Abstract
Introduction
Quality of emergency department (ED) care affects patient outcomes substantially. Quality indicators (QIs) for ED care are a major challenge due to the heterogeneity of patient populations, health care structures and processes in Germany. Although a number of quality measures are already in use, there is a paucity of data on the importance of these QIs on medium-term and long-term outcomes. The evaluation of outcome relevance of quality indicators in the emergency department study (ENQuIRE) aims to identify and investigate the relevance of QIs in the ED on patient outcomes in a 12-month follow-up.
Methods and analysis
The study is a prospective non-interventional multicentre cohort study conducted in 15 EDs throughout Germany. Included are all patients in 2019, who were ≥18 years of age, insured at the Techniker Krankenkasse (statutory health insurance (SHI)) and gave their written informed consent to the study.
The primary objective of the study is to assess the effect of selected quality measures on patient outcome. The data collected for this purpose comprise medical records from the ED treatment, discharge (claims) data from hospitalised patients, a patient questionnaire to be answered 6–8 weeks after emergency admission, and outcome measures in a 12-month follow-up obtained as claims data from the SHI.
Descriptive and analytical statistics will be applied to provide summaries about the characteristics of QIs and associations between quality measures and patient outcomes.
Ethics and dissemination
Approval of the leading ethics committee at the Medical Faculty of the University of Magdeburg (reference number 163/18 from 19 November 2018) has been obtained and adapted by responsible local ethics committees.
The findings of this work will be disseminated by publication of peer-reviewed manuscripts and presentations as conference contributions (abstracts, poster or oral presentations).
Moreover, results will be discussed with clinical experts and medical associations before being proposed for implementation into the quality management of EDs.
Trial registration number
German Clinical Trials Registry (DRKS00015203); Pre-results.
Keywords: accident & emergency medicine, quality in health care, health & safety, health services administration & management
Strengths and limitations of this study.
The strength of the present study is the linkage of treatment and outcome data on an individual level to evaluate the association of quality indicators in the emergency department (ED) with medium-term and long-term outcomes.
Another strength is a sophisticated data protection policy that allows data linkage from different sources at an individual level in conjunction with the protection of the personal privacy of individuals who participate.
Strength and limitation in one: the study is conducted in the real-life setting of the ED.
Limitations result from the quality of routine data in terms of completeness and accuracy.
Limitations of the study result from the necessity of a written consent, which results in a limited access to some patients and from the inclusion of only the insured persons of one statutory health insurance (Techniker Krankenkasse) that may not represent the total cohort of all ED patients.
Background
Emergency departments (EDs) play a crucial role within the healthcare system as gateway into clinical care for unscheduled arrivals of patients with acute, potentially life-threatening conditions. The patient cohort in the ED is characterised by a great heterogeneity with regards to presenting complaints,1 2 severity of illness or injury, acuity and others. Additionally, the complexity of emergency admissions increases with the ageing population and the increase in the number of patients suffering from frailty and multiple comorbidities.3
There is strong evidence that assessment of quality in the ED can improve quality of care and patient outcomes. This makes implementation of quality improvement programmes necessary to deliver high quality of care to patients.4
Over the past two decades, several systematic literature reviews have been published summarising relevant quality indicators (QIs) proposed for implementation in the EDs. Well-described and validated QIs are available for patients with trauma,5 6 and musculoskeletal injuries7 as well as geriatric patients.8
In 2013, Sørup and colleagues summarised relevant quality measures to assess overall ED performance. They divided them into three groups related to patients (eg, left without being seen), staffing (eg, occupation profile) and operational performance (eg, timelines).9
Regarding large patient numbers in EDs, routinely recorded data stored in information systems are an optimal data source for QI calculation. The use of an ED information system (EDIS) to collect structured medical information is a necessary prerequisite.10 A national documentation standard for EDs according to the German Emergency Department Medical Record (GEDMR) was established in 2010 by the German Interdisciplinary Association for Intensive Care and Emergency Medicine.11 In a systematic literature search, Hörster et al identified 25 QIs that were mentioned at least two times in independent sources. A total of 10 QIs were identified that can be derived from this GEDMR data set.12 These findings are in agreement with the findings from Kulla et al13 who rated and evaluated these QIs for their scientific relevance and practicability in German EDs using a modified QUALIFY approach.14
