Abstract
Background:
Revision surgery in cases of previously failed primary acromioclavicular (AC) joint stabilization remains challenging mainly because of anatomic alterations or technical difficulties. However, anatomic coracoclavicular ligament reconstruction (ACCR) has been shown to achieve encouraging biomechanical, clinical, and radiographic short-term to midterm results.
Purpose:
To evaluate the clinical and radiographic long-term outcomes of patients undergoing revision ACCR after failed operative treatment for type III through V AC joint injuries with a minimum 10-year follow-up.
Study Design:
Case series; Level of evidence, 4.
Methods:
A retrospective chart review was performed on prospectively collected data within an institutional shoulder registry. Patients who underwent revision ACCR for type III through V AC joint injuries between January 2003 and December 2009 were analyzed. Clinical outcome measures included the American Shoulder and Elbow Surgeons (ASES) score, Simple Shoulder Test (SST), and Single Assessment Numeric Evaluation (SANE). The coracoclavicular distance (CCD) was measured for radiographic analysis immediately postoperatively and at last postoperative follow-up.
Results:
A total of 8 patients with a mean age at the time of surgery of 44.6 ± 10.6 years and a mean follow-up of 135.0 ± 17.4 months (range, 120-167 months) were eligible for inclusion in the study. The time from initial AC joint stabilization until revision surgery was 10.2 ± 12.4 months (range, 0.5-36 months); 62.5% of the patients had undergone more than 2 previous AC joint surgical procedures. The ASES score improved from 43.9 ± 22.4 preoperatively to 80.6 ± 28.8 postoperatively (P = .012), the SST score improved from 4.4 ± 3.6 preoperatively to 11.0 ± 2.2 postoperatively (P = .017), and the SANE score improved from 31.4 ± 27.3 preoperatively to 86.9 ± 24.1 postoperatively (P = .018) at final follow-up. There was no significant difference in the CCD (P = .08) between the first (7.6 ± 3.0 mm) and final (10.6 ± 2.8 mm) radiographic follow-up (mean, 50.5 ± 32.7 months [range, 18-98 months]).
Conclusion:
Patients undergoing revision ACCR after failed operative treatment for type III through V AC joint injuries maintained significant improvement in clinical outcomes at a minimum 10-year follow-up.
Keywords: anatomic coracoclavicular ligament reconstruction, ACCR, AC joint, acromioclavicular joint injury, revision
Given that variable complication rates after acromioclavicular (AC) joint reconstruction have been reported, shoulder surgeons may encounter an increasing number of postoperative failures.11,12,20,45,52 The overall failure rate has been shown to be as high as 21% of cases, resulting in a subsequent revision rate of almost 10%.20 However, failure and revision rates may be highly dependent on the accuracy of the initial diagnosis and stabilization technique.12,20,36
In the past decade, a trend toward arthroscopically assisted techniques for AC joint stabilization has emerged; however, open approaches, such as anatomic coracoclavicular ligament reconstruction (ACCR), have been shown to achieve high subjective satisfaction rates along with significant clinical and radiographic improvement.2,9,12,35,38 Biomechanically, ACCR using a free tendon allograft to replicate the native coracoclavicular (CC) ligaments has been demonstrated to provide better vertical and horizontal stability compared with that of nonanatomic techniques.21,26,32 Especially in the setting of revision surgery, this technique may allow for more detailed visualization of existing anatomic alterations along with effective restoration of the native joint kinematics. Additionally, using free tendon grafts results in similar loads to failure and elongation when compared with the native CC ligaments while being a less stiff construct.11,12
However, the effect of previous AC joint stabilization on postoperative outcomes in revision surgery is still lacking in the current literature or limited to short follow-up periods and small case series.12,23,25,45,49 When considering revision cases, a higher rate of complications may be expected because of bony disorders, such as bone loss at the distal clavicle or large bone tunnels created in the clavicle and/or coracoid.12,13,25,28,29,47,48,50 Thus, performing a detailed failure analysis is of great importance to reduce failure rates and adequately restore native joint biomechanics for ensuring an optimal healing environment.12
The purpose of this study was to investigate the long-term clinical and radiographic outcomes of patients undergoing revision ACCR after previously failed AC joint reconstruction of type III through V injuries. We hypothesized that patients undergoing revision ACCR would maintain significant improvement in clinical and radiographic outcomes at a minimum 10-year follow-up.
