Abstract
This chapter describes the general treatment and immune principles and internal management for AECHB and HBV ACLF, including ICU monitoring, general supportive medications/nutrition/nursing, immune therapy, artificial liver supportive systems, hepatocyte/stem cell, and liver transplant, management for special populations, frequently clinical complications and the utilization of Chinese traditional medicines.
Early clinical indicators of severe hepatitis B include acratia, gastrointestinal symptoms, a daily increase in serum bilirubin >1 mg/dL, toxic intestinal paralysis, bleeding tendency and mild mind anomaly or character change, and the presence of other diseases inducing severe hepatitis. Laboratory indicators include T-Bil, PTA, cholinesterase, pre-albumin and albumin. The roles of immune indicators (such as IL-6, TNF-α, and fgl2), gene polymorphisms, HBV genotypes, and gene mutations as early clinical indicators.
Intensive Care Unit monitor patients with severe hepatitis include intracranial pressure, infection, blood dynamics, respiratory function, renal function, blood coagulation function, nutritional status and blood purification process. Nursing care should not only include routine care, but psychological and special care (complications).
Nutrition support and nursing care should be maintained throughout treatment for severe hepatitis. Common methods of evaluating nutritional status include direct human body measurement, creatinine height index (CHI) and subject global assessment of nutrition (SGA). Malnourished patients should receive enteral or parenteral nutrition support.
Immune therapies for severe hepatitis include promoting hepatocyte regeneration (e.g. with glucagon, hepatocyte growth factor and prostaglandin E1), glucocorticoid suppressive therapy, and targeting molecular blocking. Corticosteroid treatment should be early and sufficient, and adverse drug reactions monitored. Treatments currently being investigated are those targeting Toll-like receptors, NK cell/NK cell receptors, macrophage/immune coagulation system, CTLA-4/PD-1 and stem cell transplantation.
In addition to conventional drugs and radioiodine, corticosteroids and artificial liver treatment can also be considered for severe hepatitis patients with hyperthyreosis. Patients with gestational severe hepatitis require preventive therapy for fetal growth restriction, and it is necessary to choose the timing and method of fetal delivery. For patients with both diabetes and severe hepatitis, insulin is preferred to oral antidiabetic agents to control blood glucose concentration. Liver toxicity of corticosteroids and immune suppressors should be monitored during treatment for severe hepatitis in patients with connective tissue diseases including SLE, RA and sicca syndrome. Patient with connective tissue diseases should preferably be started after the antiviral treatment with nucleos(t)ide analogues.
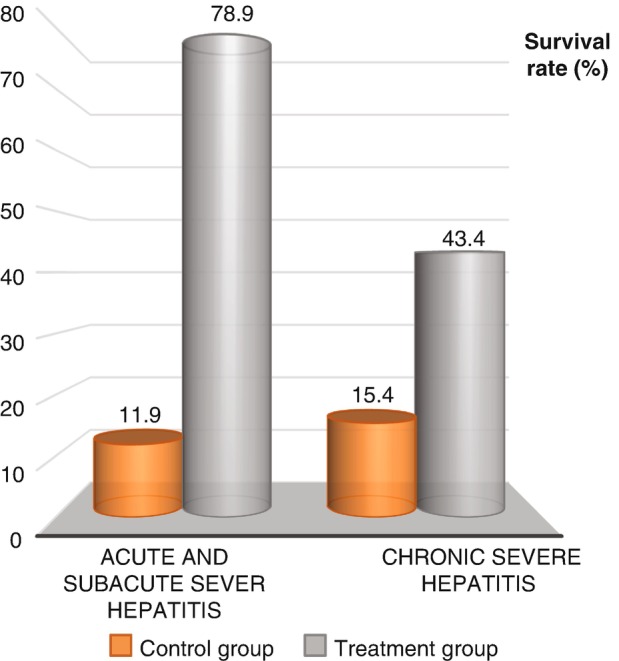
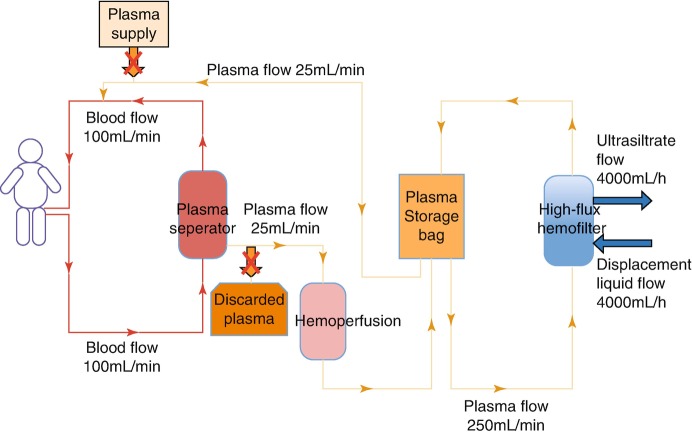
An artificial liver can improve patients’ liver function; remove endotoxins, blood ammonia and other toxins; correct amino acid metabolism and coagulation disorders; and reverse internal environment imbalances. Non-bioartificial livers are suitable for patients with early and middle stage severe hepatitis; for late-stage patients waiting for liver transplantation; and for transplanted patients with rejection reaction or transplant failure. The type of artificial liver should be determined by each patient’s condition and previous treatment purpose, and patients should be closely monitored for adverse reactions and complications. Bio- and hybrid artificial livers are still under development.
MELD score is the international standard for choosing liver transplantation. Surgical methods mainly include the in situ classic type and the piggyback type; transplantation includes no liver prophase, no liver phase or new liver phase. Preoperative preparation, management of intraoperative and postoperative complications and postoperative long-term treatment are keys to success.
Severe hepatitis belongs to the categories of “acute jaundice”, “scourge jaundice”, and “hot liver” in traditional Chinese medicine. Treatment methods include Chinese traditional medicines, acupuncture and acupoint injection, external application of drugs, umbilical compress therapy, drip, blow nose therapy, earpins, and clysis. Dietary care is also an important part of traditional Chinese medicine treatment.
Contributor Information
Qin Ning, Email: qning@vip.sina.com.
Han Bai, Email: baih@sj-hospital.org.
Xi-Ping Zhao, Email: xpzhao@tjh.tjmu.edu.cn.
Lan-Juan Li, Email: ljli@zju.edu.cn.
Zhi-Shui Chen, Email: zschen@tjh.tjmu.edu.cn.
References
- 1.Huifen W, Haibin S. Intensive care management of liver failure. Infect Dis Inform. 2009;22(5):273–275. [Google Scholar]
- 2.Chunrong H, Ruide L. Intensive care of liver failure. New Chinese Med. 2006;37(10):685–686. [Google Scholar]
- 3.Dawei L. Practice of critical care medicine. 1. Shanghai: People’s Medical Publishing House; 2010. [Google Scholar]
- 4.Liver Failure, Artificial Liver Group CSoID, Association CM, Severe Liver Diseases and Artificial Liver Group CSoH, et al. Diagnostic and treatment guidelines for liver failure. Chin J Hepatol. 2006;14(9):643–6. [PubMed]
- 5.Stravitz RT, Kramer AH, Davern T, et al. Intensive care of patients with acute liver failure: recommendations of the U.S. Acute Liver Failure Study Group. Crit Care Med. 2007;35(11):2498–2508. doi: 10.1097/01.CCM.0000287592.94554.5F. [DOI] [PubMed] [Google Scholar]
- 6.Findlay JY, Fix OK, Paugam-Burtz C, et al. Critical care of the end-stage liver disease patient awaiting liver transplantation. Liver Transpl. 2011;17(5):496–510. doi: 10.1002/lt.22269. [DOI] [PubMed] [Google Scholar]
- 7.Stravitz RT. Critical management decisions in patients with acute liver failure. Chest. 2008;134(5):1092–1102. doi: 10.1378/chest.08-1071. [DOI] [PubMed] [Google Scholar]
- 8.Bernal W, Jalan R, Quaglia A, et al. Acute-on-chronic liver failure. Lancet. 2015;386(10003):1576–1587. doi: 10.1016/S0140-6736(15)00309-8. [DOI] [PubMed] [Google Scholar]
- 9.Strauss G, Hansen BA, Kirkegaard P, et al. Liver function, cerebral blood flow autoregulation, and hepatic encephalopathy in fulminant hepatic failure. Hepatology. 1997;25(4):837–839. doi: 10.1002/hep.510250409. [DOI] [PubMed] [Google Scholar]
- 10.Larsen FS, Wendon J. Brain edema in liver failure: basic physiologic principles and management. Liver Transpl. 2002;8(11):983–989. doi: 10.1053/jlts.2002.35779. [DOI] [PubMed] [Google Scholar]
- 11.Plauth M, Cabré E, Campillo B, et al. ESPEN guidelines on parenteral nutrition: hepatology. Clin Nutr. 2009;28(4):436–444. doi: 10.1016/j.clnu.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 12.Kondrup J, Rasmussen HH, Hamberg O, et al. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22(3):321–336. doi: 10.1016/s0261-5614(02)00214-5. [DOI] [PubMed] [Google Scholar]
- 13.Canabal JM, Kramer DJ. Management of sepsis in patients with liver failure. Curr Opin Crit Care. 2008;14(2):189–197. doi: 10.1097/MCC.0b013e3282f6a435. [DOI] [PubMed] [Google Scholar]
- 14.Bémeur C, Desjardins P, Butterworth RF. Role of nutrition in the management of hepatic encephalopathy in end-stage liver failure. J Nutr Metab. 2010;2010:489823. doi: 10.1155/2010/489823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ellis A, Wendon J. Circulatory, respiratory, cerebral, and renal derangements in acute liver failure: pathophysiology and management. Semin Liver Dis. 1996;16(4):379–388. doi: 10.1055/s-2007-1007251. [DOI] [PubMed] [Google Scholar]
- 16.Shawcross DL, Davies NA, Mookerjee RP, et al. Worsening of cerebral hyperemia by the administration of terlipressin in acute liver failure with severe encephalopathy. Hepatology. 2004;39(2):471–475. doi: 10.1002/hep.20044. [DOI] [PubMed] [Google Scholar]
- 17.Wright G, Sharifi Y, Jover-Cobos M, et al. The brain in acute on chronic liver failure. Metab Brain Dis. 2014;29(4):965–973. doi: 10.1007/s11011-014-9553-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rolando N, Philpott-Howard J, Williams R. Bacterial and fungal infection in acute liver failure. Semin Liver Dis. 1996;16(4):389–402. doi: 10.1055/s-2007-1007252. [DOI] [PubMed] [Google Scholar]
- 19.Rolando N, Wade J, Davalos M, et al. The systemic inflammatory response syndrome in acute liver failure. Hepatology. 2000;32(4 Pt 1):734–739. doi: 10.1053/jhep.2000.17687. [DOI] [PubMed] [Google Scholar]
- 20.Dellinger RP, Levy MM, Carlet JM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2008. Intensive Care Med. 2008;34(1):17–60. doi: 10.1007/s00134-007-0934-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clemmesen JO, Galatius S, Skak C, et al. The effect of increasing blood pressure with dopamine on systemic, splanchnic, and lower extremity hemodynamics in patients with acute liver failure. Scand J Gastroenterol. 1999;34(9):921–927. doi: 10.1080/003655299750025417. [DOI] [PubMed] [Google Scholar]
- 22.MacGilchrist AJ, Sumner D, Reid JL. Impaired pressor reactivity in cirrhosis: evidence for a peripheral vascular defect. Hepatology. 1991;13(4):689–694. [PubMed] [Google Scholar]
- 23.Annane D. Glucocorticoids in the treatment of severe sepsis and septic shock. Curr Opin Crit Care. 2005;11(5):449–453. doi: 10.1097/01.ccx.0000176691.95562.43. [DOI] [PubMed] [Google Scholar]
- 24.Harry R, Auzinger G, Wendon J. The clinical importance of adrenal insufficiency in acute hepatic dysfunction. Hepatology. 2002;36(2):395–402. doi: 10.1053/jhep.2002.34514. [DOI] [PubMed] [Google Scholar]