While there are a variety of data on QIs in EDs, systematic studies and reliable information on the effect of these QIs on medium-term and long-term outcomes are lacking. For patients with trauma, who represent a small group of ED patients, Boyd and coworkers found no association between intensity and nature of QIs in trauma centres with patient outcomes.15 For severely injured patients, a set of 40 QIs has recently been rated by experts and validated in a national registry using mortality as outcome.16 Conflicting results have been reported for other established QIs in emergency care. In some countries, length of stay in EDs (ED-LOS) was implemented as a main QI and policy measures were taken to achieve time targets under 4 or 6 hours, respectively.17–19 ED-LOS is a well-characterised QI with regards to patients outcome. However, results are conflicting. Findings from Jones et al suggest that with introduction of the 6-hour time target policy, most investigated outcomes, such as mortality and representation to the ED, remained unchanged; while others improved, such as hospital LOS.20 In contrast, Rose et al found that a prolonged ED stay may worsen outcomes for the subgroup of patients admitted to intensive care units.21 Assessing quality in the ED by using ‘LOS’ as a single key indicator remains controversial. Improvement of the ED-LOS did not result in an improvement of other ED QIs over the same time period.22 Suriyawongpaisal and coworkers conclude that a set of indicators and different outcome measures should be considered instead.23
Outcome measures in the ED such as mortality, or unplanned re-admission within 24 hours, 72 hours or 7 days for the same or similar complaint already have been analysed in detail,9 20 24–26 however, they are limited to events within the same institution. It is difficult to obtain outcome measures in a cross-sectoral setting and in a medium-term and long-term follow-up for analysis.
This manuscript describes the study design for the evaluation of outcome relevance of QIs for the EDs (ENQuIRE) in Germany using medical data from EDs, claims data from one statutory health insurance (SHI) fund and survey data. A set of QIs for application on routine ED documentation with a focus on long-term outcomes will be evaluated, established and possibly implemented into the ED quality management.
Methods/design
The study aims to evaluate QIs in the ED in terms of their relevance for the treatment outcomes including patient-reported outcomes. This is enabled by linking clinical data from the electronic documentation in the ED with quantitative and consistent outcome results in a 12-month follow-up using claims data of the SHI at an individual level.
A scientific advisory board consisting of representatives of medical associations (German Interdisciplinary Association for Intensive Care and Emergency Medicine and the German Society for Interdisciplinary Emergency and Acute Medicine), clinical experts from the field of emergency medicine and a patient representative (German Coalition for Patient Safety, Aktionsbündnis Patientensicherheit e.V., Berlin) has been established to provide scientific advice on the project, to represent the interests of patients and support the implementation of the results.
Setting
The ENQuIRE study is a prospective non-interventional multicentre cohort study. Fifteen EDs throughout Germany including university hospitals as well as municipal hospitals, clinics of different care levels and located in cities with different population numbers are participating in this study (table 1). The study includes all eligible patients throughout 2019.
Table 1.
Characteristics of participating emergency departments
| Patients per year | Emergency departments (n=15) |
| <20 000 | 2 |
| 20 000–50 000 | 10 |
| >50 000 | 3 |
| Population/city of | |
| <100 000 | 3 |
| >100 000 <200 000 | 9 |
| >500 000 | 3 |
| Level of emergency care | |
| basic | 1 |
| specialised | 6 |
| maximum | 8 |
| Academic status | |
| University hospital | 5 |
| Academic teaching hospital | 8 |
| Non teaching | 2 |
The Techniker Krankenkasse (TK) is Germany’s largest health insurance company with approximately 10.6 million persons insured. According to Hoffmann and Icks27, persons insured at the TK are more often men, have a higher education level and are in a better state of health compared with the total of all insured persons in Germany.
The study protocol was reviewed and approved by the leading ethics committee at the Medical Faculty of the University of Magdeburg (163/18 from 19 November 2018) and by relevant institutional ethics committees: Carl von Ossietzky University Oldenburg (2018-142), University Hospital Jena (2018-1259-Daten), University Medical Center Göttingen (26/12/18Ü) and by local ethics committees of the State Medical Associations: Sächsische Landesärztekammer, Dresden (EK-BR-2/19-1), Ärztekammer Schleswig Holstein, Bad Segeberg (001/19 m), Ärztekammer Bremen (654) and Landesärztekammer Rheinland-Pfalz, Mainz (2019-14014).
