Abstract
Background
The Centers for Disease Control and Prevention (CDC) offer behavioral guidance to prevent the spread of infectious diseases like COVID-19. Cleaning (e.g., cleaning surfaces, washing and sanitizing hands) and containing (e.g., covering coughs, keeping distance from others, especially sick people) behaviors are recommended.
Purpose
To develop the Clean and Contain Measure, a brief measure of compliance with CDC recommendations for prevention of infectious disease, and validate the measure in individuals experiencing the COVID-19 pandemic.
Methods
Participants were recruited from Amazon Mechanical Turk and social media.
Results
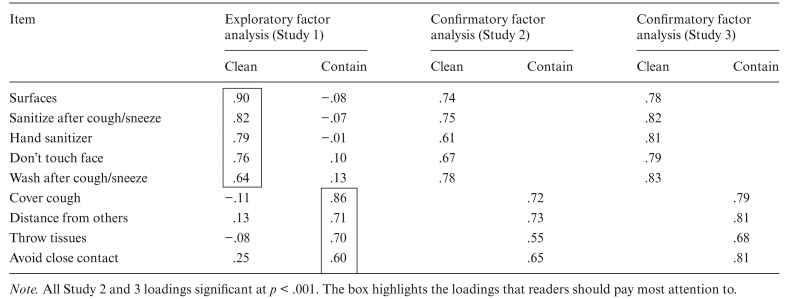
In Study 1 (N = 97), exploratory factor analysis revealed two scales: (a) five items assessing cleaning behaviors and (b) four items assessing containing behaviors. Simple structure was obtained and alpha coefficients for both scales were >.83. In Studies 2 (N = 204) and 3 (N = 527), confirmatory factor analysis verified the identical factor structure found in Study 1. All loadings were statistically significant at p < .001. Alpha coefficients for both scales were >.84 for Studies 2 and 3.
Conclusions
Our measure is a reliable and valid indicator of compliance with cleaning and containing health behaviors that help to prevent the spread of diseases like COVID-19. Future research should replicate construct validity in more diverse samples and continue to refine items, examine construct validity, including predictive and discriminant validity, and improve the measure for future use. With continued use and refinement, this measure could allow health officials and researchers to accurately assess compliance with important infection prevention behavior guidelines.
Keywords: COVID-19, Infectious disease, Health behavior, Public health, Questionnaire, Disease avoidance
Health behavior measurement is critical in limiting the spread of infectious diseases like COVID-19. This 9-item measure assesses compliance with important infectious disease prevention behaviors.
At the time of this writing, approximately 3.7 million Americans are infected with COVID-19 and approximately 140,000 have died [1]. It is likely that these numbers are underestimates due to lack of available testing. COVID-19 is understood to be a dangerous virus with a mortality rate at least three times that of the common influenza virus [2]. It is critical to limit infection using all scientific tools available to us.
Most critically at this point, without an effective treatment or vaccine, healthy behaviors are our best strategy for prevention, but as of yet, there is no scientifically validated method of assessing infection prevention behaviors relevant to pandemics such as COVID-19. While much attention has focused on lack of virus testing, we are in further short supply of accurate behavioral testing. Risk and resilience factors for upholding increasingly challenging guidelines for healthy behavior, even in spite of variability in national, state, and local regulations, are something we lack the ability to effectively measure. Our ability to understand who is most likely to comply with or dismiss recommendations on infection prevention behaviors is limited first and foremost by the lack of valid testing.
Health Behaviors
One of the key tools available to healthcare providers for fighting disease is promotion of healthy behaviors [3, 4]. Health promoting behaviors are any behaviors undertaken by individuals to maintain or improve health, including preventive and screening behaviors. We often think of health behaviors as impacting the long-term development of chronic conditions such as links between eating and exercising behavior and cardiovascular disease or diabetes, but health behaviors are highly relevant though understudied in the area of infectious disease [4, 5].
Health Behaviors and Communicable Diseases
Health behaviors are particularly important in the context of communicable diseases. Because communicable diseases, whether viral or bacterial, are passed from one person to another via various media (e.g., air, surfaces, and bodily fluids), certain behaviors can limit the transmission of these diseases. Typical recommendations include behaviors such as covering one’s mouth and nose when coughing or sneezing, frequent and sustained hand cleansing, and staying home when experiencing symptoms of communicable illness [6].