- 25.McDowell TD, Stevens RD, Gurakar A. Acute liver failure: a management challenge for the practicing gastroenterologist. Gastroenterol Hepatol (N Y) 2010;6(7):444–450. [PMC free article] [PubMed] [Google Scholar]
- 26.Patton H, Misel M, Gish RG. Acute liver failure in adults: an evidence-based management protocol for clinicians. Gastroenterol Hepatol (N Y) 2012;8(3):161–212. [PMC free article] [PubMed] [Google Scholar]
- 27.Sarin SK, Kedarisetty CK, Abbas Z, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific Association for the Study of the Liver (APASL) 2014. Hepatol Int. 2014;8(4):453–471. doi: 10.1007/s12072-014-9580-2. [DOI] [PubMed] [Google Scholar]
- 28.Lee WM, Squires RH, Nyberg SL, et al. Acute liver failure: summary of a workshop. Hepatology. 2008;47(4):1401–1415. doi: 10.1002/hep.22177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Villanueva C. Gastrointestinal bleeding: blood transfusion for acute upper gastrointestinal bleeding. Nat Rev Gastroenterol Hepatol. 2015;12(8):432–434. doi: 10.1038/nrgastro.2015.116. [DOI] [PubMed] [Google Scholar]
- 30.Zamora NLE, Aguirre VJ, Chávez-Tapia NC, et al. Acute-on-chronic liver failure: a review. Ther Clin Risk Manag. 2014;10:295–303. doi: 10.2147/TCRM.S59723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bémeur C, Butterworth RF. Reprint of: nutrition in the management of cirrhosis and its neurological complications. J Clin Exp Hepatol. 2015;5(Suppl 1):S131–S140. doi: 10.1016/j.jceh.2015.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sawhney R, Jalan R. Liver: the gut is a key target of therapy in hepatic encephalopathy. Nat Rev Gastroenterol Hepatol. 2015;12(1):7–8. doi: 10.1038/nrgastro.2014.185. [DOI] [PubMed] [Google Scholar]
- 33.Kim TY, Kim DJ. Acute-on-chronic liver failure. Clin Mol Hepatol. 2013;19(4):349–359. doi: 10.3350/cmh.2013.19.4.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Asrani SK, Kim WR. Model for end-stage liver disease: end of the first decade. Clin Liver Dis. 2011;15(4):685–698. doi: 10.1016/j.cld.2011.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Starr S, Hand H. Nursing care of chronic and acute liver failure. Nurs Stand. 2002;16(40):47–54. doi: 10.7748/ns2002.06.16.40.47.c3218. [DOI] [PubMed] [Google Scholar]
- 36.Mitchell MC, Friedman LS, McClain CJ. Medical management of severe alcoholic hepatitis: expert review from the Clinical Practice Updates Committee of the AGA Institute. Clin Gastroenterol Hepatol. 2017;15(1):5–12. doi: 10.1016/j.cgh.2016.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fung J, Lai CL, Yuen MF. Management of chronic hepatitis B in severe liver disease. World J Gastroenterol. 2014;20:16053–16061. doi: 10.3748/wjg.v20.i43.16053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wieser V, Tilg H. Management of severe alcoholic hepatitis. Wien Med Wochenschr. 2014;164:3–8. doi: 10.1007/s10354-013-0221-5. [DOI] [PubMed] [Google Scholar]
- 39.Liver F, Artificial Liver Group CSoIDCMA, Severe Liver D, Artificial Liver Group CSoHCMA Diagnostic and treatment guidelines for liver failure (2012 version) Zhonghua Gan Zang Bing Za Zhi. 2013;21:177–183. [PubMed] [Google Scholar]
- 40.Mathurin P, Moreno C, Samuel D, Dumortier J, Salleron J, Durand F, Castel H, et al. Early liver transplantation for severe alcoholic hepatitis. N Engl J Med. 2011;365:1790–1800. doi: 10.1056/NEJMoa1105703. [DOI] [PubMed] [Google Scholar]
- 41.Aberg F, Nordin A, Makisalo H, Isoniemi H. Who is too healthy and who is too sick for liver transplantation: external validation of prognostic scores and survival-benefit estimation. Scand J Gastroenterol. 2015;50:1144–1151. doi: 10.3109/00365521.2015.1028992. [DOI] [PubMed] [Google Scholar]
- 42.Oka H, Fujiwara K, Okita K, Ishii H, Sakuma A. A multi-centre double-blind controlled trial of glucagon and insulin therapy for severe acute hepatitis. Gastroenterol Jpn. 1989;24:332–336. doi: 10.1007/BF02774333. [DOI] [PubMed] [Google Scholar]
- 43.Trinchet JC, Balkau B, Poupon RE, et al. Treatment of severe alcoholic hepatitis by infusion of insulin and glucagon: a multicenter sequential trial. Hepatology. 1992;15(1):76–81. doi: 10.1002/hep.1840150115. [DOI] [PubMed] [Google Scholar]
- 44.Gohda E, Tsubouchi H, Nakayama H, Hirono S, Takahashi K, Koura M, Hashimoto S, et al. Human hepatocyte growth factor in plasma from patients with fulminant hepatic failure. Exp Cell Res. 1986;166:139–150. doi: 10.1016/0014-4827(86)90514-8. [DOI] [PubMed] [Google Scholar]
- 45.Suarez-Causado A, Caballero-Diaz D, Bertran E, Roncero C, Addante A, Garcia-Alvaro M, Fernandez M, et al. HGF/c-Met signaling promotes liver progenitor cell migration and invasion by an epithelial-mesenchymal transition-independent, phosphatidyl inositol-3 kinase-dependent pathway in an in vitro model. Biochim Biophys Acta. 1853;2015:2453–2463. doi: 10.1016/j.bbamcr.2015.05.017. [DOI] [PubMed] [Google Scholar]
- 46.Moumen A, Ieraci A, Patane S, Sole C, Comella JX, Dono R, Maina F. Met signals hepatocyte survival by preventing Fas-triggered FLIP degradation in a PI3k-Akt-dependent manner. Hepatology. 2007;45:1210–1217. doi: 10.1002/hep.21604. [DOI] [PubMed] [Google Scholar]
- 47.Kosai K, Matsumoto K, Nagata S, Tsujimoto Y, Nakamura T. Abrogation of Fas-induced fulminant hepatic failure in mice by hepatocyte growth factor. Biochem Biophys Res Commun. 1998;244:683–690. doi: 10.1006/bbrc.1998.8293. [DOI] [PubMed] [Google Scholar]
- 48.Aguilar-Valenzuela R, Carlsen ED, Liang Y, Soong L, Sun J. Hepatocyte growth factor in dampening liver immune-mediated pathology in acute viral hepatitis without compromising antiviral activity. J Gastroenterol Hepatol. 2014;29:878–886. doi: 10.1111/jgh.12456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Thatch KA, Katz MS, Haber MM, Schwartz MZ. Growth factor modulation of hepatic inflammation: a novel approach to the management of total parenteral nutrition-associated liver disease. J Pediatr Surg. 2010;45:89–94. doi: 10.1016/j.jpedsurg.2009.10.016. [DOI] [PubMed] [Google Scholar]
- 50.Ido A, Moriuchi A, Numata M, Murayama T, Teramukai S, Marusawa H, Yamaji N, et al. Safety and pharmacokinetics of recombinant human hepatocyte growth factor (rh-HGF) in patients with fulminant hepatitis: a phase I/II clinical trial, following preclinical studies to ensure safety. J Transl Med. 2011;9:55. doi: 10.1186/1479-5876-9-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ido A, Moriuchi A, Marusawa H, Ikeda K, Numata M, Yamaji N, Setoyama H, et al. Translational research on HGF: a phase I/II study of recombinant human HGF for the treatment of fulminant hepatic failure. Hepatol Res. 2008;38(Suppl 1):S88–S92. doi: 10.1111/j.1872-034X.2008.00432.x. [DOI] [PubMed] [Google Scholar]
- 52.Nakanishi C, Moriuchi A, Ido A, Numata M, Kim ID, Kusumoto K, Hasuike S, et al. Effect of hepatocyte growth factor on endogenous hepatocarcinogenesis in rats fed a choline-deficient L-amino acid-defined diet. Oncol Rep. 2006;16:25–31. [PubMed] [Google Scholar]
- 53.Togo S, Chen H, Takahashi T, Kubota T, Matsuo K, Morioka D, Watanabe K, et al. Prostaglandin E1 improves survival rate after 95% hepatectomy in rats. J Surg Res. 2008;146:66–72. doi: 10.1016/j.jss.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 54.Ikegami T, Matsuzaki Y, Kurusu J, Yoshiga S, Saito Y, Chiba T, Abei M, et al. Randomized control trial of lipo-prostaglandin E1 in patients with acute liver injury induced by lipiodol-targeted chemotherapy. Clin Pharmacol Ther. 1995;57:582–589. doi: 10.1016/0009-9236(95)90043-8. [DOI] [PubMed] [Google Scholar]
- 55.Jia C, Dai C, Bu X, Peng S, Xu F, Xu Y, Zhao Y. Co-administration of prostaglandin E1 with somatostatin attenuates acute liver damage after massive hepatectomy in rats via inhibition of inflammatory responses, apoptosis and endoplasmic reticulum stress. Int J Mol Med. 2013;31:416–422. doi: 10.3892/ijmm.2012.1213. [DOI] [PubMed] [Google Scholar]
- 56.LaBrecque DR, Pesch LA. Preparation and partial characterization of hepatic regenerative stimulator substance (SS) from rat liver. J Physiol. 1975;248:273–284. doi: 10.1113/jphysiol.1975.sp010973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fan QL, Huang CG, Jin Y, Feng B, Miao HN, Li WJ, Jiao BH, et al. Effects of shark hepatic stimulator substance on the function and antioxidant capacity of liver mitochondria in an animal model of acute liver injury. Acta Biochim Biophys Sin Shanghai. 2005;37:507–514. doi: 10.1111/j.1745-7270.2005.00081.x. [DOI] [PubMed] [Google Scholar]
- 58.Li F, Sun JY, Liu M, Lu WY, Wang JY, Shi JY. Sterically stable liposomes improve the therapeutic effect of hepatic stimulator substance on fulminant hepatic failure in rats. Biochem Pharmacol. 2011;82:556–565. doi: 10.1016/j.bcp.2011.05.025. [DOI] [PubMed] [Google Scholar]
- 59.Li S, Tang Z, Yu H, Li W, Jiang Y, Wang Y, An W. Administration of naked plasmid encoding hepatic stimulator substance by hydrodynamic tail vein injection protects mice from hepatic failure by suppressing the mitochondrial permeability transition. J Pharmacol Exp Ther. 2011;338:750–757. doi: 10.1124/jpet.111.181305. [DOI] [PubMed] [Google Scholar]
- 60.Theocharis SE, Papadimitriou LJ, Retsou ZP, Margeli AP, Ninos SS, Papadimitriou JD. Granulocyte-colony stimulating factor administration ameliorates liver regeneration in animal model of fulminant hepatic failure and encephalopathy. Dig Dis Sci. 2003;48:1797–1803. doi: 10.1023/a:1025463532521. [DOI] [PubMed] [Google Scholar]
- 61.Garg V, Garg H, Khan A, Trehanpati N, Kumar A, Sharma BC, Sakhuja P, et al. Granulocyte colony-stimulating factor mobilizes CD34(+) cells and improves survival of patients with acute-on-chronic liver failure. Gastroenterology. 2012;142:505–512.e501. doi: 10.1053/j.gastro.2011.11.027. [DOI] [PubMed] [Google Scholar]
