Abstract
Objective
Through the coronavirus disease 2019 (COVID-19) pandemic, telemedicine became a necessary entry point into the process of diagnosis, triage, and treatment. Racial and ethnic disparities in healthcare have been well documented in COVID-19 with respect to risk of infection and in-hospital outcomes once admitted, and here we assess disparities in those who access healthcare via telemedicine for COVID-19.
Materials and Methods
Electronic health record data of patients at New York University Langone Health between March 19th and April 30, 2020 were used to conduct descriptive and multilevel regression analyses with respect to visit type (telemedicine or in-person), suspected COVID diagnosis, and COVID test results.
Results
Controlling for individual and community-level attributes, Black patients had 0.6 times the adjusted odds (95% CI: 0.58–0.63) of accessing care through telemedicine compared to white patients, though they are increasingly accessing telemedicine for urgent care, driven by a younger and female population. COVID diagnoses were significantly more likely for Black versus white telemedicine patients.
Discussion
There are disparities for Black patients accessing telemedicine, however increased uptake by young, female Black patients. Mean income and decreased mean household size of a zip code were also significantly related to telemedicine use.
Conclusion
Telemedicine access disparities reflect those in in-person healthcare access. Roots of disparate use are complex and reflect individual, community, and structural factors, including their intersection—many of which are due to systemic racism. Evidence regarding disparities that manifest through telemedicine can be used to inform tool design and systemic efforts to promote digital health equity.
Keywords: telemedicine, disparities, COVID-19, racism, digital health
INTRODUCTION
Racial disparities in the COVID-19 pandemic have been clearly highlighted in the United States through the nonrepresentative morbidity and mortality rates in Black and Latinx populations across the nation.1,2 One study demonstrated increased risk of hospitalization for COVID-19 among Black patients as compared to white patients at a healthcare institution in San Francisco.3 Other work has concluded African Americans may have greater risk for COVID-19 given the higher burden of comorbidities such as diabetes and hypertension in these patients.1 While most studies have focused on risk of COVID-19 infection, hospital admissions, and in-hospital outcomes,4,5 barriers to timely diagnosis and appropriate care, knowledge, attitudes, and relationships with healthcare providers are well-documented factors related to healthcare disparities and outcomes across many health conditions.3,6–8 These are increasingly being recognized as important factors in COVID-19-related healthcare for Black, Latinx, and other communities of color. Identifying where, for whom, and how disparities manifest in the healthcare process is essential in order to inform effective healthcare and to better understand and address such factors.
Through the COVID-19 pandemic, telemedicine has become an essential entry point into the process of diagnosis, triage, and treatment in order to limit patient displacement to hospitals, allocate hospital capacity, and decrease the disease’s spread. While the promise of healthcare technologies such as telemedicine is great, the use of these technologies has the potential to exacerbate disparities via the “digital divide”—the disparate access to and utilization of technology and Internet among communities and populations of diverse race/ethnicity and socioeconomic demographics due to social, language, financial, and other barriers.9 While some research has shown that telemedicine can reduce healthcare inequities for patients in remote areas,10 other research suggests that the exacerbation of healthcare disparities may be an unintended consequence of large-scale deployment of telemedicine, with factors such as lower socioeconomic status and technology literacy leading to increased health disparities.11,12 Such factors have roots in racism, sexism, ageism, and their intersections; institutional racism and ageism are well-documented in in-person healthcare access and utilization contexts.13,14 Given the rapid changes in the healthcare environment during the COVID-19 pandemic, along with the consistent race and ethnic disparities in COVID-19 burden, it is critical to understand the contribution of telemedicine to augmenting or mitigating disparities.
To address this gap, here we use data from a large academic healthcare system with a robust telemedicine system15 in New York City to characterize access and subsequent care during a period of peak COVID-19 cases in 2020. We used data regarding encounters, diagnoses, and test results of those who access care through telehealth and otherwise, alongside community-level factors linked to patients’ home zip codes to identify disparities in patients’ healthcare seeking and diagnosis. The question of disparities in healthcare access through telemedicine are especially pertinent for the COVID-19 pandemic, a period when telemedicine became an integral part of the healthcare process.
MATERIALS AND METHODS
Setting
NYU Langone Health (NYULH), a large academic healthcare system in New York City, consists of 8077 healthcare providers across 4 hospitals and nearly 500 ambulatory locations all connected on a single electronic health record (EHR) system (Epic, Verona, WI). Prior to COVID -19, NYULH implemented telemedicine capabilities in approximately 25 locations. Its largest initiative was its virtual urgent care, a fully integrated video visit experience tightly integrated into its enterprise EHR and its patient portal. Patients accessing the virtual urgent care were able to check in, assess their insurance coverage in real time and pay, and have a video-enabled consultation with an NYULH emergency medicine physician that was reimbursed by multiple local payors. This system had been running since 2018 and on a typical day had < 100 visits across 5 states (New York, New Jersey, Pennsylvania, Connecticut, and Florida) managed by a pool of about 40 emergency department (ED) providers who took visits either on-site or at home. Patients access these virtual services through the NYULH app built upon the Epic MyChart suite of patient tools.
Ethical review
This study was deemed part of quality improvement and all data was collected as part of routine care. Ethics review and informed consent were not sought because the study met criteria for exemption from such review according to NYULH institutional policy.
Data
All patients with a NYC home zip code who accessed care from March 19 (the start of expanded video for ambulatory visits, “non urgent care”) to April 30, 2020, as May 1, 2020 is when office visits restarted at NYULH. We also accessed data for all patients with a NYC home zip code who accessed care during March 19 to April 30, 2019 for initial descriptive statistics and reference in how telemedicine was used prior to the pandemic, as described below.
Outcomes
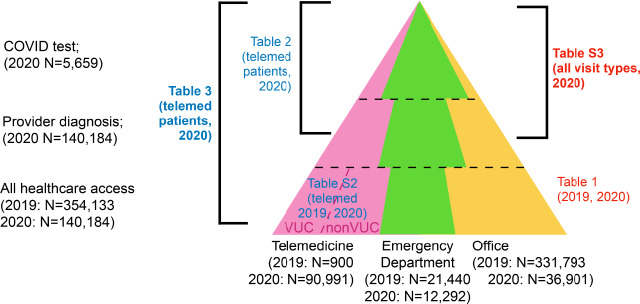
As there are multiple places where disparities may manifest in the healthcare process (eg, accessing care, being diagnosed, and receiving a COVID test result, visualized in Figure 1), the following main outcomes were considered for descriptive statistics and regression analyses:
Figure 1.
