Abstract
Background
Low-wage dormitory-dwelling migrant workers in Singapore were disproportionately affected by coronavirus disease 2019 (COVID-19) infection. This was attributed to communal living in high-density and unhygienic dormitory settings and a lack of inclusive protection systems. However, little is known about the roles of social and geospatial networks in COVID-19 transmission. The study examined the networks of non-work–related activities among migrant workers to inform the development of lockdown exit strategies and future pandemic preparedness.
Methods
A population-based survey was conducted with 509 migrant workers across the nation, and it assessed dormitory attributes, social ties, physical and mental health status, COVID-19-related variables and mobility patterns using a grid-based network questionnaire. Mobility paths from dormitories were presented based on purposes of visit. Two-mode social networks examined the structures and positions of networks between workers and visit areas with individual attributes.
Results
COVID-19 risk exposure was associated with the density of dormitory, social ties and visit areas. The migrant worker hub in the city centre was the most frequently visited for essential services of grocery shopping and remittance, followed by south central areas mainly for social gathering. The hub was positioned as the core with the highest degree of centrality with a cluster of workers exposed to COVID-19.
Conclusions
Social and geospatial networks of migrant workers should be considered in the implementation of lockdown exit strategies while addressing the improvement of living conditions and monitoring systems. Essential services, like remittance and grocery shopping at affordable prices, need to be provided near to dormitories to minimize excess gatherings.
Keywords: COVID-19, health inequity, social determinants of health, migrant workers, social and geospatial networks, mobility patterns, lockdown exit strategy, Singapore
Introduction
Singapore is among the biggest hit countries by the coronavirus disease 2019 (COVID-19) pandemic. As of 15 August 2020, the city–state reported 55 661 laboratory-confirmed cases of COVID-19 in a total of 5.7 million population, the highest number of 975.8 cases per 100 000 in Asia, compared with 2.0 in Taiwan, 29.9 in South Korea, 42.4 in Japan and 58.7 in Hong Kong and 182.9 in India.1 Low-wage dormitory-dwelling workers (‘migrant workers’, hereafter) constituted 94.6% of the cases, with a prevalence rate of 16.3% compared with 0.04% in the local population.2 Such a sharp disparity in COVID-19 infection is explained by high-density and unhygienic living conditions of migrant workers3–5 and a lack of inclusive protection system of equal access to healthcare and social safety nets.6–9
Of 323 000 migrant workers, ~200 000 workers reside in purpose-built dormitories (PBDs; specially built with features for their needs); the rest are housed in dormitories converted from disused industrial sites and other unlicensed residences.10 Although a minimum of 4.5 square meters of ‘living space’ per worker in PBDs is mandated,11 nearly half breached licencing conditions every year.12 Migrant workers are excluded from the state planning of healthcare and covered by medical insurance that employers purchase for workers under their charge, without eligibility for subsidized healthcare.9,13,14 Healthcare quality is limited to meeting compliance standards of immigration procedures and occupational safety.15 They are covered only for care for acute conditions but not for specialized outpatient treatments, allied health (e.g. physiotherapy), rehabilitative, preventive or mental health services.9
From the early COVID-19 outbreak, Singapore undertook a whole-of-government approach by establishing a Multi-Ministry Task Force.16 It implemented effective measures to limit the importation of COVID-1917 and augmented active case finding, extensive contact tracing and quarantine, testing, clinical management and community and social measures.16,18 The Ministry of Manpower (MOM) issued advisories to dormitories on maintaining clean residential premises and promoting personal hygiene among workers. However, the monitoring system was lacking.19 As COVID-19 continued to spread in the local community, much of the government’s focus was on curbing spread among local residents. The potential risk of migrant workers’ contracting COVID-19 was not given much priority.17 It was not long before the vulnerability of this population became evident. From the first confirmed case among migrant workers reported on 9 February 2020, another four colleagues of the index case, who lived at ‘different’ dormitories, were infected.20
Since then, the cases among migrant workers have risen sharply despite immediate contact tracing and disinfecting affected sites.21 MOM’s guideline for precautionary measures in dormitories was not successfully implemented due to crowdedness in the dormitory, sharing facilities (e.g. toilet and shower rooms), lack of supplies of masks and hand sanitizers and inadequate manpower resources. Since the first cluster at S11 dormitory, which housed 13 000 workers, on 30 March, the number of cases in various dormitories has escalated exponentially. In total, 25 out of 43 PBDs were declared as isolation areas within 1 month from the first case.