Methods
Patient Selection
Institutional review board approval was obtained before the initiation of the study (No. 17-066-3). A retrospective chart review was performed on patients undergoing revision ACCR using a free tendon allograft by a single shoulder fellowship-trained surgeon (A.D.M.) between January 2003 and December 2009. Patients eligible for study inclusion were those aged ≥18 years who underwent a revision ACCR procedure for failed AC joint reconstruction or repair after an acute or chronic type III, IV, or V AC joint dislocation (defined by the Rockwood classification42). Failure was defined as loss of reduction, leading to chronic scapular or glenohumeral joint dysfunction or pain, upper limb impairment, persistent vertical or horizontal instability of the AC joint, hardware failure, and fractures.1,28,30,46–48 After the diagnosis of recurrent instability, all patients underwent nonoperative treatment for a minimum of 1 month, which included physical therapy. Exclusion criteria included vulnerable populations (eg, inmates).
Surgical Technique
Each patient underwent ACCR using a tendon allograft (semitendinosus or peroneus longus) with subsequent interference screw fixation in the clavicle as previously described.9,32,38 Overall, two 5.0-mm bone tunnels (posteromedial and anterolateral) were drilled into the clavicle according to the anatomic locations of the conoid and trapezoid ligaments and then tapped to 5.5 mm. When possible, a minimum distance of 20 to 25 mm was maintained between tunnels, and the trapezoid tunnel was placed at least 15 mm medial from the distal end of the clavicle.9,32,38
The graft was passed beneath the coracoid process from medial to lateral under direct visualization and crossed before being shuttled through both tunnels. An additional suture augmentation procedure was performed to act as an internal brace and support the healing process. While maintaining accurate AC joint reduction, both graft limbs were secured using 5.5 × 8–mm PEEK interference screws (Arthrex) with continuous tension on the graft. One patient required 7.0 × 8–mm PEEK interference screw fixation for the lateral limb. The longer limb of the graft was used to reinforce the superior and posterior parts of the repaired AC joint capsule by suturing it to the acromion. Small drill tunnels or suture anchors were placed into the acromion, when possible.38 Additional distal clavicle excision (DCE; 5-8 mm) was performed in 2 patients, as osteophytes did not allow optimal AC joint reduction. By removing some of the bony tissue, optimal reduction was achieved. Meticulous closure of the deltotrapezial fascia was performed using interrupted nonabsorbable sutures.9,32,38
Postoperative Rehabilitation
Postoperative rehabilitation consisted of wearing a shoulder unloader brace (Lerman Shoulder Orthosis; DonJoy) for 6 weeks as previously described by Muench et al.38 Pendulum exercises were allowed for the first 6 weeks. Patients were permitted to initiate upright range of motion exercises at 2 months postoperatively. Strengthening exercises were implemented after 12 weeks, focusing on scapular stabilizers, to decrease AC joint loads. Weight training was incorporated within 3 to 5 months, and contact athletic activity began as early as 6 months after surgery.9,38
Clinical Outcomes
Outcome measures included the American Shoulder and Elbow Surgeons (ASES) score, the Simple Shoulder Test (SST), and the Single Assessment Numeric Evaluation (SANE).27,38,41,51 These scores were collected preoperatively and at a minimum of 10 years postoperatively. Previous studies3,19,38,51 have confirmed these scores in terms of reliability, validity, and responsiveness.
Radiographic Outcomes
Radiographic measurements were performed on unweighted anterior-posterior bilateral Zanca view radiographs. Loss of reduction during follow-up was evaluated by calculating the difference between the coracoclavicular distance (CCD) of the involved side immediately postoperatively and that at final radiographic follow-up. The CCD was measured in millimeters as the distance between the tip of the coracoid and the inferior cortex of the clavicle.53,54
Statistical Analysis
Descriptive statistics including mean, standard deviation, median, and interquartile range were calculated to characterize the clinical and radiographic outcomes of the study cohort. Differences between preoperative and postoperative (change in score from preoperatively to postoperatively [delta]) outcomes were examined using the Wilcoxon signed rank test. A P value of <.05 was considered statistically significant. All analyses were performed using Stata statistical software (Release 15; StataCorp).
Results
Participants
In a single surgeon’s practice, 37 consecutive patients underwent ACCR using a free tendon allograft between January 2003 and December 2009. Of these, 10 patients were eligible for inclusion in the study (Figure 1). However, 2 of these patients declined to participate in the study. The mean age of the patients at the time of surgery was 44.6 ± 10.6 years (range, 29-57 years), with a mean follow-up of 135.0 ± 17.4 months (range, 120-167 months). Overall, 7 patients (87.5%) were male. The mean time from initial (primary) instability to revision surgery was 112.4 ± 158.8 months (range, 7-400 months). Moreover, 50.0% of the patients had a new injury resulting in recurrent instability. The mean time from primary AC joint stabilization to revision surgery was 10.2 ± 12.4 months (range, 0.5-36 months).
Figure 1.
Flowchart displaying patients meeting study criteria.