Data privacy is in agreement with the General Data Protection Regulation. A data protection policy has been developed involving a trusted third party (TTP). This TTP maintains the patient lists, mails patient questionnaires and queries ED treatment data as well as claims data from the SHI. For data linkage, the pseudonymisation is carried out in two stages. First, a subject identification code is generated within the TTP. Second, a data delivery web service is used to generate random 64-digit, second-level alphanumeric pseudonyms. Pseudonymised data are then routed to the project’s evaluation unit for analysis.
An application had been submitted to the German Federal Insurance Office (in German Bundesversicherungsamt) for permission to use the claims data of the SHI while guaranteeing all data protection aspects according to §75 Sozialgesetzbuch, that is, Social Security Code (SGB) X.
Inclusion and exclusion criteria
All patients attending a participating ED in 2019 were screened for eligibility. The inclusion criteria were defined as follows: 18 years of age or older and insured at the TK. Exclusion criteria were insufficient German language skills and no residence in Germany. All eligible patients should be included, independently of presenting complaints, severity of illness or injury, mode of arrival, acuity, hospital admission or outpatient treatment, weekday and daytime.
If possible, patients were asked for written consent in the ED by a study nurse or by trained nursing staff. Additionally, admitted patients could be contacted during their inpatient stay if informed consent was not possible in the ED. Non-admitted patients who did not have the opportunity to provide consent during their stay in the ED were contacted by post.
The target number of participants to be recruited was calculated according to the mean number of ED attendees in the participating EDs in the last 2 years and an average percentage of TK insured patients of about 12.9%. After reduction by an expected amount of about 10% of patients aged <18 years, the number of patients to be recruited was estimated at about 25 900. A subgroup of 5000 patients who have given consent to be contacted again received a questionnaire 6–8 weeks after emergency admission to evaluate health-related quality of life (HrQoL). The self-reported questionnaire includes items adapted from the short form 12 version 2 (SF12v2) survey of the German Socio-Economic Panel28 as well as socioeconomic items and questions on patient satisfaction. To test the questionnaire, a pretest had been conducted in two study centres for evaluation in terms of readability and ease of understanding.
Selection of QIs
For the selection of QI, a set of QIs was collected based on systematic literature search in MEDLINE (PubMed) and screening of publications of health organisations (National Health Service, Agency for Healthcare Research and Quality, National Quality Forum, Canadian Institute for Health Information, German Institute for Quality assurance and Transparency in Healthcare). Extracted QIs were discussed with clinical and IT experts with regards to practicability, operational feasibility for routine collection and data validity. A core set of selected QIs including mainly patient-centred parameters and process times as well as selected structural data are shown in table 2.
Table 2.
Core set of quality indicators for analysis
| Quality indicator | Reference |
| Time from arrival to CT | 12 |
| Length of stay (LOS) of admitted patients | 12 41–49 |
| LOS of non-admitted patients | 12 |
| Left before/without being seen | 12 46–48 |
| Time from arrival to initial triage | 12 46 |
| Brain imaging in stroke suspicious patients | 50 |
| Time from arrival to pain management | 7 47 |
| Emergency department staffing: nurses (full-time equivalent) per patients | 41 46 48 |
| Left before treatment completion | 41 46 48 49 |
| Time from arrival to provider | 41 42 46 48 |
| Left against medical advice | 48 |
| Time from arrival to first ECG in suspected cardiac chest pain or acute myocardial infarction | 49 51 |
| Time from arrival to brain CT for patients presenting within 4 hours of onset of symptoms consistent with a stroke | 42 49 |
| ECG within 10 min of arrival for patients presenting with chest pain | 51 |
| ECG for patients with non-traumatic chest pain | 51 |
| Time from arrival to intravenous tissue plasminogen activator within 4.5 hours of symptom onset in patients with acute ischaemic stroke | 42 52 |
| ECG performed for syncope | 53 |
| Time from arrival to chest radiography for admitted patients | 54 |
| Time from arrival to chest radiography for non-admitted patients | 54 |
| Determination of the respiratory rate at admission for patients with outpatient-acquired pneumonia | 55 |
| Time from arrival to reperfusion for patients with acute myocardial infarction | 56 |
Outcome
The primary aims of the study are:
Identification of strengths and weaknesses of the QI.
Checking operationalisability and feasibility of QIs in real life.
Evaluation of the outcome relevance of QIs in the ED by determination of the influence of QI performance on mortality, morbidity, incapacity to work and the use of healthcare facilities after discharge from the ED.
The long-term goal of the investigation is a set of evaluated QIs ready for implementation into quality assessment programmes in EDs.
