Abstract
Background and Objectives
The novel coronavirus outbreak (SARS-CoV-2) began in late 2019 and dramatically impacted health care systems. This study aimed to describe the impact of the early phase of the pandemic on physician decision-making, practice patterns, and mental health.
Methods
An anonymous survey was distributed to physician members of the Spine Intervention Society (SIS) on March 24 and April 7, 2020. Respondents provided information regarding changes in clinical volume, treatment, and mental health (Patient Health Questionnaire [PHQ-4]) before April 10, 2020.
Results
Of the 1,430 individuals who opened the survey, 260 completed it (18.2%). Overall clinical and procedural volume decreased to 69.6% and 13.0% of prepandemic volume, respectively. Mean in-person clinic visits were reduced to 17.7% of total prepandemic clinic volume. Ongoing clinical visits were predominantly completed via telemedicine (video) or telephone (74.5%), rather than in-person (25.5%). Telemedicine and telephone visits represented 24.6% and 27.3% of prepandemic clinical volume, respectively. Respondents decreased in-person visits of select groups of high-risk patients by 85.8–94.6%. Significantly more providers reported increasing rather than decreasing prescriptions of the following medications: opioids (28.8% vs 6.2% of providers, P < 0.001), muscle relaxants (22.3% vs 5.4%, P < 0.001), neuropathic pain medications (29.6% vs 3.8%, P < 0.001), and acetaminophen (26.2% vs 4.2%, P < 0.001). Respondents’ mean PHQ-4 score was 3.1, with 19% reporting moderate or severe psychological distress. Several demographic factors were significantly associated with practice changes.
Conclusions
The novel coronavirus pandemic dramatically altered the practice and prescribing patterns of interventional pain physicians.
Keywords: Coronavirus, COVID, Pandemic, Opioids, Telemedicine, Pain
Introduction
The novel coronavirus outbreak (SARS-CoV-2) began in late 2019 in Wuhan, China, but has since become a global pandemic, significantly impacting health care systems worldwide. Recent investigation into health care systems has focused on the effect of the virus on emergency room, hospital, and intensive care unit operations [1–3]. However, outpatient care has also profoundly changed since the pandemic. In March of 2020, the US Centers for Disease Control and Prevention (CDC), as well as a variety of state and local governments, recommended that all nonurgent evaluation and treatment be postponed or canceled. More recently, multisociety guidelines have been published that discuss risk mitigation, staffing contingencies, and use of telemedicine, opioids, nonsteroidal anti-inflammatory drugs (NSAIDs), and corticosteroids in context of the pandemic [4, 5]. To date, the impact of the pandemic on outpatient interventional pain practice has not been studied. Yet, it is likely that the sudden decrease in in-person visits has impacted multiple aspects of patient care.
The present study aimed to describe the impact of the global pandemic on certain aspects of outpatient interventional pain practices. Specifically, we investigated physician beliefs and actions regarding risk mitigation, use of telemedicine, physician well-being, and alterations in practice patterns that affect patients. Ideally, this report will provide knowledge about the effects of the pandemic on patients with chronic pain, so as to better prepare practices for upcoming changes should the pandemic recur or should new large-scale emergencies arise [6].
Methods
An anonymous survey, deemed exempt by the University of Utah Institutional Review Board, was sent to physician members of the Spine Intervention Society (SIS) on March 24 and on April 7, 2020, via e-mail. Survey responses were recorded from March 24 until April 21, 2020, with responses collected over a total of 28 days. For reference, the average United States state-wide school closure occurred on March 15, 2020, and the first state-wide stay-at-home measure (California) was enacted on March 18, 2020. To preserve anonymity, respondents were technically able to complete the survey more than once. However, the survey could only be completed once if the survey link was accessed on the same computer and IP address. The survey consisted of a series of questions assessing prepandemic physician demographics and practice patterns, as well as new beliefs and behaviors following government-based medical policy changes resulting from the SARS-CoV-2 global pandemic (Supplementary Data). To assess changes in practice volume, respondents were asked how their current practice on the date of the survey compared with their prepandemic volume. As an example, to determine changes in in-person clinical volume, respondents were asked the following question: “Since the pandemic has begun, what percentage of patients are you now seeing IN PERSON compared to your typical practice? (Do not include procedures.) For example, if you had to cut down your practice by half, and seeing only half of the remaining patients in person, please choose 25%.” To assess changes in prescribing patterns, respondents were asked to rate changes in their medication prescriptions or suggestions on a five-point Likert scale with the following options: much less, slightly less, unchanged, slightly more, and much more. Significant differences were evaluated by comparing the proportions of subjects prescribing slightly more or much more with those who were prescribing slightly less or much less. The Patient Health Questionnaire–4 (PHQ-4) [7] was used to screen for symptoms of anxiety and depression of the physician respondents, though all respondents were allowed to opt out of completing this portion of the survey, as it contained sensitive information that they may have otherwise not wanted to disclose.