- 62.Duan XZ, Liu FF, Tong JJ, Yang HZ, Chen J, Liu XY, Mao YL, et al. Granulocyte-colony stimulating factor therapy improves survival in patients with hepatitis B virus-associated acute-on-chronic liver failure. World J Gastroenterol. 2013;19:1104–1110. doi: 10.3748/wjg.v19.i7.1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Huebert RC, Rakela J. Cellular therapy for liver disease. Mayo Clin Proc. 2014;89:414–424. doi: 10.1016/j.mayocp.2013.10.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Glanemann M, Shi B, El-Zidy N, Gaebelein G, Kronbach Z, Neuhaus P, Nussler AK. Subcutaneous administration of epidermal growth factor: a true treatment option in case of postoperative liver failure? Int J Surg. 2009;7:200–205. doi: 10.1016/j.ijsu.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 65.Khai NC, Takahashi T, Ushikoshi H, Nagano S, Yuge K, Esaki M, Kawai T, et al. In vivo hepatic HB-EGF gene transduction inhibits Fas-induced liver injury and induces liver regeneration in mice: a comparative study to HGF. J Hepatol. 2006;44:1046–1054. doi: 10.1016/j.jhep.2005.10.027. [DOI] [PubMed] [Google Scholar]
- 66.Ciardiello F, Tortora G. EGFR antagonists in cancer treatment. N Engl J Med. 2008;358:1160–1174. doi: 10.1056/NEJMra0707704. [DOI] [PubMed] [Google Scholar]
- 67.Li CY, Cao CZ, Xu WX, Cao MM, Yang F, Dong L, Yu M, et al. Recombinant human hepassocin stimulates proliferation of hepatocytes in vivo and improves survival in rats with fulminant hepatic failure. Gut. 2010;59:817–826. doi: 10.1136/gut.2008.171124. [DOI] [PubMed] [Google Scholar]
- 68.Assy N, Spira G, Paizi M, Shenkar L, Kraizer Y, Cohen T, Neufeld G, et al. Effect of vascular endothelial growth factor on hepatic regenerative activity following partial hepatectomy in rats. J Hepatol. 1999;30:911–915. doi: 10.1016/s0168-8278(99)80147-0. [DOI] [PubMed] [Google Scholar]
- 69.Antoine M, Tag CG, Wirz W, Borkham-Kamphorst E, Sawitza I, Gressner AM, Kiefer P. Upregulation of pleiotrophin expression in rat hepatic stellate cells by PDGF and hypoxia: implications for its role in experimental biliary liver fibrogenesis. Biochem Biophys Res Commun. 2005;337:1153–1164. doi: 10.1016/j.bbrc.2005.09.173. [DOI] [PubMed] [Google Scholar]
- 70.Wu JY, Li M, Zhang H. Effect of glucocorticoid treatment on the clinical outcome of patients with early-stage liver failure. Nan Fang Yi Ke Da Xue Xue Bao. 2011;31:554–556. [PubMed] [Google Scholar]
- 71.Mathurin P, O’Grady J, Carithers RL, Phillips M, Louvet A, Mendenhall CL, Ramond MJ, et al. Corticosteroids improve short-term survival in patients with severe alcoholic hepatitis: meta-analysis of individual patient data. Gut. 2011;60:255–260. doi: 10.1136/gut.2010.224097. [DOI] [PubMed] [Google Scholar]
- 72.Wasmuth HE, Kunz D, Yagmur E, Timmer-Stranghoner A, Vidacek D, Siewert E, Bach J, et al. Patients with acute on chronic liver failure display “sepsis-like” immune paralysis. J Hepatol. 2005;42:195–201. doi: 10.1016/j.jhep.2004.10.019. [DOI] [PubMed] [Google Scholar]
- 73.Denson JL, Maller A, Beckwith CA, Schwartz DR. A 25-year-old man with fulminant hepatic failure after treatment with corticosteroids. Chest. 2013;144:1717–1719. doi: 10.1378/chest.13-1056. [DOI] [PubMed] [Google Scholar]
- 74.Dyson JK, Hudson M, McPherson S. Lesson of the month 2: severe reactivation of hepatitis B after immunosuppressive chemotherapy. Clin Med. 2014;14:551–555. doi: 10.7861/clinmedicine.14-5-551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Di Bisceglie Adrian M., Lok Anna S., Martin Paul, Terrault Norah, Perrillo Robert P., Hoofnagle Jay H. Recent US Food and Drug Administration warnings on hepatitis B reactivation with immune-suppressing and anticancer drugs: Just the tip of the iceberg? Hepatology. 2015;61(2):703–711. doi: 10.1002/hep.27609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fujiwara K, Yokosuka O, Kojima H, Kanda T, Saisho H, Hirasawa H, Suzuki H. Importance of adequate immunosuppressive therapy for the recovery of patients with "life-threatening" severe exacerbation of chronic hepatitis B. World J Gastroenterol. 2005;11:1109–1114. doi: 10.3748/wjg.v11.i8.1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Camerini R, Garaci E. Historical review of thymosin alpha 1 in infectious diseases. Expert Opin Biol Ther. 2015;15(Suppl 1):S117–S127. doi: 10.1517/14712598.2015.1033393. [DOI] [PubMed] [Google Scholar]
- 78.Romani L, Bistoni F, Perruccio K, Montagnoli C, Gaziano R, Bozza S, Bonifazi P, et al. Thymosin alpha1 activates dendritic cell tryptophan catabolism and establishes a regulatory environment for balance of inflammation and tolerance. Blood. 2006;108:2265–2274. doi: 10.1182/blood-2006-02-004762. [DOI] [PubMed] [Google Scholar]
- 79.Giacomini E, Severa M, Cruciani M, Etna MP, Rizzo F, Pardini M, Scagnolari C, et al. Dual effect of Thymosin alpha 1 on human monocyte-derived dendritic cell in vitro stimulated with viral and bacterial toll-like receptor agonists. Expert Opin Biol Ther. 2015;15(Suppl 1):S59–S70. doi: 10.1517/14712598.2015.1019460. [DOI] [PubMed] [Google Scholar]
- 80.Yang X, Qian F, He HY, Liu KJ, Lan YZ, Ni B, Tian Y, et al. Effect of thymosin alpha-1 on subpopulations of Th1, Th2, Th17, and regulatory T cells (Tregs) in vitro. Braz J Med Biol Res. 2012;45:25–32. doi: 10.1590/S0100-879X2011007500159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zhang YY, Chen EQ, Yang J, Duan YR, Tang H. Treatment with lamivudine versus lamivudine and thymosin alpha-1 for e antigen-positive chronic hepatitis B patients: a meta-analysis. Virol J. 2009;6:63. doi: 10.1186/1743-422X-6-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Liaw YF, Kao JH, Piratvisuth T, Chan HL, Chien RN, Liu CJ, Gane E, et al. Asian-Pacific consensus statement on the management of chronic hepatitis B: a 2012 update. Hepatol Int. 2012;6:531–561. doi: 10.1007/s12072-012-9365-4. [DOI] [PubMed] [Google Scholar]
- 83.Kim BH, Lee YJ, Kim W, Yoon JH, Jung EU, Park SJ, Kim YJ, et al. Efficacy of thymosin alpha-1 plus peginterferon alpha-2a combination therapy compared with peginterferon alpha-2a monotherapy in HBeAg-positive chronic hepatitis B: a prospective, multicenter, randomized, open-label study. Scand J Gastroenterol. 2012;47:1048–1055. doi: 10.3109/00365521.2012.694902. [DOI] [PubMed] [Google Scholar]
- 84.Antoniades CG, Berry PA, Wendon JA, Vergani D. The importance of immune dysfunction in determining outcome in acute liver failure. J Hepatol. 2008;49:845–861. doi: 10.1016/j.jhep.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 85.Tan YC, Xie F, Zhang HL, Zhu YL, Chen K, Tan HM, Hu BS, et al. Hydrogen-rich saline attenuates postoperative liver failure after major hepatectomy in rats. Clin Res Hepatol Gastroenterol. 2014;38:337–345. doi: 10.1016/j.clinre.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 86.Rutherford AE, Hynan LS, Borges CB, Forcione DG, Blackard JT, Lin W, Gorman AR, et al. Serum apoptosis markers in acute liver failure: a pilot study. Clin Gastroenterol Hepatol. 2007;5:1477–1483. doi: 10.1016/j.cgh.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 87.Gabay C, Emery P, van Vollenhoven R, Dikranian A, Alten R, Pavelka K, Klearman M, et al. Tocilizumab monotherapy versus adalimumab monotherapy for treatment of rheumatoid arthritis (ADACTA): a randomised, double-blind, controlled phase 4 trial. Lancet. 2013;381:1541–1550. doi: 10.1016/S0140-6736(13)60250-0. [DOI] [PubMed] [Google Scholar]
- 88.Panaccione R, Ghosh S, Middleton S, Marquez JR, Scott BB, Flint L, van Hoogstraten HJ, et al. Combination therapy with infliximab and azathioprine is superior to monotherapy with either agent in ulcerative colitis. Gastroenterology. 2014;146:392–400.e393. doi: 10.1053/j.gastro.2013.10.052. [DOI] [PubMed] [Google Scholar]
- 89.Ungar B, Chowers Y, Yavzori M, Picard O, Fudim E, Har-Noy O, Kopylov U, et al. The temporal evolution of antidrug antibodies in patients with inflammatory bowel disease treated with infliximab. Gut. 2014;63:1258–1264. doi: 10.1136/gutjnl-2013-305259. [DOI] [PubMed] [Google Scholar]
- 90.Sharma P, Kumar A, Sharma BC, Sarin SK. Infliximab monotherapy for severe alcoholic hepatitis and predictors of survival: an open label trial. J Hepatol. 2009;50:584–591. doi: 10.1016/j.jhep.2008.10.024. [DOI] [PubMed] [Google Scholar]
- 91.Boetticher NC, Peine CJ, Kwo P, Abrams GA, Patel T, Aqel B, Boardman L, et al. A randomized, double-blinded, placebo-controlled multicenter trial of etanercept in the treatment of alcoholic hepatitis. Gastroenterology. 2008;135:1953–1960. doi: 10.1053/j.gastro.2008.08.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Malik R, Mookerjee RP, Jalan R. Infection and inflammation in liver failure: two sides of the same coin. J Hepatol. 2009;51:426–429. doi: 10.1016/j.jhep.2009.06.013. [DOI] [PubMed] [Google Scholar]
- 93.Bojalil R, Mata-Gonzalez MT, Sanchez-Munoz F, Yee Y, Argueta I, Bolanos L, Amezcua-Guerra LM, et al. Anti-tumor necrosis factor VNAR single domains reduce lethality and regulate underlying inflammatory response in a murine model of endotoxic shock. BMC Immunol. 2013;14:17. doi: 10.1186/1471-2172-14-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Xu Y, Wang H, Bao S, Tabassam F, Cai W, Xiang X, Zhao G, et al. Amelioration of liver injury by continuously targeted intervention against TNFRp55 in rats with acute-on-chronic liver failure. PLoS One. 2013;8:e68757. doi: 10.1371/journal.pone.0068757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Szabo G, Csak T. Inflammasomes in liver diseases. J Hepatol. 2012;57:642–654. doi: 10.1016/j.jhep.2012.03.035. [DOI] [PubMed] [Google Scholar]
