Abstract
Many major cities that witnessed heavy air pollution by nitrogen dioxide (NO2) and particulate matter (PM) have experienced a high rate of infection and severity of the coronavirus disease pandemic (COVID-19). This phenomenon could be explained by the overexpression of the angiotensin converting enzyme 2 (ACE-2) on epithelial cell surfaces of the respiratory tract. Indeed, ACE-2 is a receptor for coronaviruses including the severe acute respiratory syndrome coronavirus 1 and 2 (SARS-CoV), and ACE-2 is overexpressed under chronic exposure to air pollution such as NO2 and PM2.5. In this review, we explain that ACE-2 acts as the sole receptor for the attachment of the SARS-CoV-2 via its spike protein. The fact that respiratory and vascular epithelial cells express ACE-2 has been previously observed during the 2003 epidemic of the SARS-CoV-1 in China, and during the 2012 Middle East respiratory syndrome in Saudi Arabia. High ACE-2 expression in respiratory epithelial cells under air pollution explains the positive correlation between the severity in COVID-19 patients and elevated air pollution, notably high NO2 and PM2.5 levels. Specific areas in India, China, Italy, Russia, Chile and Qatar that experience heavy air pollution also show high rates of COVID-19 infection and severity. Overall, we demonstrate a link between NO2 emissions, PM2.5 levels, ACE-2 expression and COVID-19 infection severity. Therefore, air pollution should be reduced in places where confirmed cases of COVID-19 are unexpectedly high.
Keywords: Air pollution, Angiotensin converting enzyme 2 expression, COVID-19 severity, environmental intervention, NO2 emissions, Particulate matters 2.5
Introduction
The world is facing challenges of an outbreak of the disease called coronavirus disease (COVID-19) caused by a mutated strain of pre-existing coronaviruses. The World Health Organization (WHO) has named this virus ‘severe acute respiratory syndrome coronavirus-2′ (SARS-CoV-2). The COVID-19 has been documented to be widespread covering almost all geographic areas irrespective of human race and climatic condition (Chafekar and Fielding 2018). Exceptionally, it affected all aspects of society and a very high proportion of the world population as compared to any such previous infectious diseases has been infected (Das et al 2020a, b; She et al. 2020; Shereena et al. 2020).
The SARS-CoV-2 is a highly infectious strain and studies indicate that it is a mutated form of the previously existing coronaviruses namely Severe Acute Respiratory Syndrome-1 (SARS-CoV-1) and Middle East respiratory syndrome coronavirus (MERS-CoV). Both the pre-existing coronaviruses, i.e. SARS-CoV-1 and MERS-CoV made endemic and epidemic in China in 2003 and in the Middle East especially in Saudi Arabia (was the epicentre) in 2012 (Chafekar and Fielding 2018; BBC 2020; CDC 2020, FDA 2020; WHO 2020a, b, c, d, e, f, g; Yao et al. 2020), respectively. SARS-CoV-2 has 50 and 79% similar nucleotide sequence with that of the genome sequence of SARS-CoV-1 and MERS-CoV, respectively (Andersen et al. 2020). According to the WHO chief scientist, the SARS-CoV-2 genome does not contain any genetic marker that is used during genetic engineering (Ramesh 2020). It proves the fact that SARS-CoV-2 is a natural strain of the coronavirus family (Paital 2020).
SARS had its epicentre in China, with death toll of 774, and the MERS had its epicentre mostly in Saudi Arabia, as this country alone experienced 1,807 infections and 705 deaths, with total infection of 2182 out of which 779 have died in the affected 27 countries (BBC 2020; Guo et al. 2020; Habibzadeh and Stoneman 2020; She et al. 2020; Shereen et al. 2020). However, all previous records by coronaviruses were broken by the present COVID-19 outbreak because, as per rolling data as on 29th August 2020, it has infected 24, 587, 513 individuals, out of which, 833, 556 from 216 countries have lost their live in the disease (WHO 2020e). The fatality rate—all infected to death cases—by MERS was high (35.7%) as compared COVID-19 (6.89% in June 2020 and 3.39% in last week of August 2020), and this is the less panicking message for us in relation to SARS-CoV-2 (WHO 2020e). On the other hand, no specific vaccine or medicine is available publicly against COVID-19, although many vaccines are declared to be in the pipe line (Saurabh et al. 2020). As a result, countries such as the USA, Italy, Russia, Germany, Spain, France and Brazil who offer the most advanced clinical care to their citizens, top the list among the most affected countries (WHO a, b, c). Mostly American and European countries are mostly affected next to Asian countries (Fig. 1).
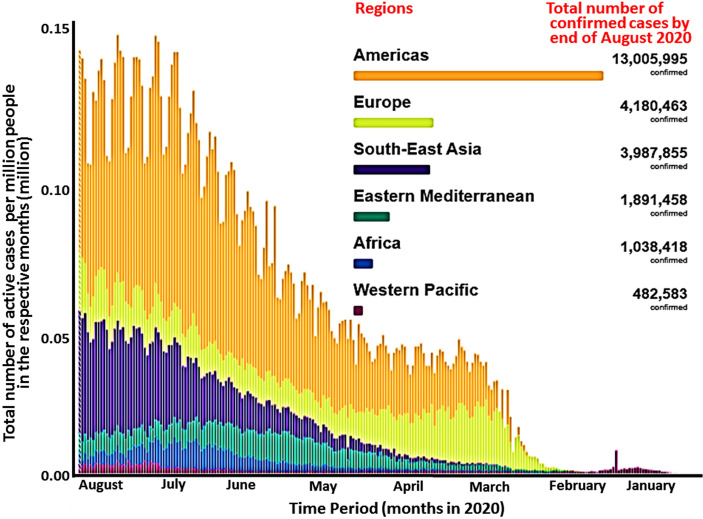
Fig. 1.
Current global status of COVID-19 outbreak by end of August 2020. As per the latest data obtained from the world health organization zonation up to the end of August 2020, the total numbers of confirmed COVID-19 cases per million people are higher in American countries followed by the European and Asian countries (total number indicated in insert). However, the outbreak has affected 2016 countries as of August 2020 (Source WHO 2020b under creative common attribution)
The COVID-19 disease had positive effects on the self-regeneration process of nature. Air, water and noise pollution were reduced in many parts of the planet because of the stationary activity of humans (Wang et al. 2020a). Humans are now off the street and self-locked inside home to avoid SARS-CoV-2 infection (Paital et al. 2020a, b). Wild-life and biodiversity now are expanding in a never seen manner. However, in some places in countries such as India, China, Italy and USA, a positive correlation is observed between the existing level of the higher air pollution and severity/death rate under COVID-19 infection. This is one of the important issues in relation to control COVID-19 severity and environmental intervention is suggested at such places where both air pollution and COVID-19 made their common hot spots (Domingo and Rovira 2020; Woon and Sun 2020).
Environmental factors may explain partly the behaviour and fate of COVID-19 (Sharma et al. 2020; Sun and Han 2020). For instance, air pollution by aerosols in public toilets increase the risk of infection, in particular for infants and lactating mothers (Wang et al 2020b). Air pollution acts as the causative agent for diseases such as bronchitis, asthma and many other respiratory diseases. The SARS-CoV-2 has chosen respiratory tracts as its primary attacking organs because of the predominant expression of the angiotensin-converting enzyme-2 (ACE-2) in their epithelial cells. The protein ACE-2 acts as the receptor for the attachment of the SARS-CoV-2 spike protein “S” and hence increases the chance of infection as well as severity of the disease in humans. COVID-19 is known for its fatal activity by causing respiratory choke and therefore, causes mainly respiratory disorders and common cold associated symptoms. Therefore, it is observed that COVID-19 and air pollution have intricate relations with each other. On one hand, polluted air can create many breathing issues in humans leading to easy ways for the virus to enter and infect, and, on the other hand, NO2 and particulate matter (PMs), especially particulate matter 2.5 (PM2.5), can be responsible for the over-expression of ACE-2 in human respiratory cells for the viral attachment.
Aerosols can carry the viruses and they can live in aerosols up to 3 h. So, SARS-CoV-2 is acknowledged to be responsible to infect healthy people via aerosols (van Doremalen et al. 2020; WHO 2020h). This explains that COVID-19 can be transmitted and increase the severity via air pollution. In some areas, the indoor air quality is also not up to level for breathing as it crosses the limit set by many international organizations including WHO. Therefore, extra care and precaution is suggested in such areas to prevent the severity of the disease (Wang et al. 2020b). Taking above facts into consideration, we try to review and decipher the mechanisms of high air pollution with high risk of COVID-19 infection or severity of the disease via the over-expression of ACE-2. We found three routes in which air pollution and COVID-19 are associated with each other: (1) induction of respiratory diseases by both COVID-19 and air pollution especially via NO2 emissions in general, (2) PM2.5 mediated ACE-2 up-regulation, and (3) NO2 mediated high expression of ACE-2 in respiratory cells of human hosts.
Rolling data on 29 August 2020 indicate that in PubMed, total 11 articles on COVID-19 in relation to environmental interventions especially in regulating air pollution are available. Particularly, articles written on term “COVID-19, NO2, PM2.5 and ACE-2” within the last 6 months are almost nil although 47,935 articles are published on “Coronavirus” (Fig. 2). Therefore, in this article, we attempt to correlate the COVID-19 pandemic with air pollution, especially with the increase in severity in COVID-19 patients. Specifically, we try to draw the correlation among COVID-19 infection/severity, NO2 emission and PM2.5 level and ACE-2 expression level (Fig. 2).
Fig. 2.
Number of articles published in PubMed on COVID-19 in relation to environment and ACE-2 expression. Although articles as on 29.08.2020 on coronavirus is although approaching 0.05 million, environmental intervention related articles are very few. Especially, articles on Angiotensin Converting Enzyme 2 (ACE-2) expression that acts as the receptor for the coronaviruses, in relation to air pollution more particularly on the contribution of NO2 emission and PM2.5. level for COVID-19 infection is scanty. The term mentioned in “X” axis were searched in PubMed as on 29.08.2020. It indicates the gap on research on COVID-19, ACE-2 expression under high NO2 emission and PM2.5 dominated areas
COVID-19 severity under high air pollution
The current status of air pollution especially NO2 emission and safety limits are presented in Fig. 3 and Tables 1 and 2. The intricate relations among air pollution, PMs and human health including cardiovascular, respiratory and associated diseases are systematically discussed in many recent articles and reputed forums (Kim et al. 2015; Tositti et al. 2018; Thompson 2018; WHO 2020f). Specific example of NO2-associated health risks are COPD, multiple ischaemic heart disease, chronic cardiopulmonary diseases in elderly, atopic diseases, nerve disorders, dementia, chronic kidney disease, childhood leukaemia, and multiple organ dysfunction, hypertension like health disorders (Filippini et al. 2015; Krauskopf et al. 2018; Hassoun et al. 2019).
