Abstract
Background
While recent reports suggest that people with disabilities (PwDs) are likely to be adversely impacted by COVID-19 and face multiple challenges, previous research has not examined if COVID-19 burdens are unequally distributed with respect to the disability characteristics of the U.S. population.
Objective
This article presents the first national scale study of the relationship between COVID-19 incidence and disability characteristics in the U.S. The objective is to determine whether COVID-19 incidence is significantly greater in counties containing higher percentages of socio-demographically disadvantaged PwDs, based on race, ethnicity, poverty status, age, and biological sex.
Methods
This study integrates county-level data on confirmed COVID-19 cases from the Johns Hopkins Center for Systems Science and Engineering database with multiple disability variables from the 2018 American Community Survey. Statistical analyses are based on bivariate correlations and multivariate generalized estimating equations that consider spatial clustering in the data.
Results
Greater COVID-19 incidence rate is significantly associated with: (1) higher percentages of PwDs who are Black, Asian, Hispanic, Native American, below poverty, under 18 years of age, and female; and (2) lower percentages of PwDs who are non-Hispanic White, above poverty, aged 65 or more years, and male, after controlling for spatial clustering.
Conclusions
Socio-demographically disadvantaged PwDs are significantly overrepresented in counties with higher COVID-19 incidence compared to other PwDs. These findings represent an important starting point for more detailed investigation of the disproportionate impacts of COVID-19 on PwDs and highlight the urgent need for COVID-19 data collection systems to incorporate disability information.
Keywords: COVID-19, Disability, Intra-categorical analysis, Race/ethnicity, Poverty
Introduction
People with disabilities (PwDs) represent a rapidly expanding and diverse group, with almost 25% of adult Americans reporting some type of disability.1 Recent reports suggest that PwDs are likely to be adversely impacted by the COVID-19 pandemic and face multiple challenges.2, 3, 4, 5, 6 The first barrier involves adopting recommended public health guidelines and practicing routine prevention measures (e.g., social distancing and washing hands) that do not consider the needs of PwDs, especially those relying on assistance with personal care. Second, equitable access to health care, a well-documented barrier for PwDs, has worsened during this pandemic.7 Medical resource allocation, including ventilators, may also be discriminatory against patients with disabilities, and complaints have been filed in several states about these rationing policies.5 Third, PwDs often have difficulty communicating symptoms of illness, resulting in delays in diagnosis and additional virus spread.3 Finally, PwDs are more likely to have underlying health problems and reside in congregate settings than those without disabilities, thus increasing their infection risks.5 , 8 , 9
While recent studies have documented greater COVID-19 incidence and fatality rates in U.S. counties containing higher proportions of non-White and socioeconomically disadvantaged residents,10, 11, 12 research on the socio-spatial distribution of COVID-19 burdens has paid limited attention to PwDs. To address this gap, this article presents the first national scale study of the relationship between confirmed COVID-19 cases and disability characteristics in the U.S. The specific objective is to determine whether COVID-19 incidence is significantly greater in counties containing higher percentages of socio-demographically disadvantaged PwDs, based on their race, ethnicity, poverty status, age, and biological sex.
Methods
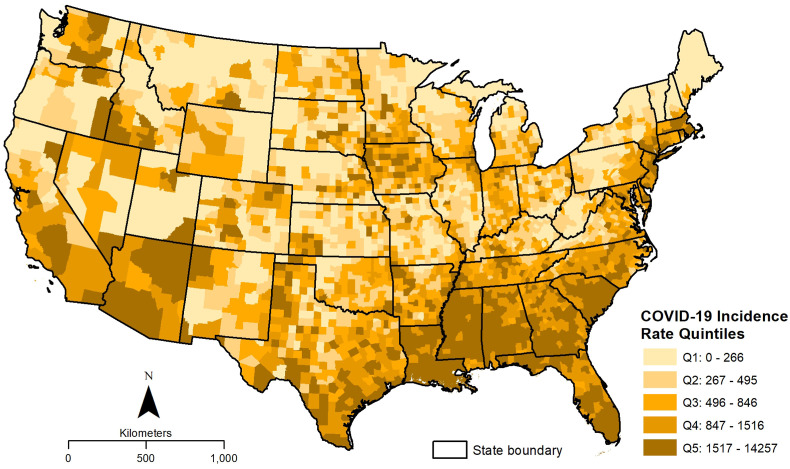
Data on COVID-19 incidence were retrieved from the Johns Hopkins University Center for Systems Science and Engineering database13 on August 1, 2020, for all counties in the continental U.S. This repository provides the most comprehensive and latest county-level COVID-19 data reported by the Centers for Disease Control and Prevention and state health departments, updated daily. The total number of COVID-19 cases in the 3108 counties of the continental U.S. (which excludes Alaska, Hawaii, and Puerto Rico) was 4,483,338 on the date this information was downloaded. The COVID-19 incidence rate, estimated as the number of confirmed cases per 100,000 people in each county, was used as the dependent variable for this study. The spatial distribution of this variable is depicted in Fig. 1 , where counties in the continental U.S. are classified into five quintiles based on the COVID-19 incidence rate. Summary statistics for this dependent variable are included in the first row of Table 1 .