Singapore implemented a ‘circuit breaker’ phase (a local term for lockdown) for 2 months from 7 April. While migrant workers were confined, extensive swab operations and serological testing were undertaken in all dormitories. Medical and recovery services were established to transfer infected workers with mild symptoms to ‘community care facilities’ and recovered workers to ‘community recovery facilities’ before their transition to work.22 As of 15 August, 22 800 workers yet remained in centralized government isolation facilities.
Two weeks before the end of ‘circuit breaker’, the government laid out a three-phase approach to exit lockdown: (i) safe reopening, (ii) safe transition and (iii) safe nation.23 Accordingly, the government was set to resume construction projects with transition strategies, including regular testing to identify those with asymptomatic infection and safe distancing guidelines for workplaces and construction sites.24 Although these strategies are essential to allow migrant workers to resume their economic roles in due time, special attention needs to be paid to non-work–related activities of workers. The lockdown has slowed the transmission of COVID-19, yet the sustained human-to-human spread will still occur in the community. Migrant workers remain at high risk of contracting the disease if there are no guidelines to provide guidance when they engage in non-work activities. Knowledge of the social-ecological contexts of the activities in the population is crucial to implement a well-informed lockdown exit strategy to protect workers and prevent further spread of COVID-19. The study was designed to address the issue with its objectives to examine social and geospatial network patterns of non-work–related activities among workers and to develop responsible and effective lockdown exit strategies for the population.
Methods
Sampling and procedure
A survey was conducted on 22–26 April 2020. Ethics committee approval was obtained. As in-person contacts with workers were not allowed during ‘circuit breaker’, several recruitment strategies were employed. The study invitation flyers in English, Bengali, Tamil and Chinese were distributed to migrant workers through non-governmental organizations (NGOs). We contacted social networking sites (SNS; Facebook) run by migrant workers, who were ‘SNS influencers’ with a large number of migrant worker followers. With permission, the survey invitation was posted on their SNS. There were meal distribution services to dormitories. The flyers (>300 copies) were handed with meals to workers. We also adopted a participant-driven sampling, frequently used in behavioural surveillance in hard-to-reach populations.25 Migrant workers were asked to refer their friends outside their dormitories to the survey. To increase the heterogeneity of the sample, friends in their dormitories were excluded. They received the same amount of survey incentive if five of their referrals completed the survey. They were offered either a phone interview or an online survey in English and Bengali. Those confident with completing an online survey were given the link to it. Bilingual volunteers, who provided translation services at NGOs, were trained and conducted interviews. The survey took up to 30 minutes to complete. Verbal informed consent was obtained before the survey. They received SG$10 (US$7) top up to their prepaid mobile phone. A total of 509 migrant workers completed the survey (Supplementary Figure S1).
Measures
The survey measures included: (i) living conditions, (ii) social ties, (iii) physical and mental health, using Kessler Psychological Distress Scale26 and (iv) COVID-19 knowledge, source of information, perceived susceptibility, self-efficacy and COVID-19 risk exposure, assessed by whether they had infected friends. All the infected workers were transferred to isolation facilities. Thus, all survey respondents were either COVID-19 negative or not tested. Social and geospatial networks of non-work–related activities were assessed using a grid-type measure, asking to answer the following question, ‘On your rest day, where do you usually go? List the places you usually went on your rest day before “circuit breaker” based on (i) place, (ii) time, (iii) purpose and (iv) number of friends’ up to five events (Supplementary Table S1).
Analysis
For geospatial analysis, we prepared the geographic data by generating latitude and longitude coordinates of the workers’ residences and visit destinations. We categorized the 106 identified locations of visit into nine areas in a combination of the official districts and migrant worker communities to contextualize their mobility data27 (Supplementary Figure S2, Tables S2 and S3). The frequency of visit to each area and the density according to the following purposes were presented: (i) grocery shopping, (ii) remittance, (iii) social gathering, (iv) outdoor leisure, (v) religious activities, (vi) movie/cinema, (vii) medical care, (viii) dating and (ix) training. ArcGIS was used to draw the lines of mobility paths between dormitories and destinations by purposes among low-wage dormitory-dwelling migrant workers.