COVID-19 Health Behavior Recommendations
As cases of COVID-19 began to appear and increase in a staggering fashion, US agencies and municipalities scrambled to make recommendations on how citizens could protect themselves from infection. The Centers for Disease Control and Prevention (CDC) released guidance on health behaviors that individuals should adopt to prevent the spread of the disease with the main goal of avoiding exposure to the novel coronavirus [7]. In March 2020, the CDC recommended the following types of health behaviors in relation to COVID-19: (a) clean your hands; (b) avoid touching your face with unwashed hands; (c) avoid close contact with people who are sick; (d) distance yourself from others if COVID-19 is spreading in your community; (e) stay home if you are sick; (f) cover your mouth and nose with a tissue when you cough or sneeze; (g) throw used tissues in the trash; (h) wash your hands, or clean them with hand sanitizer, after coughing or sneezing; (i) wear a face mask if you are sick; and (j) clean and disinfect frequently touched surfaces daily. Importantly, these recommendations are nothing new to infectious disease prevention. Advice to clean hands, avoid touching one’s face with unclean hands, maintain social distance, etc. has been offered for some time; even as recently as 2019 the CDC made some of these same recommendations for preventing the common cold [8].
Monitoring Health Behaviors as a Tool to Limit Infectious Disease Spread
Health behaviors are our most important tools for preventing individual infections and limiting the spread of communicable diseases such as COVID-19 because often there is no immediate vaccine and limited treatment [9]. Even when vaccines and/or cures become available, it remains paramount to contain the growth of the disease to a manageable rate to ensure an adequate healthcare response. As such, it is crucial for public health officials and researchers to be able to quickly assess engagement with these health behaviors. Understanding who is complying with behavioral recommendations and characteristics that predict this compliance is key to directing educational efforts and identifying communities at risk for greater spread. The importance of monitoring notwithstanding, few, if any, monitoring tools of infection prevention behaviors have been rigorously developed and evaluated, rather most assessment is by single items or checklist counts for which reliability and validity are often unknown.
Present Study
Our first line of defense against epidemics and pandemics is a behavioral response that affords medical, biological, and policy responses the necessary time to catch up and offer an effective vaccine and/or cure. Monitoring, understanding, and predicting human behavior in the face of these types of threats is a crucial component of an effective response, yet often less is known about these aspects of epidemics and pandemics than the biological/genetic aspects of the disease. The current COVID-19 pandemic offers an opportunity to develop a brief measure of infection prevention behaviors for widespread use in research and practice. Exploratory and confirmatory factor analyses and known-groups validity coefficients were used to determine the construct validity of the measure. Regarding known-groups validity, research shows that multiple health behaviors are associated with demographic variables [10, 11]. The literature is smaller and somewhat mixed on relations between demographic variables and infectious-disease-prevention per se [12]. Nonetheless, it appears that older, female, higher socioeconomic status (higher education and income) and non-White respondents tend to engage in infection prevention behaviors more consistently [12]. Married respondents likewise appear to engage in more prevention, but the number of studies is quite low, so it is included for exploratory purposes in this study.
Methods
Measure Development
To develop our brief measure, we created nine items based broadly on the health behavior recommendations made by the CDC in March of 2020 and we administered these items between March 24, 2020 and April 12, 2020. Responses were on a five-point scale with choices 1 = Never, 2 = Sometimes, 3 = About half the time, 4 = Most of the time, and 5 = Always (see Appendix for complete instrument). Our items reference COVID-19, but items can be easily modified for use with other infectious diseases. All studies were approved by an institutional review board and respondents provided informed consent.
Participants
Study 1, 2, and 3 samples were 97, 204, and 527 individuals who completed an online survey on health behaviors and demographics. Study 1 and 3 samples were Amazon Mechanical Turk workers. The Study 2 sample was 97 Amazon Mechanical Turk workers and 107 participants recruited via Facebook and LinkedIn. Sample characteristics are presented in Table 1.
Table 1.