Data linkage
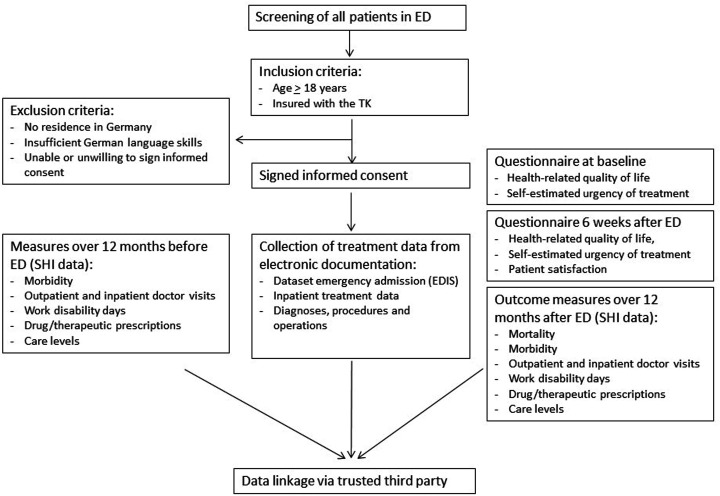
After completion of the recruitment phase, clinical records will be extracted from the routine documentation (clinical dataset is shown in table 3) using, for example, the infrastructure of the German Emergency Department Data Registry (GEDD-registry, AKTIN) and linked with outcome variables from SHI collected in a follow-up over 12 months. This includes variables such as mortality, morbidity, incapacity to work, levels of care, prescriptions of drugs, therapeutic remedies and aids as well as repeated outpatient and inpatient treatments (table 4). For adjustment of patients’ health status before ED admission, the claims data of the SHI over 12 months before the ED contact will be used (figure 1).
Table 3.
Patient and treatment data derived from the basic module of the German Emergency Department Medical Record
| Patient data |
| Age (years) |
| Gender |
| Referral |
| Transport |
| Anamnesis |
| Presenting complaints (CEDIS) |
| Duration of symptoms |
| Triage system (MTS or ESI) |
| Triage level |
| Vital signs |
| Respiratory frequency |
| Oxygen saturation |
| Systolic blood pressure |
| Heart rate |
| Core temperature |
| VAS pain (0–10) |
| Glasgow coma scale |
| Rankin |
| Pupillary reflex |
| Diagnosis |
| Leading diagnosis |
| Number of diagnoses |
| Discharge (outpatient, inpatient) |
| Examinations |
| ECG |
| Sonography |
| Echocardiography |
| CT/cCT |
| Traumascan |
| X-ray (spine, thorax, pelvis, limbs) |
| MRI |
| Laboratory (BGA, urine) |
| Time stamps |
| Admission |
| Triage |
| Start of therapy |
| First contact with a physician |
| ECG |
| Sonography |
| Echocardiography |
| CT/cCT |
| Traumascan |
| X-ray (spine, thorax, pelvis, limbs) |
| MRI |
| Laboratory (BGA, urine) |
| Discharge from ED |
BGA, blood gas analysis; (c)CT, (cranial) computer tomography; CEDIS, Canadian emergency department information system; ECG, electrocardiogram; ED, emergency department; ESI, Emergency Severity Index; MRI, magnetic resonance imaging; MTS, Manchester Triage System; VAS, Visual Analogue Scale.
Table 4.
Contents of SHI claims data for deriving patients’ outcome
| Patient data |
| Year of birth |
| Postcode |
| Type of employment |
| Claim to sick pay |
| Duration of occupational disability |
| Nursing care level |
| Duration of need for nursing care |
| Termination (reason and date) |
| Periods of insurance (duration pre and post) |
| Cases of incapacity for work |
| Diagnosis (ICD) |
| Date of beginning and end of incapacity |
| Physician’s specialty (code) |
| Quarter of diagnosis identification |
| Therapeutic products and aids |
| Physician’s specialty (code) |
| Type and amount of therapeutical sessions/aid |
| Date of prescription |
| Service provider (code and date) |
| Outpatient treatment |
| Service provider (code) |
| Date of beginning and end of treatment |
| Physician’s specialty (code) |
| Diagnosis (ICD) |
| Services provided (code and date) |
| Procedures (OPS-code and localisation) |
| Inpatient treatment |
| Department’s specialty (code) |
| Admission (reason and date) |
| Discharge (reason and date) |
| Diagnosis (ICD) |
| Procedure (OPS-code, date, localisation) |
| Outpatient pharmaceutical supply |
| Physician’s specialty (code) |
| Date of prescription and date of prescription filled |
| Amount of prescripted unit dose (daily defined dose) |
| Anatomical therapeutic chemical code |
ICD, International Classification of diseases and related health problems; OPS, German classification of operations and procedures; SHI, statutory health insurance.