Overview of places where disparities may manifest through healthcare access, provider diagnoses, and testing process. Sample sizes for each visit type and healthcare process by year are provided. Each analysis and the corresponding Table where results are reported are also indicated. Red font/tables listed on right side used for analyses on data from all patients; blue font/tables on left side represent analyses on telemedicine patients only. Bold font used to indicate regression analyses. Triangle sizes are for illustration only.
Type of visit (telemedicine—virtual urgent care and nonurgent care versus office or emergency department).
Provider diagnosis code in the EHR (suspected COVID-related versus unrelated, irrespective of COVID testing).
Test results for telemedicine patients who were tested (COVID positive versus negative).
Type of visit is noted in the EHR. Telemedicine encounters were categorized into 2 groups: 1) urgent care and 2) nonurgent ambulatory care visits. For diagnosis, we captured COVID-suspected visits by considering diagnosis codes containing relevant respiratory issues via partial matching with any of the following keywords: 1) COVID, 2) RESP, 3) FLU, 4) PNEU, 5) FEVER, 6) SHORTNESS OF BREATH, 7) COUGH, 8) DYSPNEA, 9) PHARYNGITIS, 10) BRONCHITIS, 11) SINUSITIS, 12) URI. Tested patients are those who first had an NYU visit and who received a SARS-COV-2 virus by PCR (polymerase chain reaction) test at NYULH. Of those patients, those who had at least 1 positive result from the SARS-COV-2 virus by PCR test are included as COVID positive.
Individual-level variables
For all individuals, in both 2020 and 2019, we obtained relevant demographic, social, and comorbidity information based on a priori clinical significance to COVID from the EHRs: age at time of call, gender, race as reported by the patient (aggregated into White, African American, Asian, other, and unknown), ethnicity as reported by the patient (Latinx or non-Latinx), any past cardiac history (as defined by a history of hypertension, hyperlipidemia, coronary artery disease or heart failure), any past pulmonary disease (as defined by chronic obstructive pulmonary disease or asthma), and preferred language.16,17 For the race/ethnicity variables, because patients are allowed to select more than 1 race/ethnicity category, we grouped patients in the race category for those who only picked that 1 category. If multiple categories were selected, we put the patient in the “multiple” race category. Patients who declared Latinx race or ethnicity were assigned to the Latinx category.
Zip-code level variables
We also considered community-level variables as independent variables in order to identify if there were any disparities related to community-level characteristics. From the American Community Survey (latest data from 2018) we obtained the following variables to capture area-level measures with a priori significance to COVID: population, ratio of women to men (all ages), percent Hispanic or Latinx of any race, percent white (alone or in combination), percent Black or African American (alone or in combination), percent Asian (alone or in combination), median household income, educational attainment—bachelor’s degree or higher, and average household size.16,18,19Zip-code was the geographic unit used as it provides a balance between larger county geographic units where spatial heterogeneity would be lost—but there is a clearer contextual understanding given the history of geographic marginalization in NYC—and smaller census tracts which may lose the community-level aspects of consideration and would each represent smaller samples from our population.20,21
Statistical analysis
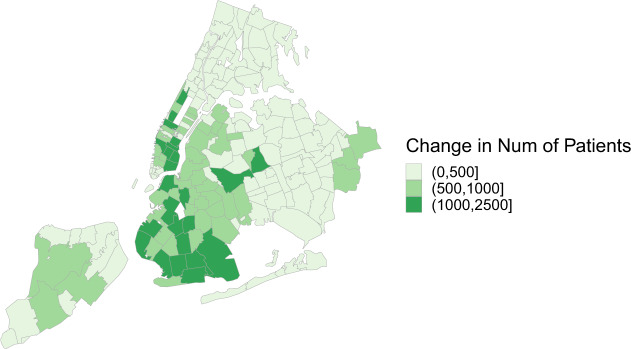
We first visualized the change in spatial distribution of telemedicine calls for the study dates, from 2019 to 2020, by zip code. Next, we summarized the proportion of each race/ethnicity group that had an office visit, an ED visit, and a telemedicine visit.
We then summarized the count and proportion of patients for each age, gender, race, comorbidity, and preferred language category for both 2019 and 2020 data by each visit type (telemedicine, office visit, emergency department). Differences between 2019 and 2020 for telemedicine visits were computed for each variable category, along with confidence intervals. Next we computed the count and proportion of patients for the outcomes above: telemedicine calls, with COVID or non-COVID suspected diagnosis, and results of telemedicine callers COVID tests (positive versus negative) for the 2020 data across the individual-level variables described above (means and standard deviation for age, count and proportion for all other variables). Differences in each COVID positive versus negative suspected diagnosis and COVID positive versus negative test across all variable categories were computed. As supplementary analyses, we computed count and proportion for categorical variables groups and mean and standard deviation across virtual urgent care and nonvirtual urgent care telemedicine visits for both 2019 and 2020, across all individual-level variables. Differences between 2019 and 2020 for virtual urgent care were computed. In all analyses, Chi-squared tests were used for differences for all categorical variables. For age, which was the only continuous variable, we used quantile-quantile plots and the Shapiro-Wilk test to first confirm normal distribution, and thus the 2-sample t-test was used to compute differences. Confidence intervals were computed using the Wald method.
