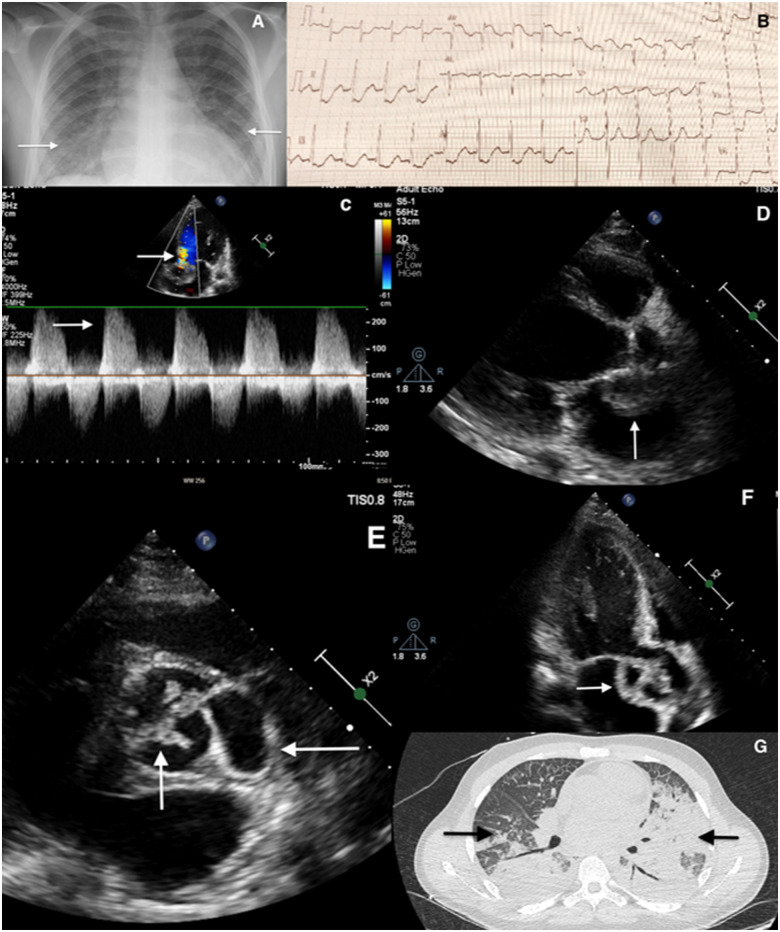
A 20-year-old man with known bicuspid aortic valve, and aortic coarctation repair in childhood presented with 4 weeks of vomiting, diarrhoea, low grade fever, productive cough, and progressive breathlessness. Auscultation revealed fine crackles bilaterally and a loud systolic murmur at the base of the heart. Inflammatory markers and troponin were elevated (troponin T 388 ng/L; cut-off for normal <14 ng/L). Initial ECG showed only sinus tachycardia. Chest X-ray (Panel A) showed bilateral airspace infiltrates suspicious of COVID pneumonitis. Shortly after admission, he deteriorated, with rising oxygen requirements and haemoptysis. A repeat ECG showed first-degree atrioventricular (AV) block with widespread ischaemia (Panel B).
Bedside echocardiogram revealed severe aortic regurgitation (Panel C), a large aortic valve vegetation, and aortic root abscess (Panels D–F). The left ventricle was dilated with severe systolic dysfunction, and the right ventricle was normal. Incomplete CT chest (Panel G) showed bilateral multilobular consolidation, not typical for COVID-19 pneumonitis. While in the CT scanner, the patient developed complete heart block deteriorating into pulseless electrical activity (PEA) followed by asystole refractory to adrenaline and both transcutaneous and transvenous pacing attempts.
With this case we aim to emphasize that even in a pandemic period like COVID-19, it is prudent to seek medical help especially for those at high risk of developing infective endocarditis and who have symptoms of infection. Timely presentation is essential as any delay can lead to fatal consequences.
Conflict of interest: The authors have submitted their declaration which can be found in the article Supplementary Material online.
Supplementary Material
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.