Figure 1.
Flowchart of the study design. ED, emergency department; EDIS, ED information system; SHI, statutory health insurance; TK, Techniker Krankenkasse.
Analyses
Descriptive and analytical statistics will be applied to provide an overview about the characteristics of the QI and the associations between quality measures and patient outcome. Quality measures will be analysed as either dichotomous or graded variables and associated with appropriate outcome measures. Analyses will be performed for the entire cohort and for subgroups of selected presenting complaints (Canadian Emergency Department Information System (CEDIS) presenting complaint list).29 30
In order to assess representativeness of the cohort of patients, who have given consent (a subgroup of the TK insured), the distribution of variables (demographic data, eg, age, gender and ED data, eg, mode of arrival, presenting complaints, triage, admission), will be compared with anonymised corresponding data from the total cohort of all ED patients of participating hospitals in the observation period.
Furthermore, the validity of retrospective reporting of HrQoL when arriving in the ED will be investigated in a subgroup of study participants who receive a questionnaire to report their HrQoL during the initial ED visit and 6 weeks after. The retrospective recording of HrQoL in the setting of EDs is neither validated nor has the extent and direction of a possible systematic bias due to retrospective survey or the current emergency situation been investigated sufficiently.31–33
Patient and public involvement
There was no patient or public involvement in the design of the study.
Discussion
Care structures and processes in EDs as well as the healthcare service provided can directly influence the outcome of patients in terms of quality of health and HrQoL. The ultimate goal for quality improvement is a better treatment outcome. Quality management is required from the healthcare providers by Federal law (§136 SGB V). The identification of outcome-related QIs is of considerable interest for the patient-relevant quality management in EDs. These QIs may support improvements in patient-relevant processes in the ED. The ENQuIRE study will help to establish a set of meaningful QIs evaluated for their relation to patients’ outcome. For the first time, ENQuIRE will link clinical routine data with SHI data to analyse the influence of patient-centred parameters, process times and treatment procedures on patient medium-term and long-term outcomes. Regarding patient morbidity and utilisation of health services, routine data of the SHI system are an important source of information. These data are usually characterised by high external validity.34 However, since these data are secondary data, they must be critically examined for use in scientific questions.35 While the linkage of patient data from different sources as applied in our study is a relatively new approach in medical research,36 several scientific standards for using claims data in research actually have been established.37
The use of quality measures should ideally result in an improvement of outcome measures without increasing the risk for unintended dysfunctional consequences,38 misplaced incentives or side effects.39 Focusing on a single QI without considering other factors that affect quality of care can lead to poor clinical outcomes. These findings support the approach of this study to define not a single but a set of outcome-relevant QIs.
Results of this study can be implemented into the current activities for the planned reorganisation of emergency care in Germany.40 Considering the patient-related quality of care, optimised organisational models can be developed from healthcare providers. The results of the ENQuIRE project will constitute the basis for a future standardised and comprehensive quality management in EDs.
Preliminary results will be submitted for publication in 2021. The discussion of results will be performed with clinical experts and medical associations before being proposed for implementation into the quality management of the ED. Thus, the results of ENQuIRE could be directly implemented into the quality management and could be relevant to health policy decisions.
Ethics and dissemination
This study was approved by the leading ethics committee at the Medical Faculty of the University of Magdeburg (163/18 from 19 November 2018) and by relevant institutional ethics committees: Carl von Ossietzky University Oldenburg (2018-142), University Hospital Jena (2018-1259-Daten), University Medical Center Göttingen (26/12/18Ü) and by local ethics committees of the State Medical Associations: Sächsische Landesärztekammer, Dresden (EK-BR-2/19-1), Ärztekammer Schleswig Holstein, Bad Segeberg (001/19 m), Ärztekammer Bremen (654) and Landesärztekammer Rheinland-Pfalz, Mainz (2019-14014). Written informed consent was obtained from all participants who were informed about the purpose and risks of the study. Findings of the study will be made available as oral or poster presentations at scientific conferences and through peer-reviewed journals.
Supplementary Material
Acknowledgments
The authors would like to acknowledge all ENQuIRE study participants. Additionally, the authors would like to thank Dr Christopher Shanley, University of Technology Sydney, for proofreading of the manuscript.
