Abstract
Evidence regarding the important role of adolescents and young adults (AYA) in accelerating and sustaining coronavirus disease 2019 (COVID-19) outbreaks is growing. Furthermore, data suggest that 2 known factors that contribute to high severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) transmissibility—presymptomatic transmission and asymptomatic case presentations—may be amplified in AYA. However, AYA have not been prioritized as a key population in the public health response to the COVID-19 pandemic. Policy decisions that limit public health attention to AYA and are driven by the assumption of insignificant forward transmission from AYA pose a risk of inadvertent reinvigoration of local transmission dynamics. In this viewpoint, we highlight evidence regarding the increased potential of AYA to transmit SARS-CoV-2 that, to date, has received little attention, discuss adolescent and young adult–specific considerations for future COVID-19 control measures, and provide applied programmatic suggestions.
Keywords: adolescents and young adults, SARS-CoV-2 transmission, COVID-19 pandemic
Adolescents and young adults (AYA), that is, those who are between the ages of 10 and 24 years, account for approximately 20% of the total population in the United States, but the extent to which AYA contribute to forward transmission of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is not fully understood. While the published evidence remains inconclusive and contains methodological limitations, such as small sample sizes [1, 2], missing information regarding the timing of test administration relative to exposure [3], and potential selection and collider biases [4, 5], the body of evidence that supports the importance of AYA in accelerating and sustaining coronavirus disease 2019 (COVID-19) outbreaks is growing [6–9].
Policy decisions that are driven by the still prevalent assumption of insignificant forward transmission from AYA pose a risk of inadvertent reinvigoration of local transmission dynamics, particularly as jurisdictions relax social distancing measures and explore ways to reopen schools and universities and as economies rebound and AYA enter the workforce. In this viewpoint, we highlight evidence regarding the increased potential of AYA to transmit SARS-CoV-2 that, to date, has received little attention, discuss adolescent and young adult–specific considerations for future COVID-19 control measures, and provide applied programmatic suggestions.
AYA TRANSMISSION OF SARS-COV-2
Clinical Considerations
Examination of 2 known factors that contribute to high SARS-CoV-2 transmissibility—presymptomatic transmission and asymptomatic case presentations [10]—provides insights into the transmission potential of specific populations. Emerging evidence suggests that both of these transmissibility factors can be amplified in AYA, indicating that AYA may represent an underaddressed population for SARS-CoV-2 transmission control.
Presymptomatic transmission represents a key facilitator of COVID-19 outbreaks. The median serial interval of infectious diseases, that is, the time between symptom onset for an index case and the date of symptom onset for secondary cases, can provide information about the likelihood of presymptomatic transmission. For COVID-19, a median serial interval that is shorter than the incubation period indicates a high probability of presymptomatic transmission [10]. Importantly, emerging evidence suggests that the median serial interval for AYA may be significantly shorter (1–2 days) [6, 7] than in the general population (4–6 days) [11–13]. Given an estimated median COVID-19 incubation period of 5 days [14], these data suggest presymptomatic transmission may be more common among AYA than among older age cohorts. Variability in serial intervals has been linked to differential incubation periods, profiles of infectiousness, and contact patterns [13], the role of which needs to be better understood in AYA transmission dynamics.
In addition, asymptomatic infections complicate case finding and isolation. Therefore, the large proportion of asymptomatic COVID-19 cases, estimated to be approximately 16% in a recent meta-analysis where included estimates ranged from 6% to 41%, facilitates transmission [15]. While low risk-of-bias estimates of the asymptomatic fraction by age are scarce [15], a growing body of evidence suggests that disease severity is increasing with age and that AYA are more likely to experience no or only mild symptoms compared with older age cohorts [12, 16, 17]. While a growing body of evidence suggests comparable viral loads of symptomatic and asymptomatic individuals infected with SARS-CoV-2 [18], accurate estimates of forward transmission from AYA are not possible in the absence of conclusive data regarding the disease severity-dependent infectiousness of SARS-CoV-2. Furthermore, recognition of the full range of COVID-19 clinical manifestations in AYA continues to evolve. Most recently, AYA have presented with atypical symptoms, such as multisystem inflammatory syndrome in children, presumed to be associated with COVID-19 [19]. Given slowly expanding testing capacity, clinically defined testing criteria, and prioritization of severely symptomatic cases for COVID-19 testing, timely identification and isolation of AYA infected with SARS-CoV-2 but with no, mild, or atypical symptoms is less likely, thereby increasing the risk of forward transmission.
