While data continue to emerge around prevalence rates of coronavirus disease 2019 (COVID-19) in the general population, there is limited understanding of infection rates among health care workers (HCWs), a particularly important component of the response to this pandemic as more areas of the world experience surges in severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection rates.1-3 Viral testing through reverse transcription polymerase chain reaction (RT-PCR) demonstrates active infection, whereas serologic testing for SARS-CoV-2 may answer epidemiologic questions about the prevalence of COVID-19, especially in areas where viral testing has been limited.4,5 Here we provide data showing SARS-CoV-2 antibody prevalence in HCWs working in a hospital in New York City (NYC) during the early pandemic in the United States.
The first case in NYC was identified on March 1, 2020, and cases steeply grew over the ensuing weeks. Beginning on April 17, 2020, serologic testing was offered to HCWs who were employed at our 862-bed Manhattan quaternary-care teaching hospital, an affiliated Queens 535-bed tertiary-care community teaching hospital, and an affiliated 180-bed Manhattan nonteaching community hospital. To qualify for testing, HCWs were required to be asymptomatic for 14 days after illnesses consistent with COVID-19, regardless of prior viral testing.
The SARS-CoV-2 cyclic enhanced fluorescence assay (CEFA) used (ET Healthcare) was validated against the Food and Drug Administration emergency use authorization–approved New York State (NYS) Department of Health method, showing excellent concordance (n = 145 HCW samples, 95.5% agreement excluding indeterminate results, κ = 0.905; 95% confidence interval [CI], 0.831-0.979). The CEFA also demonstrated excellent specificity (IgG = 98.8% and IgM = 99.4%) using 320 pre-COVID-19 samples.6 The SARS-CoV-2 RT-PCR assay was performed using the cobas SARS-CoV-2 test on the cobas 6800 platform (Roche Diagnostics), which detects SARS-CoV-2 RNA extracted from nasopharyngeal swab specimens.
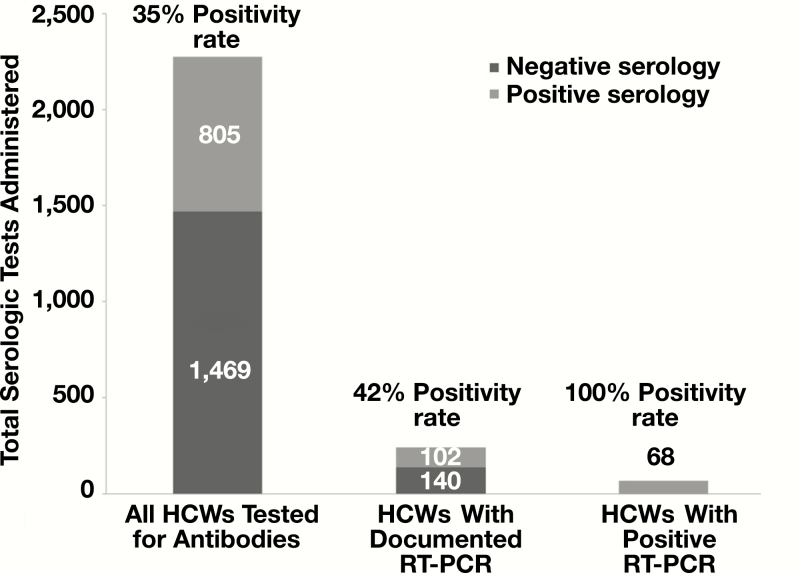
Among the 2,274 HCWs who received a serologic test between April 17, 2020, and May 7, 2020, 35.4% (805/2,274) tested positive for seroconversion of SARS-CoV-2 antibodies, 61.6% (1,401/2,274) tested negative, and 3.0% (68/2,274) were indeterminate Table 1. The majority of HCWs who had seroconverted were either IgG (573/805; 71.2%) or IgG/IgM positive (225/805; 27.9%) Table 2. Of the 2,274 HCWs receiving the serologic assay, 242 (10.6%) had a previous documented RT-PCR viral test. Among this dually tested population, all 68 HCWs (100%) who tested positive for COVID-19 by RT-PCR also tested positive for antibodies Figure 1, demonstrating IgG (47/68; 69.1%) or IgG/IgM (21/68; 30.9%) positivity (Table 2). In comparison, of the 174 HCWs with a negative RT-PCR test, 19.5% (34/174) tested positive for antibodies, reflective of (1) the clinical sensitivity of SARS-CoV-2 molecular assays, which are estimated to be between 58% and 96%, or (2) the timing of the molecular testing.7 Those with positive RT-PCR and serology tests had a higher median age (48 years; interquartile range, 41, 55 years) compared to all others (P < .001).