Footnotes
Twitter: @RainerRohrig
Contributors: WiS, FG, FW, SaD, AS, MM, RL, DH-S and RR were involved in the design of the study. SuD, WeS, JP, RO, JH and MM contributed to the design and development of the study protocol. First draft of the manuscript was written by SuD, WeS, JP, JB, AS, FG and WiS. All authors critically revised the manuscript, gave final approval of the manuscript and are accountable for the accuracy and integrity of the manuscript.
Funding: The study is funded by the Innovation Committee of the Federal Joint Committee (in German: Innovationsfonds des Gemeinsamen Bundesausschusses) under the grant number: 01VSF17005. The funder had no role in the study design and data collection and on writing the manuscript.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Mockel M, Searle J, Muller R, et al. Chief complaints in medical emergencies: do they relate to underlying disease and outcome? the Charité emergency medicine study (CHARITEM). Eur J Emerg Med 2013;20:103–8. 10.1097/MEJ.0b013e328351e609 [DOI] [PubMed] [Google Scholar]
- 2.Greiner F, Brammen D, Kulla M, et al. Standardisierte Erhebung von Vorstellungsgründen in Der Notaufnahme Implementierung von codierten Vorstellungsgründen in das elektronische Notaufnahmeinformationssystem eines Schwerpunktversorgers und deren Potenzial für die Versorgungsforschung. Med Klin Intensivmed Notfmed 2018;113:115–23. [DOI] [PubMed] [Google Scholar]
- 3.Pines JM, Mullins PM, Cooper JK, et al. National trends in emergency department use, care patterns, and quality of care of older adults in the United States. J Am Geriatr Soc 2013;61:12–17. 10.1111/jgs.12072 [DOI] [PubMed] [Google Scholar]
- 4.Schuur JD, Hsia RY, Burstin H, et al. Quality measurement in the emergency department: past and future. Health Aff 2013;32:2129–38. 10.1377/hlthaff.2013.0730 [DOI] [PubMed] [Google Scholar]
- 5.Stelfox HT, Straus SE, Nathens A, et al. Evidence for quality indicators to evaluate adult trauma care: a systematic review. Crit Care Med 2011;39:846–59. 10.1097/CCM.0b013e31820a859a [DOI] [PubMed] [Google Scholar]
- 6.Bieler D, Hörster A, Lefering R, et al. Evaluation of new quality indicators for the TraumaRegister DGU® using the systematic QUALIFY methodology. Eur J Trauma Emerg Surg 2020;46:449–60. 10.1007/s00068-018-1055-z [DOI] [PubMed] [Google Scholar]
- 7.Strudwick K, Nelson M, Martin-Khan M, et al. Quality indicators for musculoskeletal injury management in the emergency department: a systematic review. Acad Emerg Med 2015;22:127–41. 10.1111/acem.12591 [DOI] [PubMed] [Google Scholar]
- 8.Burkett E, Martin-Khan MG, Gray LC. Quality indicators in the care of older persons in the emergency department: a systematic review of the literature. Australas J Ageing 2017;36:286–98. 10.1111/ajag.12451 [DOI] [PubMed] [Google Scholar]
- 9.Sørup CM, Jacobsen P, Forberg JL. Evaluation of emergency department performance - a systematic review on recommended performance and quality-in-care measures. Scand J Trauma Resusc Emerg Med 2013;21:62. 10.1186/1757-7241-21-62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lucas B, Schladitz P, Schirrmeister W, et al. The way from pen and paper to electronic documentation in a German emergency department. BMC Health Serv Res 2019;19:558. 10.1186/s12913-019-4400-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kulla M, Baacke M, Schöpke T, et al. Kerndatensatz „Notaufnahme“ der DIVI. Notfall Rettungsmed 2014;17:671–81. 10.1007/s10049-014-1860-9 [DOI] [Google Scholar]
- 12.Hörster AC, Kulla M, Brammen D, et al. [Potential for the survey of quality indicators based on a national emergency department registry : A systematic literature search]. Med Klin Intensivmed Notfmed 2018;113:407–17. 10.1007/s00063-016-0180-x [DOI] [PubMed] [Google Scholar]
- 13.Kulla M, Goertler M, Somasundaram R, et al. Bewertung von Qualitätsindikatoren für die Notaufnahme. Notfall Rettungsmed 2016;19:646–56. [Google Scholar]
- 14.Reiter A, Fischer B, Kötting J, et al. [QUALIFY--a tool for assessing quality indicators]. Z Arztl Fortbild Qualitatssich 2007;101:683–8. 10.1016/j.zgesun.2007.11.003 [DOI] [PubMed] [Google Scholar]