The association between each of the 3 main outcomes above (type of visit; telemedicine versus office or emergency department, provider diagnosis of suspected COVID related versus unrelated, and COVID test result positive versus negative for patients who were tested) and patient-level and community-level covariates were analyzed with multilevel logistic regression models with random intercepts for 2020 data. Both individual-level and community-level covariates were assessed, as they represent levels of influence that impact health outcomes through a variety of mechanisms.22 Age was centered and community-level variables were standardized. Nine community-level variables which have been relevant in infectious disease outcomes were initially identified and assessed in the model: ratio of women to men, percent Hispanic/Latinx, percent white, percent Black, percent Asian, median household income, labor force participation rate for females 16 years and older, number of people with bachelor’s degree or higher and average household size.19,23,24 In the final model 5 community variables remained: ratio of women to men, percent of Hispanic/Latinx, median household income, number of people with Bachelor’s degree or higher, and average household size, based on variance inflation factor (VIF < 2.5) to ensure noncollinearity.25 After eliminating variables due to collinearity, we find that the remaining community-level characteristics do indeed capture factors not represented at the individual level.
As supplementary analyses, we also implemented the same multilevel logistic analysis for outcomes of: provider diagnosis of suspected COVID-related versus unrelated, COVID test result positive versus negative for patients who were tested, and if a patient got tested at NYULH or not, for patients of all visit types during the 2020 time period. This enabled us to compare likelihood of diagnoses and test result for those who accessed care through telemedicine compared to all patients. As well, it enabled us to assess the likelihood of someone getting tested at NYULH in relation to individual and community-level factors. Lastly, as another supplementary analysis to better understand how the Black population accessed care at our institution during the peak COVID period, we computed the mean age of all Black patients as well as proportion of those who were female, who had a cardiac history, and who had a pulmonary history for those who sought care via telemedicine and in person in 2020. Differences between telemedicine and in-person for each variable category were also computed.
All statistical analyses were performed using the R statistical software version 4.0.0; regression was performed using lme4 library, and all maps and figures were generated using the ggplot2 and chloropleth libraries.
RESULTS
Figure 1 illustrates all analyses and in which Tables results are reported. Demographics of patients by visit type for March 19–April 30, 2019 and 2020 are first summarized in Table 1. During March 19, 2020 to April 30, 2020, 140 184 patients visited NYULH for any reason, which was a decrease compared to the same time period in 2019 (354 138 patients) (Supplementary Table S1). The proportion of patients who used telemedicine in 2020 versus 2019 was significantly increased from 0.25% (95% confidence interval [CI], 0.24% to 0.27%) to 64.6% (95% CI, 64.4% to 64.9%) (Table 1), representing an increased geographic spread of the home locations of patients reached (Figure 2). The mean age of patients using telemedicine in 2020 went up from 40.7 years (standard deviation [SD]: 13.7) in 2019 to 47.3 years (SD: 19.8) a difference of 6.5 years (95% CI, 5.6–7.4 years), and the proportion of men using telemedicine increased from 33.3% to 39.3% a difference of 5.9% (95% CI, 2.9% to 9.0%). The proportion of telemedicine visits by white patients decreased from 2019 to 2020, from 53.3% to 51.1%, a difference of −2.2% (95% CI, −5.5% to 1.0%), while those by Black patients increased from 8.0% to 12.9%, a difference of 4.9% (95% CI, 3.1% to 6.7%) respectively (Table 1). Subsequent subgroup analysis showed that this difference was driven by a younger (20–45) and more female population (69.8%) compared to nontelemedicine visits in 2020 (57.9%), a difference of −11.9% (95% CI, −13.3% to −10.6%) (Supplementary Table S4) as well as compared to telemedicine visits in 2019 (Supplementary Figure S1). Overall, the total proportion of patients at NYULH who are Black also increased from 2019 to 2020 across all visit types; the proportion of in-person visits went from 10.4% in 2019 to 16.9% a difference of 6.5% (95% CI, 6.1% to 6.9%) (office) and from 14.5% in 2019 to 16.5%, a difference of 2.0% (95% CI, 1.2% to 2.8%) (ED) (Table 1). The proportion of telemedicine visits which were for virtual urgent care versus nonurgent care is further described in Supplementary Table S2, and it should be noted that the proportion of Black patients seeking virtual urgent care went from 8.7% to 13.3%, an increase of 4.6% (95% CI, 2.6% to 6.7%) from 2019 to 2020.
Table 1.
Demographics of patients by visit type for March 19–April 30, 2019 and 2020. Differences are in the same units as values in the same row
| 2019 Total Visit (N = 354 133) |
2020 Total Visit (N = 140 184) |
Difference between 2019 and 2020 (Telemedicine) |
|||||
|---|---|---|---|---|---|---|---|
| Office (N = 331 793) | ED (N = 21 440) | Telemed (N = 900) | Office (N = 36 901) | ED (N = 12 292) | Telemed (N = 90 991) | Difference (95% CI) | |
| Age in years (mean, SD) | 51.0 (23.3) | 42.3 (24.0) | 40.7 (13.7) | 48.6 (23.5) | 49.6 (21.2) | 47.3 (19.3) | 6.5 (5.6–7.4) |
| Male (%) | 41.7 | 46.9 | 33.3 | 44.2 | 54.4 | 39.3 | 5.9 (2.9–9.0) |
| Race/ ethnicity (%) | |||||||
| White | 61.5 | 42.5 | 53.3 | 47.9 | 37.9 | 51.1 | −2.2 (−5.5–1.0) |
| Black | 10.4 | 14.5 | 8.0 | 16.9 | 16.5 | 12.9 | 4.9 (3.1–6.7) |
| Latinx | 1.2 | 1.4 | 3.2 | 1.3 | 1.4 | 2.0 | −1.2 (−2.4– −0.1) |
| Asian | 4.7 | 7.0 | 6.6 | 5.8 | 6.7 | 5.3 | −1.3 (−2.9–0.3) |
| Other | 9.3 | 25.5 | 9.3 | 15.3 | 28.9 | 12.4 | 3.1 (1.1–4.9) |
| Multiple | 1.1 | 1.1 | 3.0 | 1.1 | 1.3 | 1.7 | −1.3 (−2.4– −0.2) |
| Unknowna | 11.7 | 8.0 | 16.6 | 11.7 | 7.3 | 14.7 | −1.9 (−4.3–0.6) |
| Cardiac History (%) | 51.1 | 33.1 | 30.1 | 53.8 | 43.4 | 49.1 | 19.0 (16.0–22.0) |
| Pulmonary History (%) | 15.1 | 15.5 | 16.6 | 17.6 | 16.0 | 19.4 | 2.8 (0.4–5.3) |
| Preferred Language (%) | |||||||
| English | 87.3 | 81.7 | 92.3 | 73.5 | 77.1 | 89.7 | −2.6 (−4.4– −0.9) |
| Spanish | 5.7 | 11.3 | 1.0 | 15.3 | 15.6 | 3.7 | 2.7 (2.0–3.4) |
Abbreviations: ED, emergency department; SD, standard deviation.
