Abstract
Aim
To assess the oncological outcomes of patients with early breast cancer treated with breast-conserving surgery and adjuvant hypofractionated radiation therapy.
Methods and Material
This retrospective analysis included all patients ≥50 year of age with T1-2 N0 M0 breast cancer treated at our Radiation Oncology Unit between 2008 and 2011. Whole-breast radiation therapy was delivered to a dose of 42.5 Gy in 16 fractions, without boost. The primary outcome was local control.
Results
212 patients were identified. With a median follow up of 60 months, we found 3% local recurrence and 5.3% regional and/or distant recurrences. At the moment of data analysis, 17 patients had died. Out of 5 local recurrences, 2 had previously had a distant recurrence, both of them died. The other three were still alive at the last follow up. These results are comparable to those observed in Phase III trials that use this fractionation scheme.
Conclusions
The results obtained with this retrospective analysis are comparable to those obtained in large randomized trials. This data also supports the use of hypofractionated radiation therapy in Latin America. Hypofractionated radiation therapy for early breast cancer patients should be the standard adjuvant treatment.
Keywords: Early breast cancer, hypofrationated whole breast radiation therapy
1. Introduction
Breast cancer is the second most common cancer worldwide and the most frequent in women. It occupies the second place of cancer-related mortality in developed countries, and the first place in undeveloped countries (1).
The Early Breast Cancer Trialists’ Collaborative Group meta-analysis established the benefit of adjuvant radiation therapy after breast-conserving surgery in reducing locoregional and distant recurrence and breast cancer death (2). This meta-analysis included more than 10,000 women from 17 randomized controlled trials, most of which included treatment to doses around 50 Gy in 2 Gy per fraction, with or without boost to the lumpectomy cavity. One of the major considerations of radiation therapy is related precisely to the number of sessions needed. The treatment consisting of 5 to 7 weeks of daily fractions has been associated in the United States with 30% of patients not receiving adjuvant radiation therapy after breast-conserving surgery (3). This may be related to economic and patient-related issues(4).
Hypofractionation emerged as an attractive alternative based on the observed radiobiology of breast cancer (5,6), which suggests breast cancer has a lower α/β, close to 4, than other tumors such as squamous cell carcinoma. This led to the opening of multiple clinical trials ([7], [8], [9]) assessing the non-inferiority of hypofractionated treatments in terms of overall survival, local control and cosmesis, with up to 10 years of follow up ([10], [11], [12]). The good results obtained in those studies established the recommendation to treat selected patients with breast cancer with hypofractionated whole-breast radiation therapy with doses ranging from 40 Gy to 42.5 Gy according to different guidelines (13,14).
Breast cancer is a leading cause of cancer-related mortality in women globally (15) and also in Chilean women. Since 2005, breast cancer treatment has been guaranteed by law and performed according to national guidelines. Our Radiation Oncology Unit is considered a high-complexity center within the public health system and provides coverage to around 1.5 million people, with over 400 patients treated with adjuvant radiation therapy after breast cancer surgery in 2016. Hypofractionated whole-breast irradiation was adopted in 2008 as the standard treatment for women over 50 years of age with early, node negative breast cancer. The current report aims to analyze the outcomes of patients treated with hypofractionated whole-breast irradiation between 2008 and 2011.
As the molecular profile currently plays a major role in the prognostic and management of breast cancer ([16], [17], [18]), we attempt to perform an analysis for local recurrence according to molecular profiles.
2. Methods
For this retrospective review we included breast cancer patients treated between 2008 and 2011 in our radiation Oncology Unit. Inclusion criteria were T1-2 N0 M0 tumors, according to the American Joint Committee on Cancer 7th Edition, and age ≥50 years. All patients underwent breast-conserving surgery. All patients were treated with 3D conformal radiation therapy using 6 to 18 MV photons using opposed tangential fields. Fields were conformed using a multileaf collimator and wedges as needed. A hypofractionated whole breast irradiation (HF-WBI) dose of 42.5 Gy in 16 fractions was planned, no nodal irradiation or lumpectomy cavity boost was used. Treatment planning was performed using Varian Eclipse Software. The protocol was reviewed and approved by the local Ethics Committee.
