Abstract
The SARS-CoV-2 virus was initially contained in China but rapidly spread across the globe. The grave threat was not apparent until it was already in our midst. Our organization implemented an Incident Command System (ICS), based on previous experience, to respond to the COVID-19 pandemic in a comprehensive and effective manner. This well-known management and response framework is used by many specialties and organizations in disasters of different complexity and size. Our ICS was able to assemble the appropriate people, assess the situation, and develop and implement plans to deal with the COVID-19 crisis. The effectiveness of the ICS structure and its execution was instrumental in getting in front of the virus and managing regional activities. The ICS is an effective tool to improve safety and mitigate risk when dealing with large-scale disasters and should be implemented and practiced before the need arises.
Our organization implemented a formal Incident Command System (ICS) very early as a response to the COVID-19 pandemic. Although it recently disbanded, we are maintaining its core functionality and communication as we continue to deal with COVID-19 into the future. The author has observed the ICS being used at hospitals through hurricanes, blizzards, and riots but never saw it work as well as it did during the initial weeks of the pandemic. This group deftly navigated through uncharted waters by leveraging the spirit and structure of Incident Command.
Keywords: management, operations, incident command, COVID, supply chain, pandemic
Incident Command System
The ICS was developed by U.S. firefighting agencies in the 1970s as a response to dealing with wildfires in Southern California. The original group was called Firescope (Firefighting Resources of Southern California Organized for Potential Emergencies) and is still in existence today. Firescope developed the original concept of the ICS structure to improve the effectiveness of intra-agency cooperation and communication when responding to potentially disastrous emergencies or incidents. Initial work for the group was done by the U.S. Forest Service as a research and development effort. Many of the participants had military backgrounds, and this was reflected in the hierarchical nature of the ICS structure to support centralized command and control in high-stakes environments. Firescope continues to work on expanding the theory and applicability and providing training and resources for the ICS process.1
The terrorist attacks on September 11, 2001, brought additional attention to the ICS. As a result of the complex nature of the event and lessons learned, former President George W. Bush established the National Incident Management System (NIMS) to identify an appropriate working structure to help coordinate all responders in a major event. The ICS seeks to establish centralized command and control for rapid and effective response to disasters. The NIMS is now part of the Federal Emergency Management Agency, a division of the U.S. Department of Homeland Security. The ICS has been heavily tested in real-life scenarios such as Hurricanes Katrina, Sandy, and Harvey. Expansion of the theory and practice of the ICS continues to evolve as we respond to new challenges.
The success of the ICS is based on its clear objectives as outlined by Phibbs and Snawder.2
Create a set of objectives and goals
Develop appropriate tactics
Ensure allocation of resources
Review the plan and confirm that it is sound
Communicate goals, tactics, and expectations
Establish accountability
The ICS has been used by many agencies in many situations. Because of its effectiveness and adaptability, it has been used in fires, natural disasters, search and rescue, hazardous materials situations, disease outbreaks, and criminal acts and investigations. Phibbs and Snawder2 described its use, effectiveness, and applicability in law enforcement. It has also been encouraged and used in health care. The Hospital Emergency Incident Command System (HEICS) was created in the late 1980s. It serves as a basis for hospital emergency preparedness and planning in the United States. There is applicability and effectiveness of the ICS in emergency situations to protect health and safety and sustain operations.
The flexibility, adaptability, and scalability of the ICS make it ideal as an off-the-shelf solution to dealing with complex situations and problems involving risk and safety with multiple stakeholders and various levels of expertise. Although it is not perfect, the ICS creates a complete structure for planning and responding to disasters.3 A formal ICS has 7 principles, including4 standardization, functional specificity, a manageable span of control, unit integrity, unified command, management by objectives, and comprehensive resource management. These principles are addressed by having definitions and common terminology to establish effective communication and expectations. By simplifying and streamlining, these concepts can be codified into manageable work units with an appropriate span of control and accountability. The simplicity of the principles and responsibility for each member is built into the structure and tasks for the essential functioning of the ICS. By having clearly defined roles and a hierarchical reporting structural, each unit can work within its assigned parameters to accomplish tasks, request resources, and report.
The roles for a basic ICS system are defined but can be adapted to meet a variety of incidents. Objectives are carried out through 5 major functional areas5: command, operations, planning, logistics, and finance/administration. There is almost no end to resources available for the ICS structure, including training, examples, practical application, and forms/documentation. Anyone with leadership roles or aspirations is encouraged to study and complete training on ICS to improve value to an organization and to society. Resources are listed at the end of this article.