4834 patients had missing data for race and are grouped in the unknown category.
Figure 2.
New York City map illustrating the change from March 19–April 30 2019 to the same time period in 2020 of number of telemedicine patients shaded by the patients’ home zip codes.
In terms of other subgroups, the proportion of telemedicine patients who were Asian decreased from 2019 to 2020, 6.6% to 5.3%, a difference of −1.3% (95% CI, −2.9% to 0.3%); while in-person office visits for this group increased from 4.7% to 5.8%, a difference of 1.1% (95% CI, 0.9% to 1.4%) and ED visits decreased from 7.0% to 6.7%, a difference of −0.3% (95% CI, −0.8% to 0.3%). Distribution of patient demographic attributes by all visit types in 2019 and 2020 are summarized in Table 1 and the distribution of visit types by race group in Supplementary Table S1. The proportion of those with cardiac history increased in all visit types with telemedicine visits demonstrating the largest increase from 30.1% to 49.1%, a difference of 19.0% (95% CI, 16.0% to 22.0%). Visits with a patient with a pulmonary history also increased for all visit types with the increase in telemedicine visits going from 16.6% to 19.4%, a difference of 2.8% (95% CI, 0.4% to 5.3%).
Next, Table 2 summarizes demographics of the telemedicine cohort (N = 90 991) based on who were assigned a COVID-suspected diagnosis, and of those telemedicine patients who were tested, the test results (N = 5659). In 2020, of all the telemedicine calls, 28 908 (31.8%) were given a COVID-suspected diagnosis by the physician, and the remaining were deemed non-COVID 62 083 (68.2%). The proportion of patients with a positive COVID test who were Black compared to the proportion who were given a COVID-suspected diagnosis at a telemedicine call who were Black were greater (21.0% compared to 13.4%), whereas for proportions who were White, this was 49.5% compared to 36%.
Table 2.
Descriptive statistics by age, gender, race, comorbidities, and preferred language for outcomes of telemedicine calls and test results of telemedicine patients (March 19–April 30, 2020)
| Suspected COVID Diagnosis Code (N = 90 991) |
Test results (N = 5659) |
|||||
|---|---|---|---|---|---|---|
| Non-COVID (N = 62 083) |
COVID (N = 28 908) |
Difference (95% CI) | COVID neg (N = 3598) |
COVID pos (N = 2061) |
Difference (95% CI) |
|
| Age (mean, SD) | 47.2 (20.2) | 47.4 (17.2) | 0.2 (−0.4–0.1) | 45.9 (17.9) | 48.6 (16.6) | 2.7 (1.8–3.6) |
| Male (%) | 39.4 | 39.0 | −0.4 (−0.3–1.1) | 31.6 | 39.3 | 7.7 (5.1–10.3) |
| Race/ ethnicity (%) | ||||||
| White | 51.8 | 49.5 | −2.3 (−3.0– −1.6) | 45.4 | 36.0 | −9.4 (−12.0– −6.8) |
| Black | 12.6 | 13.4 | 0.8 (0.3–1.2) | 14.3 | 21.0 | 6.7 (4.6–8.8) |
| Latinx | 1.9 | 2.1 | 0.2 (0.1–0.4) | 3.3 | 3.5 | 0.2 (−0.8–1.1) |
| Asian | 5.2 | 5.4 | 0.2 (−0.1–0.1) | 8.6 | 6.5 | −2.1 (−3.5– −0.7) |
| Other | 12.4 | 12.3 | −0.1 (−0.1–0.4) | 15.4 | 20.8 | 5.4 (3.3–7.5) |
| Multiple | 1.8 | 1.6 | −0.2 (−0.3–0.05) | 2.1 | 1.6 | −0.5 (−1.2–0.3) |
| Unknown | 14.3 | 15.6 | 1.3 (0.8–1.8) | 10.9 | 10.6 | −0.3 (−1.9–1.4) |
| Cardiac History (%) | 48.3 | 51.0 | 2.7 (2.1–3.5) | 47.9 | 51.3 | 3.4 (0.7–6.2) |
| Pulmonary History (%) | 18.3 | 21.8 | 3.5 (2.9–4.1) | 23.8 | 20.7 | −3.1 (−5.3– −0.9) |
| Preferred Language (%) | ||||||
| English | 89.6 | 89.9 | 0.3 (−0.1–0.7) | 92.7 | 90.6 | −2.1 (−3.7– −0.6) |
| Spanish | 4.3 | 2.5 | −1.8 (−2.0– −1.6) | 2.6 | 4.9 | 2.3 (1.2–3.3) |
Abbreviations: CI, confidence interval; SD, standard deviation.
Note: Differences are in the same units as values in the same row.
