DOI] [PubMed] [Google Scholar]
- Brown-Kramer C.R., Kiviniemi M.T. Affective associations and cognitive beliefs relate to individuals' decisions to perform testicular or breast self-exams. J. Behav. Med. 2015;38(4):664–672. doi: 10.1007/s10865-015-9641-6. [DOI] [PubMed] [Google Scholar]
- CDC. HPV Vaccine Recommendations. Vaccines and Preventable Diseases 2016; https://www.cdc.gov/vaccines/vpd/hpv/hcp/recommendations.html.
- CDC. HPV Vaccination Coverage Data. Human Papillomavirus (HPV) 2018; https://www.cdc.gov/hpv/hcp/vacc-coverage/index.html.
- CDC. Advisory Committee on Immunization Practices. 2019; https://www.cdc.gov/vaccines/acip/index.html. Accessed July 30, 2019, 2019.
- Chapman G.B., Coups E.J. Emotions and preventive health behavior: worry, regret, and influenza vaccination. Health Psychol. 2006;25(1):82–90. doi: 10.1037/0278-6133.25.1.82. [DOI] [PubMed] [Google Scholar]
- Christy S.M., Winger J.G., Raffanello E.W., Halpern L.F., Danoff-Burg S., Mosher C.E. The role of anticipated regret and health beliefs in HPV vaccination intentions among young adults. J. Behav. Med. 2016;39(3):429–440. doi: 10.1007/s10865-016-9716-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christy S.M., Winger J.G., Mosher C.E. Does self-efficacy mediate the relationships between social-cognitive factors and intentions to receive HPV vaccination among young women? Clin. Nurs. Res. 2019;28(6):708–725. doi: 10.1177/1054773817741590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper D.L., Zellner-Lawrence T., Mubasher M., Banerjee A., Hernandez N.D. Examining HPV awareness, sexual behavior, and intent to receive the HPV vaccine among racial/ethnic male college students 18–27 years. Am. J. Mens Health. 2018;12(6):1966–1975. doi: 10.1177/1557988318803163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coor A., Esie P., Dittus P.J., Koumans E.H., Kang J., Habel M.A. Assessment of sexual health services at US colleges and universities, 2001 and 2014. Sex. Health. 2018;15(5):420–423. doi: 10.1071/SH18014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crites S.L., Fabrigar L.R., Petty R.E. Measuring the affective and cognitive properties of attitudes: conceptual and methodological issues. Pers. Soc. Psychol. Bull. 1994;20(6):619–634. [Google Scholar]
- Cummings T., Kasting M.L., Rosenberger J.G., Rosenthal S.L., Zimet G.D., Stupiansky N.W. Catching up or missing out? Human papillomavirus vaccine acceptability among 18- to 26-year-old men who have sex with men in a US national sample. Sex. Transm. Dis. 2015;42(11):601–606. doi: 10.1097/OLQ.0000000000000358. [DOI] [PubMed] [Google Scholar]
- Eisenberg M.E., Lechner K.E., Frerich E.A., Lust K.A., Garcia C.M. Characterizing sexual health resources on college campuses. J Commun Health. 2012;37(5):940–948. doi: 10.1007/s10900-011-9536-6. [DOI] [PubMed] [Google Scholar]
- Ellis E.M., Homish G.G., Parks K.A., Collins R.L., Kiviniemi M.T. Increasing condom use by changing people's feelings about them: An experimental study. Health Psychol. 2015;34(9):941–950. doi: 10.1037/hea0000205. [DOI] [PubMed] [Google Scholar]