- 96.Butterworth RF. The liver-brain axis in liver failure: neuroinflammation and encephalopathy. Nat Rev Gastroenterol Hepatol. 2013;10:522–528. doi: 10.1038/nrgastro.2013.99. [DOI] [PubMed] [Google Scholar]
- 97.Sgroi A, Gonelle-Gispert C, Morel P, Baertschiger RM, Niclauss N, Mentha G, Majno P, et al. Interleukin-1 receptor antagonist modulates the early phase of liver regeneration after partial hepatectomy in mice. PLoS One. 2011;6:e25442. doi: 10.1371/journal.pone.0025442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Hu J, Yan D, Gao J, Xu C, Yuan Y, Zhu R, Xiang D, et al. rhIL-1Ra reduces hepatocellular apoptosis in mice with acetaminophen-induced acute liver failure. Lab Investig. 2010;90:1737–1746. doi: 10.1038/labinvest.2010.127. [DOI] [PubMed] [Google Scholar]
- 99.Zheng YB, Zhang XH, Huang ZL, Lin CS, Lai J, Gu YR, Lin BL, et al. Amniotic-fluid-derived mesenchymal stem cells overexpressing interleukin-1 receptor antagonist improve fulminant hepatic failure. PLoS One. 2012;7:e41392. doi: 10.1371/journal.pone.0041392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Nam JL, Ramiro S, Gaujoux-Viala C, Takase K, Leon-Garcia M, Emery P, Gossec L, et al. Efficacy of biological disease-modifying antirheumatic drugs: a systematic literature review informing the 2013 update of the EULAR recommendations for the management of rheumatoid arthritis. Ann Rheum Dis. 2014;73:516–528. doi: 10.1136/annrheumdis-2013-204577. [DOI] [PubMed] [Google Scholar]
- 101.Aly L, Iking-Konert C, Quaas A, Benten D. Subacute liver failure following anakinra treatment for adult-onset still disease. J Rheumatol. 2013;40:1775–1777. doi: 10.3899/jrheum.121309. [DOI] [PubMed] [Google Scholar]
- 102.Ishibe T, Kimura A, Ishida Y, Takayasu T, Hayashi T, Tsuneyama K, Matsushima K, et al. Reduced acetaminophen-induced liver injury in mice by genetic disruption of IL-1 receptor antagonist. Lab Investig. 2009;89:68–79. doi: 10.1038/labinvest.2008.110. [DOI] [PubMed] [Google Scholar]
- 103.Jin X, Zimmers TA, Perez EA, Pierce RH, Zhang Z, Koniaris LG. Paradoxical effects of short- and long-term interleukin-6 exposure on liver injury and repair. Hepatology. 2006;43:474–484. doi: 10.1002/hep.21087. [DOI] [PubMed] [Google Scholar]
- 104.Zhang Y, Zhang J, Korff S, Ayoob F, Vodovotz Y, Billiar TR. Delayed neutralization of interleukin 6 reduces organ injury, selectively suppresses inflammatory mediator, and partially normalizes immune dysfunction following trauma and hemorrhagic shock. Shock. 2014;42:218–227. doi: 10.1097/SHK.0000000000000211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Alfreijat M, Habibi M, Bhatia P, Bhatia A. Severe hepatitis associated with tocilizumab in a patient with rheumatoid arthritis. Rheumatology (Oxford) 2013;52:1340–1341. doi: 10.1093/rheumatology/kes397. [DOI] [PubMed] [Google Scholar]
- 106.Kawai T, Akira S. The roles of TLRs, RLRs and NLRs in pathogen recognition. Int Immunol. 2009;21:317–337. doi: 10.1093/intimm/dxp017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Szabo G, Billiar TR, Machida K, Crispe IN, Seki E. Toll-like receptor signaling in liver diseases. Gastroenterol Res Pract. 2010;2010:971270. doi: 10.1155/2010/971270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kitazawa T, Tsujimoto T, Kawaratani H, Fukui H. Therapeutic approach to regulate innate immune response by Toll-like receptor 4 antagonist E5564 in rats with D-galactosamine-induced acute severe liver injury. J Gastroenterol Hepatol. 2009;24:1089–1094. doi: 10.1111/j.1440-1746.2008.05770.x. [DOI] [PubMed] [Google Scholar]
- 109.Jiang W, Sun R, Zhou R, Wei H, Tian Z. TLR-9 activation aggravates concanavalin A-induced hepatitis via promoting accumulation and activation of liver CD4+ NKT cells. J Immunol. 2009;182:3768–3774. doi: 10.4049/jimmunol.0800973. [DOI] [PubMed] [Google Scholar]
- 110.Bamboat ZM, Ocuin LM, Balachandran VP, Obaid H, Plitas G, DeMatteo RP. Conventional DCs reduce liver ischemia/reperfusion injury in mice via IL-10 secretion. J Clin Invest. 2010;120:559–569. doi: 10.1172/JCI40008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Cao QY, Chen F, Li J, Wu SS, Wang J, Chen Z. A microarray analysis of early activated pathways in concanavalin A-induced hepatitis. J Zhejiang Univ Sci B. 2010;11:366–377. doi: 10.1631/jzus.B1000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Masson MJ, Carpenter LD, Graf ML, Pohl LR. Pathogenic role of natural killer T and natural killer cells in acetaminophen-induced liver injury in mice is dependent on the presence of dimethyl sulfoxide. Hepatology. 2008;48:889–897. doi: 10.1002/hep.22400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Fullerton AM, Roth RA, Ganey PE. Pretreatment with TCDD exacerbates liver injury from Concanavalin a: critical role for NK cells. Toxicol Sci. 2013;136:72–85. doi: 10.1093/toxsci/kft174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Zou Y, Chen T, Han M, Wang H, Yan W, Song G, Wu Z, et al. Increased killing of liver NK cells by Fas/Fas ligand and NKG2D/NKG2D ligand contributes to hepatocyte necrosis in virus-induced liver failure. J Immunol. 2010;184:466–475. doi: 10.4049/jimmunol.0900687. [DOI] [PubMed] [Google Scholar]
- 115.Wu Z, Han M, Chen T, Yan W, Ning Q. Acute liver failure: mechanisms of immune-mediated liver injury. Liver Int. 2010;30:782–794. doi: 10.1111/j.1478-3231.2010.02262.x. [DOI] [PubMed] [Google Scholar]
- 116.Chen Y, Wei H, Sun R, Dong Z, Zhang J, Tian Z. Increased susceptibility to liver injury in hepatitis B virus transgenic mice involves NKG2D-ligand interaction and natural killer cells. Hepatology. 2007;46:706–715. doi: 10.1002/hep.21872. [DOI] [PubMed] [Google Scholar]
- 117.Vilarinho S, Ogasawara K, Nishimura S, Lanier LL, Baron JL. Blockade of NKG2D on NKT cells prevents hepatitis and the acute immune response to hepatitis B virus. Proc Natl Acad Sci U S A. 2007;104:18187–18192. doi: 10.1073/pnas.0708968104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Han DW. Intestinal endotoxemia as a pathogenetic mechanism in liver failure. World J Gastroenterol. 2002;8:961–965. doi: 10.3748/wjg.v8.i6.961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.West MA, Heagy W. Endotoxin tolerance: a review. Crit Care Med. 2002;30:S64–S73. [PubMed] [Google Scholar]
- 120.Chen T, Zhu L, Zhou Y, Pi B, Liu X, Deng G, Zhang R, et al. KCTD9 contributes to liver injury through NK cell activation during hepatitis B virus-induced acute-on-chronic liver failure. Clin Immunol. 2013;146:207–216. doi: 10.1016/j.clim.2012.12.013. [DOI] [PubMed] [Google Scholar]
- 121.Tsutsui H, Nishiguchi S. Importance of Kupffer cells in the development of acute liver injuries in mice. Int J Mol Sci. 2014;15:7711–7730. doi: 10.3390/ijms15057711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Yang Q, Liu Y, Shi Y, Zheng M, He J, Chen Z. The role of intracellular high-mobility group box 1 in the early activation of Kupffer cells and the development of Con A-induced acute liver failure. Immunobiology. 2013;218:1284–1292. doi: 10.1016/j.imbio.2013.04.011. [DOI] [PubMed] [Google Scholar]
- 123.Fisher JE, McKenzie TJ, Lillegard JB, Yu Y, Juskewitch JE, Nedredal GI, Brunn GJ, et al. Role of Kupffer cells and toll-like receptor 4 in acetaminophen-induced acute liver failure. J Surg Res. 2013;180:147–155. doi: 10.1016/j.jss.2012.11.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Ye Y, Liu J, Lai Q, Zhao Q, Peng L, Xie C, Zhang G, et al. Decreases in activated CD8+ T cells in patients with severe hepatitis B are related to outcomes. Dig Dis Sci. 2015;60:136–145. doi: 10.1007/s10620-014-3297-x. [DOI] [PubMed] [Google Scholar]
- 125.Salama AK, Hodi FS. Cytotoxic T-lymphocyte-associated antigen-4. Clin Cancer Res. 2011;17:4622–4628. doi: 10.1158/1078-0432.CCR-10-2232. [DOI] [PubMed] [Google Scholar]
- 126.Metushi IG, Hayes MA, Uetrecht J. Treatment of PD-1(−/−) mice with amodiaquine and anti-CTLA4 leads to liver injury similar to idiosyncratic liver injury in patients. Hepatology. 2015;61:1332–1342. doi: 10.1002/hep.27549. [DOI] [PubMed] [Google Scholar]
- 127.Li ZL, Xue WJ, Tian PX, Ding XM, Tian XH, Feng XS, Hou J. Prolongation of islet allograft survival by coexpression of CTLA4Ig and CD40LIg in mice. Transplant Proc. 2007;39:3436–3437. doi: 10.1016/j.transproceed.2007.09.025. [DOI] [PubMed] [Google Scholar]
- 128.Uchida T, Hiraga N, Imamura M, Tsuge M, Abe H, Hayes CN, Aikata H, et al. Human cytotoxic T lymphocyte-mediated acute liver failure and rescue by immunoglobulin in human hepatocyte transplant TK-NOG mice. J Virol. 2015;89:10087–10096. doi: 10.1128/JVI.01126-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Mellman I, Coukos G, Dranoff G. Cancer immunotherapy comes of age. Nature. 2011;480:480–489. doi: 10.1038/nature10673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zhang Z, Zhang JY, Wherry EJ, Jin B, Xu B, Zou ZS, Zhang SY, et al. Dynamic programmed death 1 expression by virus-specific CD8 T cells correlates with the outcome of acute hepatitis B. Gastroenterology. 2008;134:1938–1949, 1949.e1–3. doi: 10.1053/j.gastro.2008.03.037. [DOI] [PubMed] [Google Scholar]
- 131.Ji H, Shen X, Gao F, Ke B, Freitas MC, Uchida Y, Busuttil RW, et al. Programmed death-1/B7-H1 negative costimulation protects mouse liver against ischemia and reperfusion injury. Hepatology. 2010;52:1380–1389. doi: 10.1002/hep.23843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Leifeld L, Trautwein C, Dumoulin FL, Manns MP, Sauerbruch T, Spengler U. Enhanced expression of CD80 (B7-1), CD86 (B7-2), and CD40 and their ligands CD28 and CD154 in fulminant hepatic failure. Am J Pathol. 1999;154:1711–1720. doi: 10.1016/S0002-9440(10)65427-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Urakami H, Ostanin DV, Hunig T, Grisham MB. Combination of donor-specific blood transfusion with anti-CD28 antibody synergizes to prolong graft survival in rat liver transplantation. Transplant Proc. 2006;38:3244–3246. doi: 10.1016/j.transproceed.2006.10.042. [DOI] [PubMed] [Google Scholar]