All 8 patients had undergone previous CC ligament reconstruction. The most common procedures were noted to be DCE and ACCR, with 5 cases each (35.7%). In those patients with failed ACCR, previous anatomic bone tunnels could be reused. However, as noted, 1 patient required larger screw fixation (7.0 × 8–mm PEEK interference screw) for the lateral limb. Previous nonanatomic CC ligament reconstruction (including open or arthroscopic-assisted CC ligament repair using high-strength tensile sutures) was noted in 3 patients. Patient characteristics are demonstrated in Tables 1 and 2.
Table 1.
Patient Characteristics of Cohort (n = 8)a
| Sex, n (%) | |
| Male | 7 (87.5) |
| Female | 1 (12.5) |
| Age, y | 44.6 ± 10.6 |
| Follow-up, mo | 135.0 ± 17.4 |
| Right shoulder, n (%) | 4 (50.0) |
| Dominant extremity, n (%) | 4 (50.0) |
| Injury pattern, n (%) | |
| Type III | 1 (12.5) |
| Type IV | 1 (12.5) |
| Type V | 6 (75.0) |
| Time from initial stabilization to recurrence, mo | 10.2 ± 12.4 |
| History of trauma, n (%) | 4 (50.0) |
| Type of primary surgery, n (%) | |
| DCE | 5 (35.7) |
| CA ligament transfer | 1 (7.1) |
| ACCR | 5 (35.7) |
| Nonanatomic CC ligament reconstruction | 3 (21.4) |
aData are shown as mean ± SD unless otherwise indicated. ACCR, anatomic coracoclavicular ligament reconstruction; CA, coracoacromial; CC, coracoclavicular; DCE, distal clavicle excision.
Table 2.
Individual Patient Characteristics of All 8 Included Patientsa
| Patient | Sex | Age, y | Dominant Side | Time From Primary Instability to Revision ACCR, mo | Clinical Follow-up, mo | Previous Surgical Procedures |
|---|---|---|---|---|---|---|
| 1 | Female | 55 | Left | 400 | 121 | ACCR, DCE |
| 2 | Male | 29 | Left | 12 | 120 | Nonanatomic CC ligament reconstruction, CA ligament transfer, DCE |
| 3 | Male | 34 | Left | 22 | 147 | ACCR, DCE |
| 4 | Male | 56 | Right | 12 | 125 | ACCR |
| 5 | Male | 44 | Left | 324 | 167 | ACCR, DCE |
| 6 | Male | 57 | Right | 9 | 131 | ACCR |
| 7 | Male | 39 | Right | 7 | 149 | Nonanatomic CC ligament reconstruction, DCE |
| 8 | Male | 43 | Right | 108 | 120 | Nonanatomic CC ligament reconstruction |
| Mean ± SD | 44.6 ± 10.6 | 112.4 ± 158.8 | 135.0 ± 17.4 |
aACCR, anatomic coracoclavicular ligament reconstruction; CA, coracoacromial; CC, coracoclavicular; DCE, distal clavicle excision.
Clinical Outcomes
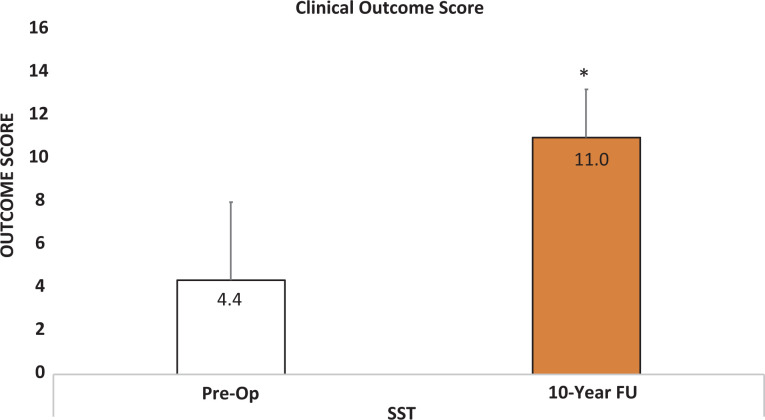
For all patients, there was a significant improvement on all primary outcome measures from preoperatively to postoperatively. The ASES score improved from 43.9 ± 22.4 preoperatively to 80.6 ± 28.8 postoperatively (P = .012), the SST score improved from 4.4 ± 3.6 preoperatively to 11.0 ± 2.2 postoperatively (P = .017), and the SANE score improved from 31.4 ± 27.3 preoperatively to 86.9 ± 24.1 postoperatively (P = .018) at final follow-up (Figures 2 and 3).
Figure 2.
Preoperative and postoperative American Shoulder and Elbow Surgeons (ASES) and Single Assessment Numeric Evaluation (SANE) scores at final follow-up for all patients undergoing revision anatomic coracoclavicular ligament reconstruction. *Significant improvement (P < .05) when compared with preoperatively. FU, follow-up; Pre-Op, preoperative.