- Fisher H., Audrey S., Mytton J.A., Hickman M., Trotter C. Examining inequalities in the uptake of the school-based HPV vaccination programme in England: a retrospective cohort study. J. Public Health (Oxf). 2014;36(1):36–45. doi: 10.1093/pubmed/fdt042. [DOI] [PubMed] [Google Scholar]
- Fisher K.A., Cahill L., Tseng T.S., Robinson W.T. HPV vaccination coverage and disparities among three populations at increased risk for HIV. Transl. Cancer Res. 2016;5:S1000–S1006. [Google Scholar]
- Fontenot H.B., Fantasia H.C., Sutherland M.A., Lee-St J.T. HPV and HPV vaccine information among a national sample of college and university websites. J. Am. Assoc. Nurse Pract. 2016;28(4):218–223. doi: 10.1002/2327-6924.12312. [DOI] [PubMed] [Google Scholar]
- Fritz M.S., MacKinnon D.P. Required sample size to detect the mediated effect. Psychol. Sci. 2007;18(3):233–239. doi: 10.1111/j.1467-9280.2007.01882.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerend M.A., Shepherd J.E., Monday K.A. Behavioral frequency moderates the effects of message framing on HPV vaccine acceptability. Ann. Behav. Med. 2008;35(2):221–229. doi: 10.1007/s12160-008-9024-0. [DOI] [PubMed] [Google Scholar]
- Gerund M.A., Barley J. Human papillomavirus vaccine acceptibility among young adult men. Sex. Transm. Dis. 2009;36(1):58–62. doi: 10.1097/OLQ.0b013e31818606fc. [DOI] [PubMed] [Google Scholar]
- Gilbert P., Brewer N.T., Reiter P.L., Ng T.W., Smith J.S. HPV vaccine acceptability in heterosexual, gay, and bisexual men. Am. J. Mens Health. 2011;5(4):297–305. doi: 10.1177/1557988310372802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grace-Leitch L., Shneyderman Y. Using the health belief model to examine the link between HPV knowledge and self-efficacy for preventive behaviors of male students at a two-year college in New York City. Behav. Med. 2016;42(3):205–210. doi: 10.1080/08964289.2015.1121131. [DOI] [PubMed] [Google Scholar]
- Hayes A.F. (2012). PROCESS: A versatile computational tool for observed variable mediation, moderation, and conditional process modeling. Manuscript submitted for publication.
- Helfer S.G., Elhai J.D., Geers A.L. Affect and exercise: positive affective expectations can increase post-exercise mood and exercise intentions. Ann. Behav. Med. 2015;49(2):269–279. doi: 10.1007/s12160-014-9656-1. [DOI] [PubMed] [Google Scholar]
- Jun J., Arendt S.W. Undersanding healthy eating behaviors at casual dinging restaurants using the extended theory of planned behavior. Int. J. Hosp. Manage. 2016;53:106–115. [Google Scholar]
- Katz M.L., Kam J.A., Krieger J.L., Roberto A.J. Predicting HPV vaccine intentions of college-age males: An examination of parents and son's perceptions. J. Am. Coll. Health. 2012;60(6):449–459. doi: 10.1080/07448481.2012.673523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiviniemi M.T. Stucture and content of affective association with health behaviors: is the behavior 'good OR bad' or 'good AND bad'. Psychol. Health. 2018 doi: 10.1080/08870446.2017.1314476. [DOI] [PubMed] [Google Scholar]
- Kiviniemi M.T., Klasko-Foster L.B. The behavioral affective associations model. In: DM Williams RR, & MT Conner, ed. Affective Determinants of Health Behavior. New York, NY: Oxford University Press; 2018.