Statistical analysis for this cross-sectional study was performed with Stata/MP 16.1 for Windows (StataCorp LLC, College Station, TX, USA), with an α level of 0.05. Descriptive statistics were calculated. For differences in proportions of prescriptions, a chi-square (χ2) test with the calculations of a Monte Carlo exact P value (10,000 replications) was performed. Multiple linear and logistic regression models were fit to continuous and dichotomous dependent variables, respectively, with independent variables consisting of the following: age, sex, training background (primary residency), number of years since completion of training, geographic region (Northeast, Midwest, South, Northwest, and international), regional density (rural, suburban, or urban) of practice location, practice setting (private practice, academic/university, hospital system employee, or other), prepandemic clinic/procedure volumes, and personal relationship with someone who had tested positive for SARS-CoV-2 infection (defined as a positive test for the respondent, someone they live with, a personal patient, staff member they work with, or colleague in the group). For dichotomous variables, odds ratios were calculated, with numbers >1.00 representing higher odds and numbers <1.00 representing lower odds. For continuous variables, positive beta coefficients indicate positive associations, while negative beta coefficients indicate negative associations. For categorical predictors, P value adjustments, such as a Bonferroni test, were not performed, as our reference category for each categorical predictor was identified before performing the regression analysis. Preliminary examinations indicated heteroscedasticity for some of the continuous dependent variables; hence the Huber-White sandwich estimator of variance was used in such cases [8–10].
Results
The e-mail containing the link to the study survey was viewed by 1,430 individuals and completed by 260 individuals, representing an 18.2% response rate. The demographic information of survey participants is listed in Table 1. Demographic data for respondents were unable to be compared with SIS membership as a whole, as general membership data were not available. Survey respondents were most commonly male, trained in physical medicine & rehabilitation (PM&R) or anesthesiology, and were practicing in an urban or suburban environment.
Table 1.
Demographic and early-phase pandemic survey response information for study participants
| No. | % | Mean | SD | |||
|---|---|---|---|---|---|---|
| Baseline demographics | Age, y | 48.6 | 10.0 | |||
| Years post-training | 15.0 | 10.2 | ||||
| Weekly clinic volume (before pandemic) | Number of patients | 73.2 | 44.2 | |||
| Number of procedures | 34.9 | 22.5 | ||||
| Gender | Male | 222 | 86.0 | |||
| Female | 36 | 14.0 | ||||
| Practice population density | Urban | 120 | 46.2 | |||
| Suburban | 114 | 43.8 | ||||
| Rural | 26 | 10.0 | ||||
| Training background | PM&R | 139 | 53.5 | |||
| Anesthesiology | 96 | 36.9 | ||||
| Other | 25 | 9.6 | ||||
| Region of the United States | South | 69 | 26.5 | |||
| West | 67 | 25.8 | ||||
| Midwest | 42 | 16.2 | ||||
| Northeast | 39 | 15.0 | ||||
| International | 43 | 16.5 | ||||
| Practice type | Private practice | 163 | 62.7 | |||
| Academic/university | 45 | 17.3 | ||||
| Hospital system | 39 | 15.0 | ||||
| Other | 13 | 5.0 | ||||
| Postpandemic | In-person clinic visit volume, % of normal | 17.7 | 22.9 | |||
| Telephone visit volume, % of normal | 27.3 | 29.6 | ||||
| Telemedicine (video) visit volume, % of normal | 24.6 | 30.3 | ||||
| In-person procedural visit volume, % of normal | 13.0 | 20.4 | ||||
| Rationale for decreasing in-person visits | Public safety | 179 | 68.8 | |||
| Concern for patients | 161 | 61.9 | ||||
| Staff safety | 155 | 59.6 | ||||
| Patients are not coming in | 137 | 52.7 | ||||
| Personal/family safety | 128 | 49.2 | ||||
| Administration requirement | 121 | 46.5 | ||||
| Corticosteroid concerns | 111 | 42.7 | ||||
| Overwhelming health care system | 110 | 42.3 | ||||
| Limited PPE | 84 | 32.3 | ||||
| Other | 18 | 6.9 | ||||
| Knowledge of person testing positive for SARS-CoV-2 | Someone in the hospital system | 98 | 37.7 | |||
| Someone in the building | 28 | 10.8 | ||||
| One of your patients | 22 | 8.5 | ||||
| Staff you work with | 22 | 8.5 | ||||
| Colleagues in department/group | 22 | 8.5 | ||||
| Self | 4 | 1.5 | ||||
| Someone you’re living with | 3 | 1.2 | ||||
| PHQ-4 | Anxiety subscale (0–6) | 2.09 | 1.74 | |||
| Depression subscale (0–6) | 1.02 | 1.31 | ||||
| Total (0–12) | 3.13 | 2.82 | ||||
PHQ-4 = Patient Health Questionnaire (four questions); PM&R = physical medicine & rehabilitation; PPE = personal protective equipment.
Also as detailed in Table 1, at the time of survey response, respondents reported that their in-person clinical volume (SD) was reduced to 17.7% (22.9%) of normal, and their procedural volume (SD) was reduced to 13.0% (20.4%) of normal. Telephone and video telemedicine visits represented a mean (SD) of 27.3% (29.6%) and 24.6% (30.3%) of respondents’ typical clinical volume, respectively. This suggests that ∼74.5% of all ongoing clinic visits were virtual (telephone or video telemedicine, as opposed to in-person).
The most common rationale for limiting patient interaction in clinic and procedural settings was public safety (68.8% of respondents). Concerns regarding patient safety (61.9%), staff safety (59.6%), personal/family safety (49.2%), corticosteroid concerns (42.7%), overwhelming the health care system (42.3%), and limited personal protective equipment (32.3%) were also reported. Extrinsic factors also appeared to influence the number of in-person clinic visits; 46.5% of respondents noted that they limited in-person visits due to an administrative requirement, and 52.7% of respondents noted that patients opted to avoid in-person visits.