Fig. 1.
County level distribution of COVID-19 incidence rate (cases per 100,000 people) in the continental USA, August 1, 2020.
Table 1.
Summary statistics for variables analyzed and bivariate correlations with county COVID-19 incidence rate.
| Min | Max | Mean | SD | Pearson’s r | |
|---|---|---|---|---|---|
| COVID-19 incidence rate (confirmed cases per 100,000 people) | 0.00 | 14,257 | 967 | 1004 | |
| Percent1 with a disability | 3.83 | 33.71 | 15.95 | 4.40 | −0.056∗∗ |
| Race: | |||||
| Percent w/disability: White alone | 0.85 | 33.26 | 13.55 | 4.63 | −0.326∗∗ |
| Percent w/disability: Black alone | 0.00 | 20.70 | 1.48 | 2.66 | 0.456∗∗ |
| Percent w/disability: Native American | 0.00 | 13.74 | 0.28 | 0.94 | 0.020 |
| Percent w/disability: Asian alone | 0.00 | 3.45 | 0.09 | 0.18 | 0.097∗∗ |
| Percent w/disability: Other race | 0.00 | 15.24 | 0.55 | 0.65 | 0.028 |
| Ethnicity: | |||||
| Percent w/disability: Non-Hispanic White | 0.10 | 33.16 | 12.84 | 4.81 | −0.355∗∗ |
| Percent w/disability: Hispanic | 0.00 | 25.26 | 0.99 | 2.15 | 0.119∗∗ |
| Percent w/disability: Non-Hispanic non-White | 0.00 | 20.93 | 2.13 | 2.75 | 0.439∗∗ |
| Poverty status: | |||||
| Percent w/disability: Below poverty level | 0.00 | 14.97 | 3.57 | 1.85 | 0.108∗∗ |
| Percent w/disability: Above poverty level | 0.00 | 27.30 | 12.48 | 3.06 | −0.146∗∗ |
| Age: | |||||
| Percent w/disability: Age 5–17 years | 0.00 | 5.08 | 1.03 | 0.48 | 0.083∗∗ |
| Percent w/disability: Age 18–34 years | 0.00 | 5.59 | 1.56 | 0.67 | 0.066∗ |
| Percent w/disability: Age 35–64 years | 1.01 | 18.36 | 6.35 | 2.30 | −0.005 |
| Percent w/disability: Age 65–74 years | 0.00 | 12.73 | 3.09 | 1.16 | −0.089∗∗ |
| Percent w/disability: Age 75 years or more | 0.00 | 11.13 | 3.87 | 1.19 | −0.181∗∗ |
| Biological Sex: | |||||
| Percent w/disability: Male | 1.30 | 18.19 | 8.06 | 2.37 | −0.131∗∗ |
| Percent w/disability: Female | 1.91 | 19.94 | 7.90 | 2.26 | 0.028 |
1Disabilty percentages are based on the civilian noninstitutionalized population.
∗∗p < 0.01; ∗p < 0.05; n = 3108 counties.
Data on disability characteristics were obtained from the 2018 American Community Survey (ACS) five-year estimates. The ACS defines PwDs as members of the civilian non-institutionalized population who reported having serious self-care, hearing, vision, independent living, ambulatory, and/or cognitive difficulties on the ACS form. The ACS disability estimates allow disaggregation of PwDs based on five socio-demographic categories (race, ethnicity, poverty status, age, and biological sex) that were used for this intra-categorical analysis. County percentages for each disability subgroup were calculated by dividing the number of PwDs in each subgroup by the total civilian non-institutionalized population relevant to the variable category. The names and descriptive statistics for these explanatory variables are provided in Table 1.