- Kiviniemi M.T., Duangdao K.M. Affective associations mediate the influence of cost-benefit beliefs on fruit and vegetable consumption. Appetite. 2009;52(3):771–775. doi: 10.1016/j.appet.2009.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiviniemi M.T., Ellis E.M. Worry about skin cancer mediates the relation of perceived cancer risk and sunscreen use. J. Behav. Med. 2014;37(6):1069–1074. doi: 10.1007/s10865-013-9538-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiviniemi M.T., Voss-Humke A.M., Seifert A.L. How do I feel about the behavior? The interplay of affective associations with behaviors and cognitive beliefs as influences on physical activity behavior. Health Psychol. 2007;26(2):152–158. doi: 10.1037/0278-6133.26.2.152. [DOI] [PubMed] [Google Scholar]
- Kiviniemi M.T., Saad-Harfouche F.G., Ciupak G.L. Pilot intervention outcomes of an educational program for biospecimen research participation. J. Cancer Educ. 2013;28(1):52–59. doi: 10.1007/s13187-012-0434-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiviniemi M.T., Jandorf L., Erwin D.O. Disgusted, embarrassed, annoyed: affective associations relate to uptake of colonoscopy screening. Ann. Behav. Med. 2014;48(1):112–119. doi: 10.1007/s12160-013-9580-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiviniemi M.T., Ellis E.M., Hall M.G. Mediation, moderation, and context: Understanding complex relations among cognition, affect, and health behaviour. Psychol. Health. 2018;33(1):98–116. doi: 10.1080/08870446.2017.1324973. [DOI] [PubMed] [Google Scholar]
- Klasko-Foster L.B., Jandorf L., Erwin D.O., Kiviniemi M.T. Predicting colonoscopy screening behavior and future screening intentions for African Americans over age 50. Behav. Med. 2018 doi: 10.1080/08964289.2018.1510365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klasko-Foster L.B., Kiviniemi M.T., Jandorf L., Erwin D.O. Affective components of perceived risk mediate the relation between cognitively-based perceived risk and colonoscopy screening. J. Behav. Med. 2019 doi: 10.1007/s10865-019-00049-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawton R., Conner M., Parker D. Beyond cognition: predicting health risk behaviors from instrumental and affective beliefs. Health Psychol. 2007;26(3):259–267. doi: 10.1037/0278-6133.26.3.259. [DOI] [PubMed] [Google Scholar]
- Lawton R., Conner M., McEachan R. Desire or reason: predicting health behaviors from affective and cognitive attitudes. Health Psychol. 2009;28(1):56–65. doi: 10.1037/a0013424. [DOI] [PubMed] [Google Scholar]
- Licht A.S., Murphy J.M., Hyland A.J., Fix B.V., Hawk L.W., Mahoney M.C. Is use of the human papillomavirus vaccine among female college students related to human papillomavirus knowledge and risk perception? Sex Transm Infect. 2010;86(1):74–78. doi: 10.1136/sti.2009.037705. [DOI] [PubMed] [Google Scholar]
- Malo T.L., Gilkey M.B., Hall M.E., Shah P.D., Brewer N.T. Messages to motivate human papillomavirus vaccination: national studies of parents and physicians. Cancer Epidemiol. Biomarkers Prev. 2016;25(10):1383–1391. doi: 10.1158/1055-9965.EPI-16-0224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meites E., Kempe A., Markowitz L.E. Use of a 2-dose schedule for human papillomavirus vaccination - updated recommendations of the advisory committee on immunization practices. MMWR Morb. Mortal. Wkly Rep. 2016;65(49):1405–1408. doi: 10.15585/mmwr.mm6549a5. [DOI] [PubMed] [Google Scholar]
- Moser R.P., McCaul K., Peters E., Nelson W., Marcus S.E. Associations of perceived risk and worry with cancer health-protective actions: data from the Health Information National Trends Survey (HINTS) J. Health Psychol. 2007;12(1):53–65. doi: 10.1177/1359105307071735. [DOI] [PubMed] [Google Scholar]
- Mourad M., Jetmore T., Jategaonkar A.A., Moubayed S., Moshier E., Urken M.L. Epidemiological trends of head and neck cancer in the United States: A SEER population study. J. Oral Maxillofac. Surg. 2017;75(12):2562–2572. doi: 10.1016/j.joms.2017.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCES. Fast Facts. 2018; https://nces.ed.gov/fastfacts/display.asp?id=372.
- ODPHP. Healthy People 2020. Immunization and Infectious Diseases 2019; https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives.
