Abstract
Background
The No Action Protocol (NAL) was used to diminish the systematic set-up error. Recently, owing to the development of image registration technologies, the on-line positioning control is more often used. This method significantly reduces the CTV–PTV margin at the expense of the lengthening of a treatment session. The efficiency of NAL in decreasing the total treatment time for Head&Neck patients was investigated.
Methods
Results of set-up control of 30 patients were analyzed. The set-up control was carried out on-line. For each patient and each fraction, the set-error and the time needed for making the set-up control procedure were measured. Next, retrospectively, the NAL was applied to this data. The number of initial errors (without interventions) and after NAL protocol were compared in terms of errors larger than 3 and 4 mm. The average and total time used for portal control was calculated and compared.
Results
The number of setup errors in the posterior-anterior, inferior-superior, and right–left directions ≥3 mm and ≥4 mm were 98, 79, and 91 sessions and 44, 38 and 30 sessions out of 884 sessions. After NAL protocol the number of errors ≥3 mm and ≥4 mm decreased to 84, 57, and 39 sessions and 31, 15 and 10 sessions, respectively. The average time needed for one set-up control was 5.1 min. NAL protocol allows saving 4049 min for the whole group.
Conclusions
For locations where the random set-up errors are small, the NAL enables a very precise treatment of patients. Implementation of this protocol significantly decreases the total treatment time.
Keywords: Set-Up control, Head and neck, No action protocol, Treatment time
1. Introduction
Setup control is the key issue for safe and efficient external beam radiotherapy. Dosimetric errors, if noticed at an early stage of fractionated therapy, may be corrected. Setup errors, especially larger than the Clinical Target Volume – Planning Target Volume margin cannot be corrected in most situations. 1,2,3,4 Considerable technological changes to treatment linear accelerators have resulted in major changes of the setup control procedures. 5, 6, 7, 8, 9, 10, 11, 12
Today, all accelerators are equipped with electronic portal imaging devices, which makes portal control much easier. For accelerators equipped with an additional kV X-Rays source of radiation, the quality of portal images is very good. This equipment is also used for performing cone beam computed tomography, thus providing three-dimensional image information. A comparison of images collected just before, or even during the treatment session, becomes possible, also with ultrasound systems. The sophisticated software allows, with minimal intervention from the user, the matching of the planning and setup images, and this in turn illustrates the setup error. These solutions have resulted in more frequent performance of the on-line setup control. In each fraction, the setup control is performed and, if needed, the position of the patient is corrected before the start of irradiation. Certainly, this procedure makes the irradiation more accurate, but is that always rational and needed? From the geometrical point of view, the high quality of irradiation requires that systematic errors are minimized 13 For many years, in order to reduce the systematic error, the No Action Level (NAL), the extended NAL or the Shrinking Action Level protocols were widely used. 14, 15, 16 The implementation of the NAL protocol allows efficient minimization of the systematic error, at least for patients for whom small random errors were observed. According to this protocol, during the first three fractions (it may be more fractions), the setup errors are measured. These values were used to estimate the systematic error. In subsequent fractions, prior to irradiation, the position of the patient is corrected for the estimated systematic set-up error, by a couch shift. Due to random errors, the systematic error was not fully corrected. The residual error of about σ/√N remains, where σ is the random error and N is the number of images taken to estimate the systematic error. In Head&Neck (HN) patients, due to good immobilization obtained with thermoplastic masks, the NAL protocol might be very efficient. In our center the on-line setup verification protocol has been implemented. In this paper, we analyze the on-line setup control results for 30 H N patients. The aim of the work is to analyze the efficiency of the NAL protocol for the HN patients in terms of the number of set-up errors larger than a given value and in terms of the time needed to perform the on-line and NAL protocols. The time of performing the NAL is compared with the total time of on-line setup control.