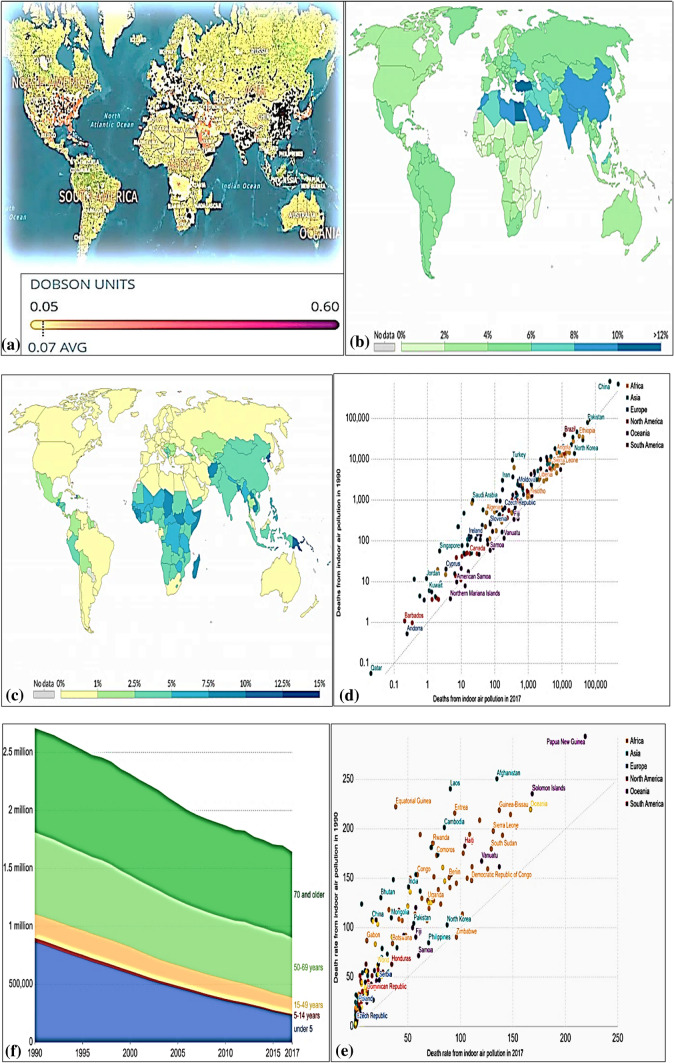
Fig. 3.
Status of air pollution mediated death in world. a Footage given by the European Space Agency indicates that Nitrogen Dioxide (NO2) pollution is predominant in the global troposphere, i.e. the lowest (and largest) layer of the Earth’s atmosphere that ranges from ground level to 10 km upwards. The darker or pinker cloud indicates the higher level of NO2 (Dobson units) in an area. The black dots shows the highly NO2 polluted area. Data are generated by the new Sentinel 5P satellite of the European Space Agency from an average values measured daily for 90 days, i.e. from June to August 2018 (Source Chow 2020; Environmental Protection Agency, 2020, Myllyvirta and Howard 2020). b Colour intensity showing global death rate by air pollution. Percentage shows the death rate by air pollution as compared to other diseases (Source Institute for Health Metrics and Evaluation 2020), c Indoor and outdoor air pollution mediated death in world. A colour intensity of air pollution showing global death rate by indoor air pollution. Percentage shows the death rate by indoor air pollution as compared to other diseases, d Number of deaths by indoor air pollution in 1990 versus 2017, e Indoor air pollution death as a function of age. Old age people above 69 year are more prone for indoor air pollution risk, f Indoor air pollution rate per 100,000 people in 1990 versus 2017 in country wise distribution. Raising indoor air pollution makes a concern globally (Source Institute for Health Metrics and Evaluation 2020 under creative common license attribution)
Table 1.
Safe levels of air pollutants according to the World Health Organization (WHO)
| Pollutants | Annual mean | 24-h mean | 8-h mean | 1-h mean | 10-min mean |
|---|---|---|---|---|---|
| PM2.5 | 10 μg/m3 | 25 μg/m3 | – | – | – |
| PM10 | 20 μg/m3 | 50 μg/m3 | – | – | – |
| Ozone (O3) | – | – | 100 μg/m3 | – | – |
| NO2 | 40 μg/m3 | – | – | 200 μg/m3 | |
| SO2 | – | 20 μg/m3 | – | – | 500 μg/m3 |
Above values are recommended to be safe by scientific experiments conducted by WHO. The above values are applied to ambient outdoor air (Source WHO 2020i)
Table 2.
Standard air quality index (AQI)
| Daily AQI colour | Levels of concern | Values of index | Description of air quality |
|---|---|---|---|
| Green | Good | 0 to 50 | Air quality is satisfactory, and air pollution poses little or no risk |
| Yellow | Moderate | 51 to 100 | Air quality is acceptable. However, there may be a risk for some people, particularly those who are unusually sensitive to air pollution |
| Orange | Unhealthy for sensitive groups | 101 to 150 | Members of sensitive groups may experience health effects. The general public is less likely to be affected |
| Red | Unhealthy | 151 to 200 | Some members of the general public may experience health effects; members of sensitive groups may experience more serious health effects |
| Purple | Very unhealthy | 201 to 300 | Health alert: The risk of health effects is increased for everyone |
| Maroon | Hazardous | 301 and higher | Health warning of emergency conditions: everyone is more likely to be affected |
The AQI is divided into six categories and are given with a different level of health concern. Each category has also been assigned to a universal colour mark as stated in the table and it makes it easy for people to quickly determine whether air quality is reaching unhealthy levels in their communities. AQI near 100 is usually considered as safe (Source USA AQI 2020)
Coronavirus infection and air pollution found to have interdependent relations with each other during COVID-19 periods across the world (Bashir et al. 2020). In many places, COVID-19-induced lockdowns had a positive impact on reducing air pollution (Paital 2020; Paital et al. 2020a), whereas in places where air pollution is high and are above the limits (Tables 1 and 2) are found to experience very negative impacts. Because such places are documented with an enhanced rate of both infection and severity in COVID-19 patients as compared to least polluted areas (Bashir et al. 2020, 2020).
Air pollution and COVID-19 severity
Air pollution acts as one of the major risks for causing many diseases and death, and it attributes to ~ 9% of deaths globally. Air pollution also acts as the route for much other secondary diseases and associated deaths (Walker 2020). Lower COVID-19 mortality in forested areas reinforces the influence of air pollution and suggests immunoprotection by Mediterranean plants (Roviello and Roviello 2020). Death rates under air pollution-related diseases and associated complications are at least 100-folds more in poor countries in comparison to the countries with high income. It is because poor countries do not get clear fuel for consumption especially in households. It is estimated that about 4.2 and 3.8 million deaths per year are attributed to breathing polluted ambient air (outdoor air pollution) and household exposure to smoke from dirty fuel sources such as cooking stoves (indoor air pollution), respectively. It is very dangerously true that nine out of every ten persons in world are unable to breathe cleaner air as set by WHO (2020f, Table 1).
Air pollution induces many age-specific respiratory and cardiovascular associated diseases. Some of them are chronic obstructive pulmonary diseases, hypertension, respiratory allergies and many cardio-respiratory illnesses including thrombogenesis (Brauer 2010; Carlsten et al. 2011; Willyard 2020; Table 3). Mainly air pollution aggravates the above diseases that act as a cause for contracting other associated diseases such as heart attack, blood pressure and diabetes. Respiratory issues are mainly linked with NO2 emission. And, the atmospheric level of NO2 is considered as a marker gas for the health of the ecosystem (fewer emissions) in one hand and the industrial or massive vehicular activity (increased level) on the other hand. The latter case is positively correlated with morbidity and mortality of patients who suffer from various other diseases such as COVID-19 in the present case (Carugno et al. 2016; He et al. 2020a, b).
Table 3.
Risk of co-morbidity (diseases) under air pollution
| Health outcome | Evidence | Population | Relative risk | Relative risk* | Proof |
|---|---|---|---|---|---|
| Acute infections in LST | Strong | Children aged 0–4 years | 2.3 | 1.9–2.7 | SE |
| Chronic OPD | Strong | Women aged ≥ 30 years | 3.2 | 2.3–4.8 | SE |
| Moderate I | Men aged ≥ 30 years | 1.8 | 1.0–3.2 | SE | |
| Lung cancer (coal) | Strong | Women aged ≥ 30 years | 1.9 | 1.1–3.5 | SE |
| Moderate I | Men aged ≥ 30 years | 1.5 | 1.0–2.5 | SE | |
| Lung cancer (biomass) | Moderate II | Women aged ≥ 30 years | 1.5 | 1.0–2.1 | ISE |
| Asthma | Moderate II | Children aged 5–14 years | 1.6 | 1.0–2.5 | ISE |
| Moderate II | Adults aged ≥ 15 years | 1.2 | 1.0–1.5 | ISE | |
| Cataracts | Moderate II | Adults aged ≥ 15 years | 1.3 | 1.0–1.7 | ISE |
| Tuberculosis | Moderate II | Adults aged ≥ 15 years | 1.5 | 1.0–2.4 | ISE |
Air pollution is considered to cause many deaths mainly due to causing respiratory disorders (Brauer 2010). As per a study done by WHO, breathing poor quality air alone contributes to the death of 4.6 million people annually (Cohen et al. 2017). Even it was estimated that poor air quality imposed deaths are more than the death accounted for road accidents each year (European Environment Agency 2005). Breathing impure air is a universal air pollution issue and in 2102, PMs have caused 193,000 deaths alone in European countries (Ortiz et al. 2017). For example, under severe air pollution in China in 2016 was responsible to increase the risk of 4,000 preventable deaths daily and finally it contributes to 1.6 million documented and un-documented mortalities (Rohde and Muller 2015; Wang et al. 2012).
Massive steps are taken to have a grip on the rapidly increasing air pollution, albeit results obtained are not satisfactory. Countries such as UK alone experience 40,000 excess deaths each year under air pollution (Liu et al. 2020). Therefore, identifying the toxic element level in the air and their control has created an emergency not only in UK but also in many other counties such as China (Liu et al. 2020), Italy, India and Qatar. Each year air pollution causes millions of premature deaths largely associated with co-morbidities including Chronic Obstructive Pulmonary Diseases (COPDs), brain and heart stroke, neural diseases, faster ageing, skin diseases, lung cancer and many acute respiratory infections (Carugno et al. 2016; Gori et al. 2020; Table 3).
Air pollution can increase the chances of COVID-19 outbreak via comorbidities or by increasing the chance of other respiratory illness (Dutheil et al. 2020a; Table 3). In China, air pollution is considered a risk factor for several respiratory infections as they carry microorganisms and create immuno-deficiency. Significant positive association was observed between air pollutants, such as PM2.5, PM10, NO2, CO2, SO2, CO and O3, and the current pandemic in China (Zhou et al. 2020; Zhu et al. 2020b). The above authors have found that COVID-19 confirmed cases are positively correlated with the level of air pollution. They have noticed that about 10 μgm−3 increases in PM2.5 and PM10 and other air pollution gases such as O2, and O3 was associated with a significant 2.24%, 1.76%, 6.94%, and 4.76% increase in daily COVID-19 positive cases in China. In contrast, a 10 μgm−3 increase in SO2 level was negatively correlated with a 7.79% decrease in COVID-19 positive patients (Zhu et al. 2020b). Therefore, specific precautions are advised to be taken under high air (especially NO2) polluted areas. Indoor air pollution, e.g. by aerosols of laser printers, is also likely to increase risks of contaminations (He and Han 2020). A long-term exposure to air pollutants may act as one of the major contributor to fatality caused by the COVID-19.