- 134.Dhawan A, Puppi J, Hughes RD, Mitry RR. Human hepatocyte transplantation: current experience and future challenges. Nat Rev Gastroenterol Hepatol. 2010;7:288–298. doi: 10.1038/nrgastro.2010.44. [DOI] [PubMed] [Google Scholar]
- 135.Meyburg J, Alexandrova K, Barthold M, Kafert-Kasting S, Schneider AS, Attaran M, Hoerster F, et al. Liver cell transplantation: basic investigations for safe application in infants and small children. Cell Transplant. 2009;18:777–786. doi: 10.3727/096368909X470775. [DOI] [PubMed] [Google Scholar]
- 136.Wang F, Zhou L, Ma X, Ma W, Wang C, Lu Y, Chen Y, et al. Monitoring of intrasplenic hepatocyte transplantation for acute-on-chronic liver failure: a prospective five-year follow-up study. Transplant Proc. 2014;46:192–198. doi: 10.1016/j.transproceed.2013.10.042. [DOI] [PubMed] [Google Scholar]
- 137.Enosawa S, Horikawa R, Yamamoto A, Sakamoto S, Shigeta T, Nosaka S, Fujimoto J, et al. Hepatocyte transplantation using a living donor reduced graft in a baby with ornithine transcarbamylase deficiency: a novel source of hepatocytes. Liver Transpl. 2014;20:391–393. doi: 10.1002/lt.23800. [DOI] [PubMed] [Google Scholar]
- 138.Li ZR, Mao XH, Hu XX, Nie SD, Shi YZ, Xiang H, Yang JH, et al. Primary human hepatocyte transplantation in the therapy of hepatic failure: 2 cases report. Asian Pac J Trop Med. 2012;5:165–168. doi: 10.1016/S1995-7645(12)60018-2. [DOI] [PubMed] [Google Scholar]
- 139.Fisher RA, Bu D, Thompson M, Tisnado J, Prasad U, Sterling R, Posner M, et al. Defining hepatocellular chimerism in a liver failure patient bridged with hepatocyte infusion. Transplantation. 2000;69:303–307. doi: 10.1097/00007890-200001270-00018. [DOI] [PubMed] [Google Scholar]
- 140.Bilir BM, Guinette D, Karrer F, Kumpe DA, Krysl J, Stephens J, McGavran L, et al. Hepatocyte transplantation in acute liver failure. Liver Transpl. 2000;6:32–40. doi: 10.1002/lt.500060113. [DOI] [PubMed] [Google Scholar]
- 141.Baccarani U, Adani GL, Sanna A, Avellini C, Sainz-Barriga M, Lorenzin D, Montanaro D, et al. Portal vein thrombosis after intraportal hepatocytes transplantation in a liver transplant recipient. Transpl Int. 2005;18:750–754. doi: 10.1111/j.1432-2277.2005.00127.x. [DOI] [PubMed] [Google Scholar]
- 142.Habibullah CM, Syed IH, Qamar A, Taher-Uz Z. Human fetal hepatocyte transplantation in patients with fulminant hepatic failure. Transplantation. 1994;58:951–952. doi: 10.1097/00007890-199410270-00016. [DOI] [PubMed] [Google Scholar]
- 143.Yokoyama T, Ohashi K, Kuge H, Kanehiro H, Iwata H, Yamato M, Nakajima Y. In vivo engineering of metabolically active hepatic tissues in a neovascularized subcutaneous cavity. Am J Transplant. 2006;6:50–59. doi: 10.1111/j.1600-6143.2005.01155.x. [DOI] [PubMed] [Google Scholar]
- 144.Allen KJ, Mifsud NA, Williamson R, Bertolino P, Hardikar W. Cell-mediated rejection results in allograft loss after liver cell transplantation. Liver Transpl. 2008;14:688–694. doi: 10.1002/lt.21443. [DOI] [PubMed] [Google Scholar]
- 145.Lu WY, Bird TG, Boulter L, Tsuchiya A, Cole AM, Hay T, Guest RV, et al. Hepatic progenitor cells of biliary origin with liver repopulation capacity. Nat Cell Biol. 2015;17:971–983. doi: 10.1038/ncb3203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Bai YQ, Yang YX, Yang YG, Ding SZ, Jin FL, Cao MB, Zhang YR, et al. Outcomes of autologous bone marrow mononuclear cell transplantation in decompensated liver cirrhosis. World J Gastroenterol. 2014;20:8660–8666. doi: 10.3748/wjg.v20.i26.8660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Lyra AC, Soares MB, da Silva LF, Braga EL, Oliveira SA, Fortes MF, Silva AG, et al. Infusion of autologous bone marrow mononuclear cells through hepatic artery results in a short-term improvement of liver function in patients with chronic liver disease: a pilot randomized controlled study. Eur J Gastroenterol Hepatol. 2010;22:33–42. doi: 10.1097/MEG.0b013e32832eb69a. [DOI] [PubMed] [Google Scholar]
- 148.Lyra AC, Soares MB, da Silva LF, Fortes MF, Silva AG, Mota AC, Oliveira SA, et al. Feasibility and safety of autologous bone marrow mononuclear cell transplantation in patients with advanced chronic liver disease. World J Gastroenterol. 2007;13:1067–1073. doi: 10.3748/wjg.v13.i7.1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Couto BG, Goldenberg RC, da Fonseca LM, Thomas J, Gutfilen B, Resende CM, Azevedo F, et al. Bone marrow mononuclear cell therapy for patients with cirrhosis: a phase 1 study. Liver Int. 2011;31:391–400. doi: 10.1111/j.1478-3231.2010.02424.x. [DOI] [PubMed] [Google Scholar]
- 150.Esch JS, 2nd, Knoefel WT, Klein M, Ghodsizad A, Fuerst G, Poll LW, Piechaczek C, et al. Portal application of autologous CD133+ bone marrow cells to the liver: a novel concept to support hepatic regeneration. Stem Cells. 2005;23:463–470. doi: 10.1634/stemcells.2004-0283. [DOI] [PubMed] [Google Scholar]
- 151.Burganova GR. Effectiveness of autologous hematopoietic stem cells transplantation in patients with liver cirrhosis. Eksp Klin Gastroenterol. 2012;4:91–97. [PubMed] [Google Scholar]
- 152.Salama H, Zekri AR, Zern M, Bahnassy A, Loutfy S, Shalaby S, Vigen C, et al. Autologous hematopoietic stem cell transplantation in 48 patients with end-stage chronic liver diseases. Cell Transplant. 2010;19:1475–1486. doi: 10.3727/096368910X514314. [DOI] [PubMed] [Google Scholar]
- 153.Salama H, Zekri AR, Bahnassy AA, Medhat E, Halim HA, Ahmed OS, Mohamed G, et al. Autologous CD34+ and CD133+ stem cells transplantation in patients with end stage liver disease. World J Gastroenterol. 2010;16:5297–5305. doi: 10.3748/wjg.v16.i42.5297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.El Omar R, Beroud J, Stoltz JF, Menu P, Velot E, Decot V. Umbilical cord mesenchymal stem cells: the new gold standard for mesenchymal stem cell-based therapies? Tissue Eng Part B Rev. 2014;20:523–544. doi: 10.1089/ten.TEB.2013.0664. [DOI] [PubMed] [Google Scholar]
- 155.Hass R, Kasper C, Bohm S, Jacobs R. Different populations and sources of human mesenchymal stem cells (MSC): a comparison of adult and neonatal tissue-derived MSC. Cell Commun Signal. 2011;9:12. doi: 10.1186/1478-811X-9-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Li Q, Zhou X, Shi Y, Li J, Zheng L, Cui L, Zhang J, et al. In vivo tracking and comparison of the therapeutic effects of MSCs and HSCs for liver injury. PLoS One. 2013;8:e62363. doi: 10.1371/journal.pone.0062363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Jang YO, Kim YJ, Baik SK, Kim MY, Eom YW, Cho MY, Park HJ, et al. Histological improvement following administration of autologous bone marrow-derived mesenchymal stem cells for alcoholic cirrhosis: a pilot study. Liver Int. 2014;34:33–41. doi: 10.1111/liv.12218. [DOI] [PubMed] [Google Scholar]
- 158.Xu L, Gong Y, Wang B, Shi K, Hou Y, Wang L, Lin Z, et al. Randomized trial of autologous bone marrow mesenchymal stem cells transplantation for hepatitis B virus cirrhosis: regulation of Treg/Th17 cells. J Gastroenterol Hepatol. 2014;29:1620–1628. doi: 10.1111/jgh.12653. [DOI] [PubMed] [Google Scholar]
- 159.Peng L, Xie DY, Lin BL, Liu J, Zhu HP, Xie C, Zheng YB, et al. Autologous bone marrow mesenchymal stem cell transplantation in liver failure patients caused by hepatitis B: short-term and long-term outcomes. Hepatology. 2011;54:820–828. doi: 10.1002/hep.24434. [DOI] [PubMed] [Google Scholar]
- 160.Salama H, Zekri AR, Medhat E, Al Alim SA, Ahmed OS, Bahnassy AA, Lotfy MM, et al. Peripheral vein infusion of autologous mesenchymal stem cells in Egyptian HCV-positive patients with end-stage liver disease. Stem Cell Res Ther. 2014;5:70. doi: 10.1186/scrt459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Mohamadnejad M, Alimoghaddam K, Bagheri M, Ashrafi M, Abdollahzadeh L, Akhlaghpoor S, Bashtar M, et al. Randomized placebo-controlled trial of mesenchymal stem cell transplantation in decompensated cirrhosis. Liver Int. 2013;33:1490–1496. doi: 10.1111/liv.12228. [DOI] [PubMed] [Google Scholar]
- 162.Zhang Z, Lin H, Shi M, Xu R, Fu J, Lv J, Chen L, et al. Human umbilical cord mesenchymal stem cells improve liver function and ascites in decompensated liver cirrhosis patients. J Gastroenterol Hepatol. 2012;27(Suppl 2):112–120. doi: 10.1111/j.1440-1746.2011.07024.x. [DOI] [PubMed] [Google Scholar]
- 163.Shi M, Zhang Z, Xu R, Lin H, Fu J, Zou Z, Zhang A, et al. Human mesenchymal stem cell transfusion is safe and improves liver function in acute-on-chronic liver failure patients. Stem Cells Transl Med. 2012;1:725–731. doi: 10.5966/sctm.2012-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Parekkadan B, van Poll D, Suganuma K, Carter EA, Berthiaume F, Tilles AW, Yarmush ML. Mesenchymal stem cell-derived molecules reverse fulminant hepatic failure. PLoS One. 2007;2:e941. doi: 10.1371/journal.pone.0000941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Wang H, Zhao T, Xu F, Li Y, Wu M, Zhu D, Cong X, et al. How important is differentiation in the therapeutic effect of mesenchymal stromal cells in liver disease? Cytotherapy. 2014;16:309–318. doi: 10.1016/j.jcyt.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 166.di Bonzo LV, Ferrero I, Cravanzola C, Mareschi K, Rustichell D, Novo E, Sanavio F, et al. Human mesenchymal stem cells as a two-edged sword in hepatic regenerative medicine: engraftment and hepatocyte differentiation versus profibrogenic potential. Gut. 2008;57:223–231. doi: 10.1136/gut.2006.111617. [DOI] [PubMed] [Google Scholar]