Reliability of Available Case Data
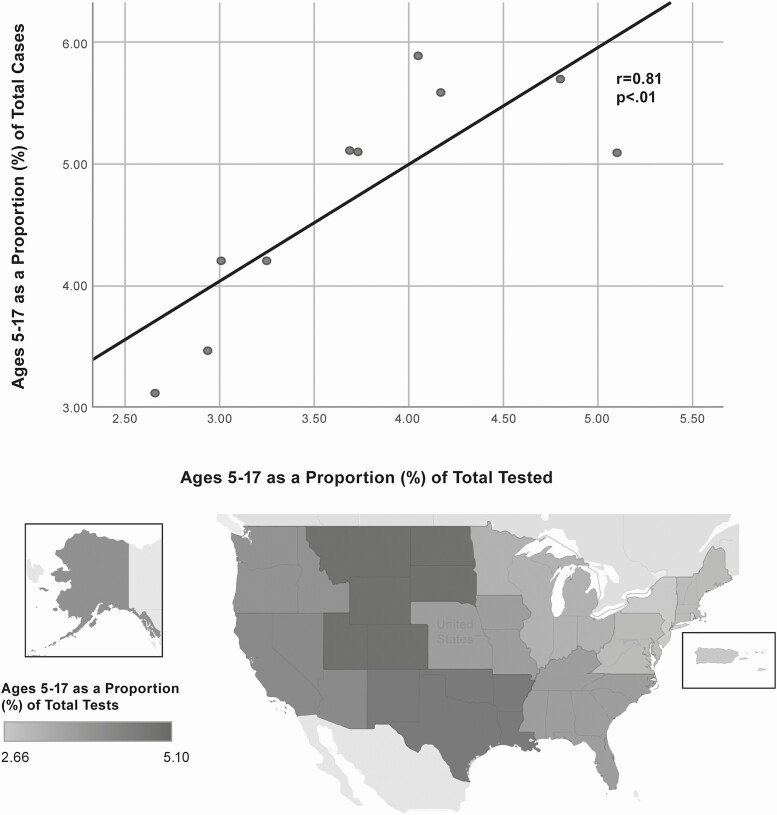
Despite recent expansions, significant gaps and regional differences in testing capacities for SARS-CoV-2 in the United States persist. Limited testing capacities complicate surveillance efforts and likely result in a substantial undercount of true infections. Testing practices, which prioritize severe cases and patients who present with specific symptoms, render available COVID-19 case data for AYA particularly unreliable. Data for the period March 29–June 27 from commercial laboratories, which process approximately 80% of all COVID-19 tests nationwide, show that individuals aged 5–17 years accounted for only 3.5% of all COVID-19 tests conducted in the United States and a corresponding 4.4% of confirmed COVID-19 cases [20], despite accounting for 17% of the population. However, testing data also show that across the Department of Health and Human Services geographic operating regions, the proportion of tests conducted among those aged 5–17 years is approximately proportional to the share of confirmed COVID-19 cases accounted for by that age group (Figure 1). In other words, low testing rates in the cohort of those aged 5–17 years could significantly contribute to the low COVID-19 case counts, particularly given that the proportion of positive tests among individuals aged 5–17 years (12.3%) is higher than for any other age group (0–4 years, 8.4%; 18–49 years, 10.8%; 50–64 years, 9.0%; ≥ 65 years, 7.5%) [20].
Figure 1.
Youth (aged 5–17 years) proportion of total severe acute respiratory syndrome coronavirus 2 tests by youth proportion of total positive cases.
While available surveillance statistics fail to disaggregate young adults, the data presented here for children and adolescents aged 5–17 years are compelling in illustrating the impact of low testing rates on the disproportionately small number of young people in national case statistics, serving as further evidence for the increased risk of undetected infection in young people. In fact, serologic testing data from New York State [21] identified a similar seroprevalence of SARS-CoV-2 antibodies among young adults aged 18–24 years (10.9%) and among older adults aged 55–64 years (11.9%), 65–74 years (10.4%), as well as among those aged ≥75 (9.5%). Similarly, a population-based study in Geneva, Switzerland, found the seroprevalence of SARS-CoV-2 antibodies to be similar in the 10–19 years (9.6%), 20–49 years (9.9%), and 50–64 years (7.4%) age cohorts, but found lower seroprevalence among those aged <10 years (0.8%) or >64 years (4.1%) [22]. Importantly, available serologic data may reflect the impact of social distancing measures (eg, school closures, shelter-in-place orders) that were implemented promptly during the epidemic and have been shown to disproportionately reduce the contact rates of AYA [23], leaving uncertainty regarding the validity of inferences about COVID-19 prevalence distributions across age groups in the absence of these control measures.