The primary endpoint was local control, defined by means of local recurrence from the date of surgery until development of recurrence within the breast. Regional and distant recurrence were also analyzed from the moment of surgery until development of regional nodal recurrence or distant metastases, respectively. Information was retrieved until the last follow-up visit by reviewing clinical records from the Radiation Oncology Unit or Breast Pathology Unit, aiming at the most updated information. Patients were censored at last follow-up visit if no evidence of recurrent disease (by means of clinical, histological or imaging studies) or if they died without evidence of recurrent disease. Overall survival was defined as the time from date of breast surgery to the date of death from any cause. Survival analysis was performed using the Kaplan-Meyer method and log rank test.
Molecular classification was performed using immunohistochemistry techniques, when available according to local practice. Confirmatory c-erbB2 FISH was not performed routinely for equivocal 2+ or 3+ c-erbB2 immunohistochemistry in the period of time included in this study. Patients were classified into molecular subtypes using Hormone receptor and Her2 immunohistochemistry information when possible.
2.1. Results
A total of 212 patients were treated with hypofractionated whole breast radiation therapy between 2008 to 2011. All patients were female with a median age of 69.3 years (RIQ 63-74), 99% of whom were post-menopausic. Pathological and molecular features are described in Table 1. We were able to classify 70.7% of identified patients into molecular subtypes: 101 (67.3%) corresponding to Luminal patients, 42 (28%) Her2 and 7 (4.7%) who were Triple negative breast cancer subtype. Staging according to AJCC 7 and the prognostic AJCC 8 staging system was performed for patients whose data is available as detailed in Table 2.
Table 1.
Pathological and molecular tumor features.
| Tumor characteristic |
num – ( %) |
|---|---|
| Tumor Size | (n-%) |
| Tis | 2 (0.94%) |
| T1 | 145 (68.4%) |
| T2 | 65 (30.66%) |
| Tumor grade | |
| G1 | 51 (24%) |
| G2 | 96 (45.2%) |
| G3 | 20 (10.6%) |
| Unknown | 45 (21.2%) |
| Estrogen receptor | |
| Positive | 171 (80.6%) |
| Negative | 34 (16%) |
| Unknown | 7 (3.3%) |
| Progesterone receptor | |
| Positive | 138 (65%) |
| Negative | 59 (27.8%) |
| Unknown | 15 (7%) |
| Her2 status | |
| Positive | 42 (19.8%) |
| Negative | 108 (50.9%) |
| Unknown | 62 (29.2%) |
| Lymph-vascular space invasion (LVSI) | |
| Present | 58 (27.3%) |
| Absent | 121 (57%) |
| Unknown | 33 (15%) |
Table 2.
AJCC 7 and 8 stages.
| AJCC 7 Staging | |
| 0 | 1 (0.4%) |
| IA | 145 (68.3%) |
| IIA | 65 (30.6%) |
| Unknown | 1 (0.4%) |
| AJCC 8 Pronostic staging | |
| 0 | 2 (0.9%) |
| IA | 43 (20%) |
| IB | 44 (20.7%) |
| IIA | 18 (8.4%) |
| IIB | 2 (0.9%) |
| IIIA | 8 (3.7%) |
| Unknown | 95 (44.8%) |
2.2. Treatment
All patients were surgically managed with breast-conserving surgery (BCS). The management of axillary nodes was axillary dissection in 84.3%, sentinel lymph node 15.7% and not performed in 2 in-situ patients. A median of 14 (IQR 11-18) nodes were removed when axillary dissection was performed and a median of 3 (IQR 2-4) in sentinel lymph node cases. No patient presented metastatic lymph nodes.
Thirty-four patients received adjuvant chemotherapy, 29 (85.3%) patients received AC, 2 (5.9%) CMF, one (2.9%) FAC and two (5.9%) received AC plus Trastuzumab. Hormonotherapy was received by 164 (83.5%) patients, mainly Tamoxifen, as per local clinical guidelines. No patient received neoadjuvant treatment.