Figure 3.
Preoperative and postoperative Simple Shoulder Test (SST) scores at final follow-up for all patients undergoing revision anatomic coracoclavicular ligament reconstruction. *Significant improvement (P < .05) when compared with preoperatively. FU, follow-up; Pre-Op, preoperative.
Radiographic Outcomes
The mean time from the first postoperative radiographic follow-up to last radiographic follow-up was 50.5 ± 32.7 months (range, 18-98 months). The CCD increased from 7.6 ± 3.0 mm to 10.6 ± 2.8 mm at final radiographic follow-up. However, this was found to be nonsignificant (P = .08).
Postoperative Complications
Overall, 1 patient was found to have postoperative osteolysis at the distal clavicle, requiring no further surgical intervention. Additionally, this patient was noted to have undergone previous DCE. No infections or clinical failures were noted.
Discussion
The most important finding of this study was that patients undergoing revision ACCR for chronic AC joint separation maintained postoperative clinical improvement at a minimum 10-year follow-up. One patient had postoperative osteolysis around the distal clavicle; however, this complication did not require a further surgical intervention. Interestingly, this patient was noted to have undergone DCE before the revision ACCR procedure.
Recurrent AC joint instability remains a common challenge in the orthopaedic literature.1,7,12,20,36 The definition of failure includes loss of reduction, leading to chronic scapular or glenohumeral joint dysfunction or pain, (sub)luxation with persistent vertical or horizontal instability of the AC joint, infections, hardware failure, and fractures.1,28,30,46–48 To date, more than 150 different stabilization techniques have been described, with complication rates being highly dependent on the type of repair.1,7,12,20,36 Currently, AC joint reconstruction is recognized as a safe procedure with distinct complication profiles, varying between 5% and 89% of cases, depending on the specific surgical technique.12,28,52 The most common complications can be classified into 5 categories including infections, fractures, hardware/button failure, calcification, and osteolysis of the distal clavicle.20 Subsequently, most of these complications are caused by technical errors and a steep learning curve of the operating surgeon, which has to be taken into account when performing AC joint reconstruction.34
As the data from this study showed, 7 of 8 patients underwent DCE. Complication rates after DCE for AC joint instability remain high, with almost 65% of the patients having postoperative complications.10,31 Thus, when performing DCE, inadequate resection (underresection or overresection) and wrong indications can result in significant pain or instability (Figure 4).5,40 Overresection, which may cause persistent horizontal and vertical instability, remains a challenging problem, resulting in significant pain and dysfunction.40,44 The precise amount of recommended resection length remains unknown; however, resection of greater than 8 mm (women) or 10 mm (men) may put the trapezoid ligament at risk.5,8,16,39 Additionally, there is little evidence that excision of the lateral clavicle successfully addresses the pathological entities encountered at the AC joint.40 Thus, DCE, when needed, may not exceed these 8- and 10-mm recommendations.
Figure 4.

(A) A patient with recurrent acromioclavicular (AC) joint instability after failed distal clavicle excision. (B) Postoperative imaging 18 months after revision anatomic coracoclavicular ligament reconstruction for AC joint instability.
When considering revision cases, controversy exists on how to best address recurrent AC joint instability, with only limited data regarding clinical and radiographic outcomes having been published.12,20,25,45,49 In 2007, Tauber et al45 demonstrated good clinical and radiographic outcomes in 12 patients undergoing revision AC joint reconstruction with arthroscopically assisted CC ligament reconstruction using a semitendinosus tendon autograft and additional cerclage or Bosworth screw fixation. Kraus et al25 investigated a series of 14 patients undergoing revision AC joint reconstruction with arthroscopic AC and CC ligament stabilization using a gracilis tendon autograft and TightRope augmentation, with good clinical and radiographic outcomes after a median follow-up of 28.8 months. In patients with previously failed ligament transfer (eg, Weaver-Dunn), Kany et al23 proposed all-arthroscopic augmented transposition of the conjoined tendons (eg, Vargas technique) as a salvage procedure in 2 patients, with no loss of reduction at final follow-up. However, long-term data regarding clinical and radiographic outcomes of patients undergoing revision ACCR after failed primary AC joint reconstruction are limited.