2. Materials and methods
2.1. Treatment preparation
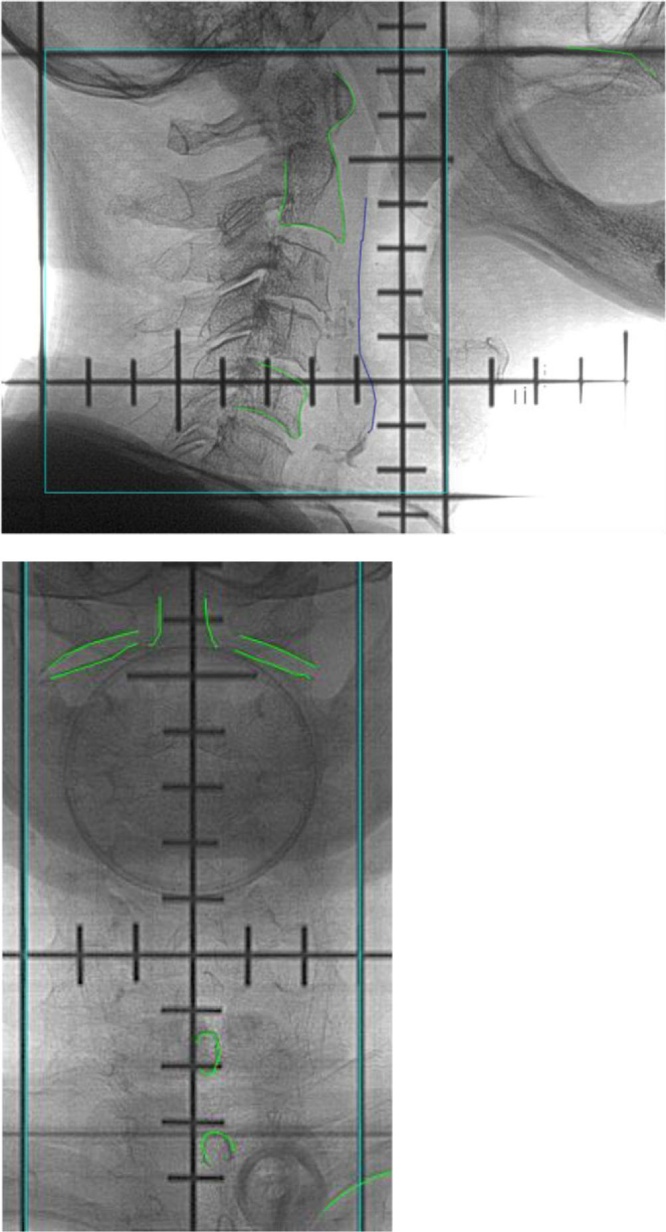
The analysis was carried out for 30 H N patients treated in our center. These were patients with nasopharyngeal and larynx cancer. For each patient a customized 5-point head, neck and shoulders thermoplastic mask (Orfit Industries, Belgium) was made. In addition, a standard, but individually chosen, head support was used. All patients underwent a planning CT scan with 2 mm slice thickness. The scanned region was the PTV plus about 5 cm cranially and caudally. The central axes (three small crosses) were marked on the mask. All the images were sent to the contouring station for target and critical structures delineation. For each patient, an IMRT or VMAT plan was prepared. For almost all patients, the integrated simultaneous boost technique was used. The isotropic margin CTV-PTV of 3–4 mm was always added. The Digitally Reconstructed Radiographs (DRR) are prepared for vertical and lateral position of the gantry. On each DRR, before start of the treatment, the contours of stable anatomical structures were drawn. The anatomical structures used for matching are shown in Fig. 1. During the treatment, the setup position of the patient was accomplished by aligning the lasers with the points marked on the masks. If needed, the position of the isocenter was achieved by treatment couch shifts.
Fig. 1.
Digitally Reconstructed Radiographs, AP and lateral, with edges of anatomical structures used for matching. Edges in green (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article).