2.3. Follow-Up
With a median follow up of 60 months (CI95% 9-91%), we found 3% local recurrence, which corresponds to 5 local recurrences, all of them in the same breast quadrant as the primary lesion. 5.5% of regional and/or distance relapses was observed during this follow-up period. At five years, overall survival was 88.7% IC95% (82.3-92.9%), freedom from local recurrence 95.8% IC95% (90.2-98.2%) and disease free survival 84.3% IC95% (77.1-89.4%).
Within the five patients that relapsed locally, two had a simultaneous distance relapse, both finally died; meanwhile, the other three were still alive at the moment of this analysis. Of the 17 patients that ultimately died, two had previously a local recurrence and five had a regional or distant recurrence previous to death.
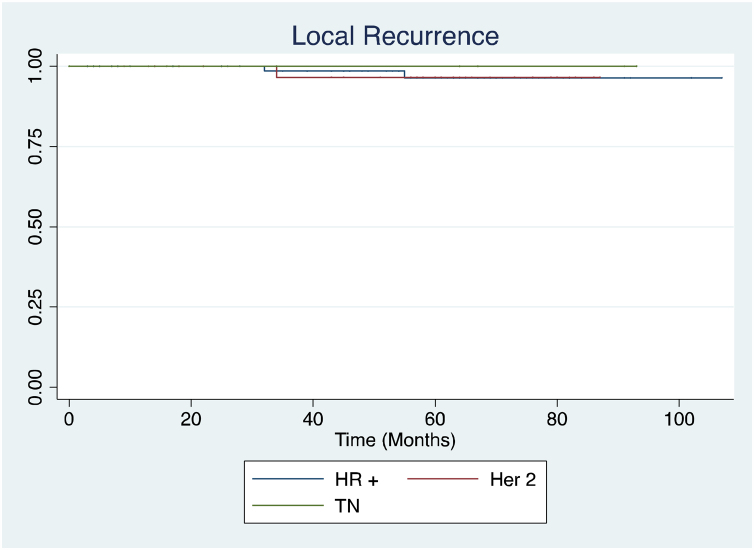
Local recurrences were also analyzed according to molecular subtypes (Fig. 1). Two occurred in hormone receptor positive patients, one in her2 and the two remaining were not classified because of missing molecular profile data.
Fig. 1.
Kaplan Meier curves for local recurrence, incidence according to molecular profile (time in moths). HR+ (Hormone receptor positive)
In an exploratory analysis for overall survival, no differences were found within molecular subtypes (p = 0.57) or tumor grade (p = 0.95).
An analyses of recurrence pattern regarding AJCC 7 and AJCC 8 staging systems were not performed on account of the very low incidence of local and regional and distant recurrences.
2.4. Discussion
Our local recurrence rate of 3%, with a median follow-up of 5 years, is close to local control rates reported in prospective randomized trials. Wheelan et al. reported a 5-year local recurrence-free survival of 97.2% in the group with the HF-WBI regimen. At 10 years, local-relapse rate for this group was 6.2% (10). When comparing 2 HF-WBI schedules studied at the Royal Marsden Hospital (RMH) and Gloucestershire Oncology Centre (GOC) in the UK(19), local-recurrence rate at 5 years was 9.1% (95% CI 6.4-11.7) in the 39 Gy in 13 fractions group, and 7.1% (95% CI 4.6-9.5) in the 42.9 Gy in 13 fractions group. Local control was significantly improved in the 42.9 Gy group. This relapse rate may seem high compared to our report, but the inclusion criteria in the RMH-GOC study allowed women with more advanced stage disease to be included. Similar inclusion criteria where considered in the UK START trials (11), although RT scheme was different and boost to the tumor bed was allowed. Reported rates of local recurrence at 5 years in UK START A were 3.2 (95% CI 1.9-4.5) in the 41.6 Gy in 13 fractions group, and 4.6% (95% CI 3.0-6.2) in the 39 Gy in 13 fractions group. The UK START B (8)(9) trial used a treatment schedule closer to the Canadian protocol (7) and ours. The rate of local recurrence at 5 years was 2.0% (95% CI 1.1-2.8) in the HF-WBI. Comparison of regional and distant control is difficult due to the difference in reporting methods and systemic management. Hormone therapy and chemotherapy were used more frequently in our report than in other node-negative population (10).