The relations between workers and visit areas were examined using two-mode networks where workers were linked to each other through the places they visited.28 To identify the most influential areas in the network, three key centrality metrics were calculated: (i) degree (the number of workers connected to each area); (ii) closeness (how close each place node is to the other nodes based on the number of ties separating the nodes); (iii) betweenness (how frequently a place node lies on the shortest path between two nodes).29 UCINET was used for network analysis and NetDraw for visualization. The nodes of visit areas were arranged to reflect their approximate locations on the Singapore map and geographical proximity. The worker nodes were coloured according to various attributes to determine if individual characteristics influence where workers visited, and by extension, their susceptibility to infection.
Results
Participant characteristics
Forty percent of workers were from 35 PBDs out of a total of 43 PBDs (coverage rate: 81.4%). Figure 1 shows the location of PBDs by isolation and recruitment.
Figure 1.
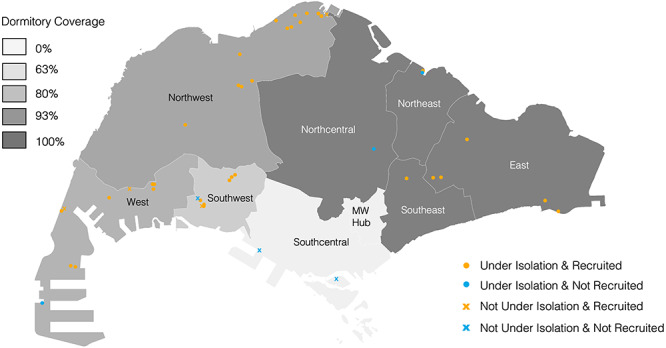
Locations of 43 PBDs by COVID-19 isolation (n = 25) and recruitment
The majority were aged between 20 and 40 years old (90%), from Southeast Asia (91%), completed at least secondary education (83%) and worked in construction (76%) and shipyard (11%). The mean number of work years in Singapore, work hours per day and rest days per month were 7 years, 10 hours and 3 days, respectively. The mean monthly income was SG$828 (US$590). The mean numbers of workers living per room and rooms on the level were 10.4 [standard deviation (SD) = 7.2] and 8.2 (SD = 13.0). About five showers and toilets were provided on the floor, indicating that about 16 workers shared one shower/toilet if all function properly. About three quarters had a minimart or supermarket in their dormitories or nearby. The mean numbers of migrant worker friends from their dormitories and other dormitories were 6.1 (SD = 8.4) and 4.8 (SD = 8.1) and foreign domestic workers and locals were 2.2 (SD = 7.9) and 1.4 (SD = 8.2) (occupation-related diseases and mental health in Supplementary Tables S5–S7).
COVID-19 variables
The majority (90%) reported correct knowledge of COVID-19 and measures of protection. Most (84%) actively sought for COVID-19 information and 74% responded to having sufficient information. The sources of the information included SNS (83%), government notices (78%), friends and co-workers (60%), news media from Singapore (52%) and home (52%) countries. Two-thirds (65%) were worried about getting infected in the past week, 47% responded that they would likely to be infected in the next 1 month and 25% didn’t feel confident in COVID-19 protection and prevention of spread to others. About a quarter (24%) had at least one infected friend. The level of COVID-19 exposure was associated with residence type and density, social ties and visit to the migrant worker hub (MW hub). (See Supplementary Tables S4–S7 for the comparisons.)
Frequency and density of mobility patterns
The top three purposes were social gathering (34%), grocery shopping (34%) and remittance (32%), followed by religious activities (14%), outdoor leisure (13%), medical care (2%) (Supplementary Table S8). Figure 2 presents the frequency and density of visits for the three primary purposes: essential services of grocery, remittance and non-essential activities of social gathering. While PBDs are located remotely across the island, the visit areas with more frequency were concentrated in the city centre, in particular, the MW hub for essential services. South central area was mainly for social gatherings.
