Abstract
Objective
To explore whether racial/ethnic differences in telehealth use existed during the peak pandemic period among NYC patients seeking care for COVID-19 related symptoms.
Materials and Methods
This study used data from a large health system in NYC – the epicenter of the US crisis – to describe characteristics of patients seeking COVID-related care via telehealth, ER, or office encounters during the peak pandemic period. Using multinomial logistic regression, we estimated the magnitude of the relationship between patient characteristics and the odds of having a first encounter via telehealth versus ER or office visit, and then used regression parameter estimates to predict patients’ probabilities of using different encounter types given their characteristics.
Results
Demographic factors, including race/ethnicity and age, were significantly predictive of telehealth use. As compared to Whites, Blacks had higher adjusted odds of using both the ER versus telehealth (OR: 4.3, 95% CI: 4.0-4.6) and office visits versus telehealth (OR: 1.4, 95% CI: 1.3-1.5). For Hispanics versus Whites, the analogous ORs were 2.5 (95% CI: 2.3-2.7) and 1.2 (95% CI: 1.1-1.3). Compared to any age groups, patients 65+ had significantly higher odds of using either ER or office visits versus telehealth.
Conclusions
The response to COVID-19 has involved an unprecedented expansion in telehealth. While older Americans and minority populations among others are known to be disadvantaged by the digital divide, few studies have examined disparities in telehealth specifically, and none during COVID-19. Additional research into sociodemographic heterogeneity in telehealth use is needed to prevent potentially further exacerbating health disparities overall.
Keywords: Telehealth, telemedicine, healthcare disparities, healthcare delivery
INTRODUCTION
The novel coronavirus of 2019 (COVID-19) global pandemic has disrupted the way healthcare is delivered in the United States. Essentially overnight, as part of efforts to reduce the transmission of COVID-19, 2 of the major previous barriers to telehealth use—poor financial reimbursement and low provider willingness1—were eliminated, thus massively speeding up adoption. On March 17, shortly after widespread stay-at-home orders were issued, the Center for Medicare and Medicaid Services (CMS) and commercial insurers made sweeping changes increasing telehealth coverage,2 and providers began promoting it as a way to provide medical services—including for COVID-related symptoms—while maintaining social distance. One recent study found urgent virtual video visits in New York City (NYC) increased by almost 700 percent from early March to mid-April, 56% of which were for COVID-related care.3
Using a dataset from a single health system in NYC (the initial epicenter of the US crisis), this study describes differential characteristics of patients seeking care related to COVID-19 during the peak pandemic period whose first encounter with the health system occurred via telehealth, an ER visit, or another modality. Documenting these differences is important given the sudden telehealth explosion and the nascent identification of racial disparities in COVID-19 prevalence and outcomes. While telehealth has many benefits, especially during a global pandemic, it may create and/or exacerbate health disparities.4 Research prior to the pandemic found that older Americans, rural communities, vulnerable populations, racial and ethnic minorities, and those with lower socioeconomic status (SES) status are all groups disadvantaged by the digital divide.5–7 However, apart from a few studies,8,9 the existing literature offers little analysis of the digital divide phenomenon applied to the subsector of telehealth. This gap is partially a result of minimal use of telehealth overall before COVID-19; 1 report found, among certain enrollees with employer-sponsored insurance, only 2.4% had utilized at least 1 telehealth service in 2018.10 Our findings are relevant to policy makers and health leaders interested in understanding the extent of differential utilization of telehealth in the context of COVID-19.
MATERIALS AND METHODS
The Mount Sinai deidentified COVID-19 database is a resource made available by the Mount Sinai Data Warehouse (MSDW) to promote research on COVID-19. The data contain all patients diagnosed with, placed under investigation for, or screened negative for COVID-19 with any Mount Sinai system provider starting March 20, 2020. We downloaded the data on May 18, 2020.