Bivariate Pearson product-moment correlations were first used to measure statistical associations between COVID-19 incidence rate and each disability variable. Generalized estimating equations (GEEs) were then used for a multivariate analysis of disability subgroups within each socio-demographic category. GEEs extend the generalized linear model to accommodate clustered data,14 in addition to relaxing several assumptions of traditional regression (i.e., normality).
For estimating a GEE, clusters of observations must be defined based on the assumption that observations within a cluster are correlated, while observations from different clusters are independent.15 A combination of two different approaches were utilized to define county clusters for this study. The state in which a county is located was first used to account for potential correlation in counties within the same state, because of similar COVID-19 response and testing policies, socio-cultural systems, and healthcare system characteristics16, 17, 18 that imply similarities in counties within a given state and differences between states. Since the use of states as the only clustering variable potentially ignores intra-state and regional geographic variations in COVID-19 outcomes, a second approach based on identifying significant clusters of COVID-19 cases was incorporated. Specifically, SatScan19 software was used to implement a spatial scan statistic based on the Poisson model, determine spatial clusters, and estimate relative risk (RR) for COVID-19 incidence rates at the county level. A similar methodology was recently employed by Desjardins et al.20 to detect space-time clusters of COVID-19 cases in the continental U.S. The RR is defined as the estimated risk at a given location divided by the risk outside of the location (or, everywhere else). If a county has a RR of 3.0, for example, then the population within that county are three times more likely to be exposed to COVID-19. All U.S. counties were classified into six groups based on the estimated RR values (<1.0, 1.00–1.99, 2.00–2.99, 3.00–3.99, 4.00–4.99, and 5.0 or more). The use of both states (n = 49) and RR groups (n = 6) for the GEE cluster definition resulted in a total of 102 clusters, with the number of counties per cluster ranging from 1 to 245.
GEEs also require the specification of an intra-cluster dependency correlation matrix.15 The ‘exchangeable’ correlation matrix was selected for the results reported here, since this specification yielded the best statistical fit based on the QIC (quasi-likelihood under the independence) model criterion. For each GEE, the normal, gamma, and inverse Gaussian distributions with logarithmic and identity link functions were explored. The gamma distribution with logarithmic link function was chosen for all GEEs since this model specification provided the lowest QIC value.
Since PwDs were disaggregated separately based on five socio-demographic characteristics (i.e., race, ethnicity, poverty status, age, and biological sex), five different GEE models were utilized. Each GEE included all disability subgroups relevant to that socio-demographic category. Finally, potential multicollinearity among the variables was also examined based on variance inflation factor, tolerance, and condition index criteria; inferences from the GEEs are not affected by multicollinearity. All independent variables were standardized before inclusion in the GEE and their statistical significance was estimated using two-tailed p-values from the Wald chi-square test.
Results
Bivariate correlation analysis results are summarized in the rightmost column of Table 1. A relatively weak (r = 0.056) but significantly negative correlation is observed between COVID-19 incidence and the overall disability percentage in the county. COVID-19 incidence is also negatively and significantly correlated with the percentages of PwDs who are White alone, non-Hispanic White, and above poverty, as well as those who are older (65 years or more) and male. However, the percentages of PwDs who are Black alone, Asian alone, Hispanic, non-Hispanic non-White, below poverty, and aged 5–34 years all indicate a positive and significant correlation with COVID-19 incidence.
Results from the multivariate GEEs, shown in Table 2 , are consistent with the bivariate correlations. In the Race model, a significant and positive coefficient is observed only for the percentage of White PwDs, while all other racial (i.e., non-White) subgroups yield significantly negative coefficients. The Ethnicity model shows significantly positive associations for the percentages of Hispanic and non-Hispanic non-White PwDs, but a negative association with non-Hispanic White percentage. The percentage of PwDs below poverty level indicates a significantly positive effect in the Poverty status model, but a significantly negative relationship is observed for the percentage of those above poverty. In the Age model, the percentage of PwDs aged 5–17 years are significantly and positively related to COVID-19 incidence, while those aged 65–74 and 75 years or more reveal a significantly negative association. Finally, the Biological sex model indicates a significant and positive relationship with COVID-19 incidence for the percentage of female PwDs, but a negative relationship for the percentage of male PwDs.