Some considerations must be made regarding our analysis. We did not assess cosmesis or quality of life in our cohort because these issues are not evaluated during follow-up visits at our institution with a properly standardized instrument. Evidence from international trials suggests that there is no difference in cosmetic outcomes with HF-WBI. The immunohistochemistry study performed in our center between 2008 and 2011 did not include evaluation of Ki 67, and patients with equivocal HER-2 were not further evaluated with FISH. This clinical information is currently considered when managing patients with breast cancer, but it is not clear if local adjuvant therapy should be tailored according to this, because the relationship between radiosensitivity and molecular subtype is not completely understood (20). In our data base, no evidence of interaction between immunohistochemical profile and local relapse was found.
3. Conclusion
Our local recurrence rate obtained using HF-WBI for early breast cancer patients is similar to those obtained in large randomized trials.
Our data supports that a hypofractionated radiation scheme can be used safely and with equivalent oncological outcomes in a Latin American Cancer center.
This information is valuable as shorter treatments reduce costs, a key issue in limited resource centers.
References
- 1.Globocan 2012. accessed March 30, 2018, http://globocan.iarc.fr/Pages/fact_sheets_cancer.aspx.
- 2.Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10 801 women in 17 randomised trials. The Lancet. 2011;378(November (9804)):1707–1716. doi: 10.1016/S0140-6736(11)61629-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suh W.W., Pierce L.J., Vicini F.A., Hayman J.A. A cost comparison analysis of partial versus whole-breast irradiation after breast-conserving surgery for early-stage breast cancer. Int J Radiat Oncol. 2005;62(July (3)):790–796. doi: 10.1016/j.ijrobp.2004.10.039. [DOI] [PubMed] [Google Scholar]
- 4.Lautner M., Lin H., Shen Y., Parker C., Kuerer H., Shaitelman S. Disparities in the Use of Breast-Conserving Therapy Among Patients With Early-Stage Breast Cancer. JAMA Surg. 2015;150(August (8)):778. doi: 10.1001/jamasurg.2015.1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yarnold J., Ashton A., Bliss J., Homewood J., Harper C., Hanson J. Fractionation sensitivity and dose response of late adverse effects in the breast after radiotherapy for early breast cancer: long-term results of a randomised trial. Radiother Oncol. 2005;75(April (1)):9–17. doi: 10.1016/j.radonc.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 6.Qi X.S., White J., Li X.A. Is α/β for breast cancer really low? Radiother Oncol. 2011;100(August (2)):282–288. doi: 10.1016/j.radonc.2011.01.010. [DOI] [PubMed] [Google Scholar]
- 7.Whelan T., MacKenzie R., Julian J., Levine M., Shelley W., Grimard L. Randomized trial of breast irradiation schedules after lumpectomy for women with lymph node-negative breast cancer. J Natl Cancer Inst. 2002;94(August (15)):1143–1150. doi: 10.1093/jnci/94.15.1143. [DOI] [PubMed] [Google Scholar]