For context, it is important to understand the NYC environment during this time. The peak of the NYC pandemic (6370 new daily cases) occurred on April 6. Throughout the first half of the peak period, from early-March until mid-April, COVID-19 tests were only available in hospital emergency rooms (ERs), or their specially designated alternatives (ie, temporary assessment centers, tents, etcetera, set up in close physical proximity to ERs), as well as several publicly run community-based health centers and drive-thru test sites.11,12 Until late-April, physician offices and urgent care centers were operating in limited capacity and did not have testing available.13 However, health systems rapidly expanded video visits for online urgent care; patients seeking medical advice for COVID-related symptoms, but not necessarily an immediate test, could make a telehealth appointment. Moreover, tests were in short supply—essential workers, at-risk patients, and those showing moderate-to-severe symptoms were most likely to get tested. Patients going to the ER were likely to be sent home without being tested, depending on symptoms, medical history, and hospital capacity; and, given an extreme shortage in intensive care unit beds, only the sickest patients were admitted.12,14,15
For this study, we are interested in describing the characteristics of patients who sought care or testing voluntarily for COVID-19—either because of symptoms or potential exposure—via telehealth versus ER encounters versus office visits (We use telehealth as the broad term to cencompass basic and advanced communication.10). As just described, these sites were close substitutes during the peak-pandemic period,12,14–16 when even non-severe patients were using the ER to obtain COVID-19 testing, because tests were not widely available. In sensitivity analysis, we extend this comparison across more encounter types. We include only patients’ first encounters with the system, because we want to understand initial contact points for care. We also exclude patients who came to the hospital not through the ER—that is, those who were tested incidental to non-COVID care, such as women delivering babies in the labor and delivery unit. See the Supplementary online appendix for more details about classifying encounters.
Patient characteristics include race/ethnicity (Black, Hispanic, White, Asian, Other/Unknown), defined using a categorization scheme developed by the Mount Sinai Office for Diversity and Inclusion; age category (<18, 18–29, 30–49, 50–64, 65+), defined based on work by Pew Research Center;17 preferred language (English, Spanish, and Other/Unspecified); and a comorbidity index (0–3+), defined as an unweighted sum across the 18 conditions in our data and censored at 3. See the Supplementary online appendix for more details on the race/ethnicity categorization and comorbidity conditions.
Using multinomial logistic regression, we estimate the magnitude of the relationship between patient characteristics and the odds of having a first encounter via telehealth versus ER or office visit. We use parameter estimates from the regressions to predict patients’ probabilities of using different encounter types given their characteristics. In sensitivity analyses, we interact race/ethnicity with age and comorbidities and also broaden the number of encounter types.
RESULTS
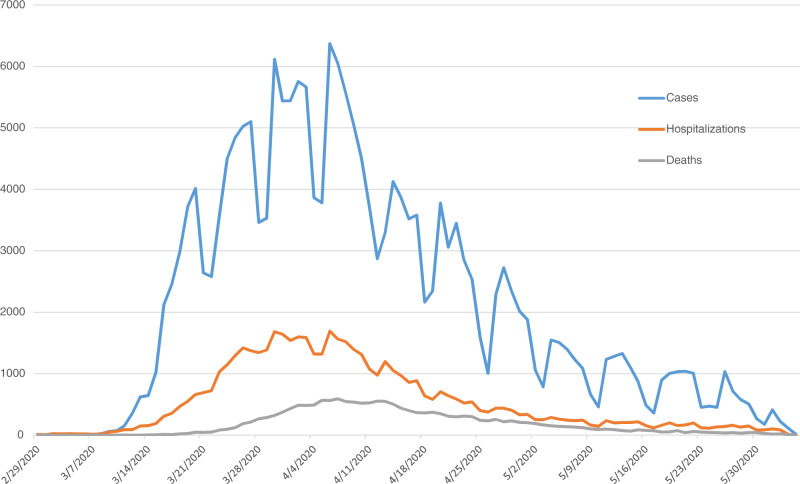
Our data contain 76 845 encounters for 52 585 unique patients diagnosed with, tested for, or placed under investigation for COVID-19 between March 20 and May 18, 2020. As seen in Figure 1, this time period encompasses the entirety of the NYC pandemic peak. Given data limitations, 4261 patients erroneously appear to have multiple first encounters, so for those we select one randomly. Applying inclusion criteria—omitting 13 356 patients (25.4%) who have an encounter other than by ER, outpatient office, or telehealth—there are 39 229 first encounters. Omitted first encounters consisted mostly of lab work and “orders only”; see Supplementary AppendixTable 1 for more details on encounters.