In case of failed AC joint reconstruction, conducting an accurate failure analysis is essential.12 Recently, Dyrna et al12 proposed a treatment algorithm for revision AC joint reduction based on the most common modes of failure. If insufficient primary fixation is suspected, anatomic stabilization of the CC and AC ligaments using a free tendon graft should be considered, as anatomic reconstruction of the conoid and trapezoid ligaments using a tendon graft best restores native biomechanical properties.11,32,33 Furthermore, given that higher bone mineral density values were found at the anatomic CC ligament insertions, this may result in higher fixation strength along with a reduced risk of fractures.18,50 In revision cases, bone tunnels can be reutilized if no significant tunnel widening and correct tunnel positioning are given.50 Additionally, chronic scapular or glenohumeral joint dysfunction or pain may be related to (sub)luxation with persistent horizontal or rotational instability of the AC joint.1 In case of persisting horizontal and rotational instability, the scapula lacks an anterior strut; therefore, additional augmentation of the AC joint capsule should be considered, as chronic and painful limitation of the shoulder girdle might result.1,4,12,14,15,22,43 Furthermore, the importance of the superior-posterior capsuloligamentous structures of the AC joint and their deficiency in chronic AC joint instability have been highlighted in biomechanical studies.14,15,17,24,37 Thus, surgeons should carefully evaluate the AC joint intraoperatively and adapt their treatment algorithm to the clinical findings.12
The data from this study showed that the mean increase in the radiographic CCD over the postoperative course was almost 3 mm. However, this observation was found to be nonsignificant, which may have been caused by type II errors. For this, radiographic loss of reduction could not be investigated at final clinical follow-up, which would have been of interest, as the time from injury to surgery may have an influence on postoperative clinical or radiographic complications, such as loss of reduction and subsequent clinical failure.38 However, Berthold et al6 recently demonstrated that radiographic alterations (eg, loss of reduction), which may occur through a combination of complex loading and unloading mechanisms, such as the windshield wiper or bungee cord effect, and biological factors had no influence on clinical outcomes, benefits, and satisfaction after surgery. Yet, patients with confirmed radiographic loss of reduction should still be evaluated critically, as insufficient stabilization techniques, wrong indications, or radiographic complications may lead to the observed findings, thus resulting in clinical failures. As a final point, the current literature is still lacking a clear consensus for defining a threshold for radiographic loss of reduction, which indicates the difficulty in assessing the CCD over the postoperative course.20
There were several limitations to this study. First, outcomes for this study were collected prospectively; however, data were reviewed retrospectively, which could create selection bias. Second, this study was conducted with a small patient cohort over a long time period without having a control group. However, patients requiring revision AC joint surgery account for only 9.5% of all patients with AC joint reconstruction, characterizing these patients with chronic AC joint instability as a rare and challenging cohort.20 The small cohort size may have resulted in type II errors for the radiographic CCD measurements being nonsignificant. Additionally, preoperative CCD measurements were not performed, and no good method to assess horizontal and/or rotational stability was available. Third, the patient population in the current study was older than was the younger, athletic population in which these injuries have been described,4 making the results possibly less generalizable. For this, no data on activity or sports participation could be collected. The patient cohort described in this study was very heterogeneous with regard to previous surgical procedures. Therefore, comparing our results to the current literature was difficult, as to date, there is a lack of studies regarding revision AC joint surgery. Lastly, 7 of 8 patients underwent DCE; thus, it remains unclear how much of the benefit may be a result of DCE.
Conclusion
Patients undergoing revision ACCR after failed operative treatment for type III through V AC joint injuries maintained significant improvement in clinical outcomes at a minimum 10-year follow-up.
Footnotes
Final revision submitted May 17, 2020; accepted June 8, 2020.
One or more of the authors has declared the following potential conflict of interest or source of funding: The University of Connecticut Health Center/UConn Musculoskeletal Institute has received direct funding and material support from Arthrex; the company had no influence on the study design, data collection, or interpretation of the results or the final article. K.B. has received consulting fees from Arthrex. R.A.A. has received research support from Arthrex and DePuy and consulting fees from Biorez. A.D.M. has received research support from Arthrex, consulting fees from Arthrex and Astellas Pharma, and honoraria from Arthrosurface. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the University of Connecticut (No. 17-066-3).