Accounting for Physiological and Behavioral Differences Between AYA and Young Children
It is important to note that much of the available evidence that suggests infrequent forward transmission of SARS-CoV-2 from young people relies on data specific to young children (<10 years), fails to disaggregate young children from adolescents (10–19 years), or excludes young adults (20–24 years) [1, 2, 24]. However, physiological and behavioral factors indicate AYA may have greater susceptibility and transmission potential compared with younger children. For example, angiotensin-converting enzyme 2 (ACE-2) expression, which has been linked to COVID-19 susceptibility, has been shown to increase with age, with ACE-2 expression among young adults aged 20–24 and adolescents aged 10–19 years falling within 2% and 10% of the expression among older adults (≥25 years), respectively, while young children show significantly lower expression (>20% difference) [25].
Interestingly, a recent mathematical modeling analysis found that a decreased SARS-CoV-2 susceptibility in the age groups 0–9 years and 10–19 years by approximately 50% relative to individuals aged ≥20 years is consistent with observed case data from various settings globally [17]. In contrast, susceptibility of individuals aged 20–29 years was estimated to be approximately as high as that in older age cohorts. Given that disease susceptibility is determined by biological factors and that adolescent physiological development is gradual and takes place over the course of adolescence rather than instantaneously, the estimated stepwise increase in susceptibility, doubling from those aged <20 years to those aged ≥20 years, is unlikely to be an accurate representation of the underlying physiological changes. A biologically more plausible scenario is that SARS-CoV-2 susceptibility in AYA mirrors a developmental trajectory that is analogous to the one shown for ACE-2 expression, with susceptibility among older adolescents and young adults approaching that of older adults and with susceptibility among younger adolescents increasing gradually throughout pubertal development. Importantly, data from both surveillance and research studies that disregard important developmental stages in early, mid, and late adolescence as well as young adulthood may obscure gradual but meaningful changes in SARS-CoV-2 susceptibility, resulting in the underestimation of true susceptibility among AYA.
Furthermore, behavioral factors unique to AYA may increase the risk of forward transmission of SARS-CoV-2 relative to both younger children and older adults. For example, data suggest AYA tend to have a higher frequency of contacts effective in the transmission of respiratory infections (ie, close contact with individuals in enclosed settings for longer than 5 minutes) than do younger children and older adults [23]. In addition, motivating AYA to adhere to social distancing and other COVID-19 control strategies (eg, hand washing, using hand disinfectant) appears to be particularly difficult [26]. For these reasons, we argue that AYA represent a distinct population that warrants specific considerations in COVID-19 prevention and containment efforts.
Taken as a whole, the evidence regarding the prevalence of COVID-19 among AYA and their role in the forward transmission of SARS-CoV-2 in the United States is not conclusive, but data suggest current estimates may inadequately reflect the contribution of AYA to accelerating and sustaining COVID-19 outbreaks. These insights have important implications for improving the effectiveness and durability of the COVID-19 response. As an evidence base for the design, communication, and implementation of AYA-centered control measures, detailed age disaggregation of surveillance and research data as well as research on AYA exposures, household data, prevention behavior, and symptom profiles are needed.
AYA-SPECIFIC CONSIDERATIONS FOR COVID-19 CONTROL MEASURES
The SARS-CoV-2 transmission potential of young people, including AYA, has received increasing attention in the context of scientific, political, and public discourse about the utility of school closures for population-level COVID-19 control. A growing body of research, including mathematical modeling studies, suggests moderate effects of school closures on the population-level incidence of COVID-19 [17, 27]. This notwithstanding, caution is warranted when implementing gradual school and university reopening, given that the quality of available surveillance data remains questionable, the published evidence contains methodological limitations, and forward transmission of SARS-CoV-2 from AYA is not fully understood. Accordingly, there is growing consensus in the scientific community that approaches that combine the return to in-person instruction with other effective control measures, such as reduced student density in classroom indoor settings, maintenance of adequate social distance, and use of face masks, hand disinfectant, and similar precautions [28], represent the most promising strategies for balancing the benefits and potential risks of reopening school and university systems in the United States and globally.
However, it is important to note that current public health measures do not prioritize AYA-specific considerations in domains of the COVID-19 response other than school closures, which represents a missed opportunity for increasing the long-term effectiveness of COVID-19 control measures. We argue that there is a need for AYA-specific considerations for testing, averting household transmission, leveraging family influence, evaluating AYA brain development, and evaluating AYA social context and provide a set of applied programmatic suggestions to strengthen the design, communication, and implementation of future COVID-19 control measures that warrant consideration by policymakers and public health professionals (Table 1).