Figure 1.
Daily counts of COVID-19 cases, hospitalizations & deaths in NYC.
Source: Figure based on authors’ analyses of the Github database.
Note: This figure shows the number of confirmed cases by diagnosis date, hospitalizations by admission date, and deaths, by date of death, from COVID-19 on a daily basis since February 29, 2020. Given delays in reporting, which can take up to a week, recent data are incomplete.
Table 1.
Descriptive statistics of final sample
| Variable | Categories | Frequency | Percent (%) |
|---|---|---|---|
| Encounter Type | ER | 15 041 | 38.34 |
| Telehealth | 15 098 | 38.49 | |
| Office | 9090 | 23.17 | |
| Race/Ethnicity | Black or African-American | 7458 | 19.01 |
| White | 12 501 | 31.87 | |
| Hispanic/Latinx | 7471 | 19.04 | |
| Asian | 2310 | 5.89 | |
| Other/Unknown | 9489 | 24.19 | |
| Age | <18 | 4617 | 11.77 |
| 18–0 | 13 420 | 34.21 | |
| 30–<50 | 10 376 | 26.45 | |
| 50–<65 | 9626 | 24.54 | |
| 65+ | 1190 | 3.03 | |
| Comorbidity Sum | 0 | 22 934 | 58.46 |
| 1 | 7390 | 18.84 | |
| 2 | 3942 | 10.05 | |
| 3+ | 4963 | 12.65 | |
| Preferred Language | English | 35 235 | 89.82 |
| Spanish | 2617 | 6.67 | |
| Other/Unspecified | 1377 | 3.51 |
Source: Table based on authors’ analyses of the Mount Sinai deidentified COVID-19 database.
Note: Encounter type “Telehealth” classified based on expert guidance from the Mount Sinai Data Warehouse (MSDW), “Office” defined as where encounter type equaled “Office” or “Appointment.” Race/ethnicity classified based on scheme developed by the Mount Sinai Health System Office for Diversity and Inclusion. Comorbidity sum is the unweighted sum across the 18 conditions provided in our data. See Supplementary Appendix for more details on all variables.
Table 1 displays descriptive characteristics of the final sample; 38.3% of first encounters are via the ER, 38.5% are via telehealth, and 23.2% occur at an outpatient office. In terms of race/ethnicity, 19% of the patients in our data self-identify as Black or African-American, 19% as Hispanic/Latinx, 31.9% as White, 5.9% as Asian, and 24% as Other/Unknown. The majority of patients have zero (58.5%) or 1 (18.8%) comorbidities and list English as their preferred language (89.8%).
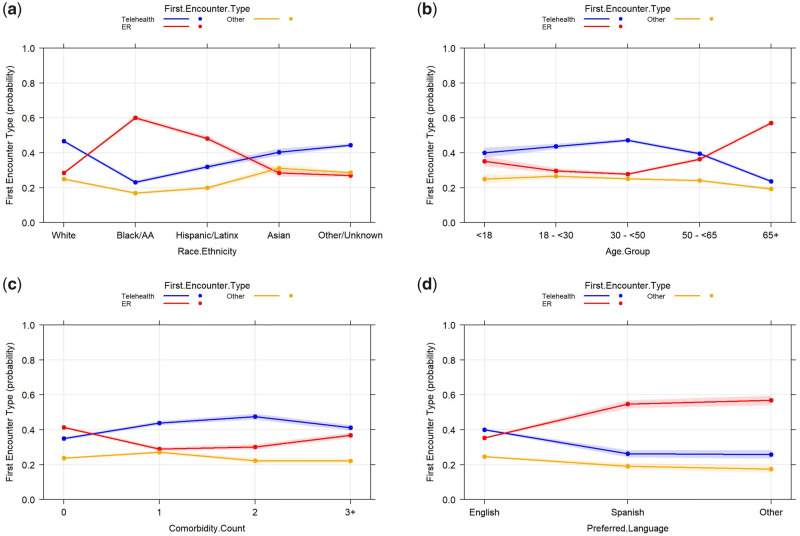
Figure 2 is derived from the multinomial regression. Figure 2a shows, after controlling for age, preferred language, and comorbidities, Whites and Asians have higher predicted probabilities (46.7% and 40.4%, respectively) of using telehealth during the pandemic than either the ER (28.4%, both), or an office visit (24.9% and 31.2%), while Blacks and Hispanics are most likely (60.1% and 48.2%) to use the ER than either telehealth (23.1% and 31.9%), or office (16.9% and 19.9%) visits. Figure 2b reflects findings from the digital divide literature3,18 that ages 18–49 have highest predicted probabilities of using telehealth (40.7% for 18–29-year olds, and 47.2% for 30–49-year olds), compared to those 65+ (23.7%). Figure 2d shows non-English speakers have a significantly lower predicted probability (26.2% for Spanish speakers and 25.8% for other language speakers) of using telehealth versus the ER.
