Abstract
We present a case of marked fetal sinus bradycardia as the sole presenting sign of congenital combined pituitary hormone deficiencies. Fetal sinus bradycardia < 120 beats/min was detected at 36 weeks of gestation during an otherwise uncomplicated pregnancy. Sinus bradycardia persisted after birth, and congenital hypothyroidism and growth hormone deficiencies were subsequently identified. Normal sinus rhythm was rapidly restored with hormone supplementation. Hypothyroidism and growth hormone deficiency should be considered in the differential diagnosis of unexplained perinatal sinus bradycardia because early diagnosis may help to avoid potential complications (ie, mental retardation, severe hypoglycemia, and growth anomaly).
Résumé
Nous présentons un cas de bradycardie sinusale fœtale significative constituant l’unique signe de déficit hypophysaire combiné d’origine congénitale. Une bradycardie sinusale fœtale avec un rythme cardiaque inférieur à 120 battements par minute a été détectée au cours de la 36e semaine d’une grossesse par ailleurs sans complications. La bradycardie sinusale a persisté après la naissance. Une hypothyroïdie ainsi qu’un déficit en hormone de croissance d’origine congénitale ont été constatés ultérieurement. Une supplémentation hormonale a permis de normaliser rapidement le rythme sinusal. L’hypothyroïdie et le déficit en hormone de croissance doivent être pris en compte dans le diagnostic différentiel d’une bradycardie sinusale périnatale inexpliquée, car un diagnostic précoce peut aider à éviter des complications potentielles (retard mental, hypoglycémie sévère et anomalie de croissance).
Fetal bradycardia most commonly occurs as the result of obstetrical and cardiac causes. Endocrine causes of bradycardia include hypothyroidism in children and adults, but it is seldom observed in fetuses as maternal thyroid hormones cross the placental barrier until near term to supply the fetus. Congenital hypothyroidism affects 1/2000 to 1/4000 neonates and most commonly results from a primary thyroid anomaly.1 Central hypothyroidism is rare (1/8000 births). It is characterized by normal or low thyrotropin (thyroid-stimulating hormone) and low thyroxine (T4), and is often associated with other pituitary hormone deficiencies.1 We present a rare case of marked fetal sinus bradycardia as the sole presenting sign of combined pituitary hormone deficiencies. Our objective is to raise awareness among fetal and pediatric cardiologists that central hormonal deficiencies may present as isolated sinus bradycardia despite transplacental passage of thyroxine.
Fetal Presentation
A healthy 29-year-old pregnant woman was referred to the fetal cardiology clinic for fetal bradycardia at 36 weeks’ gestation. She reported being told several times during her pregnancy that the fetal heart rate was at the lower limit of normal, although this could not be verified. Her obstetrical, personal, and family histories were otherwise unremarkable. Her thyroid status and serum electrolyte levels were normal. Specifically, there was no personal or familial history of long QT syndrome, and the expecting parents both had normal electrocardiograms. A fetal echocardiography showed no morphological or functional cardiac anomaly. Doppler flow patterns suggested a regular sinus bradycardia between 96 and 106 beats/min with normal atrioventricular intervals (Fig. 1). There was no sign of fetal distress. A fetal echocardiography 1 week later showed similar findings.
Figure 1.
Pulsed-wave Doppler flows from the superior vena cava and the ascending aorta (upper panel), and the left ventricle inflow/outflow (lower panel) showing an atrial rhythm (likely sinus) at 105 beats/min. The late gestational age and fetal position did not allow for a perfect Doppler alignment. Upper panel shows the flow reversal in the superior vena cava during atrial contraction (A) and the forward flow in the aorta during ventricular contraction (V). Lower panel shows normal E and A waves during diastole followed by ventricular ejection, suggesting sinus rhythm.
Neonatal Presentation
The woman presented with spontaneous labour at 37 ± 6 weeks. The fetal heart rate was monitored externally and showed a decreased baseline rate between 96 and 115 beats/min, but with otherwise adequate variability. A seemingly healthy baby girl weighing 2.8 kg was delivered without complications. Her heart rate ranged from 75 to 96 beats/min, but vital signs and physical examination results were otherwise normal. The surface electrocardiograms showed sinus bradycardia with junctional escape at 83 beats/min (normal 100-180) without prolonged QTc interval (Fig. 2). A 24-hour Holter monitor revealed sinus bradycardia with occasional junctional escape rhythm. The ventricular rate ranged from 59 to 135 beats/min (mean of 88 beats/min). The serum thyroid-stimulating hormone was 2.44 mIU/L (normal < 5), and free T4 was 6.8 pmol/L (normal 13-41). This low T4 result was not immediately recognized. All other blood work results were unremarkable. The team was reassured by a junctional rhythm that protected the baby from symptomatic bradycardia and the family was discharged after 3 days.
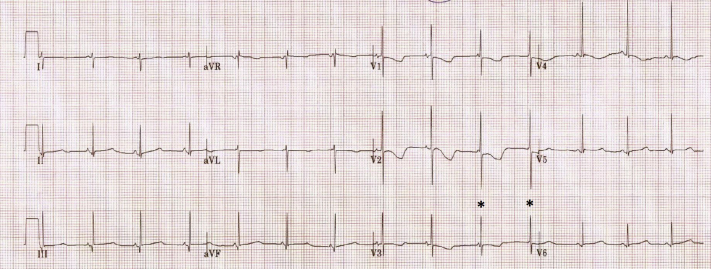
Figure 2.
Electrocardiogram tracing showing sinus rhythm with junctional escape at 84 beats/min. (Asterisks) Junctional escape beats (shorting of the PR interval or no P waves). Repolarization anomalies compatible with age are also seen.