Table 2.
Generalized estimating equations (GEE) for predicting county COVID-19 incidence rate: Standardized model coefficients and significance.
| Beta | Std Error | Lower 95% CI | Upper 95% CI | Wald Chi Square | |
|---|---|---|---|---|---|
| Race: | |||||
| Percent w/disability: White alone | −0.203 | 0.020 | −0.242 | −0.164 | 102.958∗∗ |
| Percent w/disability: Black alone | 0.111 | 0.016 | 0.079 | 0.143 | 46.214∗∗ |
| Percent w/disability: Native American | 0.051 | 0.009 | 0.033 | 0.069 | 31.438∗∗ |
| Percent w/disability: Asian alone | 0.080 | 0.018 | 0.046 | 0.115 | 21.060∗∗ |
| Percent w/disability: Other race | 0.077 | 0.017 | 0.044 | 0.110 | 21.030∗∗ |
| Intercept | 7.160 | 0.083 | 6.997 | 7.322 | 7465.214∗∗ |
| Ethnicity: | |||||
| Percent w/disability: Non-Hispanic White | −0.237 | 0.022 | −0.280 | −0.194 | 116.954∗∗ |
| Percent w/disability: Hispanic | 0.119 | 0.031 | 0.058 | 0.180 | 14.708∗∗ |
| Percent w/disability: Non-Hispanic non-White | 0.118 | 0.0161 | 0.086 | 0.149 | 53.248∗∗ |
| Intercept | 7.186 | 0.083 | 7.023 | 7.348 | 7525.648∗∗ |
| Poverty status: | |||||
| Percent w/disability: Below poverty level | 0.148 | 0.022 | 0.105 | 0.190 | 46.913∗∗ |
| Percent w/disability: Above poverty level | −0.267 | 0.023 | −0.312 | −0.222 | 134.297∗∗ |
| Intercept | 7.183 | 0.072 | 7.043 | 7.324 | 10066.93∗∗ |
| Age: | |||||
| Percent w/disability: Age 5–17 years | 0.047 | 0.016 | 0.016 | 0.078 | 8.732∗∗ |
| Percent w/disability: Age 18–34 years | 0.038 | 0.022 | −0.005 | 0.081 | 3.008 |
| Percent w/disability: Age 35–64 years | −0.026 | 0.023 | −0.071 | 0.019 | 1.300 |
| Percent w/disability: Age 65–74 years | −0.089 | 0.021 | −0.131 | −0.047 | 17.597∗∗ |
| Percent w/disability: Age 75 years or more | −0.108 | 0.020 | −0.148 | −0.069 | 29.479∗∗ |
| Intercept | 7.242 | 0.076 | 7.093 | 7.391 | 9093.179∗∗ |
| Biological Sex: | |||||
| Percent w/disability: Male | −0.298 | 0.0280 | −0.353 | −0.243 | 113.460∗∗ |
| Percent w/disability: Female | 0.153 | 0.0286 | 0.097 | 0.209 | 28.577∗∗ |
| Intercept | 7.223 | 0.072 | 7.081 | 7.365 | 9963.672∗∗ |
Note: All GEEs are based on a gamma distribution with log link function and an exchangeable correlation matrix.
QIC (quasi-likelihood under the independence model criterion) = 2582.53 (Race model), 2586.55 (Ethnicity model), 2801.46 (Poverty status model), 2978.737 (Age model), and 2892.35 (Biological Sex model).
∗∗p < 0.01; ∗p < 0.05; CI = confidence interval; n = 3059 counties (cases>0).