Setup control
Patients were irradiated up to a total dose of 68–72 Gy with the fraction dose of 2.2–2.6 Gy (26–31 fractions) on Varian Clinac 2300CD or TrueBeam accelerators. Patients were first positioned by aligning the lasers to the respective shell markings. If needed, couch shifts were applied. Next, the setup control started. It was carried out daily. Two perpendicular portals, the anterior posterior and lateral one were made and matched to the DRRs. The positioning error was obtained for three directions: anterior-posterior (AP), cranial-caudal (CC), left-right (LR). Also, the rotational error was measured. If the setup error was > 5 mm for any direction, the patient setup was restarted. If the error was ≥ 3 mm but ≤ 5 mm for any direction, the position of the patient was corrected by means of the couch shift. For longitudinal direction, the error was calculated as the average value of errors obtained from the vertical and lateral portals. If the position of a patient was corrected, additional portal verification of a patient setup was always carried out and the correctness of the position was verified. The results of the verification procedure were described in terms of systematic and random errors for the three axes separately. The rotational errors were very small, so we do not present this data. After completing the irradiation, the matching of images was checked off-line by very experienced radiation technologists. These results are presented in this work. The total time of the entire setup control was measured (from the beginning of making portal images to the start of treatment). For each patient, the data are presented as the mean of these values over all the treatment sessions.
2.2. NAL protocol simulation
Using the data collected for these 30 patients, we simulated the NAL protocol. The systematic error was estimated from the first three fractions. It has been assumed that the systematic errors ≥ 2 mm were always corrected. To describe the result of implementation of the NAL protocol for each direction and each patient separately, the number of errors larger than 3 and 4 mm were obtained. The total time saved after the NAL protocol was calculated. The average time devoted to making the portal control in the first three fractions was subtracted from the total time. The results for the NAL protocol was compared with the raw data (the initial setup error). Additionally, values of systematic and random setup errors were calculated. The definitions of systematic and random errors proposed Bijhold and de Boer were used. 17,18
3. Results
In Table 1, the setup errors before and after applying the NAL protocol in terms of the number of errors larger than 3 and 4 mm for each patient and each direction are presented. The percentages of errors ≥ 3 and ≥ 4 mm are given in relation to all fraction numbers. Results revealed that the worst results were obtained for the vertical direction. After NAL correction, there is 3.5% of errors larger than 4 mm. This is two times larger than for the Cranial-Caudal and Left-Right directions. Anyway, the 3.5% gives on average the error larger than 4 mm in less than 1 treatment session during the entire treatment, i.e. 30 fractions. For two other directions it is less than 2%, that is only little more than 1 error per 60 fractions. The average time needed to perform the portal control in each fraction was 5.1 min.
Table 1.
Number of set-up errors for each individual patients after applying the No Action Level protocol. The percentage of errors ≥ 3 mm and ≥ 4 mm are given in relation to all fractions. The total number of fractions was 886. AP – Anterior-Posterior, CC – Cranial-Caudal, LR –Left-Right.
| before NAL |
||||||
|---|---|---|---|---|---|---|
| AP | CC | LR | AP | CC | LR | |
| ≥ 3 mm | ≥ 3 mm | ≥ 3 mm | ≥ 4 mm | ≥ 4 mm | ≥ 4 mm | |
| 98 | 79 | 91 | 44 | 38 | 30 | |
| % of fractions | 11.1% | 8.9% | 10.3% | 5.0% | 4.3% | 3.4% |
| after NAL | ||||||
| AP | CC | LR | AP | CC | LR | |
| Patients number | ≥ 3 mm | ≥ 3 mm | ≥ 3 mm | ≥ 4 mm | ≥ 4 mm | ≥ 4 mm |
| Total (886) | 84 | 57 | 39 | 31 | 15 | 10 |
| % of fractions | 9.5% | 6.4% | 4.4% | 3.5% | 1.7% | 1.1% |
4. Discussion