Figure 2.
Predicted probabilities of encounter types for different patients.
Source: Table based on authors’ analyses of the Mount Sinai deidentified COVID-19 database.
Note: Figure based on parameter estimates from multinomial regression analyis of encounter type (ER vs telehealth vs office) on patient characteristics (race/ethnicity, age, preferred language, comorbidity sum).
Full regression parameter estimates (Table 2) show that the odds ratio (OR) for Blacks compared to Whites to use the ER versus telehealth is 4.3 (95% CI: 4.0–4.6) and the OR for Blacks compared to Whites to use an office visit versus telehealth is 1.4 (95% CI: 1.3–1.5). For Hispanics versus Whites, the analogous ORs are 2.5 (95% CI: 2.3–2.7) and 1.2 (95% CI: 1.1–1.3).
Table 2.
Multinomial regression results of encounter type (Telehealth vs ER vs Office) on patient characteristics
| Effect | Encounter type | OR point estimate | 95% Wald |
|
|---|---|---|---|---|
| Confidence limits | ||||
| Race Asian vs White | ER vs Telehealth | 1.156 | 1.031 | 1.297 |
| Race Asian vs White | Office vs Telehealth | 1.448 | 1.297 | 1.616 |
| Race Black or AA vs White | ER vs Telehealth | 4.275 | 3.98 | 4.591 |
| Race Black or AA vs White | Office vs Telehealth | 1.373 | 1.261 | 1.494 |
| Race Hispanic/Latinx vs White | ER vs Telehealth | 2.483 | 2.304 | 2.677 |
| Race Hispanic/Latinx vs White | Office vs Telehealth | 1.169 | 1.073 | 1.273 |
| Race Other/Unknown vs White | ER vs Telehealth | 0.999 | 0.934 | 1.069 |
| Race Other/Unknown vs White | Office vs Telehealth | 1.211 | 1.133 | 1.294 |
| Age 18–<30 vs 65+ | ER vs Telehealth | 0.281 | 0.256 | 0.309 |
| Age 18–<30 vs 65+ | Office vs Telehealth | 0.749 | 0.676 | 0.83 |
| Age 30–<50 vs 65+ | ER vs Telehealth | 0.243 | 0.226 | 0.262 |
| Age 30–<50 vs 65+ | Office vs Telehealth | 0.652 | 0.601 | 0.708 |
| Age 50–<65 vs 65+ | ER vs Telehealth | 0.381 | 0.355 | 0.408 |
| Age 50–<65 vs 65+ | Office vs Telehealth | 0.75 | 0.692 | 0.814 |
| Age <18 vs 65+ | ER vs Telehealth | 0.364 | 0.313 | 0.423 |
| Age <18 vs 65+ | Office vs Telehealth | 0.764 | 0.649 | 0.9 |
| Language Other/Unspecified vs English | ER vs Telehealth | 2.505 | 2.183 | 2.876 |
| Language Other/Unspecified vs English | Office vs Telehealth | 1.098 | 0.929 | 1.298 |
| Language Spanish vs English | ER vs Telehealth | 2.367 | 2.116 | 2.649 |
| Language Spanish vs English | Office vs Telehealth | 1.185 | 1.028 | 1.367 |
| Comorbidity Sum 1 vs 0 | ER vs Telehealth | 0.557 | 0.52 | 0.596 |
| Comorbidity Sum 1 vs 0 | Office vs Telehealth | 0.909 | 0.848 | 0.975 |
| Comorbidity Sum 2 vs 0 | ER vs Telehealth | 0.535 | 0.491 | 0.583 |
| Comorbidity Sum 2 vs 0 | Office vs Telehealth | 0.69 | 0.626 | 0.761 |
| Comorbidity Sum 3+ vs 0 | ER vs Telehealth | 0.754 | 0.694 | 0.819 |
| Comorbidity Sum 3+ vs 0 | Office vs Telehealth | 0.793 | 0.718 | 0.875 |
Source: Table based on authors’ analyses of the Mount Sinai deidentified COVID-19 database.