Table 1.
Adolescent and Young Adult Programmatic Suggestions for Coronavirus Disease 2019 Prevention and Control
| Theme | Adolescent and Young Adult-specific Consideration | Programmatic Suggestion |
|---|---|---|
| Adolescence and young adulthood as a distinct developmental period | While evidence shows AYA acquire and transmit SARS-CoV-2, AYA have not been prioritized as a key population in the COVID-19 response. | Consideration of factors unique to AYA in the design, communication, and implementation of COVID-19 control measures is warranted. |
| Adolescence and young adulthood is a distinct period of neurobiological development in which changing connectivity between brain regions results in the prioritization of short-term social and emotional reward (eg, group interactions, normative life events), rather than the long-term health consequences of potential COVID-19 infection [S1]. | Public health programs and messaging can emphasize the short-term socioemotional benefits of adopting COVID-19 measures for AYA (eg, face masks as a style accessory, social distancing as an opportunity to spend time with one’s family) and the collective nature of the COVID-19 response (eg, “We—AYA, peers, parents, other important influencers in AYA’s lives—are all in this together”). | |
| COVID-19–related research is primarily focused on adults and vulnerable populations, with limited attention placed on early, middle, late adolescence and young adulthood. | Surveillance and research studies that disaggregate data by age, as well as focus on AYA social, immune, endocrine, epigenetic, and clinical factors that may sustain COVID-19 outbreaks are needed. | |
| Public health messaging | Incomplete uptake of COVID-19 protective behaviors among AYA has been depicted as irresponsible in the media and in public health messaging. | Punitive messaging is counterproductive and does not adequately recognize the conflict of normative AYA identity development and social distancing measures. |
| Primary caregivers (ie, parents) are an important influence on adolescent and young adult health behavior [S2, S3]. | An emphasis on specific guidance for primary caregivers regarding COVID-19 communication and monitoring can address gaps in extant public health communication designed to shape AYA behavior. | |
| Public health messaging for AYA is primarily generic and has not provided specific guidance on how AYA can prevent transmission in their day-to- day lives. | Provide specific guidance regarding adolescent and young adult self-monitoring of symptoms, household behaviors (ie, shared bathroom use), and similar actions. | |
| Preventing school/ university transmission | The contribution of regular, in-person school/university education to accelerating and sustaining population-level outbreaks of COVID-19 is insufficiently understood. | Clear, evidence-based, and stakeholder-informed prevalence thresholds and plans for stepwise openings and closures should be developed and communicated by schools and universities [S4]. |
| Evidence-based best practices for a safe return to in-person instruction are needed. | Evaluation and optimization of recommended mitigation measures in schools/universities are needed (ie, situate students at least 6 feet apart, reduce class sizes, minimize mixing between student class groups, assign permanent seating, use of outdoor spaces for classroom-related activities) [S5, S6]. | |
| Mobility patterns such as cross-country travel of out-of-state university students may reinvigorate SARS-CoV-2 transmission in communities with controlled local epidemics. | Robust quarantine strategies for traveling students represent an essential piece of university COVID-19 mitigation plans. Attendance of in-state universities may reduce travel-related spread of COVID-19. | |
| COVID-19 testing | Adolescence and young adulthood is a period of optimal health in which AYA infected with SARS-CoV-2 may be more likely to experience mild, no, or atypical symptoms, making timely identification and isolation of AYA with COVID-19 a challenge. | High-volume, high-frequency, and symptom-unspecific testing in at-risk AYA populations (eg, schools, universities) can reduce reproductive rates and account for the asymptomatic transmission potential among AYA [S7, S8]. |
| Frequent and widespread testing of asymptomatic AYA, for example, in school or university settings, may be cost-prohibitive and take up laboratory capacity. | Batch testing is scalable, cost-effective, and should be considered for school/university testing initiatives [S9, S10]. | |
| School and university testing may exclude vulnerable AYA who are often disconnected from educational institutions (eg, criminal justice-involved youth, pregnant or parenting youth, sexual/gender minority youth, youth with mental health issues). | Once available, point-of-care COVID-19 testing should be offered routinely in youth-serving health and social service organizations, particularly in vulnerable communities most heavily affected by COVID-19 [S11, S12]. | |
| Preventing family/ household transmission | AYA are more likely than older individuals to co-reside with others (eg, family members, roommates), increasing the risk of household transmission [S13]. | Evidence-based and specific guidance to minimize transmission within households and among families, particularly from AYA to parents and other family members, is needed. |
| There is limited guidance that addresses the needs of AYA residing in households within low socioeconomic status communities. | Community-involved initiatives to develop culturally appropriate, feasible, effective, and replicable COVID-19 mitigation strategies within socially and economically vulnerable households are warranted [S14–S16]. | |