Table 3 reports the multilevel regression results for the 3 main outcomes (telemedicine access, COVID diagnosis, and test results for telemedicine patients). Though the proportion of patients that are diagnosed with COVID are less likely to be Black, controlling for individual and community-level characteristics, patients that are Black are more likely to test positive, adjusted odds ratio [aOR] of 1.63 (95% CI, 1.36–1.94), more likely to be diagnosed with suspected COVID after a telemedicine call aOR of 1.07 (95% CI, 1.02–1.13), and less likely to use telemedicine aOR of 0.60 (95% CI, 0.58–0.63). In comparison, patients that are black were less likely to be diagnosed with COVID after a visit when considering all in-person and telemedicine visit types together, aOR of 0.91 (95% CI, 0.87–0.95). Being female also had increased odds for use of telemedicine, aOR of.45 (95% CI, 1.41–1.48) while preferred language Spanish had decreased adjusted odds, aOR of 0.46 (95% CI, 0.43–0.49). Notably, age did not have increased or decreased odds for the use of telemedicine, aOR of 0.99 (95% CI, 0.99–0.99). Of the community-level factors, an increase in the mean income of patient’s home address zip code had a negative association with the adjusted odds of a positive COVID test [aOR of 0.89 (95% CI, 0.82–0.97)] and an adjusted odds of telemedicine use of 1.19 (95% CI, 1.12–1.25). Median household size had positive odds of a positive COVID test (aOR of 1.28, 95% CI, 1.10–1.50) and decreased odds of using telemedicine (aOR of 0.72, 95% CI, 0.65–0.80). The same multilevel regression analysis, when considering patients of all visit types (telemedicine, office and ED) in 2020, is illustrated in Supplementary Table S3; and notably, Black patients were less likely to be given a suspected COVID diagnosis when considering all visit types (aOR of 0.91, 95% CI , 0.87–0.95), though they were more likely when just considering the telemedicine patients (aOR of 1.07, 95% CI, 1.02–1.13).
Table 3.
Multilevel regression results for 3 main outcomes among telemedicine patients
| Variables | Telemedicine Use (N = 90 991) | COVID-suspected Diagnosis (N = 90 991) | COVID Test (N = 5659) |
|---|---|---|---|
| Fixed Effect | Adjusted Odds Ratio | Adjusted Odds Ratio | Adjusted Odds Ratio |
| Individual Level | |||
| Age | 0.99 (0.99–0.99) | 1.00 (1.00–1.00) | 1.01 (1.01–1.02) |
| Female | 1.45 (1.41–1.48) | 1.03 (1.00–1.06) | 0.69 (0.61–0.78) |
| Race/ethnicity | |||
| White | Ref | Ref | Ref |
| Black | 0.60 (0.58–0.63) | 1.07 (1.02–1.13) | 1.63 (1.36–1.94) |
| Asian | 1.17 (1.06–1.29) | 1.16 (1.05–1.29) | 0.99 (0.79–1.25) |
| Latinx | 0.81 (0.77–0.86) | 1.06 (0.99–1.13) | 1.18 (0.86–1.63) |
| Other | 0.76 (0.73–0.79) | 1.09 (1.04–1.14) | 1.53 (1.29–1.81) |
| Multiple | 1.17 (1.06–1.30) | 0.95 (0.85–1.06) | 0.99 (0.65–1.53) |
| Unknown | 1.18 (1.14–1.23) | 1.16 (1.11–1.21) | 1.25 (1.03–1.52) |
| Cardiac History | 1.18 (1.15–1.22) | 1.12 (1.09–1.16) | 0.88 (0.77–1.01) |
| Pulmonary History | 1.14 (1.11–1.18) | 1.26 (1.22–1.30) | 0.81 (0.70–0.93) |
| Language preference | |||
| English | 1.57 (1.50–1.64) | 0.87 (0.83–0.93) | 1.06 (0.81–1.39) |
| Spanish | 0.46 (0.43–0.49) | 0.50 (0.46–0.56) | 1.49 (0.99–2.22) |
| Community Level | |||
| Median household income | 1.19 (1.12–1.25) | 1.00 (0.96–1.03) | 0.89 (0.82–0.97) |
| Percent Hispanic | 4.12 (3.02–5.62) | 1.19 (0.98–1.45) | 1.16 (0.73–1.85) |
| Bachelor’s degree or higher | 0.98 (0.93–1.04) | 0.98 (0.95–1.01) | 0.98 (0.82–1.07) |
| Median Household Size | 0.72 (0.65–0.80) | 1.06 (0.99–1.13) | 1.28 (1.10–1.50) |
| Women to Man Ratio | 1.19 (0.78–1.80) | 0.89 (0.68–1.16) | 1.75 (0.89–3.43) |
| Random Effect | 0.084 | 0.022 | 0.023 |
DISCUSSION
Summary of main findings
In this prospective cohort study, which included 140 184 patients who sought care at NYULH during the acute pandemic period (between March 19, 2020 and April 30, 2020), we found that the proportion of Black patients accessing care through telemedicine increased compared to the same time period in 2019. Supplementary analysis showed that this change was driven primarily by a younger and more female population. However, after controlling for individual and community-level attributes of telemedicine patients, Black patients were significantly less likely to access care through telemedicine compared to white patients in 2020, aOR 0.60 (95% CI, 0.58–0.63). These adjusted odds of Black patients using telemedicine as compared to in-person office or ED visits in comparison to white patients was also lower than that of other race/ethnicity groups (Table 3). Having accessed care, the odds of a suspected COVID diagnosis after a visit was higher for Black patients who access care through telemedicine compared to white patients, aOR 1.07 (95% CI, 1.02–1.13), and lower compared to white patients when considering in-person and telemedicine visits, aOR 0.91 (95% CI, 0.87–0.95). Further, of the patients who accessed care through telemedicine, and were subsequently tested at NYULH, the odds of a Black patient testing positive for the virus (of those who got tested) were increased compared to white patients, aOR 1.63 (95% CI, 1.36–1.94). Considered together, these findings suggest that, while Black patients accessed telemedicine at higher numbers during the acute pandemic period than prior, they are utilizing at lower levels when compared to white patients and may be sicker when seeking care through telemedicine compared to white patients. We conclude this because Black patients are more likely to receive a suspected COVID diagnosis after a visit, and also to test positively if tested. It could also be that white patients are more likely to get tested, which could be because of easier access or due to access based on concern, information seeking, or a milder illness that may or may not be COVID. Finally, it should be noted that in supplementary analyses, we observed that the proportion of patients seeking urgent care through telemedicine from 2019 to 2020 who are Black increased by 4.6% (95% CI, 2.6% to 6.7%), while the percent seeking care through the ED increased by 2.0% (95% CI, 1.2% to 2.8%) showing increased use of telemedicine for urgent care by Black populations.