Note: Encounter type “Telehealth” classified based on expert guidance from the Mount Sinai Data Warehouse (MSDW), “Office” defined as where encounter type equaled “Office” or “Appointment”. Race/ethnicity classified based on scheme developed by the Mount Sinai Health System Office for Diversity and Inclusion. AA = African-American. Comorbidity sum is the unweighted sum across the 18 conditions provided in our data. See Supplementary Appendix for more details on all variables.
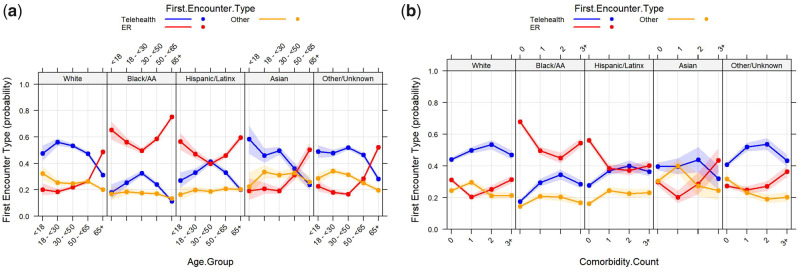
Figure 3 displays results from sensitivity analyses where we first interact race/ethnicity with age categories (Panel A) and then with the comorbidity sum (Panel B). Figure 3adisplays patterns across combinations of race/ethnicity and age. Blacks and Hispanics over 65 have lowest predicted probability (11.3%) of using telehealth among all patients. Complete results from the regressions generating those figures are found in Supplementary Appendix Exhibits 4 and 5; for example, the OR for Black versus White patients using the ER versus a telehealth appointment varies from 3.7 (95% CI: 3.3–4.2) for 30–49, to 8.6 (95% CI: 5.3–14.1) for those under 18.
Figure 3.
Predicted probabilities of encounter types for different patients across ages, or comorbidities.
Source: Table based on authors’ analyses of the Mount Sinai deidentified COVID-19 database.
Note: Figure based on parameter estimates from multinomial regression analyis of encounter type (ER vs telehealth vs office) on patient characteristics (race/ethnicity, age, preferred language, comorbidity sum), including interactions.
We also conduct a sensitivity analysis where we do not exclude other types of encounters and compare telehealth versus ER versus all other in-person visits. Relationships between patient characteristics across ER versus telehealth remain similar, except the ORs between telehealth and other in-person encounter types (eg, besides ER) for patients of different race/ethnicities are attenuated, though still marginally significant. The relative patterns, magnitudes, and significance of other variables do not significantly change. See Supplementary Appendix Exhibits 6–8.
DISCUSSION
In this paper we find that during the peak pandemic period, use of telehealth versus ER or office visits in NYC for COVID-related care significantly differed by patient characteristics. Of any age group, patients 65+ had the lowest odds of using telehealth versus other modalities. Black and Hispanic patients had higher adjusted odds of using either ER or office visits versus telehealth than either Whites or Asians.
A number of factors may contribute to our findings, such as research (prior to COVID-19) that racial/ethnic differences in ER use versus alternative care settings for a variety of conditions—differences that persist after controlling for variables like SES, insurance status, and usual-source-of-care.19–21 Also possible is that patients without a source of usual care (eg, a primary or specialty care physician) would be more likely to go to the ER and less likely to seek telehealth treatment through previously established care relationships. Furthermore, racial/ethnic disparities in patients’ prevalence and/or severity of COVID-1922 could be contributing—perhaps during the pandemic, Blacks and Hispanics use the ER more because they are sicker. These are elements we could not control for, given data limitations, but are exploring in further analysis.