Demographic characteristics of Study 1, 2, and 3 samples
| Variable | Study 1 | Study 2 | Study 3 |
|---|---|---|---|
| Age [M, Mdn, (SD)] | 36, 33 (11.4) | 37, 32 (13.3) | 38, 34 (13.8) |
| Male | 63 | 50 | 48 |
| Female | 37 | 50 | 52 |
| Marital status | |||
| Married | 54 | 44 | 53 |
| Never married | 42 | 48 | 33 |
| Widowed | 1 | 2 | 4 |
| Divorced | 3 | 6 | 7 |
| Education | |||
| High school | 13 | 8 | 9 |
| Some college | 14 | 13 | 18 |
| Associate degree | 12 | 7 | 9 |
| Bachelor degree | 43 | 43 | 45 |
| Master degree | 14 | 19 | 14 |
| Doctoral degree | 2 | 9 | 4 |
| Race | |||
| Asian | 7 | 2 | 8 |
| Black or African American | 8 | 6 | 13 |
| Native Hawaiian or Pacific Islander | 1 | 1 | 2 |
| White | 79 | 91 | 76 |
| Mixed-Race | 3 | 1 | 2 |
| Median income category | $40,000–$49,000 | $50,000–$59,000 | $50,000–$59,000 |
| Ethnicity | |||
| Hispanic | 15 | 10 | 13 |
| Non-Hispanic | 85 | 90 | 87 |
Note. Values represent percentages within each study, except for age where mean (M), median (Mdn), and standard deviation (SD) are provided and income where the median category is provided.
Analyses
Analyses in Study 1 focused on exploratory factor analysis with principal axis extraction (eigenvalues >1) and promax rotation to establish a factor structure of the nine health behavior items. Confirmatory factor analysis was used in Studies 2 and 3 to confirm the Study 1 factor structure in independent samples. Following common guidelines, we considered confirmatory models with Root Mean Square Error of Approximation (RMSEA) <.08, Standardardized Root Mean Residual (SRMR) <.08, and CFI >.90 as acceptable fitting models [13]. There were no missing data. Although the endorsement of these behaviors was quite high, minimal univariate skew/kurtosis was identified. However, multivariate kurtosis was present in Study 3 and robust bootstrap-adjusted fit indices (χ 2, RMSEA, SRMR, and CFI) were used in this instance. In addition, we conducted tests of known-groups validity by examining correlations of demographic characteristics with the scale scores [14]. Known-groups validity is the extent to which a measure distinguishes between groups known to differ on the construct of interest [14]. Statistical significance was set a p < .05.
Results
Factor Analyses
Power and sample size
Item-to-case ratios in Studies 1, 2, and 3 were 11, 23, and 59. Power to reject ill-fitting models in Studies 2 and 3 was .93 and .99, respectively.
Study 1
Exploratory factor analysis of Study 1 data showed communalities of .43–.73 with two factors extracted with eigenvalues of 4.26 and 3.64. Five items loaded on a cleanliness factor (e.g., sanitizing surfaces, washing and sanitizing hands) with loadings ranging from .64 to .90. Four items loaded on containment factor (e.g., covering coughs and social distancing) with loadings ranging from .60 to .86. Alpha coefficients were ≥.83. All factor matrices are included in Table 2.
Table 2.
Exploratory and confirmatory factor analysis standardized loadings for distance and disinfect measure
Study 2
Confirmatory factor analysis of Study 2 data, where two factors identical to the Study 1 factors were specified, showed acceptable fit to the data: χ 2 = 36.20, p = .04, CFI = .98, SRMR = .05, and RMSEA = .05. Cleanliness factor standardized loadings ranged from .61 to .78 (ps < .001). Containment factor standardized loadings ranged from .55 to .73 (ps < .001). Alpha coefficients were ≥.84.
Study 3
Confirmatory factor analysis of Study 3 data, where two factors identical to the Study 1 and 2 factors were specified, showed acceptable fit to the data: χ 2 = 44.18, p < .005, CFI = .99, SRMR = .04, and RMSEA = .04. Cleanliness factor standardized loadings ranged from .78 to .83 (ps < .001). Containment factor standardized loadings ranged from .68 to .81 (p < .001). Alpha coefficients were ≥.87.
Descriptive Statistics
Descriptive statistics for the nine items in Studies 1, 2, and 3 are included in Supplementary Table S1. The clean health behaviors that showed the most compliance were avoiding touching one’s face (Study 1) and using appropriate (i.e., 60% or more alcohol) hand sanitizer (Studies 2 and 3). The contain health behavior that showed the most compliance was throwing used tissues away. In general, participants reported being more likely to comply with containing behaviors than with cleaning behaviors.
Known-Groups Validity
Known-groups validity was evaluated by examining correlations of the Clean and Contain scales with several demographic variables. Older age was associated with more cleaning and containing behaviors in Studies 2 and 3. Being female was associated with more cleaning in Studies 1 and 3 and more containing in Studies 2 and 3. Income showed the largest associations with cleaning and containing but only in Study 1. Hispanic ethnicity was associated with more containing behaviors in all studies. Married respondents showed fewer containing behaviors but only in Study 3. Race and education were unrelated to either variable in any study. Correlations are provided in Supplementary Table S2.