Figure 2.
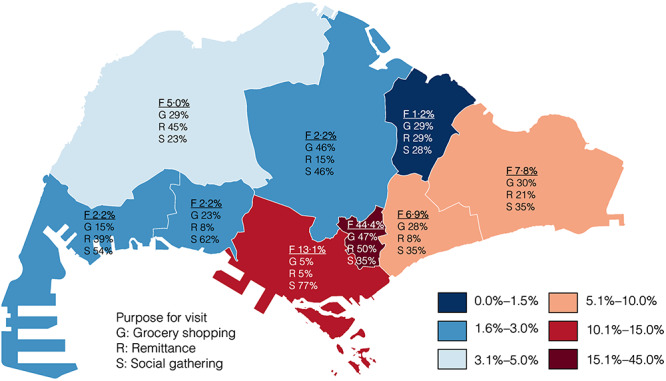
Mobility patterns by frequency (F) and density of purpose (G, R, S)
Mobility paths from PBD to destination
As seen in Figure 3, the most frequented destinations fell into three categories: (i) the MW hub, (ii) public areas on the coast (e.g. parks) throughout the island and (iii) marketplaces (e.g. malls) near to their dorms (Supplementary Figure S3). Different patterns of visits were observed by purpose. The destinations of visit for grocery shopping were highly concentrated on the MW hub or places near to PBDs. Compared with grocery shopping, fewer visits were made to places nearby for remittance. Unlike essential activities, mobility paths for social gatherings were very diverse and divergent, and the destinations of visit were spread across the island, including places of indoor and open areas of parks on the coast.
Figure 3.
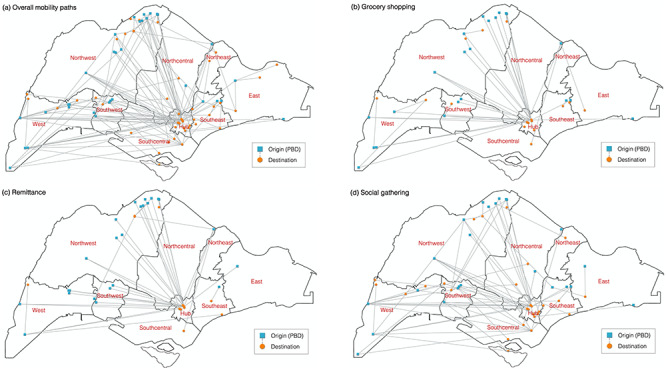
Mobility paths from dormitories to destinations (a) overall, (b) grocery shopping, (c) remittance and (d) social gathering
Two-mode networks
The MW hub was positioned as the core in the network with the highest degree, closeness and betweenness, which was followed by south central and east (Figure 4). Most workers were connected through the core. The visit areas near PBDs are positioned at the peripheral.
Figure 4.
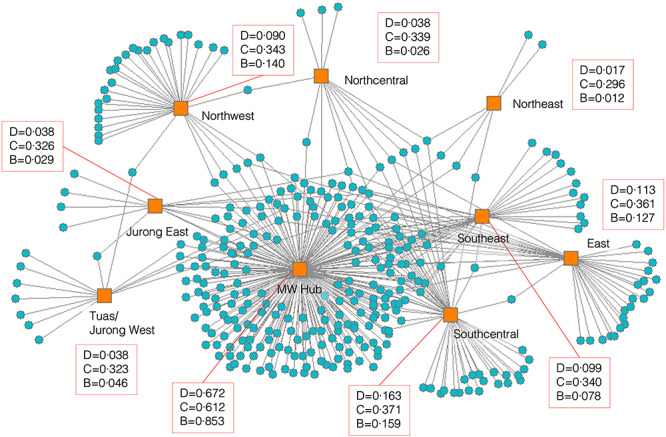
Two-mode social networks between actors (migrant workers) and designations of visit with centralities of D (degree), C (closeness) and B (betweenness)
The networks were explored with individual attributes of social ties, having a grocery market nearby and having a friend(s) with COVID-19 (Figure 5; Supplementary Figure S4). Migrant workers who reported lower social ties with friends were more seen at the peripheries with lower degrees of centrality like west, south-west, north-central and north-west areas. A similar pattern was found in the social network of having a local friend(s). Areas with a high degree of centrality were associated with increasing social ties. At peripheral areas like west, south-west and north-west, migrant workers who had a supermarket nearby did not visit the MW hub. Figure 5(d) shows the cluster of migrant workers who had a friend(s) infected with COVID-19 linked to at the core.