Comparison to existing literature
Racial and ethnic disparities in healthcare have been well-documented in COVID-19, specifically with respect to risk of infection and in-hospital outcomes once admitted.4,5 While recent research has found significant disparities in COVID-19-related healthcare among specific populations—including Black, Latinx, migrant workers, and elderly—much of the focus on this work has been on outcomes, access, and equity in in-person care. As yet, we have not seen any studies empirically demonstrating how the disparities faced by these populations have been impacted by virtual care services such as telemedicine during the pandemic. Overall, our study adds to the literature through an investigation of disparities, specifically related to healthcare access through telemedicine use, during a period when the impetus for remote healthcare access was high.
Our institution is uniquely suited to explore the impact of race, racism, and digital disparities on telemedicine given its well-developed digital health infrastructure, including digital patient platforms, high levels of patient portal (MyChart) participation, and robust telemedicine program. These programs were heavily invested in and socialized to patients during both the prepandemic and acute pandemic period.26 As a result of this investment, the potential for confounding of telemedicine technical capacities (such as technical glitches, compatibility/interoperability challenges, and provider technical competence) from an institutional perspective was likely minimized.15 Our work suggests that disparate access to and utilization of digital healthcare technologies is driven, at least in part, by features and processes beyond the digital infrastructure limitations of healthcare systems (such as the availability of telemedicine-capable clinicians), and further suggests that the mere availability of digital health services may not be enough to address disparities in digital access and utilization. Similarly, the high rates of insured patients in our population (as compared to city averages) suggest that the disparities we observe are unlikely to be linked solely to insurance status or coverage type. This conclusion is supported by findings of disparities in COVID-related infections and deaths across several metropolitan areas, although the study only considered community-level factors.27
Moreover, the observed intersectionality of disparities,14 that is, in Black and older patients, echoes well-documented challengesin healthcare due to institutional sexism and ageism (due to bias and cultural competencies among providers, access to resources, and other reasons);13,28 and again our study highlights that these forces manifest in healthcare access via telemedicine. In the next section, we discuss how this mechanism behind disparities (racism, ageism) can be addressed specifically for telemedicine systems.
At the community level, our findings, regarding median income being associated with decreased odds and median household size with positive odds of positive COVID tests from our cohort which accessed care through telemedicine, echo findings from other COVID studies that aren’t limited to patients who access care through telemedicine.19 Further, we found that mean income and median household size of the home zip code had decreased odds for use of telemedicine versus seeking care in-person; evidence from patient surveys and other research should be used to investigate reasons for these associations.
How this study informs design of telemedicine systems
Identifying where in the healthcare process disparities manifest is essential in order to inform effective programs, empower patients, and improve health outcomes. While systematic racism and ageism are well-documented in healthcare and healthcare access, this study gives evidence that such processes may also occur in telemedicine use. Here we describe how the design of telemedicine systems can be improved to decrease barriers to diverse populations.29
Findings from this and other digital disparities work can inform the design of telemedicine systems through the development of culturally and structurally appropriate tools and technology, representative provider presence and capacity, positive targeted outreach, and research. In developing tools and technology, efforts should be made to incorporate knowledge of the myriad factors affecting healthcare access and utilization at patient- and community-level, including knowledge, attitudes, cultural beliefs, health behaviors, adherence, language, health literacy, social support, religious beliefs, self-efficacy, preferences, and psychosocial factors. This can be achieved by drawing on methods that leverage participatory design; for example, it is known that information technology interfaces that include cultural and linguistic adaptations can aid in helping patients manage online systems, and prior studies have included patient and community participants to culturally tailor online systems.9,30–33 Building provider representativeness and capacity in telemedicine can draw from abundant existing data showing that Black, Latinx, and Native American physicians are more likely than white physicians to practice in underserved communities and to treat larger numbers of minority patients irrespective of income,34 and that Black and Latinx physicians, as well as women, are more likely to provide care to the poor and under- and uninsured.35,36 It is reasonable to suggest that ensuring similar representativeness among telemedicine providers would improve the telemedicine experience for diverse patients, reduce disparities, and improve health outcomes. Positive targeted outreach should ensure that communities identified as experiencing barriers to care via telemedicine are actively contacted, connected, empowered, and protected. For example, it has been shown that the intentional dissemination of health information to older Black adults can increase their utilization of preventive health services.37 Accordingly, communication of information on the use and availability of telemedicine could be studied in terms of how it may appeal to diverse populations in trustworthy ways. Another possible solution includes identifying which specific subgroups have the most difficulty accessing care through telemedicine and using this information to prioritize in-person care in situations (such as pandemics) when in-person interactions should otherwise be limited. Other systematic approaches to lowering barriers for diverse populations include: the continuing collection of data on disparities and publication of results; the systematic identification of biases and the development of educational and training programs to address them; and removing as much individual discretion of providers as possible (eg, specifically during this period, standardized and ready testing availability would help).38
Limitations
This study has several limitations. First, the ethnicity category in our electronic medical record is not a required field. Thus, it is likely that we are not capturing the Latinx community or other ethnic subpopulations accurately. Because of this limitation, we did not focus our analysis or discussion on this group. Second, the criteria for testing during the pandemic was significantly impacted by changing best-practice guidelines, operational limitations, and testing availability factors, which may result in incomplete information regarding COVID-related testing data. It’s possible, for example, that patients who accessed care at NYULH and were recommended to get tested got tested elsewhere or did not get tested for other reasons, and we do not know the characteristics of this group. If patients who accessed care at our institution subsequently did not seek testing through our institution systematically, then comparisons between likelihood of care access and testing by group would be biased. We cannot anticipate the direction of bias; data from behavioral studies during COVID-19 would be important to capture this type of information. Third, we used 2019 at the same time of year as a baseline comparison to account for already existing biases in who was using telemedicine prior to the pandemic. However, given the rapidly changing and maturing nature of telemedicine technology, platforms, and services, it is possible that the telemedicine experience between 2019 and 2020 was considerably different and therefore not easily comparable. However, to control for other effects, such as seasonal changes, this was the most relevant time period to compare to, and analysis during the COVID period represents a period when telemedicine was highly prioritized by both patients and providers, thus maximizing access and making disparities most visible. Fourth, our study is limited to our institution, which may limit the generalizability and clinical relevance of our results in other practice types or geographic areas. However, during the acute pandemic period, New York City was an epicenter of the outbreak in the United States, and our institution’s experience likely reflects similar urban academic institutions at that time. Further, the experience of our well-developed telemedicine infrastructure may be relevant to other institutions with similarly developed systems. As well, ours is a large healthcare institution well-suited to exploring disparities in telemedicine use due to its well-developed telemedicine infrastructure, minimizing the confounding of technical capacities for telemedicine during the study.15 This does not mean that the requirement of an individual to have digital access is eliminated, but rather the infrastructure reduces the possibility of technical glitches, decreases compatibility/interoperability challenges, and means that providers can easily access telemedicine for care.