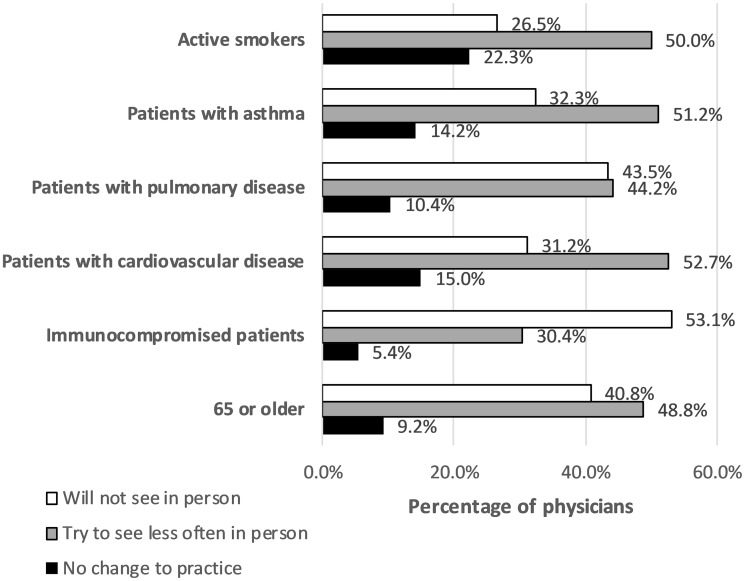
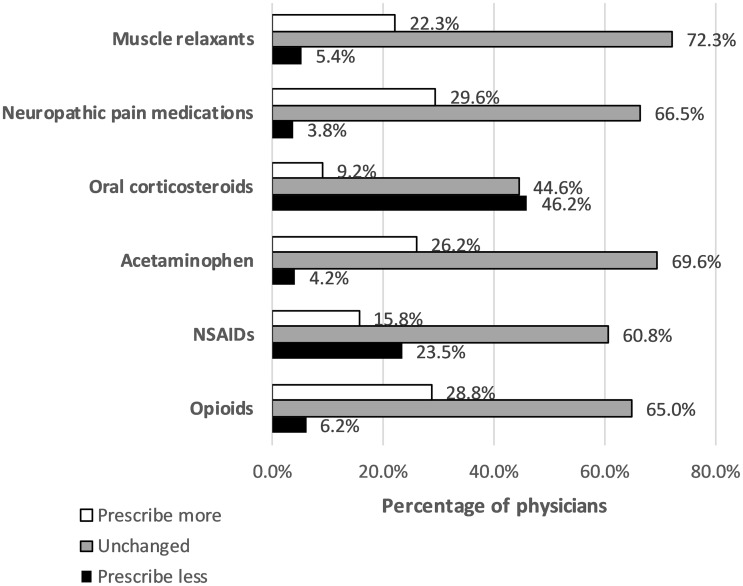
Responses to questions regarding how physicians addressed patient populations deemed by the CDC to be at high risk for severe illness at the time of survey creation are reported in Figure 1 [11]. Most survey respondents reported that they had reduced or completely eliminated in-office visits for patients who were over the age of 65 (89.6%), were immunocompromised (83.5%), had cardiovascular disease (83.9%), had pulmonary diseases other than asthma (87.7%), had asthma (83.5%), and were active smokers (76.5%). Changes in prescription patterns are reported in Figure 2. As some survey respondents may serve as consultants and not actively prescribe medications, responses represent both changes in respondents’ personal prescriptions and changes in suggestions or recommendations for various medications. Most respondents reported no changes in their prescriptions or suggested medications for all medications surveyed other than oral corticosteroids. Among those who did change their prescribing patterns, significantly more physicians reported increases in prescriptions of opioids (P < 0.001), acetaminophen (P < 0.001), neuropathic pain medications (P < 0.001), and muscle relaxants (P < 0.001), compared with those who reported decreases in prescriptions of these medications. Significantly more physicians also reported decreases in their prescriptions of oral corticosteroids (P < 0.001) compared with their prepandemic practice. The number of respondents prescribing more NSAIDs was not significantly different than the number of respondents prescribing less (P = 0.061).
Figure 1.
How physicians addressed high-risk patients during the early phase of the pandemic, N = 260 respondents.
Figure 2.
Changes in frequency of prescriptions since the onset of practice changes due to the pandemic, N = 260 respondents.
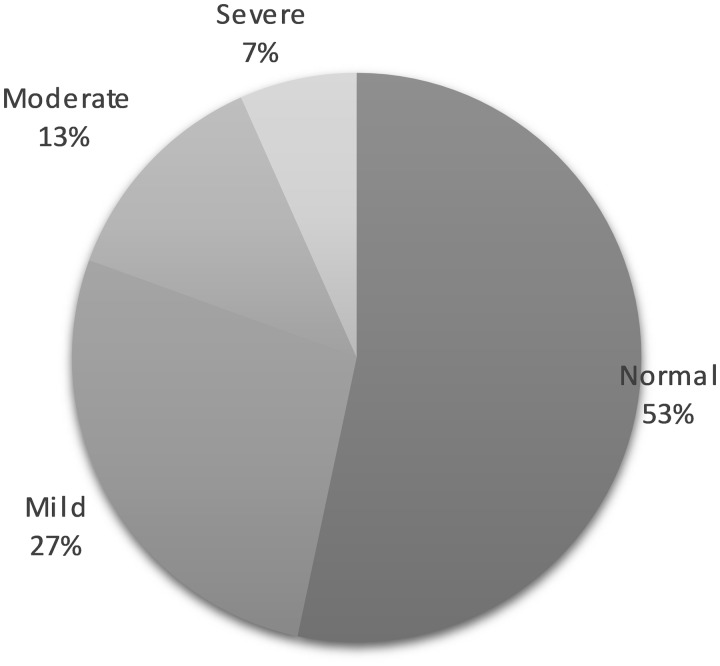
Of the 260 respondents, 183 (70.4%) opted to complete the PHQ-4. Results are reported in Figure 3. Respondents had an average total PHQ-4 score (SD, range) of 3.1 (2.8, 0–12), with an anxiety subscale score of 2.1 (1.7, 0–6) and a depression subscale score of 1.02 (1.3, 0–6). For reference, PHQ-4 scores are graded on a scale from 0–12, with scores 0–2 representing normal, 3–5 representing mild, 6–8 representing moderate, and 9–12 representing severe psychological distress. On the anxiety and depression subscales, scores ≥3 suggest concern for anxiety or depression, respectively [12].