- 167.El-Ansary M, Abdel-Aziz I, Mogawer S, Abdel-Hamid S, Hammam O, Teaema S, Wahdan M. Phase II trial: undifferentiated versus differentiated autologous mesenchymal stem cells transplantation in Egyptian patients with HCV induced liver cirrhosis. Stem Cell Rev. 2012;8:972–981. doi: 10.1007/s12015-011-9322-y. [DOI] [PubMed] [Google Scholar]
- 168.Pan Q, Fouraschen SM, de Ruiter PE, Dinjens WN, Kwekkeboom J, Tilanus HW, van der Laan LJ. Detection of spontaneous tumorigenic transformation during culture expansion of human mesenchymal stromal cells. Exp Biol Med (Maywood) 2014;239:105–115. doi: 10.1177/1535370213506802. [DOI] [PubMed] [Google Scholar]
- 169.Wobus AM, Boheler KR. Embryonic stem cells: prospects for developmental biology and cell therapy. Physiol Rev. 2005;85:635–678. doi: 10.1152/physrev.00054.2003. [DOI] [PubMed] [Google Scholar]
- 170.Kahan B, Magliocca J, Merriam F, Treff N, Budde M, Nelson J, Browning V, et al. Elimination of tumorigenic stem cells from differentiated progeny and selection of definitive endoderm reveals a Pdx1+ foregut endoderm stem cell lineage. Stem Cell Res. 2011;6:143–157. doi: 10.1016/j.scr.2010.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.He ZY, Deng L, Li YF, Xiang D, Hu JK, Chen YX, Wang MJ, et al. Murine embryonic stem cell-derived hepatocytes correct metabolic liver disease after serial liver repopulation. Int J Biochem Cell Biol. 2012;44:648–658. doi: 10.1016/j.biocel.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Chan KM, Fu YH, Wu TJ, Hsu PY, Lee WC. Hepatic stellate cells promote the differentiation of embryonic stem cell-derived definitive endodermal cells into hepatic progenitor cells. Hepatol Res. 2013;43:648–657. doi: 10.1111/j.1872-034X.2012.01110.x. [DOI] [PubMed] [Google Scholar]
- 173.Woo DH, Kim SK, Lim HJ, Heo J, Park HS, Kang GY, Kim SE, et al. Direct and indirect contribution of human embryonic stem cell-derived hepatocyte-like cells to liver repair in mice. Gastroenterology. 2012;142:602–611. doi: 10.1053/j.gastro.2011.11.030. [DOI] [PubMed] [Google Scholar]
- 174.Karabekian Z, Ding H, Stybayeva G, Ivanova I, Muselimyan N, Haque A, Toma I, et al. HLA class I depleted hESC as a source of hypoimmunogenic cells for tissue engineering applications. Tissue Eng Part A. 2015;21:2559–2571. doi: 10.1089/ten.tea.2015.0105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Schwartz SD, Regillo CD, Lam BL, Eliott D, Rosenfeld PJ, Gregori NZ, Hubschman JP, et al. Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt’s macular dystrophy: follow-up of two open-label phase 1/2 studies. Lancet. 2015;385:509–516. doi: 10.1016/S0140-6736(14)61376-3. [DOI] [PubMed] [Google Scholar]
- 176.Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–676. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 177.Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K, Yamanaka S. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131:861–872. doi: 10.1016/j.cell.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 178.Yu J, Vodyanik MA, Smuga-Otto K, Antosiewicz-Bourget J, Frane JL, Tian S, Nie J, et al. Induced pluripotent stem cell lines derived from human somatic cells. Science. 2007;318:1917–1920. doi: 10.1126/science.1151526. [DOI] [PubMed] [Google Scholar]
- 179.Semi K, Matsuda Y, Ohnishi K, Yamada Y. Cellular reprogramming and cancer development. Int J Cancer. 2013;132:1240–1248. doi: 10.1002/ijc.27963. [DOI] [PubMed] [Google Scholar]
- 180.Lister R, Pelizzola M, Kida YS, Hawkins RD, Nery JR, Hon G, Antosiewicz-Bourget J, et al. Hotspots of aberrant epigenomic reprogramming in human induced pluripotent stem cells. Nature. 2011;471:68–73. doi: 10.1038/nature09798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Ruiz S, Diep D, Gore A, Panopoulos AD, Montserrat N, Plongthongkum N, Kumar S, et al. Identification of a specific reprogramming-associated epigenetic signature in human induced pluripotent stem cells. Proc Natl Acad Sci U S A. 2012;109:16196–16201. doi: 10.1073/pnas.1202352109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Li W, Xiang AP. Safeguarding clinical translation of pluripotent stem cells with suicide genes. Organogenesis. 2013;9:34–39. doi: 10.4161/org.24317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Lin T, Wu S. Reprogramming with small molecules instead of exogenous transcription factors. Stem Cells Int. 2015;2015:794632. doi: 10.1155/2015/794632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Shan J, Schwartz RE, Ross NT, Logan DJ, Thomas D, Duncan SA, North TE, et al. Identification of small molecules for human hepatocyte expansion and iPS differentiation. Nat Chem Biol. 2013;9:514–520. doi: 10.1038/nchembio.1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Jozefczuk J, Prigione A, Chavez L, Adjaye J. Comparative analysis of human embryonic stem cell and induced pluripotent stem cell-derived hepatocyte-like cells reveals current drawbacks and possible strategies for improved differentiation. Stem Cells Dev. 2011;20:1259–1275. doi: 10.1089/scd.2010.0361. [DOI] [PubMed] [Google Scholar]
- 186.Baxter M, Withey S, Harrison S, Segeritz CP, Zhang F, Atkinson-Dell R, Rowe C, et al. Phenotypic and functional analyses show stem cell-derived hepatocyte-like cells better mimic fetal rather than adult hepatocytes. J Hepatol. 2015;62:581–589. doi: 10.1016/j.jhep.2014.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Yanagida A, Ito K, Chikada H, Nakauchi H, Kamiya A. An in vitro expansion system for generation of human iPS cell-derived hepatic progenitor-like cells exhibiting a bipotent differentiation potential. PLoS One. 2013;8:e67541. doi: 10.1371/journal.pone.0067541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Chien Y, Chang YL, Li HY, Larsson M, Wu WW, Chien CS, Wang CY, et al. Synergistic effects of carboxymethyl-hexanoyl chitosan, cationic polyurethane-short branch PEI in miR122 gene delivery: accelerated differentiation of iPSCs into mature hepatocyte-like cells and improved stem cell therapy in a hepatic failure model. Acta Biomater. 2015;13:228–244. doi: 10.1016/j.actbio.2014.11.018. [DOI] [PubMed] [Google Scholar]
- 189.Chen YF, Tseng CY, Wang HW, Kuo HC, Yang VW, Lee OK. Rapid generation of mature hepatocyte-like cells from human induced pluripotent stem cells by an efficient three-step protocol. Hepatology. 2012;55:1193–1203. doi: 10.1002/hep.24790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Espejel S, Roll GR, McLaughlin KJ, Lee AY, Zhang JY, Laird DJ, Okita K, et al. Induced pluripotent stem cell-derived hepatocytes have the functional and proliferative capabilities needed for liver regeneration in mice. J Clin Invest. 2010;120:3120–3126. doi: 10.1172/JCI43267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Sgroi A, Mai G, Morel P, Baertschiger RM, Gonelle-Gispert C, Serre-Beinier V, Buhler LH. Transplantation of encapsulated hepatocytes during acute liver failure improves survival without stimulating native liver regeneration. Cell Transplant. 2011;20:1791–1803. doi: 10.3727/096368911X564976. [DOI] [PubMed] [Google Scholar]
- 192.Ramboer E, De Craene B, De Kock J, Vanhaecke T, Berx G, Rogiers V, Vinken M. Strategies for immortalization of primary hepatocytes. J Hepatol. 2014;61:925–943. doi: 10.1016/j.jhep.2014.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Kawashita Y, Guha C, Moitra R, Wang X, Fox IJ, Roy-Chowdhury J, Roy-Chowdhury N. Hepatic repopulation with stably transduced conditionally immortalized hepatocytes in the Gunn rat. J Hepatol. 2008;49:99–106. doi: 10.1016/j.jhep.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 194.Soltys KA, Soto-Gutierrez A, Nagaya M, Baskin KM, Deutsch M, Ito R, Shneider BL, et al. Barriers to the successful treatment of liver disease by hepatocyte transplantation. J Hepatol. 2010;53:769–774. doi: 10.1016/j.jhep.2010.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Zhao X, Tang ZY, Klumpp B, Wolff-Vorbeck G, Barth H, Levy S, von Weizsacker F, et al. Primary hepatocytes of Tupaia belangeri as a potential model for hepatitis C virus infection. J Clin Invest. 2002;109:221–232. doi: 10.1172/JCI13011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Boksa M, Zeyland J, Slomski R, Lipinski D. Immune modulation in xenotransplantation. Arch Immunol Ther Exp (Warsz) 2015;63:181–192. doi: 10.1007/s00005-014-0317-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Starzl TE, Fung J, Tzakis A, Todo S, Demetris AJ, Marino IR, Doyle H, et al. Baboon-to-human liver transplantation. Lancet. 1993;341:65–71. doi: 10.1016/0140-6736(93)92553-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Nagata H, Nishitai R, Shirota C, Zhang JL, Koch CA, Cai J, Awwad M, et al. Prolonged survival of porcine hepatocytes in cynomolgus monkeys. Gastroenterology. 2007;132:321–329. doi: 10.1053/j.gastro.2006.10.013. [DOI] [PubMed] [Google Scholar]
- 199.Ekser B, Gridelli B, Veroux M, Cooper DK. Clinical pig liver xenotransplantation: how far do we have to go? Xenotransplantation. 2011;18:158–167. doi: 10.1111/j.1399-3089.2011.00642.x. [DOI] [PubMed] [Google Scholar]
- 200.Yang L, Guell M, Niu D, George H, Lesha E, Grishin D, Aach J, et al. Genome-wide inactivation of porcine endogenous retroviruses (PERVs) Science. 2015;350:1101–1104. doi: 10.1126/science.aad1191. [DOI] [PubMed] [Google Scholar]
- 201.Gridelli B, Vizzini G, Pietrosi G, Luca A, Spada M, Gruttadauria S, Cintorino D, et al. Efficient human fetal liver cell isolation protocol based on vascular perfusion for liver cell-based therapy and case report on cell transplantation. Liver Transpl. 2012;18:226–237. doi: 10.1002/lt.22322. [DOI] [PubMed] [Google Scholar]