Suggestions for future work
Given findings of decreased odds of seeking care via telemedicine, but increased odds of testing positive for Black patients compared to white patients at NYULH (controlling for individual-and community-level attributes), it appears that Black patients are accessing care through telemedicine when they are sicker compared to white patients. As well, patients with preferred language of Spanish had lower odds of telemedicine use. These findings reflect in-person care-seeking behavior that has been observed at other institutions during COVID-19,3 and indicate that factors related to in-person care access disparities such as trust in providers, health literacy, and language barriers could be relevant in telemedicine as well. Efforts to mitigate these challenges may be different in telemedicine versus in-person care (eg, the use of a virtual instead of in-person translator), thus research on specific factors related to decreased care-seeking through telemedicine are needed to best mitigate these challenges. Research on subgroup-specific challenges is also needed, given our observation that telemedicine access disparities are most prominent for intersectional groups (the larger increase in the proportion of patients who are Black and sought care from 2019 to 2020 through virtual urgent care compared to in-person in the ED, was driven by a younger and more female population). The finding that, controlling for patient- and community-level attributes, Black patients were more likely to be given a diagnosis of suspected COVID after a telemedicine visit compared to those who are white, while less likely when considering both telemedicine and in-person visits, should also be investigated further. For instance, the reason for this could be that the online platform normalizes interactions between the clinician and patient through the virtual medium39 and decrease healthcare diagnosis biases, offering a possible mitigating role for telemedicine with respect to healthcare disparities.40
CONCLUSION
Among our findings in this observational cohort study during COVID-19 peak time at our health institution in New York City, we found that, controlling for individual- and community-level factors, there are multiple groups that experience disparities in telemedicine access and subsequent aspects of care. For instance, those who are Black and those with home Zip code with a lower mean income and higher average household size were less likely to use telemedicine to seek care. The multilevel nature of observed disparities indicate that interventions solely aimed at tools and access to them are insufficient; we must also address barriers to care at the systemic level. At the same time, we also found that though Black patients were more likely than white patients to be given a diagnosis of suspected COVID after a telemedicine visit, they were less likely to get the same diagnosis after both telemedicine and in-person visits. This finding suggests that through the telemedicine medium there may be an opportunity to mitigate disparities. We also found a larger increase in the proportion of patients who are Black and sought care from 2019 to 2020 through virtual urgent care compared to in-person in the ED, driven by a younger and more female population. Overall, an understanding of particular subgroups for whom telemedicine uptake is limited is important for telemedicine tool design as well as larger strategies to address systemic racism and ageism which are at the root of both in-person and telemedicine care disparities.
FUNDING
We acknowledge funding from National Science Foundation awards 1928614 and 1845487. The NSF had no role in the study design; the collection, analysis, and interpretation of data; the writing of the report; or the decision to submit the article for publication.
AUTHOR CONTRIBUTIONS
RC, DM, KL, PT, and ON designed the study. JC curated the data. YZ and RC performed analyses. RC drafted the manuscript; all authors contributed critical edits and approved the final manuscript.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
CONFLICT OF INTEREST STATEMENT
None declared.
Supplementary Material
REFERENCES
- 1.Hooper MW, Nápoles AM, Pérez-Stable EJ. COVID-19 and racial/ethnic disparities. JAMA2020; 323 (24): 2466–7. [DOI] [PMC free article] [PubMed]
- 2.Yancy CW.COVID-19 and African Americans. JAMA 2020; 323 (19): 1891. [DOI] [PubMed] [Google Scholar]
- 3.Azar KM, Shen Z, Romanelli RJ, et al. Disparities in outcomes among COVID-19 patients in a large health care system in California: study examines disparities in access and outcomes for COVID-19 patients who are members of racial and ethnic minorities and socioeconomically disadvantaged groups. Health Aff 2020; 39 (7): 1253–62. [DOI] [PubMed] [Google Scholar]
- 4.Beaunoyer E, Dupéré S, Guitton MJ.. COVID-19 and digital inequalities: reciprocal impacts and mitigation strategies. Comp Hum Behav 2020; 111: 106424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pan D, Sze S, Minhas JS, et al. The impact of ethnicity on clinical outcomes in COVID-19: a systematic review. EClinicalMedicine 2020; 23: 100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Arthur M, Hedges JR, Newgard CD, Diggs BS, Mullins RJ.. Racial disparities in mortality among adults hospitalized after injury. Med Care 2008; 46: 192–9. [DOI] [PubMed] [Google Scholar]
- 7.Schrader CD, Lewis LM.. Racial disparity in emergency department triage. J Emerg Med 2013; 44 (2): 511–8. [DOI] [PubMed] [Google Scholar]
- 8.Nelson A.Unequal treatment: confronting racial and ethnic disparities in health care. J Natl Med Assoc 2002; 94 (8): 666. [PMC free article] [PubMed] [Google Scholar]
- 9.López L, Green AR, Tan-McGrory A, King RS, Betancourt JR.. Bridging the digital divide in health care: the role of health information technology in addressing racial and ethnic disparities. Jt Comm J Qual Patient Saf 2011; 37 (10): 437–45. [DOI] [PubMed] [Google Scholar]
- 10.Khairat S, Haithcoat T, Liu S, et al. Advancing health equity and access using telemedicine: a geospatial assessment. J Am Med Inform Assoc 2019; 26 (8-9): 796–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mitchell UA, Chebli PG, Ruggiero L, Muramatsu N.. The digital divide in health-related technology use: the significance of race/ethnicity. Gerontologist 2019; 59 (1): 6–14. [DOI] [PubMed] [Google Scholar]
- 12.Schwamm LH.Telehealth: seven strategies to successfully implement disruptive technology and transform health care. Health Aff 2014; 33 (2): 200–6. [DOI] [PubMed] [Google Scholar]
- 13.Ben J, Cormack D, Harris R, Paradies Y.. Racism and health service utilisation: a systematic review and meta-analysis. PLoS One 2017; 12 (12): e0189900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Crenshaw KW.On Intersectionality: Essential Writings. New York, NY: The New Press; 2017. [Google Scholar]
- 15.Mann DM, Chen J, Chunara R, Testa PA, Nov O.. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc 2020; 27 (7): 1132–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Petrilli CM, Jones SA, Yang J, et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ2020; 369: m1966. [DOI] [PMC free article] [PubMed]
- 17.Wang B, Li R, Lu Z, Huang Y.. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY) 2020; 12 (7): 6049–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA 2020; 323 (20): 2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chin T, Kahn R, Li R, et al. US county-level characteristics to inform equitable COVID-19 response. medRxiv2020. https://www.medrxiv.org/ content/10.1101/2020.04.08.20058248v1, doi: 10.1101/2020.04.08. 20058248.