Figure 3.
Patient Health Questionnaire (PHQ-4) scores of respondents, N = 183 respondents. “Normal” refers to a PHQ-4 total score of 0–2, “mild” to psychological stress 3–5, “moderate” to psychological stress 6–8, and “severe” to psychological stress 9–12.
Of the 260 completed surveys, the following respondents were excluded from the regression analysis because of relatively low frequencies: undefined gender (2), community clinic practice (6), and Department of Veterans Affairs/government practice location (7); a total of 245 participants were therefore included in the model. Regression modeling revealed several significant demographic and prepandemic practice factors associated with new behaviors following medical policy changes resulting from the SARS-COV-2 global pandemic; these are shown in Table 2. For clarity, the larger in magnitude the beta coefficient is, the greater the effect. An example interpretation from Table 2, volume of procedures (the second dependent variable), is as follows: Physicians practicing in the Midwest and the Northeast both reported significantly smaller procedural volumes, compared with the reference group (international physicians), during the early phase of the pandemic. When adjusted for covariates, these groups of physicians performed an average of 12% (P = 0.032) and 14% (P = 0.010) fewer procedures compared with international physicians, respectively. In other words, if international physicians performed 19% of their typical procedural volume during the early phase of the pandemic, Midwest and Northeast physicians would perform ∼7% and ∼5% of their typical procedure volume, respectively, after adjustment for other variables in the model.
Table 2.
Significant results of regression modeling
| Dependent Variable | Significant Independent Variable(s) | Effect | B Coeff/OR (95% CI) | P Value |
|---|---|---|---|---|
| Volume of clinic patients | Age | Fewer | –0.64 (–1.11 to –0.17) | 0.008 |
| (mean = 17.7 % of usual total volume) | Years since training | Greater | 0.57 (0.07 to 1.07) | 0.026 |
| Volume of procedures | Region* – Midwest | Fewer | –12.06 (–23.05 to –1.07) | 0.032 |
| (mean = 13% of usual total volume) | Region* – Northeast | Fewer | –14.16 (–24.89 to –3.43) | 0.010 |
| Density† – suburban | Greater | 7.65 (1.05 to 14.25) | 0.023 | |
| Practice type‡ – private practice | Greater | 8.74 (2.77 to 14.71) | 0.004 | |
| Personal relationship with COVID | Fewer | –6.57 (–11.79 to –1.35) | 0.014 | |
| Volume of patients by telephone | Density† – rural | Fewer | –17.85 (–30.92 to –4.78) | 0.008 |
| (mean = 27.3% of usual total volume) | Density† – suburban | Fewer | –10.44 (–19.6 to –1.29) | 0.026 |
| Practice type‡ – private practice | Fewer | –12.02 (–23.26 to –0.78) | 0.036 | |
| Volume of patients by telemedicine | Training§ – anesthesiology | Greater | 9.08 (0.37 to 17.79) | 0.041 |
| (mean = 24.6% of usual total volume) | Region* – South | Greater | 14.96 (3.56 to 26.35) | 0.010 |
| Region* – West | Greater | 15.09 (3.57 to 26.62) | 0.010 | |
| Amount of time elapsed until patient contact was reduced (larger values are later) | Region* – South | Later | 2.67 (0.06 to 5.28) | 0.045 |
| Amount of time elapsed until procedures were reduced (larger values are later) | Region* – South | Later | 3.33 (0.60 to 6.06) | 0.017 |
| Personal relationship with COVID | Earlier | –1.72 (–3.24 to –0.19) | 0.027 | |
| Higher PHQ-4 anxiety scores | Greater baseline procedure volume | More | 0.96 (0.21 to 1.72) | 0.013 |
| Higher PHQ-4 depressive scores | No associations | |||
| Higher PHQ-4 total scores | Training§ – anesthesiology | Greater | 1.13 (0.16 to 2.1) | 0.023 |
| Training§ – other | Greater | 1.8 (0.03 to 3.57) | 0.046 | |
| Personal relationship with COVID | Greater | 1.8 (0.48 to 3.12) | 0.008 | |
| Prescribing more opioids | Greater baseline procedure volume | More | OR = 0.93 (0.89 to 0.98) | 0.007 |
| Greater baseline clinic volume | More | OR = 1.27 (1.07 to 1.51) | 0.006 | |
| Personal relationship with COVID | More | OR = 0.05 (0 to 0.86) | 0.04 | |
| Prescribing more NSAIDs | No associations | |||
Dependent variables refer to those captured during the early phase of the pandemic (N = 245).