References
- 1. Aliberti GM, Kraeutler MJ, Trojan JD, Mulcahey MK. Horizontal instability of the acromioclavicular joint: a systematic review. Am J Sports Med. 2020;48(2):504–510. [DOI] [PubMed] [Google Scholar]
- 2. Baran S, Belisle JG, Granger EK, Tashjian RZ. Functional and radiographic outcomes after allograft anatomic coracoclavicular ligament reconstruction. J Orthop Trauma. 2018;32(4):204–210. [DOI] [PubMed] [Google Scholar]
- 3. Beaton D, Richards R. Assessing the reliability and responsiveness of 5 shoulder questionnaires. J Shoulder Elbow Surg. 1998;7:565–572. [DOI] [PubMed] [Google Scholar]
- 4. Beitzel K, Mazzocca AD, Bak K, et al. ISAKOS Upper Extremity Committee consensus statement on the need for diversification of the Rockwood classification for acromioclavicular joint injuries. Arthroscopy. 2014;30(2):271–278. [DOI] [PubMed] [Google Scholar]
- 5. Beitzel K, Sablan N, Chowaniec DM, et al. Sequential resection of the distal clavicle and its effects on horizontal acromioclavicular joint translation. Am J Sports Med. 2012;40(3):681–685. [DOI] [PubMed] [Google Scholar]
- 6. Berthold DP, Muench LN, Dyrna F, et al. Radiographic alterations in clavicular bone tunnel width following anatomic coracoclavicular ligament reconstruction (ACCR) for chronic acromioclavicular joint injurie. Published online April 25, 2020 Knee Surg Sports Traumatol Arthrosc. doi:10.1007/s00167-020-05980-z. [DOI] [PubMed] [Google Scholar]
- 7. Borbas P, Churchill J, Ek ET. Surgical management of chronic high-grade acromioclavicular joint dislocations: a systematic review. J Shoulder Elbow Surg. 2019;28(10):2031–2038. [DOI] [PubMed] [Google Scholar]
- 8. Branch TP, Burdette HL, Shahriari AS, Carter FM, Hutton WC. The role of the acromioclavicular ligaments and the effect of distal clavicle resection. Am J Sports Med. 1996;24(3):293–297. [DOI] [PubMed] [Google Scholar]
- 9. Carofino BC, Mazzocca AD. The anatomic coracoclavicular ligament reconstruction: surgical technique and indications. J Shoulder Elbow Surg. 2010;19(2 suppl):37–46. [DOI] [PubMed] [Google Scholar]
- 10. Chronopoulos E, Gill HS, Freehill MT, Petersen SA, McFarland EG. Complications after open distal clavicle excision. Clin Orthop Relat Res. 2008;466(3):646–651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Costic RS, Labriola JE, Rodosky MW, Debski RE. Biomechanical rationale for development of anatomical reconstructions of coracoclavicular ligaments after complete acromioclavicular joint dislocations. Am J Sports Med. 2004;32(8):1929–1936. [DOI] [PubMed] [Google Scholar]
- 12. Dyrna F, Berthold DP, Feucht MJ, et al. The importance of biomechanical properties in revision acromioclavicular joint stabilization: a scoping review. Knee Surg Sports Traumatol Arthrosc. 2019;27(12):3844–3855. [DOI] [PubMed] [Google Scholar]
- 13. Dyrna F, de Oliveira CCT, Nowak M, et al. Risk of fracture of the acromion depends on size and orientation of acromial bone tunnels when performing acromioclavicular reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(1):275–284. [DOI] [PubMed] [Google Scholar]
- 14. Dyrna F, Imhoff FB, Haller B, et al. Primary stability of an acromioclavicular joint repair is affected by the type of additional reconstruction of the acromioclavicular capsule. Am J Sports Med. 2018;46(14):3471–3479. [DOI] [PubMed] [Google Scholar]
- 15. Dyrna FGE, Imhoff FB, Voss A, et al. The integrity of the acromioclavicular capsule ensures physiological centering of the acromioclavicular joint under rotational loading. Am J Sports Med. 2018;46(6):1432–1440. [DOI] [PubMed] [Google Scholar]
- 16. Edwards SL, Wilson NA, Flores SE, Koh JL, Zhang L-Q. Arthroscopic distal clavicle resection: a biomechanical analysis of resection length and joint compliance in a cadaveric model. Arthroscopy. 2007;23(12):1278–1284. [DOI] [PubMed] [Google Scholar]
- 17. Fukuda K, Craig E, An K, Cofield R, Chao E. Biomechanical study of the ligamentous system of the acromioclavicular joint. J Bone Joint Surg Am. 1986;68(3):434–440. [PubMed] [Google Scholar]
- 18. Geaney LE, Beitzel K, Chowaniec DM, et al. Graft fixation is highest with anatomic tunnel positioning in acromioclavicular reconstruction. Arthroscopy. 2013;29(3):434–439. [DOI] [PubMed] [Google Scholar]