Supporting to the above fact, it was calculated that in Italy, Spain, France and Germany, out of 4443 fatality observed at the beginning of the pandemic, 3487 deaths contributing 78% of the total death were confined to cases where NO2 pollution was predominant (Ogen 2020). From a case study in Northern Italy, it was confirmed that air pollution can be the sole factor for the observing high rate of infection and severity in COVID-19 patients (Conticini et al. 2020). More particularly, similar suspected environmental persistence of SARS-CoV-2 via air pollution is proposed in the Po Valley of Northern Italy (2020). Since regional air pollution persistence is highly linked to COVID-19 severity, it can be considered as a putative disease risk factor (Martelletti and Martelletti 2020). Therefore, zonation may be done in such areas to employ specific management or preventative measures for COVID-19 (Frontera et al. 2020a, b) and special measures to be taken where NO2 emissions are very high.
Ecological health studies in China in 2003 during the SARS epidemic indicate that air pollution has a confirmed relation with the coronavirus (SARS-CoV-1) epidemic (Li et al. 2017, 2018, 2020). The author had analysed 100 SARS cases in 5 zones where the fatality rate under SARS was the highest in China. In the regions were having high air pollution index, the authors calculated the case fatality under SARS and number was estimated as a function of air pollution index. The number was calculated as—0.063 + 0.001 *air pollution index. Surprisingly, 84% increased risk of infection and severity was noticed in patients that were exposed to polluted air as compared to patients documented in least polluted areas. Similarly, the death rate in such patients was double (at 95% confidence level) in air polluted areas as compared to the unpolluted areas. Long term exposure to air pollutants such as NO2, CO, CO2, SO2, PMs and ground level O3 were predicted to be responsible for the negative effects on SARS and COVID-19 patients (Li et al. 2017, 2018, 2020). Data indicate that an increase of 10 mgm−3 of PM2.5 can increase 0.38% higher mortality in air polluted areas.
The author also proposed the possible mechanism of air pollution induced co-morbidities via generating reactive oxygen and nitrogen species and oxidative stress, mitochondrial dysfunction, metabolic reprogramming, apoptosis, necrosis, cell proliferation especially in smooth muscles, neutrophil infiltration, inflammation, genetic susceptibility to many diseases, inhibition of the formation of dendritic cells, large scale response of innate immuno-allergic responding cells such as mast cells, eosinophil, fibroblasts and damage in epithelium layer in respiratory tracts. Molecular mechanisms involved in regulating above processes are modulation of extracellular-signal-regulated kinase (called as ERK)/protein kinase B (called as AKT)/ 5′ adenosine monophosphate -activated protein kinase (called as AMPK)/ signal transducer and activator of transcription 1 (called as STAT-1) signalling system, high abnormal nitrogen oxide synthase activity, abnormal cytokine secretion, disturbed Ca+ signalling that leads to abnormal microRNA expression and finally the worsen physiology by modulating above processes which lead to asthma and chronic obstructive pulmonary diseases like chronic respiratory diseases (Mishra et al. 2019; Li et al. 2017, 2018, 2020).
In many case studies, NO2 was considered as one of the principal attributing factors for creating major health risks. In a 5-day long case study, it was predicted that death under additional NO2 (at 10 μg m−3) mediated air pollution is increased to 2% as compared to a 0.13% escalation of daily all-cause deaths (Chiusolo et al. 2011; Hoek et al. 2013; He et al. 2020a, b). Therefore, NO2 is responsible to increase a global hazard ratio of 1.052 per increase of 8.1 ppb in its concentration in air (Crouse et al. 2015; Dutheil et al. 2020a, b). It was noticed that reduction in NO2 emissions in China is predicted to be associated with a 6% reduction in mortality under the current scenario of COVID-19 outbreak. It counts that ~ 100,000 lives are saved in China only due to reduction of NO2 emission under COVID-19-induced lockdown.
Similar scenarios need to be calculated for other countries. However, it is summarised that air pollution especially PMs and NO2 emissions have a strong correlation with generating respiratory disorders in humans. Therefore, logically, COVID-19 must have a specific relation with air pollution, and it is analysed to be true in several case studies, in China, being the recent one (Fig. 4, Dutheil et al. 2020a, b). This could be true because both produce respiratory associated diseases. As described earlier, clear events of death under air pollution are chronic obstructive pulmonary diseases, respiratory allergies including asthma and bronchitis and other cardio-vascular diseases but not limited to these (Brauer 2010; Carugno et al. 2016) and COVID-19 symptoms are related to respiratory choke. Elaborating the specific relation between air pollution and COVID-19 severity will make the above fact clearer.
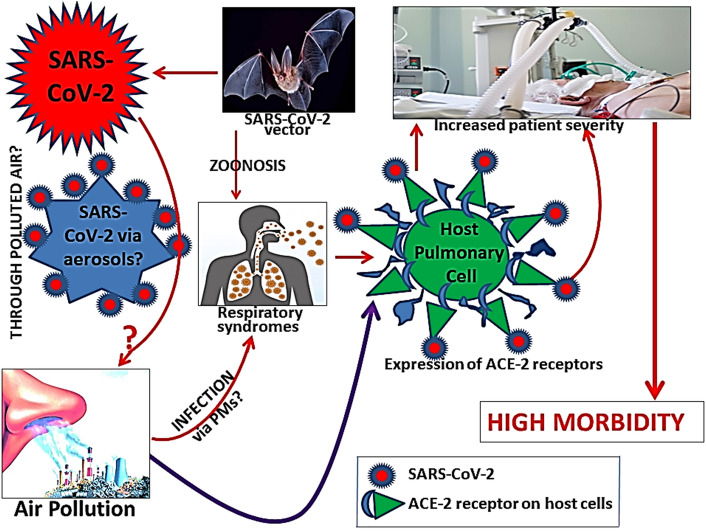
Fig.4.
General module of the viral infection. The severity of the viral disease leading to the high rate of death is believed to be increased under high air pollution in general. ACE-2- Angiotensin converting Enzyme 2, SARS-CoV-2—Severe Acute Respiratory Syndrome Coronavirus-2
Relation among PM2.5 mediated ACE-2 expression and COVID-19
Particulate matters are “a complex mixture of extremely small particles and liquid droplets, made up of acids, organic chemicals, metals, and soil or dust particles” (Li et al. 2018). A very recent study in the United States indicates that an elevation of only 1 μg m−3 in PM2.5 is associated with a rise in 8% COVID-19-induced death rate (Wu et al. 2020a, b, c). The data was observed at 95% confidence level indicating a strong relation between PM2.5 and COVID-19 spreading and deaths. Therefore, the above authors have concluded that their results underscore the importance of continuing to enforce existing air pollution regulations to protect human health under COVID-19 pandemic (Wu et al. 2020a, b, c). Similar observations are also observed in cities of China, India, Britain, Italy, and the Netherlands etc. where PM2.5 levels are high (Cole et al. 2020; Travaglio et al. 2020).
Aerosols and their associated complications are worldwide phenomena that occur due to heavy atmospheric pollution (Fu et al. 2017). They make large concerns to human and animal health, cleaner air and air visibility, cloud condensation nuclei in air, and even to global climate change events (Li et al. 2017). Aerosol can be formed in the atmosphere from several sources including moisture, dust particles, smoke particles, and vapour. On the other hand, above particles are also considered as concerns in meteorological events and few of the main contributors for air pollution (Zhu et al. 2020a). Most of the aerosols found in the air are resulted from the anthropogenic activities that produced fine, very fine and ultra-fine particles. They are also produced following gas-to-particle conversion processes (Li et al. 2020; Wu et al. 2020a). If the quantity of aerosols increases to large quantities, it increases the level of air pollution. Aerosols such as SO2, oxides of nitrogen (NOX) and PM2.5 are unavoidably resourced due to high fossil fuel consumption to meet the rapid economic progress in many countries such as China (Chauhan and Singh 2020; Yan et al. 2015; Wu et al. 2020b).
On the other hand, aerosols have found to have a lot of health risks in human and non-human organisms. Aerosols produced from biological activities such as from several anthropological interventions, instrumental operations and other human activities. The nature and heterogeneous micro-composition of bio-aerosols depend on the source, activity and methodology used in the event. Even some bio-aerosols are found to contain air and water travelling micro-organisms such as viruses and bacteria. Experimental evidences using aerosol-generating procedures indicate that exposure to aerosols can create a risk of infections as they can carry pathogens. And, such incidents are seen that lightweight pathogens including SARS viruses can be carried to health care workers by aerosols and causes acute respiratory infections in them (Tran et al. 2012). It is reviewed that Legionella species, a pathogenic group of Gram-negative bacteria, can be isolated in bio-aerosol. It is noteworthy to mention that this bacterium can induce serious respiratory issues in old age people and people with early history of respiratory disorders (Zemouri et al. 2017).
As per a very recent study by Chin et al (2020), SARS-CoV-2 is non-specifically gets adsorbed or absorbed by surfaces. They can attach to any surface ranging from paper cardboard, plastic, coin, metals, clothes, any other aerosols etc. and the virulence of the virus can be maintained from a few hours to a few days on the above aerosol materials (Table 4). The authors have also stated that SARS-CoV-2 can withstand a wide pH (3–10) while attached to the surfaces, although temperature can deactivate them substantially. Summary of their statements indicates that SARS-CoV-2 in virus transport medium kept for 14 days can retain its virulent capacity. They found that the virus is heat labile although it is stable at 4 °C. At 4 °C, the virus loses its virulent capacity by 0.7 log-unit after 14 days. However, when it is heated up to 70 °C, the above 14 days time limit is declined to 5 min (Chin et al. 2020). Although aerosols (from infected patients) can act as cargo for the tiny SARS-CoV-2 viruses is established, no specific study has been done whether they can infect healthy humans via PMs but logically it is accepted that PMs can carry them on their surfaces due to their non-specificity.
Table 4.
Stability of SARS-CoV-2 and SARS-CoV-1 in aerosols and other materials surfaces
| Types of material | SARS-CoV-2 | SARS-CoV-1 | ||
|---|---|---|---|---|
| Stability | Reduction in infectious titre (from to) | Stability | Reduction in infectious titre (from to) | |
| Aerosol | h | 103.5 to 102.7 TCID50 per litre of air | 3 h | 104.3 to 103.5 TCID50 per millilitre |
| Plastic | 72 h | 103.7 to 100.6 TCID50 per millilitre of medium | 72 h | 103.4 to 100.7 TCID50 per millilitre |
| Stainless steel | 48 h | 103.7 to 100.6 TCID50 per millilitre | 48 h | 103.6 to 100.6 TCID50 per millilitre |
| Cardboard | 24 h | – | 8 h | –- |
| Copper | 4 h | – | 8 h | – |
Tissue-culture infectious dose (TCID) 50–50% tissue-culture infectious dose, h-hours, SARS-CoV—Severe Acute Respiratory Syndrome Coronavirus
Source: van Doremalen et al. (2020) under common creative license attribute
A recent experiment done by van Doremalen et al (2020) has shown that SARS-CoV-2 is viable in aerosols. The authors have used the titre of aerosolized viable virus. The unit of activity of the virus was expressed as 50% tissue-culture infectious dose (TCID50) per litre of air. Employing a Bayesian regression model, the authors had examined the stable activity of both SARS-CoV-1 and SARS-CoV-2 viral strains in aerosols. Also, the authors had evaluated stability of the above two viral strains on several solid surfaces to monitor their rates of decay (Table 4). The author has generated aerosols of aerodynamic diameter < 5 μm containing SARS-CoV-2 (105.25 50% TCID50 per mL) and SARS-CoV-2 (106.75–7.00 TCID50 per mL) with the help of a three-jet Collison nebulizer fed into a Goldberg drum. This setting was done to mimic an aerosolized atmosphere. The viral inoculum resulted from the experiment were also exposed to the cycle-threshold values ranging from 20 and 22 which are similar when the virus sample collected from the upper and lower respiratory tracts of humans, respectively. It was noticed that both the viral SARS-CoV-2 was quite active up to 3 h of experimental duration, although their virulent capacity were reduced averagely to 102.10 TCID50 per litre of air and the value for SARS-CoV-1 was 103.9 TCID50 per millilitre (van Doremalen et al. 2020).