Table 1.
Demographic Characteristics of Health Care Workers Who Received COVID-19 Testing
| Serology | RT-PCR and Serology | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total(n = 2,274) | Positive (n = 805 [35.4%]) | Negative(n = 1,401 [61.6%]) | Indeterminate (n = 68 [3.0%]) | P Valuea | Total(n = 242) | Both Positive (n = 68 [28.1%]) | Both Negative(n = 140 [57.9%]) | PCR Negative/ Serology Positive (n = 34 [14.0%]) | PCR Positive/ Serology Negative(n = 0 [0.0%]) | P Valuea | |
| Age, y | 37 (31, 48) | 36 (30, 48) | 37 (31, 48) | 38.5 (33, 49) | .076 | 39 (32, 48) | 48 (41, 55) | 35 (30, 41) | 44 (36, 48) | 0 | <.001 |
| Sex, No. (%) | .763 | .136 | |||||||||
| Female | 1,440 | 517 (36.0) | 879 (61.0) | 44 (3.0) | 155 | 37 (23.9) | 96 (61.9) | 22 (14.2) | 0 (0.0) | ||
| Male | 834 | 288 (34.5) | 522 (62.6) | 24 (2.9) | 87 | 31 (35.6) | 44 (50.6) | 12 (13.8) | 0 (0.0) | ||
| Race, No. (%) | <.001 | .074 | |||||||||
| Asian | 237 | 90 (38.0) | 139 (58.6) | 8 (3.4) | 22 | 6 (27.3) | 9 (40.9) | 7 (31.8) | 0 (0.0) | ||
| African American | 91 | 44 (48.4) | 47 (51.6) | 0 (0.00) | 19 | 5 (26.3) | 14 (73.7) | 0 (0.00) | 0 (0.0) | ||
| White | 893 | 277 (31.0) | 580 (65.0) | 36 (4.0) | 95 | 28 (29.5) | 51 (53.7) | 16 (16.8) | 0 (0.0) | ||
| Other or declined | 1,053 | 394 (37.4) | 635 (60.3) | 24 (2.3) | 106 | 29 (27.3) | 66 (62.3) | 11 (10.4) | 0 (0.0) | ||
| Job role,b No. (%) | <.001 | .806 | |||||||||
| Physician, NP, PA | 998 | 282 (28.3) | 678 (67.9) | 38 (3.8) | 97 | 31 (31.9) | 54 (55.7) | 12 (12.4) | 0 (0.0) | ||
| Other staff in room | 570 | 225 (39.5) | 329 (57.7) | 16 (2.8) | 61 | 16 (26.2) | 35 (57.4) | 10 (16.4) | 0 (0.0) | ||
| Ancillary staff | 263 | 120 (45.6) | 137 (52.1) | 6 (2.3) | 37 | 11 (29.7) | 22 (59.5) | 4 (10.8) | 0 (0.0) | ||
| Admin staff | 286 | 130 (45.5) | 151 (52.8) | 5 (1.7) | 29 | 8 (27.6) | 17 (58.6) | 4 (13.8) | 0 (0.0) | ||
| Other | 157 | 48 (30.6) | 106 (67.5) | 3 (1.9) | 18 | 2 (11.1) | 12 (66.7) | 4 (22.2) | 0 (0.0) |
RT-PCR, reverse transcription polymerase chain reaction.
aThe P value for the comparison of age between test results is calculated with the use of the Kruskal-Wallis test with median (Q1, Q3). The P value for the comparison of sex, race, and job categories by testing result is calculated with the use of the χ 2 test and Fisher exact test.
bJob role descriptors: Physician, NP (nurse practitioner), PA (physician assistant): patient-facing health care providers. Other staff in room: patient-facing health care workers, including nurses, respiratory therapists, phlebotomists. Ancillary staff: non–patient-facing workers on a hospital floor, including desk clerks, couriers, custodial staff, physical/occupational therapists, clinical laboratory workers. Administrative staff: non–patient-facing workers not on the hospital floor working primarily in an office. Other: Non–patient-facing workers that do not fall under previously mentioned categories, including medical school staff, cafeteria workers, non–clinical laboratory workers.
Table 2.