OR = odds ratio; NSAIDs = nonsteroidal anti-inflammatory drugs; PHQ-4 = Patient Health Questionnaire (four questions); PM&R = physical medicine & rehabilitation.
Region reference: international.
Density reference: urban setting.
Practice type reference: academic/university.
Training background reference: PM&R.
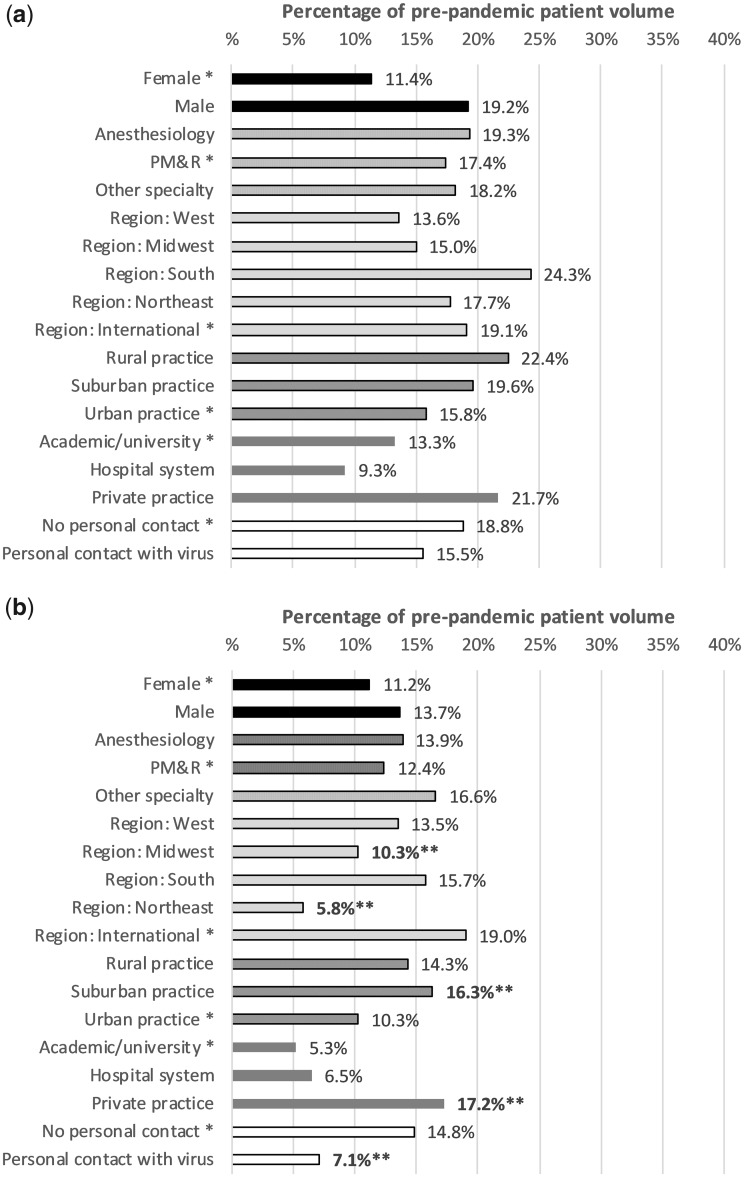
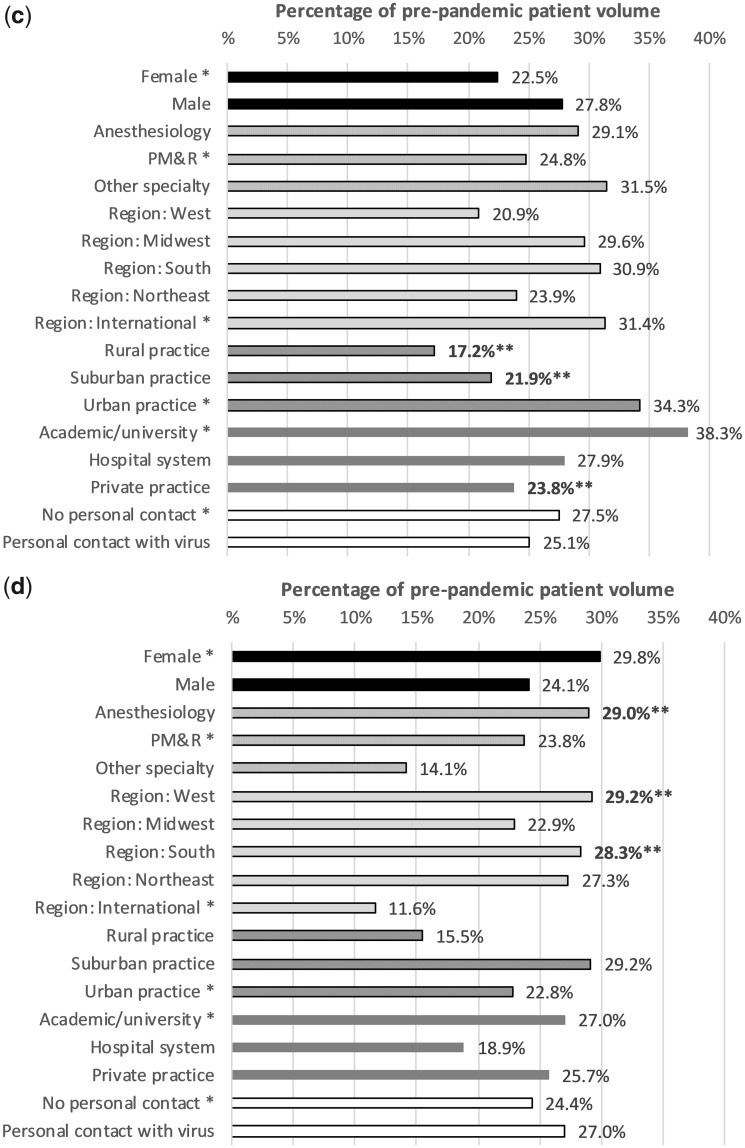
Changes in practice patterns are described in Figure 4. The significant associations (**) match the associations seen in Table 2. The Midwest and the Northeast both reported significantly reduced procedural volumes compared with other areas during the early phase of the pandemic. While physicians in the Northeast and Midwest performed only 5.8% and 10.3% of their typical procedural volume, respectively, physicians in the West and South performed 13.5% and 15.7% of their typical procedural volume. Similarly, respondents with a personal relationship to someone who has contracted SARS-COV-2 performed approximately half the number of procedures of those who did not have such a relationship (7.1% vs 14.8%). Alternatively, physicians practicing in suburban locations reported completing 16.3% of their typical procedural volume, which was significantly more than those in urban settings (10.3%, P = 0.023). Respondents in private practice performed 17.2% of their typical procedural volume, which was substantially more than those in hospital-based practices (6.5%) or academic practices (5.3%).