- 15.Boyd JM, Moore L, Atenafu EG, et al. A retrospective cohort study of the relationship between quality indicator measurement and patient outcomes in adult trauma centers in the United States. Injury 2017;48:13–19. 10.1016/j.injury.2016.10.040 [DOI] [PubMed] [Google Scholar]
- 16.Hörster AC, Kulla M, Bieler D, et al. [Empirical evaluation of quality indicators for severely injured patients in the TraumaRegister DGU®]. Unfallchirurg 2020;123:206–15. 10.1007/s00113-019-0699-4 [DOI] [PubMed] [Google Scholar]
- 17.Jones P, Chalmers L, Wells S, et al. Implementing performance improvement in New Zealand emergency departments: the six hour time target policy national research project protocol. BMC Health Serv Res 2012;12:45. 10.1186/1472-6963-12-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vezyridis P, Timmons S. National targets, process transformation and local consequences in an NHS emergency department (ED): a qualitative study. BMC Emerg Med 2014;14:12. 10.1186/1471-227X-14-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Staib A, Sullivan C, Griffin B, et al. Report on the 4-h rule and national emergency access target (NEAT) in Australia: time to review. Aust Health Rev 2016;40:319–23. 10.1071/AH15071 [DOI] [PubMed] [Google Scholar]
- 20.Jones P, Wells S, Harper A, et al. Impact of a national time target for ED length of stay on patient outcomes. N Z Med J 2017;130:15–34. [PubMed] [Google Scholar]
- 21.Rose L, Scales DC, Atzema C, et al. Emergency department length of stay for critical care admissions. A population-based study. Ann Am Thorac Soc 2016;13:1324–32. 10.1513/AnnalsATS.201511-773OC [DOI] [PubMed] [Google Scholar]
- 22.Vermeulen MJ, Guttmann A, Stukel TA, et al. Are reductions in emergency department length of stay associated with improvements in quality of care? A difference-in-differences analysis.}. BMJ quality {\&} safety 2016;25:489–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Suriyawongpaisal P, Kamlungkuea T, Chiawchantanakit N, et al. Relevance of using length of stay as a key indicator to monitor emergency department performance: case study from a rural hospital in Thailand. Emerg Med Australas 2019;31:646–53. 10.1111/1742-6723.13254 [DOI] [PubMed] [Google Scholar]
- 24.Boudi Z, Lauque D, Alsabri M, et al. Association between boarding in the emergency department and in-hospital mortality: a systematic review. PLoS One 2020;15:e0231253. 10.1371/journal.pone.0231253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amodio E, d'Oro LC, Chiarazzo E, et al. Emergency department performances during overcrowding: the experience of the health protection agency of Brianza. AIMS Public Health 2018;5:217–24. 10.3934/publichealth.2018.3.217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Credé SH, O'Keeffe C, Mason S, et al. What is the evidence for the management of patients along the pathway from the emergency department to acute admission to reduce unplanned attendance and admission? an evidence synthesis. BMC Health Serv Res 2017;17:355. 10.1186/s12913-017-2299-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoffmann F, Icks A. Unterschiede in Der Versichertenstruktur von Krankenkassen und deren Auswirkungen für die Versorgungsforschung: Ergebnisse des Bertelsmann-Gesundheitsmonitors. Gesundheitswesen 2012;74:291–7. 10.1055/s-0031-1275711 [DOI] [PubMed] [Google Scholar]
- 28.Andersen AA, Mühlbacher A, Nübling M. Computation of standard values for physical and mental health scale scores using the SOEP version of SF-12v2. Schmollers Jahrbuch 2007:171–82. [Google Scholar]
- 29.Grafstein E, Unger B, Bullard M, et al. Canadian emergency department information system (CEDIS) presenting complaint list (version 1.0). CJEM 2003;5:27–34. 10.1017/S1481803500008071 [DOI] [PubMed] [Google Scholar]
- 30.Brammen D, Greiner F, Dormann H, et al. Lessons learned in applying the International Society for pharmacoeconomics and outcomes research methodology to translating Canadian emergency department information system presenting complaints list into German. Eur J Emerg Med 2018;25:295–9. 10.1097/MEJ.0000000000000450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kwong E, Black N. Retrospectively patient-reported pre-event health status showed strong association and agreement with contemporaneous reports. J Clin Epidemiol 2017;81:22–32. 10.1016/j.jclinepi.2016.09.002 [DOI] [PubMed] [Google Scholar]