Serology and Seroconversion Results of 2,274 Health Care Workers Previously Testing Positive for SARS-CoV-2 by RT-PCR or Clinically Suspected to be Positive for SARS-CoV-2a
| IgG or IgM Total Positives | IgG Positive |
IgM Positive |
IgG and IgM Positive | IgG and IgM Negative | Indeterminate | |
|---|---|---|---|---|---|---|
| No PCR (n = 2,032) | 703 (34.6%) | 501 (24.7%) | 6 (0.3%) | 196 (9.6%) | 1,267 (62.3%) | 62 (3.1%) |
| PCR performed (n = 242) | ||||||
| Positive (n = 68) | 68 (100.0%) | 47 (69.1%) | 0 (0.0%) | 21 (30.9%) | 0 (0.0%) | 0 (0.0%) |
| Negative (n = 174) | 34 (19.5%) | 25 (14.4%) | 1 (0.6%) | 8 (4.6%) | 134 (77.0%) | 6 (3.4%) |
| Total (n = 2,274) | 805 (35.4%) | 573 (25.2%) | 7 (0.3%) | 225 (9.9%) | 1,401 (61.6%) | 68 (3.0%) |
RT-PCR, reverse transcription polymerase chain reaction.
aData are given as No. (%).
Figure 1.
Serologic prevalence of antibodies among health care workers (HCWs). RT-PCR, reverse transcription polymerase chain reaction.
The rate of antibody positivity in symptomatic HCWs was much higher than NYS testing during this time period, which demonstrated 12.2% of all HCWs and 19.9% in the general population across the NYC region.1 However, this is not surprising, as the state sampled personnel regardless of history of COVID-19 symptoms or diagnosis.1,2 A 100% seroconversion rate among those HCWs with a positive SARS-CoV-2 RT-PCR test suggests a strong detectable antibody response at 14 days or later post recovery among those with known infection. Overall, only 35.4% of symptomatic HCWs tested positive for SARS-CoV-2 antibodies despite their high risk of exposure and COVID-19–like symptoms. One possibility is that many HCWs had previous COVID-19–consistent symptoms but not the disease, as the symptoms are nonspecific. Another possibility is that the immune response was delayed in some HCWs, as internal validation analysis of the assay demonstrated optimal sensitivity at 21 days after symptom onset. For some HCWs with infections in early March, the antibody level may have already waned by early May. A final possibility is that some SARS-CoV-2–infected HCWs did not mount a detectable antibody response.8
The proportion of positive serology tests was significantly different across job role categories (P < .001), with a higher percentage of ancillary (45.6%) and administrative (45.5%) staff testing positive compared to other job categories, including patient-facing physicians, nurse practitioners, physician assistants (28.3%), and other staff in the patients’ rooms (39.5%) (Table 1). In fact, the odds of testing positive for serology, after adjusting for age, sex, and race, are statistically higher for ancillary and administrative staff with an odds ratio of 2.12 and 2.20 respectively, when compared to physicians, nurse practitioners, and physician assistants Table 3. This intriguing finding is not easily explained without further research focusing on other confounding factors. It is possible that patient-facing staff developed a more vigilant approach to personal protective equipment, not only in the hospital but also in their everyday non–work-related encounters after witnessing firsthand the severity of the disease. There may also be other unknown socioeconomic factors that relate to job roles.
Table 3.
Odds of Testing Positive for Serology, Adjusting for Age, Sex, Race, and Job Role
| Characteristic | OR | 95% CI | P Value |
|---|---|---|---|
| Age | 0.99 | 0.99-1.00 | .14 |
| Sex | |||
| Female | — | — | |
| Male | 1.12 | 0.92-1.35 | .3 |
| Race | |||
| White | — | — | |
| Asian | 1.48 | 1.09-2.00 | .011 |
| African American | 1.79 | 1.15-2.79 | .010 |
| Other or Declined | 1.34 | 1.11-1.62 | .003 |
| Job rolea | |||
| Physician, NP, PA | — | — | |
| Other staff in room | 1.68 | 1.33-2.11 | <.001 |
| Ancillary staff | 2.12 | 1.59-2.83 | <.001 |
| Admin staff | 2.20 | 1.67-2.94 | <.001 |
| Other | 1.12 | 0.77-1.61 | .6 |
CI, confidence interval; OR, odds ratio.
aJob role descriptors: Physician, NP (nurse practitioner), PA (physician assistant): patient-facing health care providers. Other staff in room: patient-facing health care workers, including nurses, respiratory therapists, phlebotomists. Ancillary staff: non–patient-facing workers on a hospital floor, including desk clerks, couriers, custodial staff, physical/occupational therapists, clinical laboratory workers. Administrative staff: non–patient-facing workers not on the hospital floor working primarily in an office. Other: Non–patient-facing workers that do not fall under previously mentioned categories, including medical school staff, cafeteria workers, non–clinical laboratory workers.