It was concluded from the above study that both the above viral strains of coronaviruses follow a constant decay curve in aerosols with median estimates of air pollution proximately 1.1 to 1.2 h and 95% credible intervals of 0.64 to 2.64 for SARS-CoV-2 and 0.78 to 2.43 for SARS-CoV-1 (van Doremalen et al. 2020). Such experimental data was the preliminary evidence to accept the fact that SARS-CoV-2 transmission can be done via air. PM2.5-induced enhanced mortality rate in COVID-19 patients in Lodi, Cremona, Bergamo and Brescia cities of Italy is very well-established and it provides additional supporting data on air transmission of SARS-CoV-2 (Frontera et al. 2020a, b). These authors have reported it as a “double hit hypothesis” because both NO2 and PM2.5 are described as responsible for increasing the severity in respiratory and associated other diseases and COVID-19 in Italy. Similar study done in mice model indicates that PM2.5 chronic exposure is highly responsible for upregulate angiotensin converting enzyme expression (Aztatzi-Aguilar et al. 2015; Lin et al. 2018). Therefore, the authors had concluded that patients who breathe polluted air that exceeds the normal limit of PM2.5 are at the higher risk of experiencing the severity of COVID-19 once they get infected.
A meta-analysis in 50 most polluted capital cities in the world indicates that the PM2.5 along with other air pollutants have caused 25, 29 and 43% of total deaths under ischemic heart diseases, lung cancer and COPD, respectively (Meteosim 2020). The capital of India (Delhi), Bangladesh (Dhaka), Afghanistan (Kabul), Bahrain (Manama), Mongolia (Ulaanbaatar), Kuwait (Kuwait city), Nepal (Kathmandu) and China (Beijing), UAE (Abu Dhabi), Indonesia (Jakarta), Uganda (Kampala) and Vietnam (Hanoi) have topped the list having annual average PM2.5 level of 1135, 971, 618, 598, 585, 563, 544, 509, 488, 408, And 408 µg m−3, respectively. And the severity of COVID-19 in all those areas in Asia, America, Europe and Africa is usually high as compared to the least polluted countries (Rodríguez-Urrego and Rodríguez-Urrego 2020). This could be one of the contributing factors for India in securing the third highest position in COVID-19 infection rate currently because it has many most polluted cities (Govt. of India 2020).
One recent analysis in Italy has found that besides concentrations of aerosols and viral load, the chronicity in COVID-19 patients under aerosols exposure follows a positive association for severity and infection rate. Area that are experiencing high aerosols and emissions of gases including NO2, CO2, O3, SO2, PM2.5 and PM10 in 71 provinces in Northern Italy particularly in Lombardy were documented with a higher rate of infection and severity in COVID-19 cases (Sarmadi et al. 2020). The authors were with a strong perception that chronic exposure to high air pollution makes a favourable condition for the easy spreading and imposing severity in COVID-19 cases. Although the authors had noticed PM-induced high pro-inflammatory responses in COVID-19 cases, incidence of high respiratory and cardiac arrest were not established from their data (Fattorini and Regoli 2020). An increase in sample size possibly could reverse their later assumption in the favour of high risk respiratory and cardiac issues in COVID-19 patients under high PM exposure condition.
In one hand, the risk of transmission of SARS-CoV-2 via aerosols is established, and on the other hand, aerosol-induced respiratory and other diseases that facilitate the virus to infect or increase the morbidity or severity in the patients have already been observed in many places at Italy, China, India and USA (Paital 2020; Sarmadi et al. 2020). Therefore, a second correlation between air pollution and COVID-19 could be via aerosol-induced complications. Thus, a long term environmental intervention against air pollution and other pollutions are suggested to combat COVID-19 like chronic health risks because a short term air pollution approach may eradicate such endemic, or pandemics for the timing would not help in coming decades (Fattorini and Regoli 2020). Since future outbreak of such pandemics cannot be ruled out, therefore, control of pollutions especially air pollution is highly suggested.
NO2 mediated ACE-2 up-regulation
As discussed previously NO2 is a major health risk factor and causes many diseases such as Chronic Obstructive Pulmonary Disease (COPD), multiple ischaemic heart disease, chronic cardiopulmonary diseases in elderly, atopic diseases and nerve disorders. Even clinical complications may led to conditions of dementia, chronic kidney diseases, childhood leukaemia, and multiple organ dysfunction, hypertension like health disorders (Filippini et al. 2015; Krauskopf et al. 2018; Hassoun et al. 2019). It is noteworthy to mention that co-morbidities especially with respiratory dysfunctions and COPD have a positive correlation with COVID-19 severity and death. Therefore, air pollution has its first-hand correlation with COVID-19 or vice versa via NO2 emission.
For example, as on 30.08.2020 in India, high air polluted states such as New Delhi (Delhi Municipality area, highly polluted), Gujarat (Industrially highly active and polluted), Maharashtra (Mumbai, highly polluted), Tamil Nadu (Chennai, highly polluted), Madhya Pradesh (Industrially active), Uttar Pradesh (Lucknow, Industrially active and highly polluted), West Bengal (Kolkata) and Telengana (Hyderabad), have comparatively high number of COVID-19 positive/death cases (171,366/4,404, 93,734/2,989, 764,281/2,4103, 415,590/7,137, 60,875/1,345, 219,457/3,356, 219,457/3,126, and 123,090/818, respectively) as compared to the less air polluted states such as Arunachal Pradesh, Dadra Nagar Haveli, Himachal Pradesh, Manipur, Mizoram, Sikkim and Nagaland (having number of COVID-19 positive/ death 3,877/05, 2,306/02, 5,781/34, 5,960/28, 1,008/00, 3,851/09, respectively) (Govt. of India 2020). It clearly indicates that air pollution has an intricate relation with COVID-19 and therefore, probably environmental approaches (to combat air pollution) also required for controlling COVID-19 along with clinical approaches. Thus, countries suffering from such pollution need to rethink to check their air pollution status for a combinatorial medico-environmental intervention plan for COVID-19 management (Woon and Sun 2020).
A very recent study by Ogen (2020) in cities of France, Germany, Italy and Spain indicates that a strong and positive correlation exists between NO2 emissions and COVID-19 deaths (Ogen 2020; Fig. 5). For example, out of the top five regions that encountered a very high mortality rate under COVID-19 in Italy, four of them were found in northern Italy. They are the places such as Lombardia Emilia-Romanga, Piemonte and Veneto of northern Italy that have witnessed 2168, 531, 175 and 115 death cases, respectively under COVID-19 which was higher as comapred to the low air polluted area during the study. Similarly in ‘Community of Madrid’ (Comunidad de Madrid) of Spain (covered with mountains like Po valley of Italy which encountered high air pollution and high infection and death under COVID-19), 498 death cases were noticed and all above places are recorded with very high level of NO2 emissions (Ogen 2020). The author stated that about 78% of all COVID-19-induced fatalities in above regions have high NO2 emissions levels ranging between 177.1 and 293.7 μmol m−2. The author noticed that out of 4443 fatalities noticed under COVID-19 by March 19, 2020 in above countries, 3701 (83%), 691(15.5%), 51 (1.5%) deaths occurred in places where NO2 emissions were 100, 50 to 100 and within 50 μmol m−2, respectively (Ogen 2020). It clearly indicates the strong positive correlation that exists between NO2 emissions and COVID-19 deaths.
Fig. 5.
Effects of NO2 level in COVID-19 deaths in France, Germany, Italy and Spain. Figure (redrawn from Ogen (2020) with permission), indicating a strong positive correlation between NO2 emissions and COVID-19 deaths in four developed countries. The parentage of death is highly upregulated, i.e. up to 80% with increased in NO2 emissions
The Renin–Angiotensin–Aldosterone System is an important cascade of vasoactive peptides that coordinate crucial molecular events in human physiology (Patel et al. 1990). Both SARS-CoV-1 and SARS-CoV-2 interact with the Renin–Angiotensin–Aldosterone System through ACE-2, an enzyme that physiologically counters Renin–Angiotensin–Aldosterone System activation in one hand, and acts as a receptor for CoVs on the other hand (Vaduganathan et al. 2020). Therefore, the interaction between the coronaviruses especially the present SARS-CoV-2 and ACE-2 has been proposed to be targeted clinically for the control of COVID-19. So, use of Renin–Angiotensin–Aldosterone System inhibitors is proposed to alter ACE-2 expression, and finally it can lead to diminish the virulent capacity of SARS-CoV-2. Therefore, developing inhibitors of ACE-2 to target SARS-CoV-2 is also advocated for the control of COVID-19 (Vaduganathan et al. 2020). However, developing Renin–Angiotensin–Aldosterone System inhibitors to use it against COVID-19 is yet not successful because clinical science is still awaiting a direct promising medicine or vaccine against SARS, MERS endemics and the present pandemic COVID-19 (Khan 2020).
ACE-2 is an enzyme that consists of around 805-amino acids. The enzyme is found to be a captopril-insensitive carboxypeptidase and its N-terminal consists of 17-amino acids long signal peptide chain whereas, it’s C-terminal consists of an anchor peptide chain that helps to bind on the cell membrane (Tipnis et al. 2004; Alifano et al. 2020). ACE-2 catalyses the cleavage of both angiotensin-I and angiotensin -II into angiotensin 1 to 9 and angiotensin 1 to 7, respectively. The latter group of angiotensins, i.e. angiotensin-1 to 7 act as vasodilator, therefore, they are elegantly accepted in clinical science as ACE plays a key role in maintaining the systemic blood pressure (Zheng et al. 2020). Therefore, ACE-2 mediated increase in production of angiotensin 1 to 7 also increases the chance of hypertension. For this reason, the chance of death of COVID-19 patients having high blood pressure issues, as one of the co-morbidities, is high (Zaki et al. 2013; Gupta and Misra 2020). This is a well-established fact from the MERS epidemic time that coronavirus can infect and replicate faster in patients with comorbidities (Bourgonje et al. 2020; Musa 2020), especially high blood pressure issues (Zaki et al. 2013; Gupta and Misra 2020).