Figure 5.
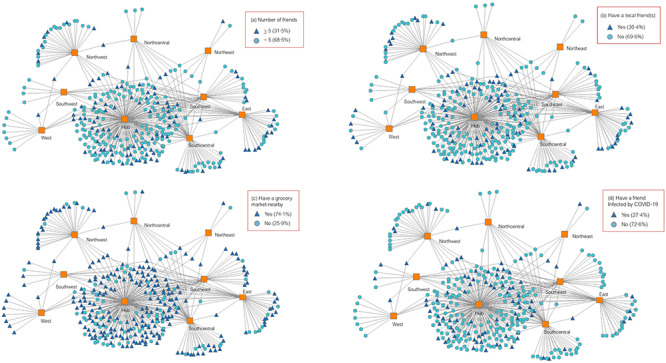
Two-mode social networks with attributes: social ties with (a) migrant worker friends and (b) locals, (c) have a grocery market near to dormitory and (d) have a friend(s) infected by COVID-19
Discussion
The study addressed a central question of what should be known to develop an effective lockdown exit strategy for the population of low-wage dormitory-dwelling migrant workers, using social and geospatial data. Also, it heeds the global call for inclusive protection systems and responsible public health information and communication for migrant workers in response to COVID-19.8 With the lockdown exit strategies, it is critical to identify to what extent and in what form of social distancing, if any, should be prescribed among migrant workers to prevent a resurgence of COVID-19 while resuming economic sectors. The findings indicate that migrant workers are at high-risk of COVID-19 owing not only to living in overcrowded and unhygienic dormitories but also through highly clustered mobility paths for essential services, which are unavailable near their residences. As a result, although most dormitories are located remotely, they are connected through geospatial networks, suggesting a case of COVID-19 in a dormitory from the west region can be easily spread to the east region through the core MW hub with a high degree of closeness and betweenness.
One of the key components in social distancing is mobility restriction. Many migrant workers who have supermarkets nearby visit the MW hub for grocery shopping. The reason for the visit, we found from the workers, is that the supermarkets in dormitories are more expensive than those in the hub. Implementing mobility restriction as a measure to reduce community transmission is only possible when their needs can be met without mobility. It is possible to impose mobility restrictions if supermarkets in closer proximity provide more affordable products. In peripheral areas like west, south-west and north-west, workers who have a supermarket nearby did not visit areas with higher degrees of centrality. Another main reason for the visit to the MW hub was remittance, which was less available than supermarkets. Provision of the essential services nearby will effectively reduce their mobility from the periphery to the core of networks. As most workers are familiar with SNS, introducing them to mobile applications for remittance can help reduce unnecessary visits.
The purposes of mobility are complex and hard to control. Visiting a specific location can serve multiple purposes. Migrant workers go to the hub to buy food, send money, attend prayer sessions at mosques, meet people and so on. Thus, venue-based confinement of the place with strong ties, like the hub, might give confusing messages and lead to increasing public mistrust if there is no evidence to support it, and their essential activities are not directly be addressed.30 Restriction of public gathering in one venue might increase more traffic in other places that serve similar purposes. Instead, measures should focus on offering more alternative locations for essential services to disperse what is now a highly centralized network. Decentralizing essential services across the island will also address distributive justice of fair allocation of necessities for migrant workers.
The finding that they had good knowledge of COVID-19 acquired from various sources, including government notices and SNS, indicated the effective health communication made to migrant workers.6 The penetration of public health information, which was gained from the control of COVID-19, has the potential to prepare future pandemic. While the mobility restriction of migrant worker will be gradually lifted in the coming months, structural interventions are necessary to turn the emerging formal and informal health communication and response channels into well-coordinated systems so that migrant workers continue to benefit from them not only for infectious disease outbreak but also for overall health promotion and disease protection. Notably, there is a discrepancy between good knowledge and high perceived susceptibility, suggesting the need to improve self-efficacy and coping strategies with COVID-19. The discrepancy might also result from their perceived protection from the government in terms of responsible public communication with them.6,8 Their existing conditions also affect their perceived susceptibility. About a quarter reported chronic cold-like symptoms, which is similar to those of COVID-19, and one-third experienced mild to severe distress. Easy access to mental health services will alleviate their distress and promote self-competence.