ICS in Action
The first case of COVID-19, caused by SARS-CoV-2 infection, in the United States was diagnosed in Snohomish County, Washington on January 20, 2020.6 The patient had recently returned from Wuhan, China, the epicenter of the pandemic, after visiting family. At the time, much of the United States saw this as an isolated travel-related case without much cause for concern. The first case in Houston, Texas, was reported on March 4, 2020, and was also a travel-related case.7 This was quickly followed by 2 more travel-related cases reported the next day. These cases were all related to travel on a cruise ship in Egypt. Houston reported its first case of community-spread COVID-19 on March 11, 2020.8 At that time, much of the country and the world were in denial that a pandemic would occur. Other SARS outbreaks had been contained, and there was widespread belief that this would be no different. However, as the scope and impact became apparent, there was a justifiable increase in anxiety and incentive to begin serious preparations to combat the spread of the virus. Our health system convened the System-Wide Incident Command Center on March 12.
At the time, the Houston region had only 17 patients with confirmed cases of COVID-19. Although this number, in a city of 6.4 million, seems insignificant and manageable, our leadership had the foresight to take it seriously and begin preparations to address potential concerns. By establishing the ICS so early, we were able to plan appropriately and get ahead of the curve to mitigate risk.
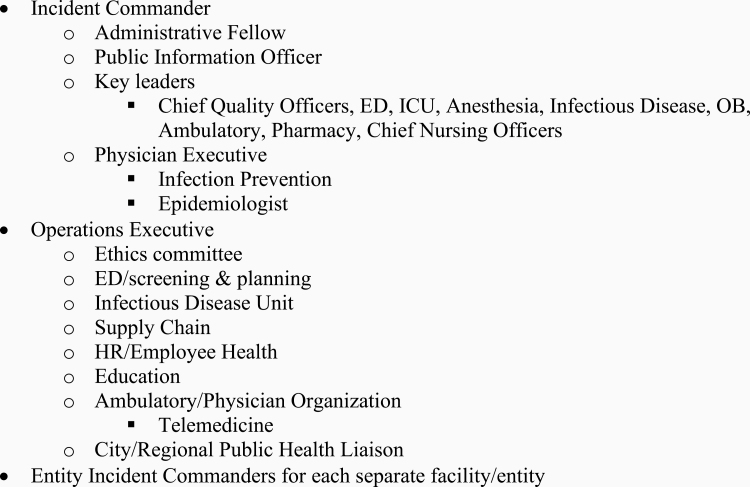
The structure included a Centralized Incident Command structure with the following components and support roles, listed beneath each function (Figure 1).
Figure 1.
COVID incident command structure.
This core group was supplemented by other permanent roles and additional ad hoc membership as needed. The group met with social distancing rules in place at our central hospital and via WebEx. The ICS met 3 times daily (twice on weekends), 7 days a week for the first month and a half. It reduced the meeting frequency to twice a day after that and officially disbanded on May 5, 2020, for a running total of 55 days in action.
The most impressive feature of our ICS was not the scope and volume of specific issues they dealt with, or even the velocity and fluidity of the situation. The most impressive role they played, collectively, was to prepare our organization, our staff, our patients, and our city to deal with the pandemic in the best way possible. This included assessment, evaluation, planning, resourcing, and implementing plans along several fronts.
In addition to identifying and addressing individual issues, the ICS ensured coordinated efforts to achieve optimal outcomes and reduce duplicative efforts and unnecessary anxiety. The ICS anticipated needs and sourced them appropriately. Because conventional wisdom initially indicated that the epidemic would not develop, COVID-19 was able to get a slight advantage and foothold. However, this advantage did not last long. As events quickly unfolded in Washington State, New York, and across the globe, the potential threat was clear. By starting our ICS just days after our first cases of infection and community spread, our organization quickly caught up and moved ahead of the curve.