Figure 4.
Clinical volumes, compared with prepandemic patient volume. For example, 20% would mean that the subgroup is seeing 20% of their typical total patient volume compared with their prepandemic baseline. If a practitioner was seeing 100 patients in clinic before the pandemic, then 20% would refer to 20 weekly patients in the clinic after the pandemic practice changes. If a practitioner was performing 100 procedures weekly, 20% would refer to 20 weekly procedures after the pandemic practice changes. a) In-person clinic visits. b) Procedural volume. c) Telephone visits. d) Telemedicine (video) visits. *Reference group for statistical comparisons. **Statistically significant difference compared with the reference group.
Telephone and video telemedicine use were also significantly different among groups. Telephone visits in rural and suburban areas were performed less often, 17.2% (P = 0.008) and 21.9% (P = 0.026), respectively, compared with urban respondents (34.3%). Although private practice physicians completed 23.8% of their typical volume via telephone visits, this was substantially lower than academic physicians, who used telephone visits for 38.3% (P = 0.036) of their typical clinic volume. Respondents in hospital systems reported using telephone visits for 27.9% of their typical volume. Interestingly, similar findings were not observed in groups utilizing video telemedicine. Rather, anesthesiologists (P = 0.041) and physicians practicing in the South (P = 0.010) or the West (P = 0.010) reported significantly higher rates of video telemedicine use.
Discussion
This survey study demonstrates multiple changes in interventional pain physician practices in the early stages of the SARS-CoV-2 global pandemic. Perhaps the most notable finding in this study is the significant decrease in clinical and procedural volume. Respondents reported that they were seeing <20% of their usual patients in-person and performing <15% of their typical interventional procedure volume. Overall clinic volume between late March and early April of 2020 was ∼30% lower than it was before the pandemic, not including the dramatic corresponding drop in interventional procedures. As interventional procedures frequently account for a significant proportion of revenue for interventional pain physicians, the economic impact of a >85% reduction in procedural volume cannot be overstated.
Several factors appear to relate to alterations in patient volumes, as seen in the regression analyses. First, older respondents reported a lower percentage of their typical clinical volume when adjusted for covariates. As the SARS-CoV-2 virus appears to have higher mortality rates among older patients [6], physicians with more advanced age may have a personal stake in avoiding patient contact. An alternative explanation may be less familiarity with adoption of telehealth platforms to evaluate patients. Additionally, younger physicians may also have greater financial obligations, such as student loan debt, practice ownership loans, or financial targets to make partner, which may influence their willingness to decrease clinical volume.
Despite most physicians reporting a dramatic decrease in their volume of procedures, physicians in private practice and those working in suburban environments reduced their procedure volume by a smaller magnitude. Although not clearly demonstrated in this study, a number of reasons may have influenced the amount private practices reduced their procedural volume, including financial implications, fewer administrative support staff, and greater reliance on consensus guidelines. Respondents in the Northeast and Midwest decreased their procedural volume more than physicians in other regions, while respondents in the South were slower to reduce their clinic or procedural volume. This may be due to a variety of factors, including differences in the relative frequency of SARS-CoV-2 infection, cultural differences, political differences, and differences in local government policy. We controlled for a handful of potentially related factors in our regression models, such as population density; thus it is unlikely that this is purely related to urban practice settings in the Northeast or Midwest.
Changes in prescribing patterns of physicians were particularly notable. For all medications surveyed other than corticosteroids, the majority of providers reported no changes in their prescribing patterns. Of the respondents who did change their prescribing patterns, significantly more providers reported increasing their use of opioids, neuropathic pain medications, and muscle relaxants. Although the survey results do not explain the rationale for these changes in prescribing patterns, possible causes include prevention of emergency visits, restrictions of interventional options, or inability to use certain in-person therapeutic treatments such as physical therapy or chiropractic care. These medication increases are notable and concerning in the setting of the ongoing opioid crisis, particularly as many of these medications impact respiratory drive when used concomitantly [13]. Opioid prescriptions have declined significantly over the past decade, likely due to increased awareness of their risks with the opioid crisis [14]. The results from the survey suggest that providers may be more likely to prescribe opioids due to the pandemic. However, it is unclear that this increased propensity to prescribe opioids, coupled with a significant decrease in clinical volume, has actually led to an increase in the overall number of opioid prescriptions. Given the current findings from this study, further evaluation of the total number of opioid prescriptions and opioid deaths during the pandemic will be useful to better understand the pandemic’s true impact on the opioid crisis. As this survey only examined a subset of physicians, it is imperative to also examine the prescribing patterns of other physicians.