- 19. Godfrey J, Hamman R, Lowenstein S, Briggs K, Kocher M. Reliability, validity, and responsiveness of the Simple Shoulder Test: psychometric properties by age and injury type. J Shoulder Elbow Surg. 2007;16(3):260–267. [DOI] [PubMed] [Google Scholar]
- 20. Gowd AK, Liu JN, Cabarcas BC, et al. Current concepts in the operative management of acromioclavicular dislocations: a systematic review and meta-analysis of operative techniques. Am J Sports Med. 2019;47(11):2745–2758. [DOI] [PubMed] [Google Scholar]
- 21. Grutter PW, Petersen SA. Anatomical acromioclavicular ligament reconstruction: a biomechanical comparison of reconstructive techniques of the acromioclavicular joint. Am J Sports Med. 2005;33(11):1723–1728. [DOI] [PubMed] [Google Scholar]
- 22. Jordan RW, Malik S, Bentick K, Saithna A. Acromioclavicular joint augmentation at the time of coracoclavicular ligament reconstruction fails to improve functional outcomes despite significantly improved horizontal stability. Knee Surg Sports Traumatol Arthrosc. 2019;27(12):3747–3763. [DOI] [PubMed] [Google Scholar]
- 23. Kany J, Guinand R, Croutzet P. All arthroscopic augmented Vargas procedure: an option after failed acromioclavicular joint dislocation reconstruction. A technical note. Orthop Traumatol Surg Res. 2016;102(5):669–672. [DOI] [PubMed] [Google Scholar]
- 24. Klimkiewicz JJ, Williams GR, Sher JS, Karduna A, Des Jardins JD, Iannotti JP. The acromioclavicular capsule as a restraint to posterior translation of the clavicle: a biomechanical analysis. J Shoulder Elbow Surg. 1999;8(2):119–124. [DOI] [PubMed] [Google Scholar]
- 25. Kraus N, Hann C, Minkus M, Maziak N, Scheibel M. Primary versus revision arthroscopically-assisted acromio- and coracoclavicular stabilization of chronic AC-joint instability. Arch Orthop Trauma Surg. 2019;139(8):1101–1109. [DOI] [PubMed] [Google Scholar]
- 26. Lee SJ, Nicholas SJ, Akizuki KH, McHugh MP, Kremenic IJ, Ben-Avi S. Reconstruction of the coracoclavicular ligaments with tendon grafts: a comparative biomechanical study. Am J Sports Med. 2003;31(5):648–655. [DOI] [PubMed] [Google Scholar]
- 27. Lippitt SB, Harryman DT, Matsen FA. A practical tool for evaluating function: the Simple Shoulder Test In: Matsen FA, Fu FH, Hawkins RJ, eds. The Shoulder: A Balance of Mobility and Stability. American Academy of Orthopaedic Surgeons; 1993:501–518. [Google Scholar]
- 28. Martetschläger F, Horan MP, Warth RJ, Millett PJ. Complications after anatomic fixation and reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2013;41(12):2896–2903. [DOI] [PubMed] [Google Scholar]
- 29. Martetschläger F, Saier T, Weigert A, et al. Effect of coracoid drilling for acromioclavicular joint reconstruction techniques on coracoid fracture risk: a biomechanical study. Arthroscopy. 2016;32(6):982–987. [DOI] [PubMed] [Google Scholar]
- 30. Martetschläger F, Tauber M, Habermeyer P, Hawi N. Arthroscopically assisted acromioclavicular and coracoclavicular ligament reconstruction for chronic acromioclavicular joint instability. Arthrosc Tech. 2016;5(6):e1239–e1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Martin SD, Baumgarten TE, Andrews JR. Arthroscopic resection of the distal aspect of the clavicle with concomitant subacromial decompression. J Bone Joint Surg Am. 2001;83(3):328. [DOI] [PubMed] [Google Scholar]
- 32. Mazzocca AD, Conway JE, Johnson S, et al. The anatomic coracoclavicular ligament reconstruction. Oper Tech Sports Med. 2004;12(1):56–61. [Google Scholar]
- 33. Mazzocca AD, Santangelo SA, Johnson ST, Rios CG, Dumonski ML, Arciero RA. A biomechanical evaluation of an anatomical coracoclavicular ligament reconstruction. Am J Sports Med. 2006;34(2):236–246. [DOI] [PubMed] [Google Scholar]
- 34. Milewski MD, Tompkins M, Giugale JM, Carson EW, Miller MD, Diduch DR. Complications related to anatomic reconstruction of the coracoclavicular ligaments. Am J Sports Med. 2012;40(7):1628–1634. [DOI] [PubMed] [Google Scholar]
- 35. Millett PJ, Horan MP, Warth RJ. Two-year outcomes after primary anatomic coracoclavicular ligament reconstruction. Arthroscopy. 2015;31(10):1962–1973. [DOI] [PubMed] [Google Scholar]
- 36. Moatshe G, Kruckeberg BM, Chahla J, et al. Acromioclavicular and coracoclavicular ligament reconstruction for acromioclavicular joint instability: a systematic review of clinical and radiographic outcomes. Arthroscopy. 2018;34(6):1979–1995.e8. [DOI] [PubMed] [Google Scholar]