However, the fact that we still find significant racial/ethnic disparities between outpatient office visits and telehealth indicate there may be other issues at play. Disparities in digital access, digital literacy, and telehealth awareness, as well as issues of cost and coverage and mistrust of digital appointments where physical examinations, labs, and vitals cannot be taken are all potential barriers to telehealth. Future research should explore these barriers in the context of the new telehealth explosion. Moreover, our findings of racial differences in telehealth use should be interpreted within the context of persistent structural racism in the US. We include race as a predictor in our model because documenting racial/ethnic differences for public awareness is a necessary first step in reducing disparities, however, we view race as a social construct. The formal and informal policies and interactions rooted in inequality, discrimination, oppression, and exclusion that underlie this construct and engender factors we hypothesize are contributing to our results should also be addressed in future research.23,24
Limitations must be acknowledged. Our data is from a single large health system; patients could have had previous encounters elsewhere. For example, it is possible that a patient had a telehealth or in-person (office, clinic, etcetera) visit outside the Mount Sinai system and were sufficiently sick that they were sent to the ER. In addition, insofar as the data is from 1 city in the early stage of the global pandemic, it is possible that our results are not generalizable to other regions or could wane over time. However, as other cities and countries navigate their own telehealth expansions, recognizing the potential for inequitable telehealth utilization may be helpful. Second, anecdotal reports suggest providers were not documenting all telehealth properly early on. Last, we only have a limited set of patient and clinical characteristics; for instance, we do not have access to patients’ zip codes or insurance status/type, although insurance coverage is generally high in NYC25—nor do we have reliable symptom/severity data.
CONCLUSION
The unprecedented speed with which providers are now adopting telehealth technology, the fact that telehealth insurance coverage changes are probably here to stay, and the number of patients who have now used it for the first time, means it is extremely likely that the percentage of patients choosing telehealth will remain high even after the pandemic ends. Policy makers and healthcare leaders must be careful to address sociodemographic heterogeneity in telehealth use to prevent further exacerbating disparities overall.
FUNDING
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
AUTHOR CONTRIBUTIONS
All authors contributed sufficiently and meaningfully to the conception, design, data acquisition or analysis, data interpretation, drafting, editing, and revising the manuscript. All authors approved the final version for submission and agreed to be accountable for all aspects of the work.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
This work was supported in part through the computational and data resources and staff expertise provided by Scientific Computing at the Icahn School of Medicine at Mount Sinai.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Smith AC, Thomas E, Snoswell CL, et al. Telehealth for global emergencies: implications for coronavirus disease 2019 (COVID-19). J Telemed Telecare 2020; 26 (5): 309–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.CMS. 2020. President Trump Expands Telehealth Benefits for Medicare Beneficiaries During COVID-19 Outbreak. March 17, 2020: Online. https://www.cms.gov/newsroom/press-releases/president-trump-expands-telehealth-benefits-medicare-beneficiaries-during-covid-19-outbreak Accessed July 17, 2020.
- 3. Mann DM, Chen J, Chunara R, et al. COVID-19 transforms health care through telemedicine: Evidence from the field. J Am Med Inform Assoc 2020; 27 (7): 1132–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Velasquez D, Mehrotra A.. Ensuring the growth of telehealth during covid-19 does not exacerbate disparities in care. Health Affairs Blog 2020; doi: 10.1377/hblog20200505.591306. [Google Scholar]
- 5. Yoon H, Jan Y, Vaughan PW, et al. Older adults’ internet use for health information: digital divide by race/ethnicity and socioeconomic status. J Appl Gerontol 2018; 39 (1): 105–10. [DOI] [PubMed] [Google Scholar]
- 6. Anderson M, Kumar M.. 2019. Digital divide persists even as lower-income Americans make gains in tech adoption. FactTank, Pew Research Center. https://pewrsr.ch/2vK1HIo Accessed July 17, 2020.
- 7. Perrin A, Turner E.. 2019. Smartphones help Blacks, Hispanics bridge some—but not all—digital gaps with Whites. FactTank, Pew Research Center. https://pewrsr.ch/2Z1PKPf Accessed July 17, 2020.