- Pitts M.J., Stanley S.J., Kim S. College males' enduring and novel health beliefs about the HPV vaccine. Health Commun. 2017;32(8):995–1003. doi: 10.1080/10410236.2016.1196421. [DOI] [PubMed] [Google Scholar]
- Reiter P.L., Brewer N.T., Gottlieb S.L., Mcree A.L., Smith J.S. Parents' health beliefs and HPV vaccination of their adolescent daughters. Soc. Sci. Med. 2009;69(3):475–480. doi: 10.1016/j.socscimed.2009.05.024. [DOI] [PubMed] [Google Scholar]
- Reiter P.L., Brewer N.T., Mcree A.L., Gilbert P., Smith J.S. Acceptability of HPV vaccine among a national sample of gay and bisexual men. Sex. Transm. Dis. 2010;37(3):197–203. doi: 10.1097/OLQ.0b013e3181bf542c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richards K. Intention of college students to receive the human papillomavirus vaccine. Health Educ. 2016;116(4):342–355. [Google Scholar]
- Satterwhite C.L., Torrone E., Meites E. Sexually transmitted infections among US women and men: prevalence and incidence estimates, 2008. Sex. Transm. Dis. 2013;40(3):187–193. doi: 10.1097/OLQ.0b013e318286bb53. [DOI] [PubMed] [Google Scholar]
- Sims T., Tsai J.L. Patients respond more positively to physicians who focus on their ideal affect. Emotion. 2015;15(3):303–318. doi: 10.1037/emo0000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson E.L., Vamos C.A., Sappenfield W.M., Straub D.M., Daley E.M. Relationship status impacts primary reasons for interest in the HPV vaccine among young adult women. Vaccine. 2016;34(27):3119–3124. doi: 10.1016/j.vaccine.2016.04.063. [DOI] [PubMed] [Google Scholar]
- Tsai J.L. Ideal affect: cultural causes and behavioral consequences. Perspect Psychol Sci. 2007;2(3):242–259. doi: 10.1111/j.1745-6916.2007.00043.x. [DOI] [PubMed] [Google Scholar]
- Tsai J.L. Ideal affect in daily life: implications for affective experience, health, and social behavior. Curr. Opin. Psychol. 2017;17:118–128. doi: 10.1016/j.copsyc.2017.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai J.L., Knutson B., Fung H.H. Cultural variation in affect valuation. J. Pers. Soc. Psychol. 2006;90(2):288–307. doi: 10.1037/0022-3514.90.2.288. [DOI] [PubMed] [Google Scholar]
- Turner J.C., Keller A. College health surveillance network: epidemiology and health care utilization of college students at US 4-year universities. J. Am. Coll. Health. 2015;63(8):530–538. doi: 10.1080/07448481.2015.1055567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh E.M., Kiviniemi M.T. Changing how I feel about the food: experimentally manipulated affective associations with fruits change fruit choice behaviors. J. Behav. Med. 2014;37:322–331. doi: 10.1007/s10865-012-9490-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein N.D., Kwitel A., McCaul K.D., Magnan R.E., Gerrard M., Gibbons F.X. Risk perceptions: assessment and relationship to influenza vaccination. Health Psychol. 2007;26(2):146–151. doi: 10.1037/0278-6133.26.2.146. [DOI] [PubMed] [Google Scholar]
- Williams W.W., Lu P.J., O'Halloran A. Surveillance of vaccination coverage among adult populations - United States, 2015. MMWR Surveill Summ. 2017;66(11):1–28. doi: 10.15585/mmwr.ss6611a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao N. The influence of absolute and comparative risk perceptions on cervical cancer screening and the mediating role of cancer worry. J. Health Commun. 2016;21(1):100–108. doi: 10.1080/10810730.2015.1033114. [DOI] [PubMed] [Google Scholar]
- Zhao X.Y., Nan X.L. The influence of absolute and comparative risk perceptions on cervical cancer screening and the mediating role of cancer worry. J Health Commun. 2016;21(1):100–108. doi: 10.1080/10810730.2015.1033114. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.