On the other hand, the expression profile of ACE-2 is found to be organ specific in humans. It is also well-established that the transcript and translational levels of ACE-2 are found to be the highest in lung alveolar cells and substantial expression also noticed in enterocytes, in endothelial cells of arteries and veins, and in the smooth muscle cells of arteries (Hamming et al. 2004). Therefore, contracting SARS-CoV-2 in an arterial and venous system cannot be ruled out for which cardiac system becomes the secondary target by the SARS-CoV-2 in humans, for example, the noticed high risk of thrombogenesis in COVID-19 patients (Willyard 2020).
Direct evidence indicates that mice show a higher risk of ACE mediated respiration disorders when exposed to the chronic 5 ppm of NO2 (Rose et al. 1988, 1989). And developments of such lung injury issues are lessened when the fact was tested in ACE knockout mice (Lin et al. 2018). It indicates the role of ACE to develop lung injuries in mouse. Hence, the SARS-CoV-2 targets respiratory epithelial cells as the primary organs and involvement of hypertension to increase the severity of the disease is clear through the above link, i.e. the virus also targets the cardiovascular system and associated diseases act as accelerating co-factors to increase the severity of the disease. So, the key molecule for the propagation of the disease is found to be the level of the expression of ACE-2 and this fact is well-known from the epidemic of SARS in China during 2003 (Hamming et al. 2004; Oudit et al. 2009; Glowacka et al. 2010), endemic of MERS in Saudi Arabia in 2012 (Ge et al. 2013; Song et al. 2018) and the present pandemic COVID-19 in 2020 (Leng et al. 2020; South et al. 2020; Sriram and Insel 2020). Hence, it is already known that although the cardiovascular systems are not the primary target of COVID-19, management of the cardiovascular disorders is also important in COVID-19 patients. It is because associated cardiovascular disorders and their management could successfully decrease the susceptibility of infection and/or severity of the clinical course in COVID-19 cases (Alifano et al. 2020).
Studies on the pandemic COVID-19 in China have opened many new mechanisms of the infection mode, rate, and possible cure plan for the disease. Many studies concentric to the severity of the disease indicate that the main biological action plan against the disease lies to target the expression or particularly to block ACE-2 N-terminal domain via suitable molecule. During the course of evolution on the studies regarding ACE-2 mediated drug development and effects of environmental factors on ACE-2 expression, it was noticed that the environmental role is clear for the control of ACE-2 expression in COVID-19 patients. Therefore, more studies are to be done on an environmental intervention predominantly on that of air pollution in general and NO2 mediated expression pattern of ACE-2 in particular for the control of COVID-19 (Alifano et al. 2020). It is because only one article is available on this aspect in PubMed as on 29.08.2020 (Fig. 2).
Various molecular mechanisms are put forth to explain the air pollution induced risk of fatality under COVID-19 outbreak. Many studies intricately explain the mechanism of medications involving administration of ACE-2 inhibitors that can prevent the action of the receptors for SARS-CoV-2. Age old studies using several animal models indicate that about 100-folds higher expression of ACE-2 is noticed under NO2 exposure that finally enhances angiotensin-II binding to its receptor (Meulenbelt et al. 1992). It is noteworthy to mention here that the up-regulation of ACE-2 is linked to the binding of angiotensin II with type-1 receptor, i.e. angiotensin-1-receptor. In human, angiotensin -II in cardiac fibroblasts found to upregulate both the transcripts and translational level of ACE-2 in a dose-dependent manner. This happens via different controlling molecule(s) that substantially responsible for biochemical intermingling with the regulatory responding sequences positioned at − 516/-481 in human ACE-2 gene (Kuan et al. 2011).
Recent results of a cross-sectional experiment done by Yang et al (2019) in China considering 15, 477 human samples indicate that exposure of 5.5 μg m−3 of NO2 is linked to a higher risk of cardiovascular diseases inducing high blood pressure (Yang et al. 2019). Coronaviruses have a long history of increasing the severity of disease as was observed in 2003 in the case of SARS-CoV-1 infection. Not only NO2, but also other air pollutants such as CO, SO2, PMs and ground-level O3 were positively correlated with the severity of SARS epidemic in China during 2003. The rate of fatality in the coronavirus-induced SARS in China was increased in the patients those were breathing polluted air, and a higher expression of ACE-2 was responsible for the case (Cui et al. 2003). Currently, the case of COVID-19 is also found to speed quickly with a high rate of severity in zones where NO2 emissions are exceeding the WHO limits (Table 2) and the cases of Po Valley of Northern Italy (Frontera et al. 2020a, b), New Delhi and Surat cities of India (Paital 2020), and many places from France, Germany, Brazil, even from USA have witnessed the fact (Paital et al. 2020a, b; Das and Paital 2020).
Therefore, it is concluded that severe air pollution can be responsible for the increase in the rate and severity of COVID-19 via the interference of NO2 mediated ACE-2 overexpression (Alifano et al. 2020). Overexpression of ACE-2 could increase the risk of getting attachment of the virus through its interface spike protein “S” into the host epithelial cells along the respiratory tracts. As a result, the virulence of the virus in terms of efficient infection could be increased in areas where air pollution is high. This could increase the risk of infection as well as facilitation of severity and death of COVID-19 patients. Probably, this could be the third correlation between air pollution and COVID-19 via air pollution mediated ACE-2 expression as comorbidities such as hypertension and other cardiovascular diseases under NO2 exposure can increase the chance of enhancing the severity of COVID-19.
Overall aspects on the correlation between COVID-19 and air pollution
Lockdowns under COVID-19 are found to be responsible for the reduction of nitrous oxide by 20 to 77% globally. Predominantly, NO2 emissions were alleviated by 16 to 60% in different cities during COVID-19 time as compared to Pre-COVID-19 time (Burnett et al. 1999; Bylin et al. 1998; Bloom et al. 2013; Brown 2015; Federal Register 2020). The pandemic COVID-19-induced lockdowns has been responsible for the reduction of nitrous oxides from 20–30% (in China, Italy, France, Spain) to 77.3% (in São Paulo, Brazil). Emission of CO2 was also noticed to be decreased by 5–10%.
Similarly, the level of particulate matters was found to be reduced globally by 9 to 200% and in New Delhi, India witnessed the later higher level of changes in a never seen manner (Rodríguez-Urrego and Rodríguez-Urrego 2020). The reduction in the level of particulate matter experienced from 5–15% in Western Europe. The reduction of CO level under lockdowns was reduced by 30 to 60%. The reasons are attributed to the reduced fossil fuel combustion as the global fuel supply has been decreased by 4% in 2020 as compared to its counter time period in 2019 (Meteosim 2020). The combustion of 8% less coal fuel by April 2020 was observed as compared to April 2019. Almost 50% traffic congestion was decreased worldwide under the lockdowns (Rodríguez-Urrego and Rodríguez-Urrego 2020).
All the above data indicate the occurrence of the high level of air pollutants especially NO2 emissions and PM2.5 level during pre-COVID-19 time. For this reason, cities that experienced high air pollution and associated co-morbidities were also found to tally high COVID-19 infection and deaths in different age groups (Dutheil et al. 2020a, b; Table 3). One of the reasons is attributed to the high level of ACE-2 expression in the respiratory tracts under high air pollution conditions that increases the chance of infection and death (Kuan et al. 2011; Alifano et al. 2020; WHO 2020h) which in turn has increased the air quality in a never seen manner in modern time under lockdowns.
From the above discussion, one assumption is very clear that COVID-19 infection rate is aggravated with air pollution. Although, air transmission of the virus causing the disease was initially refused by many including WHO, now been considered as “air pollution has definite effects on the propagation of the virus in human host” (WHO 2020g, h). Mainly the severity of the COVID-19 is noticed to be high in patients that were documented in the areas where air pollution is predominant as compared to areas that experience cleaner air (APGH 2020). Although a study in Iran on 17 March 2020 has confirmed that COVID-19 is not communicated by air but the study has a limitation that the samples were collected within 2 to 5 m distance from the patients' beds were tested negative for SARS-CoV-2 (Faridi et al. 2020), subsequent experiments show opposite results.
Finally, the mechanism of severity is attributed to PM2.5 or NO2 mediated respiratory or cardiovascular issues, high ACE-2 expression (Fig. 6) and SARS-CoV-2 induced thrombogenesis in blood of patients. Nevertheless, indoor air pollution associated diseases have a positive correlation with the rate of severity and death in COVID-19 patients, indicating the recommendation of using appropriate masks even indoor where air pollution and COVID-19 are common (Brandon 2020). Therefore, a recent literature has summarised that “air pollution appropriate face mask” must be used as one of the preventive measures against COVID-19 in public places as well as indoors where air pollution is predominantly high. Organizations such as WHO therefore recommends wearing face masks for people having respiratory symptoms and it would provide less risk factor for others whom people care. Rationally, all in the quarantine centre must wear face masks to prevent potential transmission of COVID-19 by asymptomatic or pre-symptomatic people. People such as elderly, patients with co-morbidities that are susceptible to COVD-19 must wear face masks. WHO also recommends for universal use of face masks if their supply is enough.
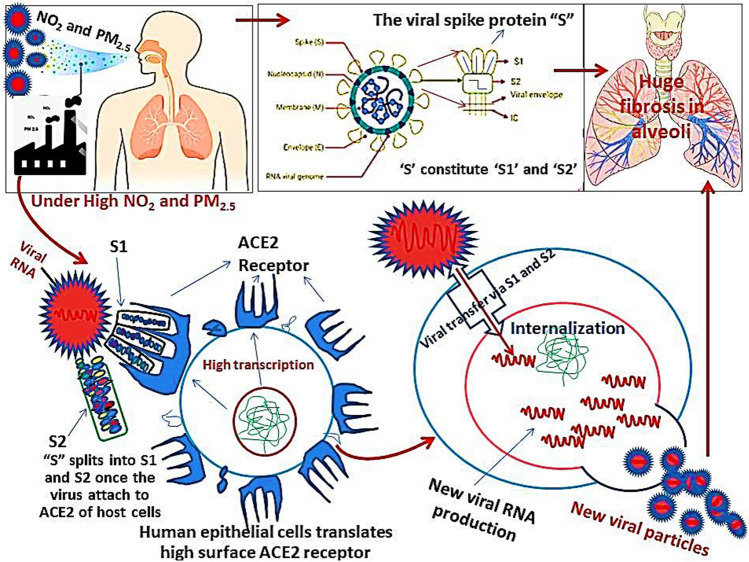
Fig. 6.
Possible effects of air pollution on COVID-19 severity via ACE-2 expression. Air pollution has a positive correlation with Angiotensin Converting Enzyme 2 (ACE-2), (that acts as Severe Acute Respiratory Syndrome Coronavirus-2 attachment receptor) expression in human respiratory epithelial cells and that may accelerate the viral infection and severity in the Coronavirus Disease COVID-19 patients leading to fatality. ACE-2 found to be upregulated under Nitrogen Dioxide (NO2) and Particulate Matter 2.5 (PM2.5) exposure; therefore, air pollution is an additional factor that causes severity in the COVID-19 patients. Therefore, both environmental interventions along with clinical approach are suggested for the management of the severity of COVID-19 where both made a common hotspot. ACE-2- Angiotensin converting Enzyme 2, Severe Acute Respiratory Syndrome Coronavirus 2, S- the Spike protein of Severe Acute Respiratory Syndrome Coronavirus -2 that constitutes two parts namely S1 and S2. RNA-Ribonucleic Acid
Hand hygiene also could be helpful to remove the virus as well as other aerosols (may contain microbes which could additionally increase the risk of comorbidities) that could contain infective materials. Additionally, urgent and deep research on the duration of protection activity provided by various types of face masks, on increasing the durability of disposable masks, and production of reusable masks are on call. It is needed to prevent air pollution associated troubles in general and to fight against infected droplet carried infective agents such as SARS-CoV-2 in particular. This must be considered as future pandemic plans in countries that are under the clutch of high air pollution” (Chin et al. 2020) because future pandemics similar to COVID-19 cannot be ruled out.