- 20.Sy KTL, Martinez ME, Rader B, White LF. Socioeconomic disparities in subway use and COVID-19 outcomes in New York City. medRxiv2020. https://www.medrxiv.org/content/10.1101/2020.05.28.20115949v1.full.pdf, doi: 10.1101/2020.05.28.20115949. [DOI] [PMC free article] [PubMed]
- 21.Ompad DC, Galea S, Marshall G, et al. Sampling and recruitment in multilevel studies among marginalized urban populations: the IMPACT studies. J Urban Health 2008; 85 (2): 268–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Von Korff M, Koepsell T, Curry S, Diehr P.. Multi-level analysis in epidemiologic research on health behaviors and outcomes. Am J Epidemiol 1992; 135 (10): 1077–82. [DOI] [PubMed] [Google Scholar]
- 23.Khullar D, Chokshi DA.. Health, income, & poverty: where we are & what could help. Health Aff 2018; 10. [Google Scholar]
- 24.Stringhini S, Carmeli C, Jokela M, et al. Socioeconomic status and the 25 × 25 risk factors as determinants of premature mortality: a multicohort study and meta-analysis of 1.7 million men and women. Lancet 2017; 389 (10075): 1229–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnston R, Jones K, Manley D.. Confounding and collinearity in regression analysis: a cautionary tale and an alternative procedure, illustrated by studies of British voting behaviour. Qual Quant 2018; 52 (4): 1957–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sherwin J, Lawrence K, Gragnano V, Testa PA.. Scaling virtual health at the epicentre of coronavirus disease 2019: a case study from NYU Langone Health. J Telemed Telecare 2020. doi: 10.1177/1357633X20941395. [DOI] [PubMed] [Google Scholar]
- 27.Adhikari S, Pantaleo NP, Feldman JM, Ogedegbe O, Thorpe L, Troxel AB.. Assessment of community-level disparities in coronavirus disease 2019 (COVID-19) infections and deaths in large US metropolitan areas. JAMA Netw Open 2020; 3 (7): e2016938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kane R, Kane R.. Ageism in healthcare and long-term care. Generations 2005; 29 (3): 49–54. [Google Scholar]
- 29.Powe NR.Let’s get serious about racial and ethnic disparities. J Am Soc Nephrol 2008; 19 (7): 1271–5. [DOI] [PubMed] [Google Scholar]
- 30.Agate S.Unlocking the power of telehealth: increasing access and services in underserved, urban areas. Harv J Hisp Policy 2017; 29: 85. [Google Scholar]
- 31.Ospina-Pinillos L, Davenport T, Diaz AM, Navarro-Mancilla A, Scott EM, Hickie IB.. Using participatory design methodologies to co-design and culturally adapt the Spanish version of the mental health eClinic: qualitative study. J Med Internet Res 2019; 21 (8): e14127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chandler J, Sox L, Kellam K, Feder L, Nemeth L, Treiber F.. Impact of a culturally tailored mHealth medication regimen self-management program upon blood pressure among hypertensive Hispanic adults. Int J Environ Res Public Health 2019; 16 (7): 1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.McCall T, Bolton CI, McCall R, Khairat S.. The use of culturally-tailored telehealth interventions in managing anxiety and depression in African American adults: a systematic review. Stud Health Technol Inform 2019; 264: 1728–9. [DOI] [PubMed] [Google Scholar]
- 34.Cohen JJ, Gabriel BA, Terrell C.. The case for diversity in the health care workforce. Health Aff 2002; 21 (5): 90–102. [DOI] [PubMed] [Google Scholar]
- 35.Alsan M, Garrick O, Graziani GC.. Does diversity matter for health? Experimental evidence from Oakland. National Bureau of Economic Research; 2018. Working Paper 24787. http://www.nber.org/papers/w24787 Accessed September 15, 2020. [Google Scholar]
- 36.Kington R, Tisnado D, Carlisle DM.. Increasing racial and ethnic diversity among physicians: an intervention to address health disparities. In: Smedley BDStith AYColburn LEvans CH, Institute of Medicine (US), eds. The Right Thing to Do, the Smart Thing to Do: Enhancing Diversity in the Health Professions Washington, DC: National Academies Press; 2001: 57–75. [Google Scholar]
- 37.Musa D, Schulz R, Harris R, Silverman M, Thomas SB.. Trust in the health care system and the use of preventive health services by older black and white adults. Am J Public Health 2009; 99 (7): 1293–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sabin JA.How We Fail Black Patients in Pain. Association of American Medical Colleges ; 2020. https://www.aamc.org/news-insights/how-we-fail-black-patients-pain Accessed September 12, 2020.
- 39.Matusitz J, Breen G-M.. Telemedicine: its effects on health communication. Health Commun 2007; 21 (1): 73–83. [DOI] [PubMed] [Google Scholar]
- 40.Snowden LR.Bias in mental health assessment and intervention: theory and evidence. Am J Public Health 2003; 93 (2): 239–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.