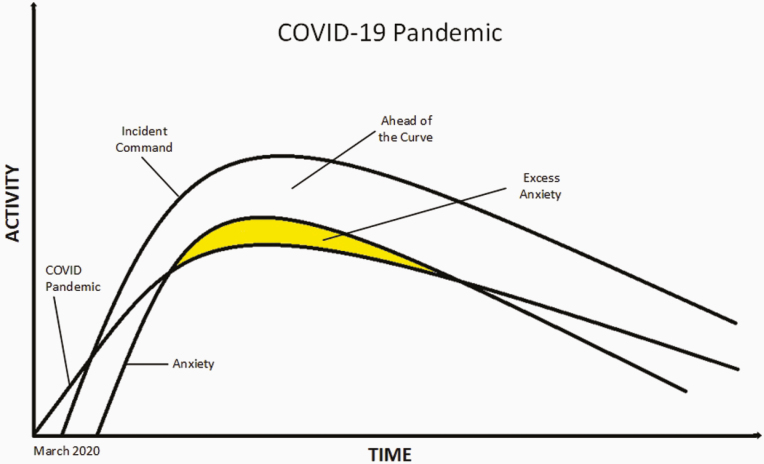
The ICS not only allowed our organization to confront challenges in real time in an effective manner, but it also reduced stress and anxiety at the same time. The ICS helped focus leadership time and attention on those issues that mattered most. As we addressed each issue, the entire organizational response improved, and tension decreased with the flow of information and plans (see Figure 2).
Figure 2.
COVID pandemic trajectory.
Anxiety lagged behind the pandemic because of a lack of total awareness of the potential implications, potential severity, and denial. As awareness increased, so did anxiety. This anxiety was alleviated through the ICS by the sharing of accurate information to protect ourselves and our patients and understanding that there were definitive plans, people, and other resources in place to confront the issues using a rational, targeted approach.
Questions
The ICS had the breadth and depth of organizational expertise to ask the right questions and come up with the right answers. Disasters and planning are not new, but the magnitude of the COVID-19 pandemic forced us to consider problems that were truly novel, like the virus. Following are some of the challenges that the ICS addressed:
Safety—How can we ensure the safety of our staff, providers, and patients while meeting the needs of our larger community?
Staffing—How can we manage our staff to ensure they are protected, effective, available, and cared for with all we are asking of them?
Testing—How can we gear up to provide appropriate testing to diagnose and monitor the progression of the virus?
Personal Protective Equipment (PPE)—How can we provide the tools and safeguards necessary in the face of massive shortages?
Visitors—How can we care for and protect our patients and staff in a compassionate manner while limiting access?
Triage and isolation—How can we handle the substantial separation and isolation needs of our patients with COVID-19?
Supply chain—How can we continue to source scarce, critical, and even common items when everyone else is trying to do the same thing?
Finance—How can we keep our health system financially viable when we are shutting down service lines?
Physician organization—How can we utilize our medical staff effectively to provide care when routine medical services are at a standstill?
Treatment—How do we care for these patients presenting with a novel virus and novel manifestations of COVID-19?
Therapeutics—What medications are effective for these patients, and how do we get sufficient quantities when everyone else is competing for them?
Blood donations—How will we maintain our blood supply when our donors are afraid to leave their homes?
Post-COVID-19 recovery—What will health care look like after this, and how will we safely get our services back online?
Answers
More important than these questions (and many more) were the answers. The collective expertise of the ICS members and the entire health system staff allowed us to develop the optimal solutions in real time—not only to cope, but to succeed. The following list is incomplete because it is not possible to identify and catalog all the innovative solutions and because we are not done yet. We continue to break ground in addressing current and future needs.
Staffing—Early adoption of workforce assessment and development of a central labor pool and work-from-home options. Numerous programs aimed at supporting and nurturing staff during extraordinary circumstances.
Highly Infectious Disease Unit—Reopened our Ebola-era Highly Infectious Disease Unit to cohort appropriate patients and manage capacity across the system.
Virtual visits—Leveraged experience with our robust virtual visit program when it became a necessity rather than a convenience.
Sourcing—Allow supply chain management flexibility to procure supplies and equipment for our system, from swabs to respirators and everything in between.
Virtual ICU—Tapped into our nascent virtual ICU program to provide clinical expertise wherever and whenever it was needed.
Treatment—Established several clinical trials for promising drugs and transfused the first COVID-19 convalescent plasma product in the nation.
Infection control—Evaluated all facets of infection prevention and control and developed creative solutions and materials to protect patients and staff, including alternative processes and procedures, when warranted.
Technology—Developed and maximized use of our electronic medical record and informatics to document, automate, report, study, and improve COVID-19 care.
Testing—Established in-house emergency use authorization polymerase chain reaction test to diagnose and monitor COVID-19. Acquired and validated several additional platforms for detection of SARS-CoV-2 and antibodies. Established several COVID-19 test collection stations across the region.