It is important to recognize the importance of the MW hub as a potential avenue to strengthen protective systems and community resilience against future pandemics in the population.24 The hub could function positively in the time of ‘new normal’ with a critical mass for the diffusion of innovation for health protection.31 The highest degrees of centralities suggest the hub could play a role as ‘gate-keeping’ to either block the diffusion of health information or facilitate it to other regions rapidly.32 The direction of either closure or opening will be dependent on how the public health agencies engage with the migrant worker community in the post-COVID-19 pandemic period.3,33
There are limitations. The majority in the sample were Southeast Asian. Migrant worker population in Singapore is a mix of different nationalities and ethnicities. Mobility paths of non-work–related activities might differ for each group. While the sample characteristics were representative in terms of the proportion of dormitory types, mobility paths were presented only from PBDs. Those who lived outside dormitories might have different paths. The study only assessed the network relations between workers and places. Thus, networks between workers are unknown. Network analyses were mainly descriptive. Further research is needed to examine the mediating effects between social networks and built environments to identify intervention focal points. Importantly, social and geospatial networks were discussed mainly from the perspectives of mitigating and managing ‘risk’. The networks also play an important role in building up resilient healthy community systems. Thus, future research should explore the protective roles of the networks among at-risk migrant workers.
Conclusions
Our study highlights the importance of distributive justice concerning the equal allocation of essential services, including healthcare and living necessities, for low-wage dormitory-dwelling migrant workers, who are disproportionately affected by COVID-19 largely due to high-density and unhygienic built environment. Exclusionary healthcare policies put the responsibility of providing for migrant worker’s health needs to the employers and thereby limit the access to preventive health services and increase the risk of developing health adversities.9 In efforts to address the structural barrier and to contain the spread of COVID-19 among migrant workers, Singapore’s multi-ministry task force has made significant efforts by increasing geographic accessibility to testing and treatment facilities,16,34 which is a key to controlling the epidemic.35 Such a multi-sectoral response system involving the MOM and the Ministry of Health should continue to provide migrant workers with coordinated care in the time of post-pandemic.36
Globally, the COVID-19 pandemic has unmasked health inequity and shed light on the complex pathways from socio-economic exclusion to infection of the disease in the diverse populations of low-wage migrant workers, racial and ethnic minorities, refugees and other marginalized people with residential instability.37–39 Individuals from lower socio-economic strata often are ‘essential workers’ with pre-existing health conditions and have to continue working during lockdowns; they were thus at higher risk of exposure, and hence disease, including deaths than the general population.40 While the risk factors of adverse health outcomes are context specific and epi-historical dependent, the literature evidences structural causes of health disparities—lack of legal, social and health protection in inadequate living conditions—and calls for accountability in global health justice.8,38 Although the COVID-19 pandemic has thrown the world into disarray, it presents us an opportunity to work together towards health equity, ensuring equal and easy access to resources for tests, treatments and future vaccines for migrants and ethnic minorities.
Authors’ Contributions
H.Y. and J.L. conceived the study design. H.Y. secured funding for the study. S.T.N., A.F., A.P.T.L. and C.M.C. managed the data collection. H.Y. and S.T.N. conducted the data analysis. S.T.N. produced output figures with input from H.Y. A.F, A.P.T.L. and C.M.C. conducted literature review. H.Y. wrote the first draft of the manuscript. J.L. provided critical feedback on the draft. All authors contributed to the interpretation of the results, reviewed and approved the final version for publication.
Supplementary Material
Acknowledgements
We thank the migrant workers who participated in this research for their time. We thank the staff members and volunteers at HealthServe, who worked to enhance the well-being of migrant workers. We especially thank Jeffrey Chua and Michael Cheah at HealthServe for providing valuable suggestions for this project and insightful feedback on this paper. We also thank TWC2 (Transient Workers Count Too) that helped the distribution of the study invitation flyers to migrant worker dormitories.