Conclusion
Air pollution has positive effects on the rate of propagation and severity of COVID-19 cases, as the rate of severity and death is higher in patients found in air polluted areas as compared to less air polluted area. The mechanism may be attributed to air pollution-mediated co-morbidities, aerosol-induced respiratory disorders and NO2-induced higher expression of ACE-2 receptor that acts as binding ligand for SARS-CoV-2 in respiratory cells in humans (Fig. 7). The pandemic COVID-19 is transmitted via air, particulate matters, and particles supporting air pollution or aerosols (infected patient’s coughs, sneezes, talks or sings) which are accepted to mediate severity or death in COVID-19 patients. It is because the virus can survive in aerosols up to 3 h. Low or medium income countries are found to experience both indoor and outdoor air pollution (WHO 2020j), so they need to take special action against combating air pollution. Both air pollution and COVID-19 lead to respiratory associated health risks and mortality. Therefore, both clinical and environmental interventions are suggested to control COVID-19 in countries where this pandemic disease and air pollution are common. Based on air pollution level, planning of nation specific present and future blueprints to combat similar air transmitted or air born endemic or pandemic is suggested.
Fig. 7.
Need of environmental co-intervention for COVID-19 control. Depending upon the level of NO2, PM2.5 level mediated Angiotensin Converting Enzyme 2 (ACE-2) expression level in alveolar cells of lungs, the Coronavirus Disease (COVID-19) patients may express the severity into asymptomatic, mild symptomatic and severely symptomatic cases depending on low (↑), moderate (↑↑) and high (↑↑↑) expression of ACE-2. Therefore, the environmental co-intervention is suggested along with clinical care to COVID-19 patients where air pollution and COVID-19 have common hot spots. NO2- Nitrogen dioxide, NOX-Oxides of nitrogen, PM2.5-Particulate matter 2.5
Acknowledgements
Thanks to the honourable Director, College of Basic Science and Humanities, Bhubaneswar to allow working from home under lockdown period during COVID-19 outbreaks for which this article could be written. The sources of few cartoons or figures collected from Deccan Heralds, EurekaAlert.com, LifeSciences.org, Giant microbes, Pharmaceutical Technology.com, Google images, WHO, NASA, weforum etc. under creative common attribution are acknowledged.
Authors Contribution
Conceptualization, data curation, formal analysis, funding acquisition, investigation, methodology, project administration, resources, software, supervision, validation, visualization, roles/writing—original draft, writing—review and editing are done by BRP and PKA.
Funding
Schemes number ECR/2016/001984 by Science Engineeing Research Board, DST, Government of India and scheme number 1188/ST, Bhubaneswar, dated 01.03.17, ST- (Bio)-02/2017 by the Department of Biotechnology DST, Government of Odisha, India to BRP are acknowledged.
Compliance with ethical standards
Conflict of interest
The author declares that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- APGH (2020) State of global air 2019: air pollution a significant risk factor worldwide. https://www.healtheffects.org/announcements/state-global-air-2019-air-pollution-significant-risk-factor-worldwide. Accessed 31 Aug 2020
- Alifano M, Alifano P, Forgez P, Iannelli A. Renin-angiotensin system at the heart of COVID-19 pandemic. Biochimie. 2020;174:30–33. doi: 10.1016/j.biochi.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF. The proximal origin of SARS-CoV-2. Nat Med. 2020 doi: 10.1038/s41591-020-0820-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aztatzi-Aguilar OG, Uribe-Ramírez M, Arias-Montaño JA, Barbier O, De Vizcaya-Ruiz A. Acute and subchronic exposure to air particulate matter induces expression of angiotensin and bradykinin-related genes in the lungs and heart: Angiotensin-II type-I receptor as a molecular target of particulate matter exposure. Part Fibre Toxicol. 2015;12:17. doi: 10.1186/s12989-015-0094-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BBC (2020) Coronavirus deaths exceed Sars fatalities in 2003. https://www.bbc.com/news/world-asia-china-51431087Accessed 31 Aug 2020
- Bashir MF, Bilal MA, Komal BJ, Bushra,, et al. Correlation between environmental pollution indicators and COVID-19 pandemic: a brief study in Californian context. Environ Res. 2020;187:109652. doi: 10.1016/j.envres.2020.109652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom B, Jones LI, Freeman G (2013) Summary health statistics for U.S. children: National health interview survey, 2012. In “Vital and health statistics”. Hyattsville MD, National Center for Health Statistics, U.S. Department of Health and Human Services. https://www.cdc.gov/nchs/data/series/sr_10/sr10_258.pdf. Accessed on 31 Aug 2020 [PubMed]
- Bourgonje AR, Abdulle AE, Timens W, et al. Angiotensin-converting enzyme-2 (ACE-2), SARS-CoV-2 and pathophysiology of coronavirus disease 2019 (COVID-19) J Pathol. 2020 doi: 10.1002/path.5471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandon S (2020) The link between air pollution and COVID-19 deaths. https://www.weforum.org/agenda/2020/04/link-between-air-pollution-covid-19-deaths-coronavirus-pandemic/. Accessed 28 Aug 2020
- Brauer M. How much, how long, what, and where: air pollution exposure assessment for epidemiologic studies of respiratory disease. Proc Am Thorac Soc. 2010;7:111–115. doi: 10.1513/pats.200908-093RM. [DOI] [PubMed] [Google Scholar]
- Brown JS. Nitrogen dioxide exposure and airway responsiveness in individuals with asthma. Inhal Toxicol. 2015;27:1–14. doi: 10.3109/08958378.2014.979960. [DOI] [PubMed] [Google Scholar]
- Burnett RT, Smith-Doiron M, Stieb D, Cakmak S, Brook JR. Effects of particulate and gaseous air pollution on cardiorespiratory hospitalizations. Arch Environ Health. 1999;54:130–139. doi: 10.1080/00039899909602248. [DOI] [PubMed] [Google Scholar]
- Bylin G, Hedenstierna G, Lindvall T, Sundin B. Ambient nitrogen dioxide concentrations increase bronchial responsiveness in subjects with mild asthma. Eur Respir J. 1988;1:606–612. [PubMed] [Google Scholar]
- CDC (2020) CDC https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidancemanagement-patients.html. Accessed on 31 Aug 2020
- Carlsten C, Dybuncio A, Becker A, Chan-Yeung M, Brauer M. Traffic-related air pollution and incident asthma in a high-risk birth cohort. Occup Environ Med. 2011;68:291–295. doi: 10.1136/oem.2010.055152. [DOI] [PubMed] [Google Scholar]
- Carugno M, Consonni D, Randi G, et al. Air pollution exposure, cause-specific deaths and hospitalizations in a highly polluted Italian region. Environ Res. 2016;147:415–424. doi: 10.1016/j.envres.2016.03.003. [DOI] [PubMed] [Google Scholar]
- Chafekar A, Fielding BC. MERS-CoV: understanding the latest human coronavirus threat. Viruses. 2018;10(2):93. doi: 10.3390/v10020093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan A, Singh RP. Decline in PM2.5 concentrations over major cities around the world associated with COVID-19. Environ Res. 2020;187:109634. doi: 10.1016/j.envres.2020.109634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin AWH, Chu JTS, Perera MRA, et al. Stability of SARS-CoV-2 in different environmental conditions. Lancet. 2020 doi: 10.1016/S2666-5247(20)30003-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiusolo M, Cadum E, Stafoggia,, et al. Air collaborative group short-term effects of nitrogen dioxide on mortality and susceptibility factors in 10 Italian cities: the EpiAir study. Environ Health Perspect. 2011;119:1233–1238. doi: 10.1289/ehp.1002904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow L (2020) World's biggest NO2 emissions hotspots revealed. https://www.ecowatch.com/worlds-biggest-no2-emissions-hotspots-2616234815.html. Accessed on 31 Aug 2020
- Cohen AJ, Brauer M, Burnett R, et al. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389(10082):1907–1918. doi: 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole M, Ozgen C, Strobl E (2020) Air pollution exposure linked to higher COVID-19 cases and deaths – new study. https://theconversation.com/air-pollution-exposure-linked-to-higher-covid-19-cases-and-deaths-new-study-141620. Accessed 28 Aug 2020
- Conticini E, Frediani B, Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ Pollut Barking Essex. 2020 doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crouse DL, Peters PA, Hystad P, et al. Ambient PM2.5, O3, and NO2 exposures and associations with mortality over 16 Years of follow-up in the Canadian census health and environment cohort (CanCHEC) Environ. Health Perspect. 2015;123(11):1180–1186. doi: 10.1289/ehp.1409276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui Y, Zhang ZF, Froines J, et al. Air pollution and case fatality of SARS in the People's Republic of China: an ecologic study. Environ Health. 2003;2(1):15. doi: 10.1186/1476-069X-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das K, Behera TR, Paital B. COVID-19 outbreak challenges in indian migrant pregnant and lactating mothers: learnt lesson demands hierarchical strategy for such future situation. In: Kaur P, Asea A, editors. Heat Shock Protein, Corona Virus. Berlin: Springer; 2020. [Google Scholar]
- Das K, Behera TR, Paital B. Global impacts of COVID-19 on socio-economic, education and ethico-religious factors. In: Kaur P, Asea A, editors. Heat Shock Protein, Corona Virus. Berlin: Springer; 2020. [Google Scholar]
- Das K, Paital B. First week of social lockdown versus medical care against COVID-19 - with special reference to India. Curr Trend Biotechnol Pharmacol. 2020;14(2):190–210. doi: 10.5530/ctbp.2020.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di-Cerbo A. Air pollution and SARS-CoV-2 in the Po Valley: possible environmental persistence? Minerva Med. 2020 doi: 10.23736/S0026-4806.20.06586-6. [DOI] [PubMed] [Google Scholar]
- Domingo JL, Rovira J. Effects of air pollutants on the transmission and severity of respiratory viral infections. Environ Res. 2020;187:109650. doi: 10.1016/j.envres.2020.109650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutheil F, Baker JS, Navel V. COVID-19 as a factor influencing air pollution? Environ Pollut. 2020;263(Pt A):114466. doi: 10.1016/j.envpol.2020.114466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutheil F, Navel V, Clinchamps M. The indirect benefit on respiratory health from the world's effort to reduce transmission of SARS - CoV-2. Chest pii. 2020;S0012–3692(20):30689–30699. doi: 10.1016/j.chest.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- European Environment Agency (2005) Communication from the Commission to the Council and the European Parliament - Thematic Strategy on Air Pollution. (COM(2005) 0446 final) https://scholar.google.com/scholar?q=European+Environment+Agency+Communication+from+the+Commission+to+the+Council+and+the+European+Parliament+-+Thematic+Strategy+on+Air+Pollution+2005+(COM(2005)+0446+final)+ Accessed 31Aug 2020