Disagreement still exists regarding the best ways to manage patients with severe pain during the SARS-CoV-2 pandemic. As pain itself may suppress the immune system, there is concern that untreated pain may increase the risk for either developing an infection or having more severe symptoms [15]. Furthermore, treating pain may help improve mobility and improve one’s overall health. Although opioids and steroid injections are frequently used to manage pain, both likely have some level of intrinsic immunosuppression [16–19]. Further studies on the impact of these treatments on the immune response and risk of acquiring viral infection may be helpful to guide decisions during future pandemics. Ultimately, there will likely need to be a balance between restricting in-person visits (that could contribute to community viral spread) and providing appropriate care.
The implementation of video telemedicine and telephone visits to assess patients during the pandemic is remarkable. Before the pandemic, some evidence suggested that video telemedicine could be effectively used to assess patients with musculoskeletal or chronic pain [20–22]. However, significant barriers were acknowledged, including technological issues, inability to perform a complete physical examination, concerns about liability, regulatory and licensing issues, and differences in reimbursement impacting viability. While we do not have baseline data for the frequency with which respondents used these platforms before the pandemic, it is likely that their use was substantially lower previously due to the aforementioned issues. As of survey completion, roughly 75% of respondents’ ongoing clinical visits were conducted via telephone or telemedicine, whereas only 25% of visits were completed in-person. As physicians, patients, and insurers gain more familiarity with telemedicine, practices may choose to continue offering these visit formats, provided that regulatory measures and reimbursement remain favorable. Further research into this area is currently ongoing and may be helpful to determine the long-term effect of the pandemic on the implementation of telemedicine.
As part of our study, we evaluated how interventional pain physician practices changed with regard to patients who are at high risk for severe illness from SARS-COV-2. Although most respondents noted significant practice changes to reduce the number of in-person visits for high-risk patients, between 5% and 15% of respondents reported no change to practice patterns when treating individuals in any given high-risk category. Of note, two pain medicine consensus guidelines with regard to the pandemic were published on April 7, 2020, nearing the end of our study recruitment [4, 5]. Seventy three percent of respondents had completed our survey before this date, and another 24% responded the day these guidelines were published. With only eight participants (3%) responding after April 7, 2020, the results from this study represent the data of physician practices before the widespread distribution or adoption of these consensus guidelines. The guidelines published toward the end of survey enrollment provided new recommendations that in-person visits and procedures should be limited to urgent or emergent cases in high-risk populations [4, 5]. It remains to be seen whether these recommendations will change practices in the coming weeks and months.
With regards to physician well-being, the average PHQ-4 was 3.1, which represents mild psychological distress. Approximately 19% of respondents were noted to have moderate or severe psychological distress. The regression analysis demonstrated that those with a personal relationship to someone who has contracted SARS-COV-2 had higher PHQ-4 scores than those who did not. This indicates that these respondents were more likely to be experiencing psychological distress. Despite the significant differences in virus prevalence in different regions of the country, or among different population densities, no significant differences were found between PHQ-4 scores among different regions of the United States when controlling for other covariates. However, anesthesiologists were more likely to have higher PHQ-4 scores than physiatrists. Those with an anesthesiology background may be taking part in more front-line activities compared with physiatrists or have more friends/family working in higher-risk settings, which could increase anxiety. Additional research will be helpful to determine how physician well-being changes as the pandemic progresses and how it affects different providers across different settings and geographic regions. For comparison, a recent study evaluated health care workers from Wuhan, China, between January 29, 2020, and February 4, 2020. The investigators found that 28.6% of Chinese health care workers reported moderate or severe psychological distress [23]. A variety of findings may account for the difference between groups, including differences in SARS-CoV-2 prevalence, socioeconomic differences, cultural differences, and differences between types of health care workers surveyed.
There are several limitations to this study. As this survey was only available to members of the SIS and only completed by 18.2% of those who received the study, there may be concerns as to the generalizability of the findings to the entire interventional pain medicine community. One might postulate that members of the SIS who chose to complete the study may have a particular interest in this disease and thus might have responded to the pandemic differently than others. Another possibility could be that those with more free time (from reduced clinical volume) were more likely to respond, thus artificially lowering the clinical volume amounts. Although the majority of responses were obtained in just over two weeks, the medical system was in a period of rapid evolution during that time and answers from respondents on March 24 might have been substantially different than answers on April 7 from those same individuals. In order to accommodate participants so that they may have enough time to reasonably complete the study, we felt that this duration was necessary.
Another limitation of this study is that answers to questions are self-reported. For example, when examining questions regarding current clinical and procedural volume, one’s impression of the changes in their practice volume might be substantially different than what the actual changes in volume are when a respondent reviews billing data from their practice. As the pandemic is rapidly evolving, we felt that there was value in obtaining data quickly from survey responses despite the inherent limitations of this model. Future review of changes in billing with large databases may better quantify the economic impact the coronavirus had on clinical and procedure volume.