The newborn was seen for a follow-up on day 15. The sinus bradycardia was unchanged, and the mother had no concerns. However, poor weight gain was identified. The mother reported no issues with breastfeeding. There was no history of vomiting, stools were normal, and urinary output was preserved. Physical examination results were remarkable for mild hypotonia, slightly yellow sclera, and a low heart rate. The infant was readmitted for feeding and endocrinology evaluation.
Investigation and Outcome
Abnormal serum levels included an elevated bilirubin of 396 μmol/L (normal < 300), a borderline glucose of 2.6 mmol/L (normal > 2.6), and a low free T4 of 7.6 pmol/L (normal 22-55). Cortisol, thyroid-stimulating hormone, metabolic workup, and urinalysis results were all normal. Serum growth hormone (GH) was undetectable and did not increase with hypoglycemia. Serial serum cortisol values were normal, whereas serum prolactin was decreased at 0.4 μg/L (normal > 12). Magnetic resonance imaging of the sella turcica showed a normal pituitary gland. Genetic testing was positive for a heterozygous POU1F1 gene mutation, which is known to be associated with a combined pituitary hormone deficiency.2 Treatment with levothyroxine and GH were initiated. The heart rate normalized within 10 days. Since then, the patient has remained in normal sinus rhythm between 115 and 150 beats/min, up to her last available follow-up at 18 months. She has short stature, but her development has so far been normal.
Discussion
Rare cases of fetal bradycardia secondary to hormonal deficiencies have been reported.3,4 To our knowledge, this is the first description of congenital hypopituitarism presenting as isolated fetal sinus bradycardia during an otherwise uneventful pregnancy and term delivery. The case also highlights that the bradycardia was rapidly reversible after neonatal treatment with levothyroxine and GH, suggesting that either or both hormonal deficiencies were responsible for the low heart rate.
It remains unclear which of the hormonal deficiencies had an impact on the fetal heart rate. Hypothyroidism causes bradycardia, but because maternal thyroid hormones cross the placental barrier, prenatal signs of congenital hypothyroidism are rare. Cases of reduced heart rate variability during labour due to congenital hypothyroidism without a change in baseline heart rate have been described,5 but we could find only one report describing reduced baseline fetal heart rate in a preterm newborn with ectopic thyroid tissue.4 GH is known to possibly increase the heart rate via the effect of the insulin-like growth factor through mechanisms that have not yet been clearly explained.6 We could not find any report of a direct effect of congenital a GH deficiency on fetal heart rate. Only 1 case report has linked fetal bradycardia to central hypopituitarism,3 but contrary to our case, the infant had significant comorbidities and needed extensive resuscitation and care at birth.
In the presence of isolated fetal bradycardia without fetal distress, the relation between atrial and ventricular systole must be thoroughly determined to rule out cardiac causes of bradycardia such as atrial bigeminy and congenital heart block. If isolated sinus bradycardia is suspected, we believe that fetal hormonal disturbances should be considered in the differential diagnosis amongst other causes of sinus bradycardia, such as long QT syndrome, sinus node dysfunction, maternal hypothyroidism, maternal autoantibodies, and medication effects. Aside from ensuring maternal euthyroid status and fetal well-being, fetal assessment of hormonal disturbances is limited. Hypopituitarism should be promptly ruled out after birth because symptoms are likely to resolve and complications avoided with hormonal supplementation.
Novel Teaching Points.
•Congenital hypopituitarism can present as isolated marked fetal sinus bradycardia and thus should be investigated promptly during the neonatal period.
•Hormonal supplementation is likely to resolve symptoms and may decrease the risk of complications.
Funding Sources
No specific funding was requested for this work.
Disclosures
The authors have nothing to disclose.
Footnotes
Ethics Statement: This study adheres to the principles of the declaration of Helsinki.
See page 422 for disclosure information.
References
- 1.Ford G., LaFranchi S.H. Screening for congenital hypothyroidism: a worldwide view of strategies. Best Pract Res Clin Endocrinol Metab. 2014;28:175–187. doi: 10.1016/j.beem.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 2.Bertko E., Klammt J., Dusatkova P. Combined pituitary hormone deficiency due to gross deletions in the POU1F1 (PIT-1) and PROP1 genes. J Hum Genet. 2017;62:755–762. doi: 10.1038/jhg.2017.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marsh T.D., Lagrew D.C., Cook L.N., Lavery J.P. Unexplained fetal baseline bradycardia in congenital panhypopituitarism. Am J Obstet Gynecol. 1987;156:977–979. doi: 10.1016/0002-9378(87)90371-1. [DOI] [PubMed] [Google Scholar]
- 4.Nakanomori A., Nagano N., Seimiya A., Okahashi A., Morioka I. Fetal sinus bradycardia is associated with congenital hypothyroidism: an infant with ectopic thyroid tissue. Tohoku J Exp Med. 2019;248:307–311. doi: 10.1620/tjem.248.307. [DOI] [PubMed] [Google Scholar]
- 5.Shoham I., Aricha-Tamir B., Weintraub A.Y. Fetal heart rate tracing patterns associated with congenital hypothyroidism. Am J Obstet Gynecol. 2009;201:48 e1–4. doi: 10.1016/j.ajog.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 6.Colao A., Marzullo P., Di Somma C., Lombardi G. Growth hormone and the heart. Clin Endocrinol (Oxf) 2001;54:137–154. doi: 10.1046/j.1365-2265.2001.01218.x. [DOI] [PubMed] [Google Scholar]