| Vaccines and novel prevention and treatment methods | AYA are a key population for efforts to promote uptake of COVID-19 prevention methods that are currently under development, including vaccines, particularly given that vaccination rates among AYA remain low and have decreased during the COVID-19 pandemic [S17, S18]. | AYA participation in ongoing and future COVID-19 trials for vaccines, hyperimmune globulin and convalescent plasma therapy, pre-exposure and post-exposure prophylaxis is important. Behavioral interventions to promote the uptake of a novel COVID-19 vaccine as well as available influenza vaccines need to account for the unique needs of AYA. |
| The implications of SARS-CoV-2 infection for vulnerable AYA populations is insufficiently understood. | Vulnerable adolescent and young adult populations that warrant special attention in the development and evaluation of COVID-19 vaccines and novel prevention and treatment modalities include ethnic/racial minority AYA, pregnant youth, young substance users, and immunocompromised youth [S11, S19]. | |
| Long-term developmental and socioeconomic consequences | Social distancing recommendations are in conflict with normative AYA social development, contributing to increasing mental health problems among AYA. | To optimize adolescent and young adult social interactions, parents can be encouraged to spend additional time with their adolescent or young adult. Additionally, the seamless continuation of AYA behavioral health service delivery, remote or in person, is essential [S21, S21]. |
| COVID-19 control measures have disrupted AYA educational trajectories, thereby impacting long-term life trajectories and reducing life opportunities, particularly for socially vulnerable AYA. | Practical strategies to avoid adolescent and young adult disengagement in remote schooling, address technology/language barriers to online schooling, and ensure adequate learning environments at home are warranted. | |
| In the current recessionary economic climate, opportunities for AYA to enter the workforce are limited. | In the contemplated rollout of workforce-intensive COVID-19 mitigation initiatives, such as contact tracing, community-based testing, and public health messaging, AYA training and professional development programs for key positions such as community health workers, contact tracers, should be considered. | |
| COVID-19 prevention represents only 1 of many AYA health priorities that are shaping long-term adult health and well-being (eg, sexual and reproductive health, mental health) | Universal access to youth-friendly COVID-19, primary and specialty healthcare, and auxiliary services is imperative for reducing long-standing health disparities in the United States. Existing non-COVID-19 specialty services for AYA represent an opportunity for integration of COVID-19 mitigation strategies. |
References cited within this table are provided in the Supplementary Material.
Abbreviations: AYA, adolescents and young adults; COVID-19, coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2.
Considerations for AYA Testing
As part of the efforts to scale-up national, regional, and local COVID-19 testing capacities, targeted strategies for increasing the proportion of tests administered to AYA are warranted. To date, settings frequented by youth, including schools, households, and community settings, have not been prioritized as sentinel surveillance sites involved in the testing and contact tracing of asymptomatic or presymptomatic cases, despite lower health-seeking behavior among AYA. Of particular importance are public health plans that enable robust testing of students, their household contacts, and school staff after reopening. In addition, tailored strategies to identify and isolate priority contacts of infected students in school and university contexts are needed. Furthermore, schools and universities will have to ensure that online learning opportunities are maintained for quarantined students, in addition to regular in-person instruction.
Considerations for Averting AYA Household Transmission
Evidence suggests that SARS-CoV-2 is frequently transmitted among cohabiting household members and at family gatherings. The household secondary attack rate of SARS-CoV-2 is estimated to be 10.6% compared with less than 1% in hospital and community settings in the United States [29]. While additional data are needed to delineate the directionality of documented household transmissions (AYA to non-AYA vs non-AYA to AYA), it is important to note that AYA are more likely than older individuals to live with family members and will be more likely to have a disproportionately higher number of contacts with whom they have had prolonged, physically close indoor contact, potentially facilitating AYA to non-AYA SARS-CoV-2 transmission [30]. Furthermore, the risk of SARS-CoV-2 transmission from AYA to older individuals, who are vulnerable to severe COVID-19, may be increased in multigenerational households, particularly given that AYA are frequently employed in occupational settings that increase the risk of exposure to SARS-CoV-2. AYA aged 16–24 years make up 22% of the service industry workforce in the United States. Notably, AYA are markedly overrepresented in occupations with significant face-to-face human contact. For example, AYA represent approximately half of all cashiers and waiters in the United States [31].