- 37. Morikawa D, Dyrna F, Cote MP, et al. Repair of the entire superior acromioclavicular ligament complex best restores posterior translation and rotational stability. Knee Surg Sports Traumatol Arthrosc. 2019;27(12):3764–3770. [DOI] [PubMed] [Google Scholar]
- 38. Muench LN, Kia C, Jerliu A, et al. Functional and radiographic outcomes after anatomic coracoclavicular ligament reconstruction for type III/V acromioclavicular joint injuries. Orthop J Sports Med. 2019;7(11):2325967119884539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Pandhi NG, Esquivel AO, Hanna JD, Lemos DW, Staron JS, Lemos SE. The biomechanical stability of distal clavicle excision versus symmetric acromioclavicular joint resection. Am J Sports Med. 2013;41(2):291–295. [DOI] [PubMed] [Google Scholar]
- 40. Rabalais RD, McCarty E. Surgical treatment of symptomatic acromioclavicular joint problems: a systematic review. Clin Orthop Relat Res. 2007;455:30–37. [DOI] [PubMed] [Google Scholar]
- 41. Richards R, An KN, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347–352. [DOI] [PubMed] [Google Scholar]
- 42. Rockwood CJ, Williams G, Young D. Disorders of the acromioclavicular joint In: Rockwood CA, Matsen FA, III, eds. The Shoulder. Vol 1 WB Saunders; 1998:483–553. [Google Scholar]
- 43. Saier T, Venjakob AJ, Minzlaff P, et al. Value of additional acromioclavicular cerclage for horizontal stability in complete acromioclavicular separation: a biomechanical study. Knee Surg Sports Traumatol Arthrosc. 2015;23(5):1498–1505. [DOI] [PubMed] [Google Scholar]
- 44. Strauss EJ, Barker JU, McGill K, Verma NN. The evaluation and management of failed distal clavicle excision. Sports Med Arthrosc Rev. 2010;18(3):213–219. [DOI] [PubMed] [Google Scholar]
- 45. Tauber M, Eppel M, Resch H. Acromioclavicular reconstruction using autogenous semitendinosus tendon graft: results of revision surgery in chronic cases. J Shoulder Elbow Surg. 2007;16(4):429–433. [DOI] [PubMed] [Google Scholar]
- 46. Tauber M, Valler D, Lichtenberg S, Magosch P, Moroder P, Habermeyer P. Arthroscopic stabilization of chronic acromioclavicular joint dislocations: triple- versus single-bundle reconstruction. Am J Sports Med. 2016;44(2):482–489. [DOI] [PubMed] [Google Scholar]
- 47. Thangaraju S, Cepni S, Magosch P, Tauber M, Habermeyer P, Martetschlager F. Arthroscopically assisted acromioclavicular joint stabilization leads to significant clavicular tunnel widening in the early post-operative period. Knee Surg Sports Traumatol Arthrosc. 2019;27(12):3821–3826. [DOI] [PubMed] [Google Scholar]
- 48. Thangaraju S, Tauber M, Habermeyer P, Martetschlager F. Clavicle and coracoid process periprosthetic fractures as late post-operative complications in arthroscopically assisted acromioclavicular joint stabilization. Knee Surg Sports Traumatol Arthrosc. 2019;27(12):3797–3802. [DOI] [PubMed] [Google Scholar]
- 49. Virk MS, Lederman E, Stevens C, Romeo AA. Coracoid bypass procedure: surgical technique for coracoclavicular reconstruction with coracoid insufficiency. J Shoulder Elbow Surg. 2017;26(4):679–686. [DOI] [PubMed] [Google Scholar]
- 50. Voss A, Beitzel K, Alaee F, et al. A biomechanical analysis of different clavicular tunnel diameters in anatomic acromioclavicular ligament reconstruction. Arthroscopy. 2016;32(8):1551–1557. [DOI] [PubMed] [Google Scholar]
- 51. Williams GN, Gangel TJ, Arciero RA, Uhorchak JM, Taylor DC. Comparison of the Single Assessment Numeric Evaluation method and two shoulder rating scales. Am J Sports Med. 1999;27(2):214–221. [DOI] [PubMed] [Google Scholar]
- 52. Woodmass JM, Esposito JG, Ono Y, et al. Complications following arthroscopic fixation of acromioclavicular separations: a systematic review of the literature. Open Access J Sports Med. 2015;6:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Zanca P. Shoulder pain: involvement of the acromioclavicular joint. (Analysis of 1,000 cases). Am J Roentgenol Radium Ther Nucl Med. 1971;112(3):493–506. [DOI] [PubMed] [Google Scholar]
- 54. Zumstein MA, Schiessl P, Ambuehl B, et al. New quantitative radiographic parameters for vertical and horizontal instability in acromioclavicular joint dislocations. Knee Surg Sports Traumatol Arthrosc. 2018;26(1):125–135. [DOI] [PMC free article] [PubMed] [Google Scholar]