- 8.The UK Standardisation of Breast Radiotherapy (START) Trial A of radiotherapy hypofractionation for treatment of early breast cancer: a randomised trial. Lancet Oncol. 2008;9(April (4)):331–341. doi: 10.1016/S1470-2045(08)70077-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The UK Standardisation of Breast Radiotherapy (START) Trial B of radiotherapy hypofractionation for treatment of early breast cancer: a randomised trial. The Lancet. 2008;371(March (9618)):1098–1107. doi: 10.1016/S0140-6736(08)60348-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Whelan T.J., Pignol J.-P., Levine M.N., Julian J.A., MacKenzie R., Parpia S. Long-Term Results of Hypofractionated Radiation Therapy for Breast Cancer. N Engl J Med. 2010;362(February (6)):513–520. doi: 10.1056/NEJMoa0906260. [DOI] [PubMed] [Google Scholar]
- 11.Haviland J.S., Owen J.R., Dewar J.A., Agrawal R.K., Barrett J., Barrett-Lee P.J. The UK Standardisation of Breast Radiotherapy (START) trials of radiotherapy hypofractionation for treatment of early breast cancer: 10-year follow-up results of two randomised controlled trials. Lancet Oncol. 2013;14(October (11)):1086–1094. doi: 10.1016/S1470-2045(13)70386-3. [DOI] [PubMed] [Google Scholar]
- 12.Hopwood P., Haviland J.S., Sumo G., Mills J., Bliss J.M., Yarnold J.R. Comparison of patient-reported breast, arm, and shoulder symptoms and body image after radiotherapy for early breast cancer: 5-year follow-up in the randomised Standardisation of Breast Radiotherapy (START) trials. Lancet Oncol. 2010;11(March (3)):231–240. doi: 10.1016/S1470-2045(09)70382-1. [DOI] [PubMed] [Google Scholar]
- 13.Breast Cancer Expert Panel of the German Society of Radiation Oncology (DEGRO), Sedlmayer F, Sautter-Bihl M-L, Budach W, Dunst J, Fastner G. DEGRO practical guidelines: radiotherapy of breast cancer I: Radiotherapy following breast conserving therapy for invasive breast cancer. Strahlenther Onkol. 2013;189(October (10)):825–833. doi: 10.1007/s00066-013-0437-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith B.D., Bentzen S.M., Correa C.R., Hahn C.A., Hardenbergh P.H., Ibbott G.S. Fractionation for Whole Breast Irradiation: An American Society for Radiation Oncology (ASTRO) Evidence-Based Guideline. Int J Radiat Oncol. 2011;81(September (1)):59–68. doi: 10.1016/j.ijrobp.2010.04.042. [DOI] [PubMed] [Google Scholar]
- 15.Ban KA, Godellas CV. Epidemiology of Breast Cancer. Surg Oncol Clin N Am. 2014;23(July (3)):409–422. doi: 10.1016/j.soc.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 16.Horton J.K., Jagsi R., Woodward W.A., Ho A. Breast Cancer Biology: Clinical Implications for Breast Radiation Therapy. Int J Radiat Oncol. 2018;100(January (1)):23–37. doi: 10.1016/j.ijrobp.2017.08.025. [DOI] [PubMed] [Google Scholar]
- 17.Park Y.H., Lee S.J., Cho E.Y., Choi Y.L., Lee S.J.E, Nam S.J. Clinical relevance of TNM staging system according to breast cancer subtypes. Ann Oncol. 2011;22(July (7)):1554–1560. doi: 10.1093/annonc/mdq617. [DOI] [PubMed] [Google Scholar]
- 18.Perou C.M., Sørlie T., Eisen MB, van de Rijn M, Jeffrey SS, Rees CA. Molecular portraits of human breast tumours. Nature. 2000;406(August (6797)):747–752. doi: 10.1038/35021093. [DOI] [PubMed] [Google Scholar]
- 19.Owen J.R., Ashton A., Bliss J.M., Homewood J., Harper C., Hanson J. Effect of radiotherapy fraction size on tumour control in patients with early-stage breast cancer after local tumour excision: long-term results of a randomised trial. Lancet Oncol. 2006;7(June (6)):467–471. doi: 10.1016/S1470-2045(06)70699-4. [DOI] [PubMed] [Google Scholar]
- 20.Speers C., Zhao S., Liu M., Bartelink H., Pierce L.J., Feng F.Y. Development and Validation of a Novel Radiosensitivity Signature in Human Breast Cancer. Clin Cancer Res. 2015;21(August (16)):3667–3677. doi: 10.1158/1078-0432.CCR-14-2898. [DOI] [PubMed] [Google Scholar]