The proportion of positive serology tests was also significantly different across race categories (P < .001). Of the 91 African American HCWs tested, 48.4% tested positive for antibodies compared to 38.0% for Asian HCWs and 31.0% for white HCWs (Table 1). While a significant number of HCWs had missing racial information, the higher positivity rates among African American HCWs is notable and reflective of the emerging literature that found similar racial disparities.9-11 In our data, we found that even when adjusting for age, sex, and job role, the odds of testing positive on serology are 79% higher for African American HCWs compared to white HCWs (Table 3 and Supplemental Table 1S; all supplemental material can be found at American Journal of Clinical Pathology online). Our limited demographic information makes it challenging to interpret this result. An increased prevalence of comorbidities associated with race may help explain the increased rate of COVID-19 among this group. Future work should assess positivity rates according to other possible confounding factors, such as comorbidities, COVID-19 exposure outside the work place, residence, and transit patterns to help garner explanations for such findings.12
This view into SARS-CoV-2 testing in symptomatic HCWs during the early weeks of the COVID-19 pandemic in NYC demonstrated high rates of seroprevalence and reinforces the need for expanded RT-PCR testing for HCWs. At our institution during this early time period, RT-PCR testing resources were prioritized for those exhibiting symptoms. As testing resources have become more available, HCWs at our hospital now have access to both serologic and RT-PCR testing. Hospital systems with limited resources currently experiencing a rapid rise in COVID-19 cases may also resort to only testing symptomatic HCWs. In light of our data, it may be prudent to pay particular attention to underrepresented minorities and older patients. Furthermore, it should not be automatically assumed that those in non–patient-facing roles are necessarily at lower risk for COVID-19. These findings can also guide the use of limited testing to enable safe return of symptomatic personnel to the workforce. Further work needs to elucidate the relationship between antibody response and immunity.
Supplementary Material
Dr Zhao received seed instruments and sponsored travel from ET Healthcare.
References
- 1. Amid ongoing COVID-19 pandemic, Governor Cuomo announces results of completed antibody testing study of 15,000 people showing 12.3 percent of population has COVID-19 antibodies https://www.governor.ny.gov/news/video-audio-photos-rushtranscript-amid-ongoing-COVID-19-pandemic-governor-cuomo-announces-21. Accessed May 12, 2020.
- 2. Rosenberg ES, Tesoriero JM, Rosenthal EM, et al. Cumulative incidence and diagnosis of SARS-CoV-2 infection in New York. medRxiv. 2020. doi: 10.1101/2020.05.25.20113050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chou R, Dana T, Buckley DI, et al. Update alert: epidemiology of and risk factors for coronavirus infection in health care workers. Ann Intern Med. 2020. doi: 10.7326/L20-0768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers for Disease Control and Prevention. Serology testing for COVID-19 https://www.cdc.gov/coronavirus/2019-ncov/lab/serology-testing.html. Accessed May 13, 2020.
- 5. Food and Drug Administration. Coronavirus (COVID-19) update: serological tests https://www.fda.gov/news-events/press-announcements/coronavirus-COVID-19-update-serological-tests. Accessed May 13, 2020.
- 6. Yang HS, Racine-Brzostek SE, Lee WT, et al. SARS-CoV-2 antibody characterization in emergency department, hospitalized and convalescent patients by two semi-quantitative immunoassays. Clin Chim Acta. 2020. doi: 10.1016/j.cca.2020.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Green DA, Zucker J, Westblade LF, et al. Clinical performance of SARS-CoV-2 molecular testing. J Clin Microbiol. 2020. doi: 10.1128/JCM.00995-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Seow J, Graham C, Merrick B, et al. Longitudinal evaluation and decline of antibody responses in SARS-CoV-2 infection. medRxiv. 2020. doi: 10.1101/2020.07.09.20148429. [DOI] [Google Scholar]
- 9. Yancy CW. COVID-19 and African Americans. JAMA. 2020;323:1891-1892. [DOI] [PubMed] [Google Scholar]
- 10. Pan D, Sze S, Minhas JS, et al. The impact of ethnicity on clinical outcomes in COVID-19: a systematic review. EClinicalMedicine. 2020. doi: 10.1016/j.eclinm.2020.100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Price-Haywood EG, Burton J, Fort D, et al. Hospitalization and mortality among black patients and white patients with Covid-19. N Engl J Med. 2020;382:2534-2543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Li AY, Hannah TC, Durbin JR, et al. Multivariate analysis of black race and environmental temperature on COVID-19 in the US. Am J Med Sci. 2020. doi: 10.1016/j.amjms.2020.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.