- 8. Sarkar U, Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc 2011; 18 (3): 318–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Goel MS, Brown TL, Williams A, Hasnain-Wynia R, Thompson JA, Baker DW.. Disparities in enrollment and use of an electronic patient portal. J Gen Intern Med 2011; 26 (10): 1112–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Weigel G, Ramaswamy A, Sobel L.. 2020. Opportunities and Barriers for Telemedicine in the U.S. During the COVID-19 Emergency and Beyond. Issue Brief, Kaiser Family Foundation. https://www.kff.org/womens-health-policy/issue-brief/opportunities-and-barriers-for-telemedicine-in-the-u-s-during-the-covid-19-emergency-and-beyond/ Accessed July 17, 2020.
- 11.NYC Health + Hospitals. 2020, March 19. Mayor De Blasio and NYC Health + Hospitals Expand Appointment Only COVID-19 Testing [Press release]. https://www.nychealthandhospitals.org/pressrelease/mayor-de-blasio-and-nyc-health-hospitals-expand-appointment-only-covid-19-testing/ Accessed July 17, 2020
- 12.Weill Cornell Medicine. March 25, 2020. COVID-19 Testing at Weill Cornell Medicine [News]. https://weillcornell.org/news/covid-19-testing-at-weill-cornell-medicine Accessed July 17, 2020.
- 13. Andrews M. April 6, 2020. NY Leads the Nation in COVID-19 Tests, But Testing Still Doesn't Meet Demand. Kaiser Health News https://khn.org/news/n-y-leads-the-nation-in-covid-19-tests-but-the-effort-still-lags-behind-demand/ Accessed July 17, 2020.
- 14. Italiano L. April 30, 2020. Getting a coronavirus test in NYC is about to get easier—finally. New York Post https://nypost.com/2020/04/30/getting-a-coronavirus-test-in-nyc-is-about-to-get-easier/ Accessed July 17, 2020.
- 15. Shulman R. March 19,2020. It took me 3 ER visits to get a coronavirus test in New York.” New York Times https://www.nytimes.com/2020/03/09/opinion/coronavirus-testing-new-york.html Accessed July 17, 2020.
- 16. Wosik J, Fudim M, Cameron B, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc 2020; 27 (6): 957–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Vogels EA, Perrin A, Rainie L, et al. 2020. 53% of Americans say the internet has been essential during the COVID-19 outbreak. Pew Research Center. https://www.pewresearch.org/internet/2020/04/30/53-of-americans-say-the-internet-has-been-essential-during-the-covid-19-outbreak/ Accessed July 17, 2020.
- 18. Perrin A, Duggan M.. 2015. Americans’ internet access: 2000–2015. Pew Research Center. https://www.pewresearch.org/internet/2015/06/26/americans-internet-access-2000-2015/ Accessed July 17, 2020.
- 19. Johnson PJ, Ghildayal N, Ward AC, et al. Disparities in potentially avoidable emergency department (ED) care. Med Care 2012; 50 (12): 1020–8. [DOI] [PubMed] [Google Scholar]
- 20. Law H-Z, Oraka E, Mannino DM.. The role of income in reducing racial and ethnic disparities in emergency room and urgent care center visits for asthma—United States, 2001–2009. J Asthma 2011; 48 (4): 405–13. [DOI] [PubMed] [Google Scholar]
- 21. Tang DH, Gilligan AM, Romero K.. Economic burden and disparities in healthcare resource use among adult patients with cardiac arrhythmia. Appl Health Econ Health Policy 2014; 12 (1): 59–71. [DOI] [PubMed] [Google Scholar]
- 22. Yancy CW. COVID-19 and African Americans. JAMA 2020; 323 (19): 1891–2. [DOI] [PubMed] [Google Scholar]
- 23. Holland PW. Causation and Race. Princeton, NJ: Educational Testing Service (RR-03-03); 2003.
- 24. Boyd RW, Lindo EG, Weeks LD, et al. On racism: a new standard for publishing on racial health inequities. Health Aff Blog 2020. doi: 10.1377/hblog20200630.939347 [Google Scholar]
- 25.US Census Bureau. QuickFacts. 2020. https://www.census.gov/quickfacts/newyorkcitynewyork Accessed July 17, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.