Discussion
Using items based on CDC recommendations, we developed and validated a brief measure of infectious-disease-prevention-related health behaviors and tested its construct validity in samples of individuals currently experiencing the COVID-19 pandemic. A series of three studies support Clean and Contain subscales of the overall measure. Study 1 identified these two subscales and in Studies 2 and 3, these subscales were replicated. In general, participants were more likely to comply with containing behaviors than with cleaning behaviors in all studies. The most highly complied with cleaning health behaviors were avoiding touching one’s face and using effective hand sanitizer. The most highly complied with containing health behavior was throwing used tissues away. In terms of known validity coefficients for cleaning and containing scales, we found small to moderate associations across both scales for age and sex. Income showed the strongest validity coefficient but only in Study 1. Hispanic ethnicity was related to greater compliance with containing across all three studies. Other demographics characteristics showed little to no correlations with the scales.
Use of the Clean and Contain Measure
Preventive health behaviors help to slow the spread of infectious diseases, allow time to develop effective vaccines and/or treatments, and keep rates of infection at manageable levels for the healthcare system [4, 5]. The Clean and Contain Measure could offer public health officials and researchers the ability to quickly assess compliance with infectious disease (e.g., COVID-19) related health behaviors. Knowing which individuals are or are not complying will allow other mitigation efforts to be efficiently targeted. Furthermore, utilizing the Clean and Contain Measure in large-scale assessment will allow researchers to characterize those who are and are not complying with behavioral recommendations. Identifying related demographic and psychological characteristics will further allow efforts to reduce or mitigate disease spread to be effectively targeted. Having an adequate measurement tool will allow behavioral epidemiologists to proceed to test theories of health behavior and better understand the implications of health behavior for the development of the infectious disease pandemics like COVID-19 [6, 15, 16].
Limitations
This study has important limitations. The sample lacks diversity being comprised of mostly white, educated, and middle income respondents. This likely limits tests of known-groups validity as attenuation of variability reduces correlations. Using more diverse and representative samples may provide improved tests of known and construct validity. Compliance with health behaviors was rated quite high potentially suggesting a need to evaluate social desirability. This is an initial attempt at scale development that demonstrates reliability and factorial validity but minimal content and construct validity (both convergent and discriminant).
Future Research Using the Clean and Contain Measure
Future studies should replicate the present findings due to the limitations of the sample, method, and types of validity demonstrated. All forms of construct validity need to be examined. For instance, might the measure predict virus and/or antibody testing or uptake of a vaccine? Research has shown that those who engage in one health promoting behavior are likely to engage in others [10, 11]. Thus, we might predict that high scores on the Clean and Contain Measure would correlate with compliance with further recommendations regarding illness prevention behaviors. Face mask wearing is now a crucial health behavior. To be content valid, perhaps an item on face mask wearing compliance is a necessary inclusion. Both clean and contain scales show higher average scores in Study 3 as compared with Studies 1 and 2. Perhaps this reflects the sensitivity of the measure to detect change, a key component of construct validity [17], in health behaviors resulting from sociocultural forces emphasizing the importance of cleaning, and to a lesser extent containing, as the pandemic progressed during its early stages. Increased adherence would not be surprising given a nearly five times increase in cases from Study 1 to 3 and associated increasing calls and legal mandates from state and local leaders for heightened vigilance and caution. No doubt the measure will need to continue to evolve as recommendations change. It is vitally important to test the measure with more diverse populations, to improve items that may show problems, and to place the items in the context of what current local, state, and federal regulations might be so it can be administered as regulations change. We hope this scale provides a starting point for measuring infection prevention behaviors and others will use and improve this scale in their research on COVID-19 and other communicable diseases.
Conclusion
Measuring health behaviors is a critical tool in limiting the spread of infectious diseases like COVID-19. The Clean and Contain Measure is a brief scale that has shown initial construct validity in US adults. With continued use and refinement, it could prove useful for healthcare providers and public health officials to target intervention as well as by researchers to increase our understanding of which behaviors are especially important and for whom. Ultimately, the Clean and Contain Measure may help to mitigate the growth of public health threats such as COVID-19.