- 202.Chinnici CM, Timoneri F, Amico G, Pietrosi G, Vizzini G, Spada M, Pagano D, et al. Characterization of liver-specific functions of human fetal hepatocytes in culture. Cell Transplant. 2015;24:1139–1153. doi: 10.3727/096368914X680082. [DOI] [PubMed] [Google Scholar]
- 203.Pietrosi G, Vizzini G, Gerlach J, Chinnici C, Luca A, Amico G, D’Amato M, et al. Phases I-II matched case-control study of human Fetal liver cell transplantation for treatment of chronic liver disease. Cell Transplant. 2015;24:1627–1638. doi: 10.3727/096368914X682422. [DOI] [PubMed] [Google Scholar]
- 204.Kamimura R, Ishii T, Sasaki N, Kajiwara M, Machimoto T, Saito M, Kohno K, et al. Comparative study of transplantation of hepatocytes at various differentiation stages into mice with lethal liver damage. Cell Transplant. 2012;21:2351–2362. doi: 10.3727/096368912X636957. [DOI] [PubMed] [Google Scholar]
- 205.Kim SR, Kubo T, Kuroda Y, Hojyo M, Matsuo T, Miyajima A, Usami M, et al. Comparative metabolome analysis of cultured fetal and adult hepatocytes in humans. J Toxicol Sci. 2014;39:717–723. doi: 10.2131/jts.39.717. [DOI] [PubMed] [Google Scholar]
- 206.Herrera MB, Fonsato V, Bruno S, Grange C, Gilbo N, Romagnoli R, Tetta C, et al. Human liver stem cells improve liver injury in a model of fulminant liver failure. Hepatology. 2013;57:311–319. doi: 10.1002/hep.25986. [DOI] [PubMed] [Google Scholar]
- 207.Ono Y, Kawachi S, Hayashida T, Wakui M, Tanabe M, Itano O, Obara H, et al. The influence of donor age on liver regeneration and hepatic progenitor cell populations. Surgery. 2011;150:154–161. doi: 10.1016/j.surg.2011.05.004. [DOI] [PubMed] [Google Scholar]
- 208.Khan AA, Parveen N, Mahaboob VS, Rajendraprasad A, Ravindraprakash HR, Venkateswarlu J, Rao P, et al. Management of hyperbilirubinemia in biliary atresia by hepatic progenitor cell transplantation through hepatic artery: a case report. Transplant Proc. 2008;40:1153–1155. doi: 10.1016/j.transproceed.2008.03.110. [DOI] [PubMed] [Google Scholar]
- 209.Khan AA, Shaik MV, Parveen N, Rajendraprasad A, Aleem MA, Habeeb MA, Srinivas G, et al. Human fetal liver-derived stem cell transplantation as supportive modality in the management of end-stage decompensated liver cirrhosis. Cell Transplant. 2010;19:409–418. doi: 10.3727/096368910X498241. [DOI] [PubMed] [Google Scholar]
- 210.Kuramitsu K, Sverdlov DY, Liu SB, Csizmadia E, Burkly L, Schuppan D, Hanto DW, et al. Failure of fibrotic liver regeneration in mice is linked to a severe fibrogenic response driven by hepatic progenitor cell activation. Am J Pathol. 2013;183:182–194. doi: 10.1016/j.ajpath.2013.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Espanol-Suner R, Carpentier R, Van Hul N, Legry V, Achouri Y, Cordi S, Jacquemin P, et al. Liver progenitor cells yield functional hepatocytes in response to chronic liver injury in mice. Gastroenterology. 2012;143:1564–1575.e7. doi: 10.1053/j.gastro.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 212.Katoonizadeh A, Nevens F, Verslype C, Pirenne J, Roskams T. Liver regeneration in acute severe liver impairment: a clinicopathological correlation study. Liver Int. 2006;26:1225–1233. doi: 10.1111/j.1478-3231.2006.01377.x. [DOI] [PubMed] [Google Scholar]
- 213.Rodrigo-Torres D, Affo S, Coll M, Morales-Ibanez O, Millan C, Blaya D, Alvarez-Guaita A, et al. The biliary epithelium gives rise to liver progenitor cells. Hepatology. 2014;60:1367–1377. doi: 10.1002/hep.27078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Dianat N, Steichen C, Vallier L, Weber A, Dubart-Kupperschmitt A. Human pluripotent stem cells for modelling human liver diseases and cell therapy. Curr Gene Ther. 2013;13:120–132. doi: 10.2174/1566523211313020006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Huang P, He Z, Ji S, Sun H, Xiang D, Liu C, Hu Y, et al. Induction of functional hepatocyte-like cells from mouse fibroblasts by defined factors. Nature. 2011;475:386–389. doi: 10.1038/nature10116. [DOI] [PubMed] [Google Scholar]
- 216.Sekiya S, Suzuki A. Direct conversion of mouse fibroblasts to hepatocyte-like cells by defined factors. Nature. 2011;475:390–393. doi: 10.1038/nature10263. [DOI] [PubMed] [Google Scholar]
- 217.Simeonov KP, Uppal H. Direct reprogramming of human fibroblasts to hepatocyte-like cells by synthetic modified mRNAs. PLoS One. 2014;9:e100134. doi: 10.1371/journal.pone.0100134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Li LJ. State of the art: the diagnosis and treatment of liver failure. Zhonghua Gan Zang Bing Za Zhi. 2010;18(11):801–802. doi: 10.3760/cma.j.issn.1007-3418.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 219.Li LJ, Zhang YM, Liu XL, Du WB, Huang JR, Yang Q, Xu XW, Chen YM. Artificial liver support system in China: a review over the last 30 years. Ther Apher Dial. 2006;10(2):160–167. doi: 10.1111/j.1744-9987.2006.00358.x. [DOI] [PubMed] [Google Scholar]
- 220.Zhou N, Li J, Zhang Y, Lu J, Chen E, Du W, Wang J, Pan X, Zhu D, Yang Y, et al. Efficacy of coupled low-volume plasma exchange with plasma filtration adsorption in treating pigs with acute liver failure: a randomised study. J Hepatol. 2015;63(2):378–387. doi: 10.1016/j.jhep.2015.03.018. [DOI] [PubMed] [Google Scholar]
- 221.Bellomo R, Tetta C, Ronco C. Coupled plasma filtration adsorption. Intensive Care Med. 2003;29(8):1222–1228. doi: 10.1007/s00134-003-1796-x. [DOI] [PubMed] [Google Scholar]
- 222.Nalesso F. Plasma filtration adsorption dialysis (PFAD): a new technology for blood purification. Int J Artif Organs. 2005;28(7):731–738. doi: 10.1177/039139880502800712. [DOI] [PubMed] [Google Scholar]
- 223.Mao HJ, Yu S, Yu XB, Zhang B, Zhang L, Xu XR, Wang XY, Xing CY. Effects of coupled plasma filtration adsorption on immune function of patients with multiple organ dysfunction syndrome. Int J Artif Organs. 2009;32(1):31–38. doi: 10.1177/039139880903200104. [DOI] [PubMed] [Google Scholar]
- 224.Livigni S, Bertolini G, Rossi C, Ferrari F, Giardino M, Pozzato M, Remuzzi G. GiVi TIGIplVdIiTIiaicnoIICu: efficacy of coupled plasma filtration adsorption (CPFA) in patients with septic shock: a multicenter randomised controlled clinical trial. BMJ Open. 2014;4(1):e003536. doi: 10.1136/bmjopen-2013-003536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Maggi U, Nita G, Gatti S, Antonelli B, Paolo R, Como G, Messa P, Rossi G. Hyperbilirubinemia after liver transplantation: the role of coupled plasma filtration adsorption. Transplant Proc. 2013;45(7):2715–2717. doi: 10.1016/j.transproceed.2013.07.019. [DOI] [PubMed] [Google Scholar]
- 226.Li L, editor. Artificial liver. Hangzhou, Zhejiang University Press; 2012. ISBN: 9787308106481 (in Chinese)
- 227.Stange J, Ramlow W, Mitzner S, Schmidt R, Klinkmann H. Dialysis against a recycled albumin solution enables the removal of albumin-bound toxins. Artif Organs. 1993;17(9):809–813. doi: 10.1111/j.1525-1594.1993.tb00635.x. [DOI] [PubMed] [Google Scholar]
- 228.Hassanein T, Blei AT, Perry W, Hilsabeck R, Stange J, Larsen FS, Brown RS, Jr, Caldwell S, McGuire B, Nevens F, et al. Performance of the hepatic encephalopathy scoring algorithm in a clinical trial of patients with cirrhosis and severe hepatic encephalopathy. Am J Gastroenterol. 2009;104(6):1392–1400. doi: 10.1038/ajg.2009.160. [DOI] [PubMed] [Google Scholar]
- 229.Mitzner SR, Stange J, Klammt S, Peszynski P, Schmidt R, Noldge-Schomburg G. Extracorporeal detoxification using the molecular adsorbent recirculating system for critically ill patients with liver failure. J Am Soc Nephrol. 2001;12(Suppl 17):S75–S82. [PubMed] [Google Scholar]
- 230.Hassanein TI, Tofteng F, Brown RS, Jr, McGuire B, Lynch P, Mehta R, Larsen FS, Gornbein J, Stange J, Blei AT. Randomized controlled study of extracorporeal albumin dialysis for hepatic encephalopathy in advanced cirrhosis. Hepatology. 2007;46(6):1853–1862. doi: 10.1002/hep.21930. [DOI] [PubMed] [Google Scholar]
- 231.Heemann U, Treichel U, Loock J, Philipp T, Gerken G, Malago M, Klammt S, Loehr M, Liebe S, Mitzner S, et al. Albumin dialysis in cirrhosis with superimposed acute liver injury: a prospective, controlled study. Hepatology. 2002;36(4 Pt 1):949–958. doi: 10.1053/jhep.2002.36130. [DOI] [PubMed] [Google Scholar]
- 232.Hetz H, Faybik P, Berlakovich G, Baker A, Bacher A, Burghuber C, Sandner SE, Steltzer H, Krenn CG. Molecular adsorbent recirculating system in patients with early allograft dysfunction after liver transplantation: a pilot study. Liver Transpl. 2006;12(9):1357–1364. doi: 10.1002/lt.20804. [DOI] [PubMed] [Google Scholar]
- 233.Tsipotis E, Shuja A, Jaber BL. Albumin dialysis for liver failure: a systematic review. Adv Chronic Kidney Dis. 2015;22(5):382–390. doi: 10.1053/j.ackd.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 234.Saliba F, Camus C, Durand F, Mathurin P, Letierce A, Delafosse B, Barange K, Perrigault PF, Belnard M, Ichai P, et al. Albumin dialysis with a noncell artificial liver support device in patients with acute liver failure: a randomized, controlled trial. Ann Intern Med. 2013;159(8):522–531. doi: 10.7326/0003-4819-159-8-201310150-00005. [DOI] [PubMed] [Google Scholar]
- 235.Rifai K, Ernst T, Kretschmer U, Bahr MJ, Schneider A, Hafer C, Haller H, Manns MP, Fliser D. Prometheus—a new extracorporeal system for the treatment of liver failure. J Hepatol. 2003;39(6):984–990. doi: 10.1016/s0168-8278(03)00468-9. [DOI] [PubMed] [Google Scholar]
- 236.Kribben A, Gerken G, Haag S, Herget-Rosenthal S, Treichel U, Betz C, Sarrazin C, Hoste E, Van Vlierberghe H, Escorsell A, et al. Effects of fractionated plasma separation and adsorption on survival in patients with acute-on-chronic liver failure. Gastroenterology. 2012;142(4):782–789.e3. doi: 10.1053/j.gastro.2011.12.056. [DOI] [PubMed] [Google Scholar]