Today, the setup control can be carried out quite easily. Therefore, various protocols of setup correction have been often replaced by the on-line protocol. This method of control is also motivated by the fact that the on-line protocol is the only one which is able to minimize both the systematic and random errors. Such an attitude is certainly valid for patient groups in which quite large random errors are expected. However, the decision on which protocol is the most effective should be analyzed carefully. Piotrowski et al. analyzed the set-up accuracy and time consumption of four different image-guidance protocols for prostate patients. 19 He showed that limited number of setup control might be the effective way to diminish the systematic component of the set-up error. The aim of this work is to check if the NAL protocol is effective for HN patients. This hypothesis was based on the method of immobilization used for these patients. These patients were immobilized with a thermoplastic mask, which ensures a good reproducibility of the position. Recently, numerous works have been published with the results of setup errors in the head and neck region. 20, 21, 22, 23, 24 The population systematic and random setup errors were usually smaller than 2.0 mm. We obtained similar results. The population systematic errors for AP, CC and LR directions were 1.2, 2.0 and 1.2 mm, respectively. The population random errors for AP, CC and LR directions were 1.4, 1.3 and 1.4 cm, respectively. The CTV-PTV margin calculated according to Marcel van Herk formulae is 4.0, 6.0, and 4.0 mm for AP, CC and LR direction, respectively. After implementation of the modified NAL protocol (during the first treatment sessions the position of a patient is corrected if error ≥ 3 mm) the residual population systematic errors for AP, CC and LR directions were 0.8, 0.5 and 0.8 mm, respectively. The CTV-PTV margin would be 3.0, 2.2, and 3.0 mm.
Is it worth controlling the position of a patient in every fraction? The precision of irradiation with on-line control is better than for NAL protocol, but only slightly. After NAL correction, positioning errors larger than 3 mm were observed in 9.5%, 6.4% and 4.4% of fractions for the AP, CC and LR directions, respectively. Errors larger than 4 mm occurred in 3.5% (31 fractions), 1.7% (15 fractions) and 1.1% (10 fractions) of all 884 fractions for the AP, IS and RL directions, respectively. For 7 patients, the largest error was ≥ 7 mm. For 17 patients the largest error was never larger than 5 mm. On the other hand, making portals in each treatment session is quite time consuming. Making one portal control took, on average, 5.1 min. For all 30 patients, the on-line portal control procedure lasted 2,432 min. If the NAL protocol were to be used, the total time needed for the control would be just 459 min. The time needed for the correction to the patient’s initial position with the vector calculated according to NAL protocol is shorter than 1 min. According to the modified NAL protocol used in our center, only errors of 2 mm or larger are corrected. Such corrections were present for 26 out of 30 patients. Still, the time saved after NAL procedure would be huge – about 4,049 min. Assuming that the time slot for one fraction is 15 min, this saved time would enable to deliver about 270 fractions more, which is the time needed to irradiate 9 additional patients (30 fractions for one treatment).
In this work, we did not analyze the rotations and local distortions of the patients. Very seldom rotations larger than 1 degree were observed. The distortions which led to larger misalignment of portal and reference images at some part of the irradiated volume were sometimes present. Especially for nasopharynx patients for whom the length of the PTV was long, larger misalignment of anatomical structures was observed close to the cranial-caudal edges of the portals. According to our protocol, the best match of portal and reference images should be obtained in the CTV region, which is usually in the center of the fields. Such policy is followed due to the fact that recurrences are most often observed in the region of the highest dose (Gross Tumor Volume) 25. For a few patients, the time trend of errors was observed. For these patients the extended No Action Level protocol might give a better result. 15 However, as we showed, the number of errors larger than 4 mm was very low.
Although the NAL protocol has been shown as very effective, it should be noted that, especially in the group treated with chemoradiotherapy, some anatomy changes are observed during radiotherapy. 26 The anatomy changes are not visible on portal images. These changes can be visualized with the Cone Beam Computed Tomography. However, the unambiguous conclusions on when the new set of CT images should be acquired were obtained. Therefore, several authors propose that CBCT should be performed once a week. It allows to implement the extended No Action Level Protocol or just to check the effectiveness of the NAL. Additionally, in case of large changes of anatomy the new plan may be prepared.
5. Conclusions
For the head and neck patients the NAL protocol was very effective in set-up control. Application of this protocol allows to decrease the average treatment time of a session by more than 4 min.