- FDA (2020) Emergency preparedness and response to coronavirus disease 2019 (COVID-19). https://www.fda.gov/emergency-preparedness-and-response/mcmissues/coronavirus-disease-2019-COVID-19. Accessed on 31 Aug 2020
- Faridi S, Niazi S, Sadeghi K, et al. A field indoor air measurement of SARS-CoV-2 in the patient rooms of the largest hospital in Iran. Sci Total Environ. 2020;725:138401. doi: 10.1016/j.scitotenv.2020.138401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fattorini D, Regoli F. Role of the chronic air pollution levels in the Covid-19 outbreak risk in Italy. Environ Pollut. 2020 doi: 10.1016/j.envpol.2020.114732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Federal Register (2020) Review of the primary national ambient air quality standards for oxides of nitrogen. https://www.federalregister.gov/documents/2018/04/18/2018-07741/review-of-the-primary-national-ambient-air-quality-standards-for-oxides-of-nitrogen. Accessed on 31 Aug 2020
- Filippini T, Heck JE, Malagoli C, DelGiovane C, Vinceti M. A review and meta-analysis of outdoor air pollution and risk of childhood leukemia. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 2015;33(1):36–66. doi: 10.1080/10590501.2015.1002999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frontera A, Cianfanelli L, Vlachos K, Landoni G, Cremona G. Severe air pollution links to higher mortality in COVID-19 patients: the "double-hit" hypothesis. J Infect. 2020;S0163–4453(20):30285–30291. doi: 10.1016/j.jinf.2020.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frontera A, Martin C, Vlachos K, Sgubin G. Regional air pollution persistence links to COVID-19 infection zoning. J Infect pii. 2020;S0163–4453(20):30173–30180. doi: 10.1016/j.jinf.2020.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fu Y, Kuppe C, Valev VK, et al. Surface-enhanced raman spectroscopy: a facile and rapid method for the chemical component study of individual atmospheric aerosol. Environ Sci Technol. 2017;51(11):6260–6267. doi: 10.1021/acs.est.6b05910. [DOI] [PubMed] [Google Scholar]
- Ge XY, Li JL, Yang XL, et al. Isolation and characterization of a bat SARS-like coronavirus that uses the ACE-2 receptor. Nature. 2013;503(7477):535–538. doi: 10.1038/nature12711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glowacka I, Bertram S, Herzog P, et al. Differential downregulation of ACE-2 by the spike proteins of severe acute respiratory syndrome coronavirus and human coronavirus NL63. J Virol. 2010;84(2):1198–1205. doi: 10.1128/JVI.01248-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gori T, Lelieveld J, Münzel T. Perspective: cardiovascular disease and the Covid-19 pandemic. Basic Res Cardiol. 2020;115(3):32. doi: 10.1007/s00395-020-0792-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Govt. of India (2020) COVID-19 State wise status. https://www.mygov.in/corona-data/covid19-statewise-status. Accessed on 30 Aug 2020
- Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak - an update on the status. Mil Med Res. 2020;7(1):11. doi: 10.1186/s40779-020-00240-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta R, Misra A. Contentious issues and evolving concepts in the clinical presentation and management of patients with COVID-19 infection with reference to use of therapeutic and other drugs used in Co-morbid diseases (Hypertension, diabetes etc) Diabetes Metab Syndr. 2020;14(3):251–254. doi: 10.1016/j.dsx.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Habibzadeh P, Stoneman EK. The novel coronavirus: a bird's eye view. Int J Occup Environ Med. 2020;11(2):65–71. doi: 10.15171/ijoem.2020.1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamming I, Timens W, Bulthuis ML, et al. Tissue distribution of ACE-2 protein, the functional receptor for SARS coronavirus. A first step in understanding SARS pathogenesis. J Pathol. 2004;203(2):631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassoun Y, James C, Bernstein DI. The effects of air pollution on the development of atopic disease. Clin Rev Allergy Immunol. 2019;57(3):403–414. doi: 10.1007/s12016-019-08730-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He S, Han J. Electrostatic fine particles emitted from laser printers as potential vectors for airborne transmission of COVID-19. Environ Chem Lett. 2020 doi: 10.1007/s10311-020-01069-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He MZ, Kinney PL, Li T, et al. Short- and intermediate-term exposure to NO2 and mortality: a multi-county analysis in China. Environ Pollut. 2020;261:114165. doi: 10.1016/j.envpol.2020.114165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He L, Zhang S, Hu J, et al. On-road emission measurements of reactive nitrogen compounds from heavy-duty diesel trucks in China. Environ Pollut. 2020;262:114280. doi: 10.1016/j.envpol.2020.114280. [DOI] [PubMed] [Google Scholar]
- Hoek G, Krishnan RM, Beelen R, et al. Long-term air pollution exposure and cardio- respiratory mortality: a review. Environ Health. 2013;12:43. doi: 10.1186/1476-069X-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute for Health Metrics and Evaluation (2020) Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. https://www.healthdata.org/research-article/measuring-universal-health-coverage-based-index-effective-coverage-health-services Accessed 31 Aug 2020 [DOI] [PMC free article] [PubMed]
- Khan J (2020) We've never made a successful vaccine for a coronavirus before. This is why it's so difficult. https://www.abc.net.au/news/health/2020-04-17/coronavirus-vaccine-ian-frazer/12146616. Accessed on 31 Aug 2020
- Kim KH, Kabir E, Kabir S. A review on the human health impact of airborne particulate matter. Environ Int. 2015;74:136–143. doi: 10.1016/j.envint.2014.10.005. [DOI] [PubMed] [Google Scholar]
- Krauskopf J, Caiment F, van Veldhoven K, et al. The human circulating miRNome reflects multiple organ disease risks in association with short-term exposure to traffic-related air pollution. Environ Int. 2018;113:26–34. doi: 10.1016/j.envint.2018.01.014. [DOI] [PubMed] [Google Scholar]
- Kuan TC, Yang TH, Wen CH, et al. Identifying the regulatory element for human angiotensin-converting enzyme 2 (ACE-2) expression in human cardiofibroblasts. Peptides. 2011;32(9):1832–1839. doi: 10.1016/j.peptides.2011.08.009. [DOI] [PubMed] [Google Scholar]
- Leng Z, Zhu R, Hou W, et al. Transplantation of ACE-2- mesenchymal stem cells improves the outcome of patients with COVID-19 pneumonia. Aging Dis. 2020;11(2):216–228. doi: 10.14336/AD.2020.0228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li T, Hu R, Chen Z, et al. Fine particulate matter (PM2.5): the culprit for chronic lung diseases in China. Chronic Dis Transl Med. 2018;4(3):176–186. doi: 10.1016/j.cdtm.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li M, Wang X, Lu C, et al. Nitrated phenols and the phenolic precursors in the atmosphere in urban Jinan. China Sci Total Environ. 2020;714:136760. doi: 10.1016/j.scitotenv.2020.136760. [DOI] [PubMed] [Google Scholar]
- Li W, Xu L, Liu X, et al. Air pollution-aerosol interactions produce more bioavailable iron for ocean ecosystems. Sci Adv. 2017;3(3):e1601749. doi: 10.1126/sciadv.1601749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C-I, Tsai C-H, Sun Y-L, et al. Instillation of particulate matter 2.5 induced acute lung 12 injury and attenuated the injury recovery in ACE-2 knockout mice. Int J Biol Sci. 2018;14:253–265. doi: 10.7150/ijbs.23489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martelletti L, Martelletti P. Air Pollution and the novel Covid-19 disease: a putative disease risk factor. SN Compr Clin Med. 2020;15:1–5. doi: 10.1007/s42399-020-00274-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meteosim (2020) World Most Polluted Cities - Meteosim [WWW Document] https://www.meteosim.com/en/world-most-polluted-citie/. Accessed on 28 Aug 2020
- Meulenbelt J, van Bree L, Dormans JA, et al. Biochemical and histological alterations in rats after acute nitrogen dioxide intoxication. Hum Exp Toxicol. 1992;11(3):189–200. doi: 10.1177/096032719201100307. [DOI] [PubMed] [Google Scholar]
- Mishra P, Paital B, Jena S, et al. Possible activation of NRF2 by Vitamin E/Curcumin against altered thyroid hormone induced oxidative stress via NFĸB/AKT/mTOR/KEAP1 signalling in rat heart. Sci Rep. 2019;9(1):7408. doi: 10.1038/s41598-019-43320-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musa S. Hepatic and gastrointestinal involvement in coronavirus disease 2019 (COVID-19): what do we know till now? Arab J Gastroenterol. 2020;21(1):3–8. doi: 10.1016/j.ajg.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myllyvirta L, Howard E (2020) Mapped: nitrogen dioxide pollution around the world. https://unearthed.greenpeace.org/2018/10/29/nitrogen-dioxide-no2-pollution-world-map/. Accessed on 31 Aug 2020
- Ogen Y. Assessing nitrogen dioxide (NO2) levels as a contributing factor to coronavirus (COVID-19) fatality. Sci Total Environ. 2020;726:138605. doi: 10.1016/j.scitotenv.2020.138605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz C, Linares C, Carmona R, Díaz J. Evaluation of short-term mortality attributable to particulate matter pollution in Spain. Environ Pollut. 2017;224:541–551. doi: 10.1016/j.envpol.2017.02.037. [DOI] [PubMed] [Google Scholar]
- Oudit GY, Kassiri Z, Jiang C, et al. SARS-coronavirus modulation of myocardial ACE-2 expression and inflammation in patients with SARS. Eur J Clin Invest. 2009;39(7):618–625. doi: 10.1111/j.1365-2362.2009.02153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paital B. Nurture to nature via COVID-19, a self-regenerating environmental strategy of environment in global context. Sci Total Environ. 2020;729:139088. doi: 10.1016/j.scitotenv.2020.139088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paital B, Das K, Behera TR. Social lockdown and ecological intervention for the prevention of the community spread of COVID 19. Cancer Res Stat Treat. 2020 doi: 10.4103/CRST.CRST_222_20. [DOI] [Google Scholar]
- Paital B, Das K, Parida SK. Inter nation social lockdown versus medical care against COVID-19, a mild environmental insight with special reference to India. Sci Total Environ. 2020;728:138914. doi: 10.1016/j.scitotenv.2020.138914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel JM, Sekharam KM, Block ER. Oxidant injury increases cell surface receptor binding of angiotensin II to pulmonary artery endothelial cells. J Biochem Toxicol. 1990;5(4):253–258. doi: 10.1002/jbt.2570050408. [DOI] [PubMed] [Google Scholar]
- Ramesh S (2020) Covid vaccine could come in a year, but life-as-usual years away, says WHO chief scientist. https://theprint.in/theprint-otc/covid-vaccine-could-come-in-a-year-but-life-as-usual-years-away-says-who-chief-scientist/409417/.Accessed on 31 Aug 2020