- 237.Seige M, Kreymann B, Jeschke B, Schweigart U, Kopp KF, Classen M. Long-term treatment of patients with acute exacerbation of chronic liver failure by albumin dialysis. Transplant Proc. 1999;31(1–2):1371–1375. doi: 10.1016/s0041-1345(98)02033-8. [DOI] [PubMed] [Google Scholar]
- 238.Kortgen A, Rauchfuss F, Gotz M, Settmacher U, Bauer M, Sponholz C. Albumin dialysis in liver failure: comparison of molecular adsorbent recirculating system and single pass albumin dialysis—a retrospective analysis. Ther Apher Dial. 2009;13(5):419–425. doi: 10.1111/j.1744-9987.2009.00760.x. [DOI] [PubMed] [Google Scholar]
- 239.Wauters J, Wilmer A. Albumin dialysis: current practice and future options. Liver Int. 2011;31(Suppl 3):9–12. doi: 10.1111/j.1478-3231.2011.02589.x. [DOI] [PubMed] [Google Scholar]
- 240.Banares R, Nevens F, Larsen FS, Jalan R, Albillos A, Dollinger M, Saliba F, Sauerbruch T, Klammt S, Ockenga J, et al. Extracorporeal albumin dialysis with the molecular adsorbent recirculating system in acute-on-chronic liver failure: the RELIEF trial. Hepatology. 2013;57(3):1153–1162. doi: 10.1002/hep.26185. [DOI] [PubMed] [Google Scholar]
- 241.Li L. Artificial liver. 2. Hangzhou: Zhejiang University Press; 2012. [Google Scholar]
- 242.Ellis AJ, Hughes RD, Wendon JA, Dunne J, Langley PG, Kelly JH, Gislason GT, Sussman NL, Williams R. Pilot-controlled trial of the extracorporeal liver assist device in acute liver failure. Hepatology. 1996;24(6):1446–1451. doi: 10.1002/hep.510240625. [DOI] [PubMed] [Google Scholar]
- 243.Mazariegos GV, Kramer DJ, Lopez RC, Shakil AO, Rosenbloom AJ, Devera M, Giraldo M, Grogan TA, Zhu Y, Fulmer ML, et al. Safety observations in phase I clinical evaluation of the Excorp Medical Bioartificial Liver Support System after the first four patients. ASAIO J. 2001;47(5):471–475. doi: 10.1097/00002480-200109000-00015. [DOI] [PubMed] [Google Scholar]
- 244.Morsiani E, Pazzi P, Puviani AC, Brogli M, Valieri L, Gorini P, Scoletta P, Marangoni E, Ragazzi R, Azzena G, et al. Early experiences with a porcine hepatocyte-based bioartificial liver in acute hepatic failure patients. Int J Artif Organs. 2002;25(3):192–202. doi: 10.1177/039139880202500305. [DOI] [PubMed] [Google Scholar]
- 245.Qian Y, Lanjuan L, Jianrong H, Jun L, Hongcui C, Suzhen F, Xia Y, Shuhong Y. Study of severe hepatitis treated with a hybrid artificial liver support system. Int J Artif Organs. 2003;26(6):507–513. doi: 10.1177/039139880302600609. [DOI] [PubMed] [Google Scholar]
- 246.Zheng S, Wu J, Yu F, Wang Y, Chen L, Cui D, Xie G, Yang X, Chen X, Zhang W, et al. Elevation of creatine kinase is linked to disease severity and predicts fatal outcomes in H7N9 infection. Clin Chem Lab Med. 2017;55(8):e163–e166. doi: 10.1515/cclm-2016-0741. [DOI] [PubMed] [Google Scholar]
- 247.Demetriou Achilles A., Brown Robert S., Busuttil Ronald W., Fair Jeffrey, McGuire Brendan M., Rosenthal Philip, Am Esch Jan Schulte, Lerut Jan, Nyberg Scott L., Salizzoni Mauro, Fagan Elizabeth A., de Hemptinne Bernard, Broelsch Christoph E., Muraca Maurizio, Salmeron Joan Manuel, Rabkin John M., Metselaar Herold J., Pratt Daniel, De La Mata Manuel, McChesney Lawrence P., Everson Gregory T., Lavin Philip T., Stevens Anthony C., Pitkin Zorina, Solomon Barry A. Prospective, Randomized, Multicenter, Controlled Trial of a Bioartificial Liver in Treating Acute Liver Failure. Annals of Surgery. 2004;239(5):660–670. doi: 10.1097/01.sla.0000124298.74199.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Sauer IM, Zeilinger K, Pless G, Kardassis D, Theruvath T, Pascher A, Goetz M, Neuhaus P, Gerlach JC. Extracorporeal liver support based on primary human liver cells and albumin dialysis—treatment of a patient with primary graft non-function. J Hepatol. 2003;39(4):649–653. doi: 10.1016/s0168-8278(03)00348-9. [DOI] [PubMed] [Google Scholar]
- 249.van de Kerkhove MP, Di Florio E, Scuderi V, Mancini A, Belli A, Bracco A, Dauri M, Tisone G, Di Nicuolo G, Amoroso P, et al. Phase I clinical trial with the AMC-bioartificial liver. Int J Artif Organs. 2002;25(10):950–959. doi: 10.1177/039139880202501009. [DOI] [PubMed] [Google Scholar]
- 250.Li L. Organization Committee of 13th Asia-Pacific Congress of Clinical Microbiology and Infection Consensus Guidelines for diagnosis and treatment of liver failure. Hepatobiliary Pancreat Dis Int. 2013;12(4):346–354. doi: 10.1016/s1499-3872(13)60055-7. [DOI] [PubMed] [Google Scholar]
- 251.Frimmel S, Schipper J, Henschel J, Yu TT, Mitzner SR, Koball S. First description of single-pass albumin dialysis combined with cytokine adsorption in fulminant liver failure and hemophagocytic syndrome resulting from generalized herpes simplex virus 1 infection. Liver Transpl. 2014;20(12):1523–1524. doi: 10.1002/lt.24005. [DOI] [PubMed] [Google Scholar]
- 252.Kono K, Toda S, Hora K, Kiyosawa K. Direct hemoperfusion with a beta2-microglobulin-selective adsorbent column eliminates inflammatory cytokines and improves pulmonary oxygenation. Ther Apher Dial. 2009;13(1):27–33. doi: 10.1111/j.1744-9987.2009.00652.x. [DOI] [PubMed] [Google Scholar]
- 253.Zagli G, Bonizzoli M, Spina R, Cianchi G, Pasquini A, Anichini V, Matano S, Tarantini F, Di Filippo A, Maggi E, et al. Effects of hemoperfusion with an immobilized polymyxin-B fiber column on cytokine plasma levels in patients with abdominal sepsis. Minerva Anestesiol. 2010;76(6):405–412. [PubMed] [Google Scholar]
- 254.Oishi K, Mimura-Kimura Y, Miyasho T, Aoe K, Ogata Y, Katayama H, Murata Y, Ueoka H, Matsumoto T, Mimura Y. Association between cytokine removal by polymyxin B hemoperfusion and improved pulmonary oxygenation in patients with acute exacerbation of idiopathic pulmonary fibrosis. Cytokine. 2013;61(1):84–89. doi: 10.1016/j.cyto.2012.08.032. [DOI] [PubMed] [Google Scholar]
- 255.Jeon H, Lee SG. Living donor liver transplantation. Curr Opin Organ Transplant. 2010;15(3):283–287. doi: 10.1097/MOT.0b013e32833983ee. [DOI] [PubMed] [Google Scholar]
- 256.Cesaretti Manuela, Dioguardi Burgio Marco, Zarzavadjian Le Bian Alban. Abdominal emergencies after liver transplantation: Presentation and surgical management. Clinical Transplantation. 2017;31(11):e13102. doi: 10.1111/ctr.13102. [DOI] [PubMed] [Google Scholar]
- 257.Li H, Chen HS, Nyberg SL. Extracorporeal liver support and liver transplant for patients with acute-on-chronic liver failure. Semin Liver Dis. 2016;36(2):153–160. doi: 10.1055/s-0036-1583197. [DOI] [PubMed] [Google Scholar]
- 258.Kok B, Ewasiuk A, Karvellas CJ. Liver transplant in acute-on-chronic liver failure: evaluating the impact of organ dysfunction. Liver Int. 2017;37(5):651–652. doi: 10.1111/liv.13365. [DOI] [PubMed] [Google Scholar]
- 259.Chen K, Cao X, Zheng Y, Xu M, Peng J. Comparative study of the MELD-Na and Child–Turcotte–Pugh scores as short-term prognostic indicators of acute-on-chronic hepatitis B liver failure. Zhonghua Gan Zang Bing Za Zhi. 2014;22(11):801–805. doi: 10.3760/cma.j.issn.1007-3418.2014.11.001. [DOI] [PubMed] [Google Scholar]
- 260.Pugh RN, Murray-Lyon IM, Dawson JL, Pietroni MC, Williams R. Transection of the oesophagus for bleeding oesophageal varices. Br J Surg. 1973;60(8):646–649. doi: 10.1002/bjs.1800600817. [DOI] [PubMed] [Google Scholar]
- 261.Leise MD, Kim WR, Kremers WK, Larson JJ, Benson JT, Therneau TM. A revised model for end-stage liver disease optimizes prediction of mortality among patients awaiting liver transplantation. Gastroenterology. 2011;140(7):1952–1960. doi: 10.1053/j.gastro.2011.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Núñez-Ramos R, Montoro S, Bellusci M, Del Fresno-Valencia MR, Germán-Díaz M, Urruzuno P, Medina E, Manzanares J. Acute liver failure: outcome and value of pediatric end-stage liver disease score in pediatric cases. Pediatr Emerg Care. 2018;34:409–412. doi: 10.1097/PEC.0000000000000884. [DOI] [PubMed] [Google Scholar]
- 263.Mallet M, Rudler M, Thabut D. Variceal bleeding in cirrhotic patients. Gastroenterol Rep (Oxf) 2017;5(3):185–192. doi: 10.1093/gastro/gox024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Babu R, Sethi P, Surendran S, Dhar P, Gopalakrishnan U, Balakrishnan D, Menon RN, Sivasankarapillai Thankamonyamma B, Othiyil Vayoth S, Thillai M. A new score to predict recipient mortality from preoperative donor and recipient characteristics in living donor liver transplantation (DORMAT score) Ann Transplant. 2017;22:499–506. doi: 10.12659/aot.904350. [DOI] [PubMed] [Google Scholar]
- 265.Wang H, Jiang W, Zhou Z, Long J, Li W, Fan ST. Liver transplantation in mainland China: the overview of CLTR 2011 annual scientific report. Hepatobiliary Surg Nutr. 2013;2(4):188–197. doi: 10.3978/j.issn.2304-3881.2013.08.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Cortes M, Vilca-Melendez H, Heaton N. The use of temporary portocaval shunt as a technical aid in auxiliary orthotopic liver transplantation. Liver Transpl. 2016;22(11):1607–1609. doi: 10.1002/lt.24510. [DOI] [PubMed] [Google Scholar]
- 267.Bismuth H. Current status of auxiliary partial orthotopic liver transplantation for acute liver failure. Liver Transpl. 2017;23(5):710. doi: 10.1002/lt.24694. [DOI] [PubMed] [Google Scholar]
- 268.Hessheimer AJ, Nacif L, Flores Villalba E, Fondevila C. Liver transplantation for acute liver failure. Cir Esp. 2017;95(4):181–189. doi: 10.1016/j.ciresp.2017.01.008. [DOI] [PubMed] [Google Scholar]
- 269.Wadhawan M, Gupta S, Goyal N, Taneja S, Kumar A. Living related liver transplantation for hepatitis B-related liver disease without hepatitis B immune globulin prophylaxis. Liver Transpl. 2013;19(9):1030–1035. doi: 10.1002/lt.23692. [DOI] [PubMed] [Google Scholar]