Discussion
Although the overall disability percentage is negatively associated with confirmed COVID-19 cases, intra-categorical analysis reveals that socio-demographically disadvantaged PwDs are significantly overrepresented in counties with higher COVID-19 incidence, after controlling for spatial clustering. Specifically, PwDs who are Black, Asian, Hispanic, Native American, below poverty, aged 5–17 years, and female are significantly more likely to reside in counties with higher COVID-19 incidence compared to their counterpart socio-demographic subgroups. However, PwDs who are White alone, non-Hispanic White, above poverty, aged 65 years or more, and male are significantly less likely to reside in counties with higher COVID-19 incidence compared to their counterpart subgroups. This suggests that PwDs are experiencing a ‘multiple jeopardy’ based on the convergence of their disability, racial/ethnic minority, and poverty status,21 that is potentially amplified by higher COVID-19 prevalence in their counties. For those under 18 years, the results align with a recent study that found higher concentrations of COVID-19 cases for younger patients with intellectual and developmental disabilities.22 The significantly higher proportion of female PwDs in counties with greater COVID-19 is also a major concern, since women with disabilities have been documented to face more discrimination and difficulties in attaining access to education, employment, housing, and healthcare, as well as higher risks of gender-based violence and sexual abuse.23 , 24 The findings imply that socio-demographically disadvantaged PwDs residing in areas of higher COVID-19 exposure are likely to suffer increased infection risks and various additional burdens that require further attention within public health research and intervention efforts.
While this study represents an important starting point for documenting the unequal impacts of COVID-19 on PwDs, it is important to consider three limitations. First, disability data from the ACS is limited to six types of difficulties, does not allow identification of prevalent health conditions (e.g., cancer or paralysis), and excludes factors that potentially contribute to disability such as discrimination and lack of reasonable accommodations.25 Second, statistical analyses are restricted to county-level associations since COVID-19-related disability information for smaller geographic units or individual cases are currently unavailable. Third, while this county level GEE analysis utilizes states and significance of COVID-19 risks to define spatial clusters, data on additional factors that influence COVID-19 variability such as testing protocols, access, and availability should be incorporated in future work. Despite these limitations, the findings emphasize the need for COVID-19 data collection and surveillance systems to incorporate disability identifiers, in addition to existing indicators of age, race/ethnicity, and gender. To understand and address the needs of PwDs affected by this pandemic, more detailed information is urgently needed on rates of infections, hospitalizations, outcomes, and fatalities, disaggregated by types of difficulty experienced by PwDs as well as their demographic and socioeconomic characteristics.
Conclusions
This study examined the disproportionate effects of COVID-19 on PwDs by analyzing county-level associations between COVID-19 incidence rate and disability characteristics in the continental U.S. Results revealed that PwDs who are racial/ethnic minority, below poverty, aged 5–17 years, and female are significantly overrepresented in counties with higher COVID-19 incidence, while PDWs who are White, above poverty, and aged 65 or more years are significantly underrepresented. These intra-categorical inequalities highlight the need for additional data and analysis to document the adverse impacts of this pandemic on physically and socially vulnerable PwDs, as well as formulate appropriate intervention strategies.
Funding
This research is funded, in part, by the Geospatial Fellows program supported by the U.S. National Science Foundation (NSF) under grant number 1743184.
Disclaimer
Any opinions, findings, and conclusions or recommendations expressed in this article are those of the author and do not necessarily reflect the views of NSF.
Conflict of interest
The author has no conflicts of interest or disclosures to report.
References
- 1.Okoro C.A., Hollis N.D., Cyrus A.C., Griffin-Blake S. Prevalence of disabilities and health care access by disability status and type among adults -- United States, 2016. Morb Mortal Wkly Rep. 2018;67:882e887. doi: 10.15585/mmwr.mm6732a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turk M.A., McDermott S. The Covid-19 pandemic and people with disability. Disabil Health J. 2020;13 doi: 10.1016/j.dhjo.2020.100944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boyle C.A., Fox M.H., Havercamp S.M. The public health response to the COVID-19 pandemic for people with disabilities. Disabil Health J. 2020;13 doi: 10.1016/j.dhjo.2020.100943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pineda S.V., Corburn J. Disability, urban health equity, and the coronavirus pandemic: promoting cities for all. J Urban Health. 2020;97:336–341. doi: 10.1007/s11524-020-00437-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hub Staff Report, John Hopkins University COVID-19 poses unique challenges for people with disabilities. 2020. https://hub.jhu.edu/2020/04/23/how-covid-19-affects-people-with-disabilities/ Available at:
- 6.World Health Organization (WHO) Disability considerations during the COVID-19 outbreak. 2020. https://www.who.int/who-documents-detail/disability-considerations-during-the-covid-19-outbreak Available at:
- 7.Pendo E. COVID-19 and disability-based discrimination in health care. 2020. https://www.americanbar.org/groups/diversity/disabilityrights/resources/covid19-disability-discrimination/ Available at:
- 8.Centers for Disease Control and Prevention (CDC) COVID-19 Response Team Preliminary estimates of the prevalence of selected underlying health conditions among patients with coronavirus disease 2019 -- United States, February 12-March 28, 2020. Morb Mortal Wkly Rep. 2020;69:382e386. doi: 10.15585/mmwr.mm6913e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Landes S.D., Turk M.A., Formica M.K., McDonald K.E., Stevens J.D. COVID-19 outcomes among people with intellectual and developmental disability living in residential group homes in New York State. Disabil Health J. 2020 doi: 10.1016/j.dhjo.2020.100969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahajan U.V., Larkins-Pettigrew K. Racial demographics and COVID-19 confirmed cases and deaths: a correlational analysis of 2886 US counties. J Public Health. 2020 doi: 10.1093/pubmed/fdaa070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Finch W.H., Hernández Finch M. Poverty and Covid-19: rates of incidence and deaths in the United States during the first 10 weeks of the pandemic. Front Soc. 2020;5:47. doi: 10.3389/fsoc.2020.00047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Karaye I.M., Horney J. The impact of social vulnerability on COVID-19 in the U.S.: an analysis of spatially varying relationships. Am J Prev Med. 2020;59(3):317–325. doi: 10.1016/j.amepre.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Center for Systems Science and Engineering (CSSE) Johns Hopkins university. COVID-19 cases U.S. https://www.arcgis.com/home/user.html?user=CSSE_GISandData Available at:
- 14.Nelder J., Wedderburn R. Generalized linear models. J Royal Stat Soc Ser A. 1972;135:370–384. [Google Scholar]
- 15.Garson G. Statistical Associates Publishing; Asheboro, NC: 2012. Generalized Linear Models and Generalized Estimating Equations. [Google Scholar]
- 16.Wu X., Nethery R.C., Sabath M.C., Braun D., Dominici F. Exposure to air pollution and COVID-19 mortality in the United States. 2020. https://www.medrxiv.org/content/10.1101/2020.04.05.20054502v2 Available at: [DOI] [PMC free article] [PubMed]
- 17.Lye W. Community use of face masks and COVID-19: evidence from a natural experiment of state mandates in the US. Health Aff. 2020;39 doi: 10.1377/hlthaff.2020.00818. https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2020.00818 [DOI] [PubMed] [Google Scholar]
- 18.Montez J.K., Beckfield J., Cooney J.K., Grumbach J.M., Hayward M.D. US state policies, politics, and life expectancy. Milbank Q. 2020 doi: 10.1111/1468-0009.12469. https://onlinelibrary.wiley.com/doi/full/10.1111/1468-0009.12469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kulldorff M. SaTScanTM user guide for version 9.6. 2018. https://www.satscan.org Available at:
- 20.Desjardins M.R., Hohl A., Delmelle E.M. Rapid surveillance of COVID-19 in the United States using a prospective space-time scan statistic: detecting and evaluating emerging clusters. Appl Geogr. 2020;118:102202. doi: 10.1016/j.apgeog.2020.102202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chakraborty J. Unequal proximity to environmental pollution: an intersectional analysis of people with disabilities in Harris County, Texas. Prof Geogr. 2020;72(4):521–534. [Google Scholar]
- 22.Turk M.A., Landes S.D., Formica M.K., Goss K.D. Intellectual and developmental disability and COVID-19 case-fatality trends: TriNetX analysis. Disabil Health J. 2020;13 doi: 10.1016/j.dhjo.2020.100942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wheaton F.V., Crimmins E.M. Female disability disadvantage: a global perspective on sex differences in physical function and disability. Ageing Soc. 2016;36(6):1136–1156. doi: 10.1017/S0144686X15000227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.United Nations Department of Economic and Social Affairs Women and girls with disabilities. https://www.un.org/development/desa/disabilities/issues/women-and-girls-with-disabilities.html Available at:
- 25.Chakraborty J. Proximity to extremely hazardous substances for people with disabilities: a case study in Houston, Texas. Disabil Health J. 2018:121–125. doi: 10.1016/j.dhjo.2018.08.004. [DOI] [PubMed] [Google Scholar]