Despite the importance of family and household contexts in facilitating the spread of SARS-CoV-2, limited guidance is provided for the prevention of asymptomatic or presymptomatic transmission in such settings. Further, the ability of AYA to maintain 6-foot distancing from sick or infectious household members as recommended may be limited as AYA are less likely to have control of family mitigation strategies. Particular attention should be given to ethnic/racial minority youth, who are more likely to live in multigenerational households and to work in the service sector.
Considerations for Leveraging Family Influence for COVID-19 Control
Research indicates that families and parents, in particular, matter in relation to AYA health behavior [32]. However, current public health messaging regarding COVID-19 only minimally addresses the parental role in influencing AYA behavior. Specific guidance for parents regarding communication and monitoring strategies that positively influence AYA health behavior in the context of COVID-19 is sorely needed.
Considerations for AYA Brain Development
Limited attention has been paid to the impact of COVID-19 and the associated immune system response on the developing AYA brain. Individuals infected with SARS-CoV-2 have presented with acute neuropsychiatric symptoms, including encephalopathy, stroke, and muscle weakness [33]. Several neuropsychological symptoms as early signs of COVID-19 have been identified, including the temporary loss of olfactory and gustatory perception, which may be common in AYA [34]. Furthermore, possible mechanisms for long-term neuroinvasive consequences of COVID-19 in youth have been described in the literature [35]. Increased attention should be given to the study of potential immediate and long-term effects of COVID-19 on the developing nervous system. Future research should also seek to determine whether SARS-CoV-2 infection can result in impairment to AYA decision-making and reduce adequate preventive behaviors.
Considerations of AYA’s Social Context
The sociodevelopmental context of AYA and its potential influence on SARS-CoV-2 transmission dynamics has received limited attention. AYA’s decisions regarding health behaviors are more likely to be shaped by immediate social and emotional benefits rather than by consideration of more distal health consequences [36], increasing the likelihood of nonadherence to social distancing [26]. This is of particular concern given that the gradual loosening of shelter-in-place measures will increase opportunities for AYA to engage in group interactions with peers in community settings that may facilitate transmission of SARS-CoV-2. Elevated contact rates [23] and increased likelihood of contacts not known by name represent potential challenges for effective contact tracing among AYA. However, novel mobile applications designed to facilitate COVID-19 contact tracing may represent an effective and AYA-friendly strategy.
Furthermore, adolescence and young adulthood are characterized as times when youth form romantic relationships that can be short in duration and at times concurrent. This structure of AYA romantic relationships may have implications for the transmission of SARS-CoV-2 among AYA. SARS-CoV-2 has been detected in the semen of male patients with active infection and after recovery [37] as well as in the vaginal fluid of female patients with active infection [38]. To date, sexual transmission of COVID-19 has not been shown, but sexual contact as a plausible mode of prolonged SARS-CoV-2 transmission after recovery from acute infection could warrant a renewed public health focus on barrier methods (ie, condoms) for AYA and needs to be explored further. Given that emerging evidence also indicates the presence of SARS-CoV-2 in saliva and feces [39, 40], extragenital anatomic sites as potential SARS-CoV-2 reservoirs warrant attention in efforts to prevent transmission among AYA.
CONCLUSIONS
The United States has initiated a step-wise reopening of the economy and public life, including the reopening of schools and universities and the hope that there will be adequate opportunities for AYA to enter the workforce. AYA have not been prioritized as a potential key population in the COVID-19 pandemic. Data suggest current estimates may inadequately reflect the importance of AYA in accelerating and sustaining COVID-19 outbreaks. These insights have important implications for improving and sustaining the effectiveness of the COVID-19 response. Specifically, consideration of factors unique to AYA should inform the design, communication, and implementation of control measures.
The United States is moving toward a “new normal,” where targeted COVID-19 control measures prioritize vulnerable populations as well as potential key populations for the forward transmission of SARS-CoV-2, such as AYA. Policymakers and public officials have to achieve a difficult balance, maximizing protection for those at greatest risk of severe infection while also minimizing disruptions to the economy and the educational, social, vocational, and developmental trajectories of AYA. Consideration of the needs of AYA is particularly important given the disproportionate impact of COVID-19 and the associated response measures on the lives of racial, ethnic minority, and socioeconomically disadvantaged youth, which threatens to exacerbate preexisting inequities in health outcomes, employment and overall socioeconomic opportunity, and overall AYA life chances. AYA represent the future of the United States, and the effectiveness and equity of the US response to the COVID-19 pandemic may shape the trajectory of the United States for years to come.