Supplementary Material
Appendix
Clean and Contain Scale
There are currently several recommendations on how to prevent the spread of the novel coronavirus (COVID-19). Please place an "X" in the appropriate box to the right of each item to indicate how often you do each of the following.
| 1: Never | 2: Sometimes | 3: About half the time | 4: Most of the time | 5: Always | |
|---|---|---|---|---|---|
| 1.Use a hand sanitizer that contains at least 60% alcohol, if soap and water are not readily available. (Hand sanitizer) | □ | □ | □ | □ | □ |
| 2.Avoid touching your eyes, nose, and mouth with unwashed hands. (Don’t touch face) | □ | □ | □ | □ | □ |
| 3.Avoid close contact with people who are sick. (Avoid close contact) | □ | □ | □ | □ | □ |
| 4.Put distance between yourself and other people if COVID-19 is spreading in your community. (Distance from others) | □ | □ | □ | □ | □ |
| 5.Cover your mouth and nose with a tissue when you cough or sneeze or use the inside of your elbow. (Cover cough/sneeze) | □ | □ | □ | □ | □ |
| 6.Throw used tissues in the trash. (Throw tissues) | □ | □ | □ | □ | □ |
| 7.After coughing or sneezing, immediately wash your hands with soap and water for at least 20 s. (Wash after cough/sneeze) | □ | □ | □ | □ | □ |
| 8.After coughing or sneezing, if soap and water are not readily available, clean your hands with a hand sanitizer that contains at least 60% alcohol. (Sanitize after cough/sneeze) | □ | □ | □ | □ | □ |
| 9.Clean AND disinfect frequently touched surfaces (tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets, and sinks). (Surfaces) | □ | □ | □ | □ | □ |
Note. Item labels from Table 2 in parentheses.
Compliance with Ethical Standards
Authors’ Statement of Conflict of Interest and Adherence to Ethical Standards Authors Loren L. Toussaint, Alyssa D. Cheadle, Jesse Fox, and David R. Williams declare that they have no conflict of interest.
Authors’ Contributions All authors made substantial contributions to conception and design; data collection/management, analysis, and interpretation; and drafting and critically revising the article. All authors provided final approval of the version to be published.
Ethical Approval All procedures performed were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
References
- 1. Centers for Disease Control and Prevention. Coronavirus disease 2019: cases in the U.S. Available at https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. Accessibility verified May 21, 2020.
- 2. Verity R, Okell LC, Dorigatti I, et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis. 2020:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Berrigan D, Dodd K, Troiano RP, Krebs-Smith SM, Barbash RB. Patterns of health behavior in U.S. adults. Prev Med. 2003;36:615–623. [DOI] [PubMed] [Google Scholar]
- 4. Weston D, Hauck K, Amlôt R. Infection prevention behaviour and infectious disease modelling: a review of the literature and recommendations for the future. BMC Public Health. 2018;18:336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Frıas-Martınez E, Williamson G, Frıas-Martınez V. An agent-based model of epidemic spread using human mobility and social network information. Third International Conference on Social Computing; Boston, MA. 2011:57–64.
- 6. Larson EL. Warned, but not well armed: preventing viral upper respiratory infections in households. Public Health Nurs. 2007;24:48–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19): how to protect yourself Available at https://www.cdc.gov/coronavirus/2019-ncov/prepare/prevention.html. Accessibility verified March 19, 2020.
- 8. Centers for Disease Control and Prevention. Common colds: protect yourself and others Available at https://www.cdc.gov/features/rhinoviruses/index.html. Accessibility verified June 16, 2020.
- 9. Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395:470–473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Saint Onge JM, Krueger PM. Health lifestyle behaviors among U.S. adults. SSM Popul Health. 2017;3:89–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Spring B, Moller AC, Coons MJ. Multiple health behaviours: overview and implications. J Public Health (Oxf). 2012;34(suppl 1):i3–i10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bish A, Michie S. Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Br J Health Psychol. 2010;15:797–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kline RB. Principles and Practice of Structural Equation Modeling. New York, NY: Guilford Press; 2004. [Google Scholar]
- 14. Streiner DL, Norman GR, Cairney J. Health Measurement Scales: A Practical Guide to Their Development and Use. 5th ed. Oxford, UK: Oxford University Press; 2015. [Google Scholar]
- 15. Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2:328–335. [Google Scholar]
- 17. Terwee CB. Responsiveness to change. In: Michalos AC, ed. Encyclopedia of Quality of Life and Well-Being Research. Dordrecht, Netherlands: Springer; 2014:5547–5550. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.