Contributor Information
Huso Yi, Saw Swee Hock School of Public Health, National University of Singapore and National University Health System, Singapore.
Shu Tian Ng, Saw Swee Hock School of Public Health, National University of Singapore and National University Health System, Singapore.
Aysha Farwin, Saw Swee Hock School of Public Health, National University of Singapore and National University Health System, Singapore.
Amanda Pei Ting Low, Saw Swee Hock School of Public Health, National University of Singapore and National University Health System, Singapore.
Cheng Mun Chang, Saw Swee Hock School of Public Health, National University of Singapore and National University Health System, Singapore.
Jeremy Lim, Saw Swee Hock School of Public Health, National University of Singapore and National University Health System, Singapore.
Funding
The NUHS Special COVID-19 Grant, NUS Start-Up Grant and COVID-19 National Effort Fund.
Conflict of interest: None declared.
References
- 1. Johns Hopkins University Coronavirus Resource Center COVID-19 dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU). https://coronavirus.jhu.edu/map.html (20 August 2020, date last accessed).
- 2. Ministry of Health Singapore Updates on COVID-19 local situation report. https://moh.gov.sg/covid-19/situation-report (20 August 2020, date last accessed).
- 3. Bagdasarian N, Fisher D. Heterogenous COVID-19 transmission dynamics within Singapore: a clearer picture of future national responses. BMC Med 2020; 18:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jefferson T, Del Mar CB, Dooley L et al. Physical interventions to interrupt or reduce the spread of respiratory viruses. Cochrane Database Syst Rev 2011; CD006207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lim J Coronavirus: workers describe crowded, cramped living conditions at dormitory gazetted as isolation area. The Strait Times 6 April 2020. https://straitstimes.com/singapore/manpower/workers-describe-crowded-cramped-living-conditions (20 August 2020, date last accessed). [Google Scholar]
- 6. Liem A, Wang C, Wariyanti Y et al. The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiatry 2020; 7:e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Kluge HHP, Jakab Z, Bartovic J et al. Refugee and migrant health in the COVID-19 response. Lancet 2020; 395:1237–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Orcutt M, Patel P, Burns R et al. Global call to action for inclusion of migrants and refugees in the COVID-19 response. Lancet 2020; 395:1482–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Rajaraman N, Yip T-W, Kuan BYH et al. Exclusion of migrant workers from national UHC system: perspectives from HealthServe, a non-profit organisation in Singapore. Asian Bioeth Rev 2020. doi: 10.1007/s41649-41020-00138-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ministry of Manpower Singapore Housing for foreign workers. https://mom.gov.sg/passes-and-permits/work-permit-for-foreign-worker/housing (20 August 2020, date last accessed).
- 11. Urban Revelopment Authority Singapore Independent Workers’ Dormitories. https://ura.gov.sg/corporate/guidelines/development-control/non-residential/c-ci/wd (20 August 2020, date last accessed).
- 12. Cheong D Nearly half of large dorms breach rules each year, says Josephine Teo. The Strait Times 5 May 2020. https://straitstimes.com/singapore/manpower/nearly-half-of-large-dorms-breach-rules-each-year-minister (20 August 2020, date last accessed). [Google Scholar]
- 13. Ang JW, Chia C, Koh CJ et al. Healthcare-seeking behaviour, barriers and mental health of non-domestic migrant workers in Singapore. BMJ Glob Health 2017; 2:e000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lee W, Neo A, Tan S et al. Health-seeking behaviour of male foreign migrant workers living in a dormitory in Singapore. BMC Health Serv Res 2014; 14:300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ministry of Manpower Singapore Employment of foreign manpower act. https://mom.gov.sg/legislation/employment-of-foreign-manpower-act (20 August 2020, date last accessed).