Supplementary Data
Supplementary materials are available at Clinical Infectious Diseases online. Consisting of data provided by the authors to benefit the reader, the posted materials are not copyedited and are the sole responsibility of the authors, so questions or comments should be addressed to the corresponding author.
Notes
Acknowledgments. The authors thank Dr Charles M. Cleland, biostatistician, NYU Langone Health, for his assistance and review of Figure 1.
Financial support. This work was supported by the William T. Grant Foundation–Reducing Inequality Initiative (189030) and the National Institutes of Health through funding for the Center for Drug Use and HIV Research (P30DA011041). The funding bodies did not influence the content or opinions expressed in this article.
Potential conflict of interest. V. G.-R. reports grants and personal fees from ViiV Healthcare outside the submitted work; he serves as a member of the US Presidential Advisory Council on HIV/AIDS and as the vice chair of the Latino Commission on AIDS Board of Directors. All other authors report no potential conflicts. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
References
- 1. Heavey L, Casey G, Kelly C, Kelly D, McDarby G. No evidence of secondary transmission of COVID-19 from children attending school in Ireland, 2020. Euro Surveill 2020; 25:2000903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. National Centre for Immunisation Research and Surveillance (NCIRS). COVID-19 in schools—the experience in NSW. New South Wales Government. Available at: http://ncirs.org.au/sites/default/files/2020-04/NCIRS%20NSW%20Schools%20COVID_Summary_FINAL%20public_26%20April%202020.pdf. Accessed 4 July 2020.
- 3. Kucirka LM, Lauer SA, Laeyendecker O, Boon D, Lessler J. Variation in false-negative rate of reverse transcriptase polymerase chain reaction–based SARS-CoV-2 tests by time since exposure. Ann Int Med 2020. doi: 10.7326/M20-1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Viner RM, Mytton OT, Bonell C, et al. . Susceptibility to and transmission of COVID-19 amongst children and adolescents compared with adults: a systematic review and meta-analysis. medRxiv 2020. doi: 10.1101/2020.05.20.20108126. [DOI] [Google Scholar]
- 5. Griffith G, Morris TT, Tudball M, et al. . Collider bias undermines our understanding of COVID-19 disease risk and severity. medRxiv 2020. doi: 10.1101/2020.05.04.20090506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Huang L, Zhang X, Zhang X, et al. . Rapid asymptomatic transmission of COVID-19 during the incubation period demonstrating strong infectivity in a cluster of youngsters aged 16–23 years outside Wuhan and characteristics of young patients with COVID-19: a prospective contact-tracing study. J Infect 2020; 80:e1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Liao J, Fan S, Chen J, et al. . Epidemiological and clinical characteristics of COVID-19 in adolescents and young adults. Innovation 2020; 1:100001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bai Y, Yao L, Wei T, et al. . Presumed asymptomatic carrier transmission of COVID-19. JAMA 2020; 323:1406–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lewis M, Sanchez R, Auerbach S, et al. . COVID-19 outbreak among college students after a spring break trip to Mexico—Austin, Texas, March 26–April 5, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:830–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Moore KA, Lipsitch M, Barry JM, Osterholm MT. The future of the COVID-19 pandemic: lessons learned from pandemic influenza. University of Minnesota Center for Disease Research and Policy. Available at: https://www.cidrap.umn.edu/sites/default/files/public/downloads/cidrap-covid19-viewpoint-part1_0.pdf. Accessed 4 July 2020.
- 11. Du Z, Xu X, Wu Y, Wang L, Cowling BJ, Meyers LA. Serial interval of COVID-19 among publicly reported confirmed cases. Emerg Infect Dis 2020; 26:1341–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bi Q, Wu Y, Mei S, et al. . Epidemiology and transmission of COVID-19 in 391 cases and 1286 of their close contacts in Shenzhen, China: a retrospective cohort study. Lancet Infect Dis 2020; 20:911–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ali ST, Wang L, Lau EH, et al. . Serial interval of SARS-CoV-2 was shortened over time by nonpharmaceutical interventions. Science 2020; 369:1106–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lauer SA, Grantz KH, Bi Q, et al. . The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Ann Int Med 2020; 172:577–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Byambasuren O, Cardona M, Bell K, Clark J, McLaws ML, Glasziou P. Estimating the extent of true asymptomatic COVID-19 and its potential for community transmission: systematic review and meta-analysis. SSRN 2020. doi: 10.2139/ssrn.3586675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. CDC COVID-19 Response Team (US). Coronavirus disease 2019 in children—United States, February 12–April 2, 2020. MMWR Morb Mort Wkly Rep 2020; 69:422–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Davies NG, Klepac P, Liu Y, et al. . Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med 2020; 26:1205–11. [DOI] [PubMed] [Google Scholar]
- 18. Huff HV, Singh A. Asymptomatic transmission during the COVID-19 pandemic and implications for public health strategies. Clin Infect Dis 2020. 2020;71(10):2752–2756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Riphagen S, Gomez X, Gonzalez-Martinez C, Wilkinson N, Theocharis P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 2020; 395:1607–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Centers for Disease Control and Prevention (US). COVIDView: a weekly surveillance summary of U.S. COVID-19 activity. Available at: https://www.cdc.gov/coronavirus/2019-ncov/covid-data/pdf/covidview-07-03.-2020.pdf. Accessed 15 July 2020.