6. Conflictofinterest
None.
7. Financial disclosure
None.
References
- 1.Hurkmans C.W., Remeijer P., Lebesque J.V. Set-up verification using portal imaging : Review of current cliical practice. Radiother Oncol. 2001;115:-120. doi: 10.1016/s0167-8140(00)00260-7. [DOI] [PubMed] [Google Scholar]
- 2.Geometric Uncertainties in radiotherapy, Definingthe Planning Target Volume . 2003. The british institute of radiology. [Google Scholar]
- 3.Ferreira S., Bonnarens E., Sá A.C., Fermento S.A.C., Neves D. Radiotherapy setup displacements in breast cancer patients: 3D surface imaging experience. Rep Pract Oncol Radiother. 2018;23(1):61–67. doi: 10.1016/j.rpor.2017.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anjanappa M., Rafi M., Bhasi S., Kumar R., Thommachan K.C., Tapesh B. Setup uncertainties and PTV margins at different anatomical levels in intensity modulated radiotherapy for nasopharyngeal cancer. XXX. 2017;22(5):396–401. doi: 10.1016/j.rpor.2017.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Langen K.M., Pouliot Anzinos C. Evaluation of ultrasound-based prostate localization for image-guided radiotherapy. Int J RadiatOncol Biol Phys. 2003;57(3):635–644. doi: 10.1016/s0360-3016(03)00633-3. [DOI] [PubMed] [Google Scholar]
- 6.Lawrence G., Dickson S. Linac with in-room CT: Technical issues and clinical implementation. Radiother Oncol. 2005;76(S2):S4. [Google Scholar]
- 7.McBain C.A., Henry A.M., Sykes J. X-ray volumetric imaging in image-guided radiotherapy: The new standard in on-treatment imaging. Int Radiat Oncol Biol Phys. 2006;64:2. doi: 10.1016/j.ijrobp.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 8.Bert C., Metheany K.G., Doppke K.P. Clinical experience with 3D surface patients setup system for alignmenet of partial-breast irradiation patients. Int Radiat Oncol Biol Phys. 2006;64(4):1265–1274. doi: 10.1016/j.ijrobp.2005.11.008. [DOI] [PubMed] [Google Scholar]
- 9.Kirby M.C., Glendinning A.G. Developments in electronic portal imaging systems. Br J Radiol. 2006;79(Spec No 1):S50–65. doi: 10.1259/bjr/21517185. [DOI] [PubMed] [Google Scholar]
- 10.Jin J.Y., Yin F.F., Tenn S.E., Medin P.M., Solberg T.D. Use of the BrainLAB ExacTrac X-Ray 6D system in image-guided radiotherapy. Med Dosim. 2008;33(2):124–134. doi: 10.1016/j.meddos.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 11.Collen C., Engels B., Duchateau M. Volumetric imaging by megavoltage computed tomography for assessment of internal organ motion during radiotherapy for cervical cancer. Int J Radiat Oncol Biol Phys. 2010;77(5):1590–1595. doi: 10.1016/j.ijrobp.2009.10.021. [DOI] [PubMed] [Google Scholar]
- 12.Camps Saskia M., Fontanarosa Davide, de With Peter H.N. The use of ultrasound imaging in the external beam radiotherapy workflow of prostate Cancer patients. Biomed Res Int. 2018 doi: 10.1155/2018/7569590. DOI: org/10.1155/2018/7569590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Herk M. Errors and margins in radiotherapy. Semin Radiat Oncol. 2004;14(1):52–64. doi: 10.1053/j.semradonc.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 14.de Boer H.C., Heijmen B.J. A protocol for reduction of systematic patient errors with minimal portal imaging workload. Int J Radiat Oncol Biol Phys. 2001;50(5):1350–1365. doi: 10.1016/s0360-3016(01)01624-8. [DOI] [PubMed] [Google Scholar]
- 15.de Boer H.C., Heijmen B.J. eNAL: An extension of the NAL setup correction protocol for effective use of weekly follow-up measurements. Int J Radiat Oncol Biol Phys. 2007;67(5):1586–1595. doi: 10.1016/j.ijrobp.2006.11.050. [DOI] [PubMed] [Google Scholar]