- 16. Lee VJ, Chiew CJ, Khong WX. Interrupting transmission of COVID-19: lessons from containment efforts in Singapore. J Travel Med 2020; 27. doi: 10.1093/jtm/taaa039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Chiew CJ, Li Z, Lee VJ. Reducing onward spread of COVID-19 from imported cases: quarantine and 'stay at home' measures for travellers and returning residents to Singapore. J Travel Med 2020; 27. doi: 10.1093/jtm/taaa049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Archuleta S, Cross G, Somani J et al. Responding to COVID-19: how an academic infectious diseases division mobilized in Singapore. BMC Med 2020; 18:179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Ministry of Manpower Singapore Advisory for dormitory operators on implementation of safe living measures in foreign worker dormitories. https://mom.gov.sg/covid-19/advisory-for-dormitory-operators-on-safe-living-measures-foreign-worker-dormitories (20 August 2020, date last accessed).
- 20. Tariq A, Lee Y, Roosa K et al. Real-time monitoring the transmission potential of COVID-19 in Singapore. BMC Med 2020; 18:166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Koh D Migrant workers and COVID-19. Occup Environ Med 2020; oemed-2020-106626. doi: 10.1136/oemed-2020-106626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Ministry of Manpower Singapore Advisory to employers with foreign workers living in dormitories. https://mom.gov.sg/covid-19/advisory-to-employers-with-foreign-workers-living-in-dormitories (20 August 2020, date last accessed).
- 23. Singapore Government Ending circuit breaker: phased approach to resuming activities safely. https://gov.sg/article/ending-circuit-breaker-phased-approach-to-resuming-activities-safely (20 August 2020, date last accessed).
- 24. Gilbert M, Dewatripont M, Muraille E et al. Preparing for a responsible lockdown exit strategy. Nat Med 2020; 26:643–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tiffany JS Respondent-driven sampling in participatory research contexts: participant-driven recruitment. J Urban Health 2006; 83:i113–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kessler RC, Andrews G, Colpe LJ et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med 2002; 32:959–76. [DOI] [PubMed] [Google Scholar]
- 27. Singapore Land Authority SLA land Survey District. https://data.gov.sg/dataset/sla-land-survey-district (20 August 2020, date last accessed).
- 28. Borgatti SP Two-mode concepts in social network analysis In: Encyclopedia of Complexity and System Science 2009; 6:8279–91. SpringerLink. [Google Scholar]
- 29. Freeman L Centrality in social networks: conceptual clarification. Soc Netw 1979; 1:215–39. [Google Scholar]
- 30. Lewnard JA, Lo NC. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect Dis 2020; 20:631–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wejnert B Integrating models of diffusion of innovations: a conceptual framework. Annu Rev Sociol 28:297–326. [Google Scholar]
- 32. Granovetter MS The strength of weak ties. Am J Sociol 1973; 78:1360–80. [Google Scholar]
- 33. Willen SS, Knipper M, Abadia-Barrero CE et al. Syndemic vulnerability and the right to health. Lancet 2017; 389:964–77. [DOI] [PubMed] [Google Scholar]
- 34. Ministry of Manpower Singapore All dormitories declared cleared of COVID-19. https://mom.gov.sg/newsroom/press-releases/2020/0811-all-dormitories-declared-cleared-of-covid-19 (20 August 2020, date last accessed).
- 35. Rader B, Astley CM, Sy KTL et al. Geographic access to United States SARS-CoV-2 testing sites highlights healthcare disparities and may bias transmission estimates. J Travel Med 2020. doi: 10.1093/jtm/taaa076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mann EM, Klosovsky A, Yen C et al. Health challenges in refugee resettlement: an innovative multi-sector partnership to improve the continuum of care for resettled refugees. J Travel Med 2020. doi: 10.1093/jtm/taaa103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Bonfiglio G, Rosal K, Henao-Martinez A et al. The long journey inside immigration detention centers in the U.S. J Travel Med 2020. doi: 10.1093/jtm/taaa083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Greenaway C, Hargreaves S, Barkati S et al. COVID-19: exposing and addressing health disparities among ethnic minorities and migrants. J Travel Med 2020. doi: 10.1093/jtm/taaa113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Millett GA, Jones AT, Benkeser D et al. Assessing differential impacts of COVID-19 on black communities. Ann Epidemiol 2020; 47:37–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Price-Haywood EG, Burton J, Fort D et al. Hospitalization and mortality among black patients and white patients with COVID-19. N Engl J Med 2020; 382:2534–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