Conclusions
The emergence of the SARS-CoV-2 virus and the subsequent global pandemic have dramatically altered practice patterns of interventional pain physicians in the United States. Emerging trends include marked reductions in clinical and interventional procedural volume, increased utilization of telemedicine, and increased opioid prescribing. Geography within the United States and practice setting appear to play a role in some of these changes. The decrease of in-person visits has caused secondary effects; it is particularly concerning that more than a quarter of physicians are recommending or prescribing more opioids than before. As the pandemic continues, ongoing research should continue to evaluate the effect of the pandemic on practice patterns, prescribing patterns, and physician well-being.
Supplementary Material
Acknowledgments
The authors would like to thank the Spine Intervention Society for their support and rapid approval of this time-sensitive project. Additionally, we would like to extend our gratitude to the institutional review board at the University of Utah, which rapidly evaluated and approved this study.
Funding sources: No funding sources were used for this project.
Conflicts of interest: AAJ, AC, RWK, GW, MT, and DMC report no potential conflicts of interest. ZLM has served on the board of directors for the Spine Intervention Society.
References
- 1. Cao Y, Li Q, Chen J, et al. Hospital emergency management plan during the COVID‐19 Epidemic. Acad Emerg Med 2020;27(4):309–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Grasselli G, Pesenti A, Cecconi M.. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: Early experience and forecast during an emergency response. JAMA 2020;323(16):1545–6. [DOI] [PubMed] [Google Scholar]
- 3. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med 2020;382(21):2049–55. [DOI] [PubMed] [Google Scholar]
- 4. Shanthanna H, Strand NH, Provenzano DA, et al. Caring for patients with pain during the COVID‐19 pandemic: Consensus recommendations from an international expert panel. Anaesthesia 2020;75(7):935–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cohen SP, Baber ZB, Buvanendran A, et al. Pain management best practices from multispecialty organizations during the COVID-19 pandemic and public health crises. Pain Med 2020;XXX(X):XXX–XX. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yan Y, Shin WI, Pang YX, et al. The first 75 days of novel coronavirus (SARS-CoV-2) outbreak: Recent advances, prevention, and treatment. Int J Environ Res Public Health 2020;17(7):2323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Löwe B, Wahl I, Rose M, et al. A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord 2010;122(1–2):86–95. [DOI] [PubMed] [Google Scholar]
- 8. White HLJ. A heteroskedasticity-consistent covariance matrix estimator and a direct test for heteroskedasticity. Econometrica 1980;48(4):817–38. [Google Scholar]
- 9. White HLJ. Maximum likelihood estimation of misspecified models. Econometrica 1982;50(1):1–25. [Google Scholar]
- 10. Huber PJ. The behavior of maximum likelihood estimates under nonstandard conditions In: LeCam LM, Neyman J, eds. Proceedings of the Fifth Berkeley Symposium on Mathematical Statistics and Probability. Volume 1. Berkeley, CA: University of California Press; 1967:221–33 [Google Scholar]
- 11.Centers for Disease Control and Prevention. People who are at increased risk for severe illness. Coronavirus disease 2019 (COVID-19). Available at: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-at-higher-risk.html? CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019- ncov%2Fhcp%2Funderlying-conditions.html. Published 2020. (accessed March 2020).
- 12. Kroenke K, Spitzer RL, Williams JBW, Lowe B.. An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics 2009;50(6):613–21. [DOI] [PubMed] [Google Scholar]
- 13. Gomes T, Juurlink DN, Antoniou T, Mamdani MM, Paterson JM, van den Brink W.. Gabapentin, opioids, and the risk of opioid-related death: A population-based nested case–control study. Tsai AC, ed. PLoS Med 2017;14(10):e1002396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zhu W, Chernew ME, Sherry TB, Maestas N.. Initial opioid prescriptions among U.S. commercially insured patients, 2012–2017. N Engl J Med 2019;380(11):1043–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Page GG. Immunologic effects of opioids in the presence or absence of pain. J Pain Symptom Manage 2005;29(5):25–31. [DOI] [PubMed] [Google Scholar]
- 16. Plein LM, Rittner HL.. Opioids and the immune system – friend or foe. Br J Pharmacol 2018;175(14):2717–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dublin S, Walker RL, Jackson ML, et al. Use of opioids or benzodiazepines and risk of pneumonia in older adults: A population-based case-control study. J Am Geriatr Soc 2011;59(10):1899–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sytsma TT, Greenlund LK, Greenlund LS.. Joint corticosteroid injection associated with increased influenza risk. Mayo Clin Proc Innov Qual Outcomes 2018;2(2):194–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Coutinho AE, Chapman KE.. The anti-inflammatory and immunosuppressive effects of glucocorticoids, recent developments and mechanistic insights. Mol Cell Endocrinol 2011;335(1):2–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Eaton LH, Gordon DB, Wyant S, et al. Development and implementation of a telehealth-enhanced intervention for pain and symptom management. Contemp Clin Trials 2014;38(2):213–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Tenforde AS, Hefner JE, Kodish-Wachs JE, Iaccarino MA, Paganoni S.. Telehealth in physical medicine and rehabilitation: A narrative review. PM&R 2017;9:S51–8. [DOI] [PubMed] [Google Scholar]
- 22. Truter P, Russell T, Fary R.. The validity of physical therapy assessment of low back pain via telerehabilitation in a clinical setting. Telemed J E Health 2014;20(2):161–7. [DOI] [PubMed] [Google Scholar]
- 23. Kang L, Ma S, Chen M, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav Immun 2020;87:11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.