- 21. New York State Governor’s Office. Amid ongoing COVID-19 pandemic, Governor Cuomo announces results of completed antibody testing study of 15 000 people showing 12.3 percent of population has COVID-19 antibodies. Available at: https://www.governor.ny.gov/news/amid-ongoing-covid-19-pandemic-governor-cuomo-announces-results-completed-antibody-testing. Accessed 4 July 2020.
- 22. Stringhini S, Wisniak A, Piumatti G, et al. . Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): a population-based study. Lancet 2020; 396:313–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Zhang J, Litvinova M, Liang Y, et al. . Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science 2020; 368:1481–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Munro APS, Faust SN. Children are not COVID-19 super spreaders: time to go back to school. Arch Dis Child 2020; 105:618–9. [DOI] [PubMed] [Google Scholar]
- 25. Bunyavanich S, Do A, Vicencio A. Nasal gene expression of angiotensin-converting enzyme 2 in children and adults. JAMA 2020; 323:2427–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Czeisler MÉ, Tynan MA, Howard ME, et al. . Public attitudes, behaviors, and beliefs related to COVID-19, stay-at-home orders, nonessential business closures, and public health guidance—United States, New York City, and Los Angeles, May 5–12, 2020. MMWR Morb Mortal Wkly Rep 2020; 69:751–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Viner RM, Russell SJ, Croker H, et al. . School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health 2020; 4:397–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cooper DM, Guay-Woodford L, Blazar BR, et al. . Re-opening schools safely: the case for collaboration, constructive disruption of pre-COVID expectations, and creative solutions. J Peds 2020; 223:183–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Burke RM, Midgley CM, Dratch A, et al. . Active monitoring of persons exposed to patients with confirmed COVID-19—United States, January–February 2020. MMWR Mor Mort Wkly Rep 2020; 69:245–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Park YJ, Choe YJ, Park O, et al. . Contact tracing during coronavirus disease outbreak, South Korea. Emerg Infect Dis 2020; 26. doi: 10.3201/eid2610.201315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. US Bureau of Labor Statistics. Employed persons by detailed occupation and age. Available at: https://www.bls.gov/cps/cpsaat11b.htm. Accessed 4 July 2020.
- 32. Dittus PJ, Michael SL, Becasen JS, Gloppen KM, McCarthy K, Guilamo-Ramos V. Parental monitoring and its associations with adolescent sexual risk behavior: a meta-analysis. Pediatrics 2015; 136:e1587–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Troyer EA, Kohn JN, Hong S. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain Behav Immun 2020; 87:34–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Mak PQ, Chung KS, Wong JS, Shek CC, Kwan MY. Anosmia and ageusia: not an uncommon presentation of COVID-19 infection in children and adolescents. Pediatr Infect Dis J 2020; 39:199–200. [DOI] [PubMed] [Google Scholar]
- 35. De Felice FG, Tovar-Moll F, Moll J, Munoz DP, Ferreira ST. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the central nervous system. Trends Neurosci 2020; 43:355–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hansen A, Turpyn CC, Mauro K, Thompson JC, Chaplin TM. Adolescent brain response to reward is associated with a bias toward immediate reward. Dev Neuropsychol 2019; 44:417–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Li D, Jin M, Bao P, Zhao W, Zhang S. Clinical characteristics and results of semen tests among men with coronavirus disease 2019. JAMA Netw Open 2020; 3:e208292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Scorzolini L, Corpolongo A, Castilletti C, Lalle E, Mariano A, Nicastri E. Comment of the potential risks of sexual and vertical transmission of Covid-19 infection. Clin Infect Dis 2020. 2020;71(16):2298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. To KK, Tsang OT, Yip CC, et al. . Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis 2020; 71:841–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Wang W, Xu Y, Gao R, et al. . Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 2020; 323:1843–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.