- 16.Bel A., van Herk M., Bartelink H., Lebesque J.V. A verification procedure to improve patient set-up accuracy using portal images. Radiother Oncol. 1993;29:253–260. doi: 10.1016/0167-8140(93)90255-7. [DOI] [PubMed] [Google Scholar]
- 17.Bijhold J., Lebesque J.V., Hart A.A.M., Vijlbrief R.E. Maximizing setup accuracy using portal images as applied to a conformal boost technique for prostatic cancer. Radiother Oncol. 1992;24:261–271. doi: 10.1016/0167-8140(92)90233-k. [DOI] [PubMed] [Google Scholar]
- 18.de Boer H.C., van Sornsen de Koste J.R., Senan S., Visser A.G., Heijmen B.J. Analysis and reduction of 3D systematic and random set-up errors during the simulation and treatment of lung cancer patients with CT-based external beam radiotherapy dose planning. Int J Radiat Oncol Biol Phys. 2001;49:857–868. doi: 10.1016/s0360-3016(00)01413-9. [DOI] [PubMed] [Google Scholar]
- 19.Piotrowski T., Kaczmarek K., Bajon T., Ryczkowski A., Jodda A., Kaźmierska J. Evaluation of image-guidance strategies for prostate cancer. Technol Cancer Res Treat. 2014;13:583–591. doi: 10.7785/tcrtexpress.2013.600258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lai Y.-L., Yang S.-N., Liang J.-A., Wang J.-C., Yu C-Y Su C.-H., Chen S.-W. Impact of body-mass factors on setup displacement in patients with head and neck cancer treated with radiotherapy using daily on-line image guidance. Radiat Oncol. 2014;9:19. doi: 10.1186/1748-717X-9-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Contesini M., Guberti M., Saccani R., Braglia L., Iotti C. Setup errors in patients with head-neck cancer (HNC), treated using the Intensity modulated Radiation Therapy (IMRT) technique: How it influences the customised immobilisation systems, patient’s pain and anxiety. Radiat Oncol. 2017;12:72. doi: 10.1186/s13014-017-0807-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moore S.J., Herst P.H., Louwe R.J.W. Review of the patient positioning reproducibility in head-and-neck radiotherapy using Statistical process Control. Radiother Oncol. 2018;127:183–189. doi: 10.1016/j.radonc.2018.01.006. [DOI] [PubMed] [Google Scholar]
- 23.Delishaj D., Ursino S., Pasqualetti F., Matteucci F., Cristaudo A. Set-up errors in heand and neck cancer treated with IMRT technique assessed by cone-beam computed tomography: A feasible protocol. Radiat Oncol J. 2018;36(1):54–62. doi: 10.3857/roj.2017.00493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang H., Wang C., Tung S., Dimmitt A.W., Wong P.F. Improved setup and positioning accuracy using a three-point customized cushion/mask/bite-block immobilization system for stereotactic reirradiation of head and neck cancer. J Appl Clinic Med Phys. 2016;17(3):180–189. doi: 10.1120/jacmp.v17i3.6038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mohamed A.S.R., Cardenas C.E., Garden A.S. Patterns-of-failure guided biological target volume definition for head and neck cancer patients: FDG-PET and dosimetric analysis of dose escalation candidate subregions. Radiother Oncol. 2017;124:248–255. doi: 10.1016/j.radonc.2017.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brouwer C.L., Steenbakkers R.J.H.M., Langendijk A.J., Sijtsema N.M. Identifying patients who may benefit from adaptive radiotherapy: Doesthe literature on anatomic and dosimetric changes in head and neckorgans at risk during radiotherapy provide information to help? Radiother Oncol. 2015;115:285–294. doi: 10.1016/j.radonc.2015.05.018. [DOI] [PubMed] [Google Scholar]