- Ritchie H, Roser M (2020) Air pollution. https://ourworldindata.org/air-pollution. Accessed on 31Aug 2020
- Rodríguez-Urrego D, Rodríguez-Urrego L. Air quality during the COVID-19: PM2.5 analysis in the 50 most polluted capital cities in the world. Environ Pollut. 2020;266(1):115042. doi: 10.1016/j.envpol.2020.115042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohde RA, Muller RA. Air pollution in China: mapping of concentrations and sources. Berkeley Earth PLoS One. 2015;10(8):e0135749. doi: 10.1371/journal.pone.0135749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose RM, Fuglestad JM, Skornik WA, et al. The pathophysiology of enhanced susceptibility to murine cytomegalovirus respiratory infection during short-term exposure to 5 ppm nitrogen dioxide. Am Rev Respir Dis. 1988;137:912–917. doi: 10.1164/ajrccm/137.4.912. [DOI] [PubMed] [Google Scholar]
- Rose RM, Pinkston P, Skornik WA (1989) Altered susceptibility to viral respiratory infection during short-term exposure to nitrogen dioxide. Res Rep Health Eff Inst 1–24. [PubMed]
- Roviello V, Roviello GN. Lower COVID-19 mortality in Italian forested areas suggests immunoprotection by Mediterranean plants. Environ Chem Lett. 2020 doi: 10.1007/s10311-020-01063-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarmadi M, Marufi N, Moghaddam VK. Association of COVID-19 global distribution and environmental and demographic factors: an updated three-month study. Environ Res. 2020 doi: 10.1016/j.envres.2020.109748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saurabh SS, Verma A, Singh A, Singh V, Pingali MS, Paital B, Das D, Varadwaj PK, Samanta SK. Outbreak of COVID-19: A detailed overview and its consequences. In: Kaur P, Asea A, editors. Heat shock protein, corona virus. Berlin: Springer; 2020. [DOI] [PubMed] [Google Scholar]
- Sharma VK, Jinadatha C, Lichtfouse E. Environmental chemistry is most relevant to study coronavirus pandemics. Environ Chem Lett. 2020;18:993–996. doi: 10.1007/s10311-020-01017-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- She J, Jiang J, Ye L, et al. 2019 novel coronavirus of pneumonia in Wuhan, China: emerging attack and management strategies. Clin Transl Med. 2020;9(1):19. doi: 10.1186/s40169-020-00271-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shereena MA, Khana S, Kazmi A, et al. COVID-19 infection: origin, transmission, and characteristics of human coronaviruses. J Adv Res. 2020;24:91–98. doi: 10.1016/j.jare.2020.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song W, Gui M, Wang X, Xiang Y. Cryo-EM structure of the SARS coronavirus spike glycoprotein in complex with its host cell receptor ACE-2. PLoS Pathog. 2018;14(8):e1007236. doi: 10.1371/journal.ppat.1007236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- South AM, Diz DI, Chappell MC. COVID-19, ACE-2, and the cardiovascular consequences. Am J Physiol Heart Circ Physiol. 2020;318(5):H1084–H1090. doi: 10.1152/ajpheart.00217.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sriram K, Insel PA. A hypothesis for pathobiology and treatment of COVID-19: the centrality of ACE1/ACE-2 imbalance. Br J Pharmacol. 2020 doi: 10.1111/bph.15082.10.1111/bph.15082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun S, Han J. Unflushable or missing toilet paper, the dilemma for developing communities during the COVID-19 episode. Environ Chem Lett. 2020 doi: 10.1007/s10311-020-01064-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson JE. Airborne particulate matter: human exposure and health effects. J Occup Environ Med. 2018;60(5):392–423. doi: 10.1097/JOM.0000000000001277. [DOI] [PubMed] [Google Scholar]
- Tipnis SR, Hooper NM, Hyde R. A human homolog of angiotensin-converting enzyme. Cloning and functional expression as a captopril-insensitive carboxypeptidase. J Biol Chem. 2000;275(43):33238–33243. doi: 10.1074/jbc.M002615200. [DOI] [PubMed] [Google Scholar]
- Tositti L, Brattich E, Parmeggiani S, Bolelli L, Ferri E, Girotti S. Airborne particulate matter biotoxicity estimated by chemometric analysis on bacterial luminescence data. Sci Total Environ. 2018;640–641:1512–1520. doi: 10.1016/j.scitotenv.2018.06.024. [DOI] [PubMed] [Google Scholar]
- Tran K, Cimon K, Severn M, et al. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS ONE. 2012;7(4):e35797. doi: 10.1371/journal.pone.0035797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travaglio M, Yu Y, Popovic R, Selley L, Leal NS, Martins LM (2020) Links between air pollution and COVID-19 in England. medRxiv. 10.1101/2020.04.16.20067405 [DOI] [PMC free article] [PubMed]
- USA AQI (2020) U.S. Air Quality Index. AQI Basics. https://www.airnow.gov/aqi/aqi-basics/. Accessed on 30 Aug 2020
- van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382(16):1564–1567. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vaduganathan M, Vardeny O, Michel T, et al. Renin-angiotensin-aldosterone system inhibitors in patients with Covid-19. N Engl J Med. 2020;382(17):1653–1659. doi: 10.1056/NEJMsr2005760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO (2020a) Coronavirus disease 2019 (COVID-19) Situation Report—91. file:///C:/Users/HP/Desktop/SToten%2520DIscussion/WHO%2520CORONA%2520status.pdf. Accessed on 31Aug 2020
- WHO (2020b) WHO Coronavirus Disease (COVID-19) Dashboard. Rolling updates on coronavirus disease (COVID-19). https://covid19.who.int/.Accessed on 31 Aug 2020
- WHO (2020c) World Health Organization. Clinical management of severe acute respiratory infection whennovel coronavirus (nCoV) infection is suspected https://www.who.int/publicationsdetail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected.Accessed on 31 Aug 2020
- WHO (2020d) Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) https://www.who.int/docs/default-source/coronaviruse/who-china-joint-mission-on-COVID-19-final-report.pdf.Accessed on 31 Aug 2020
- WHO (2020e) Coronavirus disease (COVID-19) Pandemic. https://www.who.int/emergencies/diseases/novel-coronavirus-2019. Accessed on 31 Aug 2020
- WHO (2020f) Air pollution. https://www.who.int/health-topics/air-pollution#tab=tab_1. Accessed on 31 Aug 2020
- WHO (2020g) Air pollution. https://www.who.int/health-topics/air-pollution#tab=tab_1. Accessed on 26 Aug 2020
- WHO (2020h) Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations. https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendationsAccessed on 31 Aug 2020
- WHO (2020i) Transmission of SARS-CoV-2: implications for infection prevention precautions. https://www.who.int/health-topics/air-pollution#tab=tab_1. Accessed 24 Aug 2020
- WHO (2020j) Ambient (outdoor) air pollution https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health. Accessed 28 Aug 2020
- Walker K (2020) State of Global Air 2019: Air pollution a significant risk factor worldwide. https://www.healtheffects.org/announcements/state-global-air-2019-air-pollution-significant-risk-factor-worldwide Accessed on 28Aug 2020
- Wang H, Dwyer-Lindgren L, Lofgren KT, et al. Age-specific and sex-specific mortality in 187 countries, 1970–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2071–2094. doi: 10.1016/S0140-6736(12)61719-X. [DOI] [PubMed] [Google Scholar]
- Wang X, Han J, Lichtfouse E. Unprotected mothers and infants breastfeeding in public amenities during the COVID-19 pandemic. Environ Chem Lett. 2020;18:1447–1450. doi: 10.1007/s10311-020-01054-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang L, Li M, Yu S, Chen X, Li Z, Zhang Y, Jiang L, Xia Y, Li J, Liu W, Li P, Lichtfouse E, Rosenfeld D, Seinfeld JH. Unexpected rise of ozone in urban and rural areas, and sulfur dioxide in rural areas during the coronavirus city lockdown in Hangzhou, China: implications for air quality. Environ Chem Lett. 2020;18:1713–1723. doi: 10.1007/s10311-020-01028-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Willyard C. Coronavirus blood-clot mystery intensifies Research begins to pick apart the mechanisms behind a deadly COVID-19 complication. Nature. 2020;581:250. doi: 10.1038/d41586-020-01403-8. [DOI] [PubMed] [Google Scholar]
- Woon FLW, Sun, Q (2020) Electrostatic charged nanofiber filter for filtering airborne novel coronavirus (COVID-19) and nano-aerosols. 10.1016/j.seppur.2020.116886 [DOI] [PMC free article] [PubMed]
- Wu C, Wang G, Li J, et al. Non-agricultural sources dominate the atmospheric NH3 in Xi'an, a megacity in the semi-arid region of China. Sci Total Environ. 2020;722:137756. doi: 10.1016/j.scitotenv.2020.137756. [DOI] [PubMed] [Google Scholar]
- Wu C, Wang G, Li J, et al. The characteristics of atmospheric brown carbon in Xi'an, inland China: sources, size distributions and optical properties. Atmos Chem Phys. 2020;20:2017–2030. doi: 10.5194/acp-20-2017-2020. [DOI] [Google Scholar]
- Wu X, Nethery RC., Sabath BM, Braun D, Dominici F (2020) Exposure to air pollution and COVID-19 mortality in the United States:a nationwide cross-sectional study. medRxiv. 10.1101/2020.04.05.20054502
- Yan J, Chen L, Lin Q, et al. Chemical characteristics of submicron aerosol particles during a long-lasting haze episode in Xiamen, China. Atm Environ. 2015;113:118–126. doi: 10.1016/j.atmosenv.2015.05.003. [DOI] [Google Scholar]
- Yang BY, Guo Y, Markevych I, et al. Association of long-term exposure to ambient air pollutants with risk factors for cardiovascular disease in China. JAMA Netw Open. 2019;2(3):e190318. doi: 10.1001/jamanetworkopen.2019.0318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao TT, Qian JD, Zhu WY, et al. A systematic review of lopinavir therapy for SARS coronavirus and MERS coronavirus-A possible reference for coronavirus disease-19 treatment option. J Med Virol. 2020 doi: 10.1002/jmv.25729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaki AM, van Boheemen S, Bestebroer TM, et al. Isolation of a novel coronavirus from a man with pneumonia in Saudi Arabia [published correction appears in N Engl J Med. Jul 25;369(4):394] N Engl J Med. 2013;367(19):1814–1820. doi: 10.1056/NEJMoa1211721. [DOI] [PubMed] [Google Scholar]
- Zemouri C, de Soet H, Crielaard W, Laheij A. A scoping review on bio-aerosols in healthcare and the dental environment. PLoS ONE. 2017;12(5):e0178007. doi: 10.1371/journal.pone.0178007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng Y, Ma Y, Zhang J. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020;17(5):259–260. doi: 10.1038/s41569-020-0360-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(1038):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu C, Li J, Chen H, et al. Inorganic composition and occult deposition of frost collected under severe polluted area in winter in the North China Plain. Sci Total Environ. 2020;722:137911. doi: 10.1016/j.scitotenv.2020.137911. [DOI] [PubMed] [Google Scholar]
- Zhu Y, Xie J, Huang F, Cao L. Association between short-term exposure to air pollution and COVID-19 infection: Evidence from China. Sci Total Environ. 2020;727:138704. doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]