Surveillance—Designed and implemented a significant employee surveillance program.
Engineering—Worked with engineering/medical students from Texas A&M University to develop unique containment devices to protect employees and preserve PPE, including an intubation/extubation box, procedure box, and specimen collection pod. Developed 3-dimensional printing applications and unique engineering solutions as a response to product shortages.
Institutional cooperation—Cooperated with local and state governmental health agencies to coordinate citywide efforts to manage COVID-19. Participated in Texas Medical Center (world’s largest medical district, with >60 medical institutions) planning and response efforts to influence and optimize strategies to provide effective care and bend the curve.
These items are just a small example of all the work the ICS oversaw during the first 2 months of the pandemic. We were also dealing with bifurcating emergency departments across the health system, addressing new code blue procedures, coordinating volunteer seamstresses to adapt surgical gowns for practical use, working with local hotels to provide housing for critical personnel, modeling for surge capacity needs, and developing spiritual materials for our staff, leaders, and patients. The ICS allowed us to address all these issues and maximize our effectiveness during a time of unprecedented challenges.
Update
Since this article was first written, Houston & much of the country have faced a second, more significant surge. In July 2020, after easing of mandated restrictions, the COVID-related case load in our health system rose to more than triple the original numbers seen in April—the peak of the first surge. Incident Command Leadership resumed two meetings per day in late June 2020. This team was able to successfully navigate through the second surge, facing previously unimaginable challenges for our health system, patients, and community.
Acknowledgments
I would like to acknowledge and thank Roberta Schwartz, PhD, and Vicki Brownewell, our Incident Command Leaders for the COVID-19 response. Their leadership, together with all the dedicated and talented members of the Incident Command Team, helped Houston Methodist prepare a strong plan of attack during the first wave of COVID-19. Along with the tireless efforts of clinical and nonclinical staff, we were able to face this challenge and the subsequent surge as a high-performance organization.
Training Resources
California Incident Command Certification System: https://firescope.caloes.ca.gov/training.
FEMA Emergency Management Institute: https://training.fema.gov/nims/.
Hospital Incident Command System: https://emsa.ca.gov/disaster-medical-services-division-hospital-incident-command-system/.
Glossary
Abbreviations
- ICS
Incident Command System
- NIMS
National Incident Management System
- PPE
personal protective equipment
- ICU
intensive care unit
References
- 1. Firescope California https://firescope.caloes.ca.gov/. Accessed August 7, 2020.
- 2. Phibbs WM, Snawder MA. Embracing the Incident Command System: above and beyond theory. 2014. https://leb.fbi.gov/articles/featured-articles/embracing-the-incident-command-system-above-and-beyond-theory. Federal Bureau of Investigation Law Enforcement Bulletin, U.S. Department of Justice. Published November 2014. Accessed August 7, 2020. [Google Scholar]
- 3. Chang R. A literature review and analysis of the Incident Command System. International Journal of Emergency Management. 2017;13(1):50. [Google Scholar]
- 4. Parish J. The seven principles of the Incident Command System. https://www.academia.edu/33163436/The_Seven_Principles_of_the_Incident_Command_System. Accessed August 7, 2020. [Google Scholar]
- 5. Federal Emergency Management Agency. ICS review document—extracted from E/L/G 0300 Intermediate Incident Command System for Expanding Incidents, ICS 300. https://training.fema.gov/emiweb/is/icsresource/assets/ics%20review%20document.pdf. Published March 2018. Accessed August 7, 2020. [Google Scholar]
- 6. Holshue ML, DeBolt C, Lindquist S, et al. ; Washington State 2019-nCoV Case Investigation Team First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ackerman T, Gill J, Lewis B. Fort Bend coronavirus case is first in Houston area. Houston Chronicle, March 4, 2020. https://www.chron.com/news/houston-texas/houston/article/Coronavirus-case-diagnosed-in-Fort-Bend-health-15106151.php. Accessed August 7, 2020. [Google Scholar]
- 8. Marshall B. Houston-area city, county officials recommend cancellation of large gatherings, using telecommuting to prevent coronavirus spread. Community Impact Newspaper, March 12, 2020; https://communityimpact.com/houston/sugar-land-missouri-city/government/2020/03/12/houston-area-city-county-officials-recommend-cancellation-of-large-gatherings-using-telecommuting-to-prevent-coronavirus-spread/. Accessed August 7, 2020. [Google Scholar]