- 32.Blome C, Augustin M. Measuring change in quality of life: bias in prospective and retrospective evaluation. Value Health 2015;18:110–5. 10.1016/j.jval.2014.10.007 [DOI] [PubMed] [Google Scholar]
- 33.Spronk I, Geraerds AJLM, Bonsel GJ, et al. Correspondence of directly reported and recalled health-related quality of life in a large heterogeneous sample of trauma patients. Qual Life Res 2019;28:3005–13. 10.1007/s11136-019-02256-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Swart E. Health Care Utilization Research using Secondary Data : Janssen C, Swart E, von LT, Health care utilization in Germany. New York, NY: Springer New York, 2014: 63–86. [Google Scholar]
- 35.Horenkamp-Sonntag D, Ihle P, Berghöfer A. Big data und Digitale Medizin: Datenqualität von GKV-Routinedaten für die wissenschaftliche Forschung. GuP 2017;5. [Google Scholar]
- 36.March S. Individual data linkage of survey data with claims data in Germany-An overview based on a cohort study. Int J Environ Res Public Health 2017;14. 10.3390/ijerph14121543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Swart E, Gothe H, Geyer S, et al. Gute praxis Sekundärdatenanalyse (GPS): Leitlinien und Empfehlungen. Gesundheitswesen 2015;77:120–6. [DOI] [PubMed] [Google Scholar]
- 38.Kelman S, Friedman JN. Performance improvement and performance dysfunction: an empirical examination of Distortionary impacts of the emergency room Wait-Time target in the English National health service. Journal of Public Administration Research and Theory 2009;19:917–46. 10.1093/jopart/mun028 [DOI] [Google Scholar]
- 39.Mannion R, Braithwaite J. Unintended consequences of performance measurement in healthcare: 20 salutary lessons from the English National health service. Intern Med J 2012;42:569–74. 10.1111/j.1445-5994.2012.02766.x [DOI] [PubMed] [Google Scholar]
- 40.Bedarfsgerechte Steuerung Der Gesundheitsversorgung. Available: https://www.svr-gesundheit.de/fileadmin/user_upload/Gutachten/2018/SVR-Gutachten_2018_WEBSEITE.pdf
- 41.Anderson D, Pimentel L, Golden B, et al. Drivers of ED efficiency: a statistical and cluster analysis of volume, staffing, and operations. Am J Emerg Med 2016;34:155–61. 10.1016/j.ajem.2015.09.034 [DOI] [PubMed] [Google Scholar]
- 42.Stang AS, Crotts J, Johnson DW, et al. Crowding measures associated with the quality of emergency department care: a systematic review. Acad Emerg Med 2015;22:643–56. 10.1111/acem.12682 [DOI] [PubMed] [Google Scholar]
- 43.Bobrovitz N, Lasserson DS, Briggs ADM. Who breaches the four-hour emergency department wait time target? A retrospective analysis of 374,000 emergency department attendances between 2008 and 2013 at a type 1 emergency department in England. BMC Emerg Med 2017;17:32. 10.1186/s12873-017-0145-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Khanna S, Sier D, Boyle J, et al. Discharge timeliness and its impact on hospital crowding and emergency department flow performance. Emerg Med Australas 2016;28:164–70. 10.1111/1742-6723.12543 [DOI] [PubMed] [Google Scholar]
- 45.Higginson I, Kehoe A, Whyatt J, et al. The 4-hour standard is a meaningful quality indicator: correlation of performance with emergency department crowding. Eur J Emerg Med 2017;24:25–8. 10.1097/MEJ.0000000000000417 [DOI] [PubMed] [Google Scholar]
- 46.Khalifa M, Zabani I. Developing emergency room key performance indicators: what to measure and why should we measure it? Stud Health Technol Inform 2016;226:179–82. [PubMed] [Google Scholar]
- 47.Madsen M, Kiuru S, Castrèn M, et al. The level of evidence for emergency department performance indicators. Eur J Emerg Med 2015;22:298–305. 10.1097/MEJ.0000000000000279 [DOI] [PubMed] [Google Scholar]
- 48.Wiler JL, Welch S, Pines J, et al. Emergency department performance measures updates: proceedings of the 2014 emergency department benchmarking alliance consensus Summit. Acad Emerg Med 2015;22:542–53. 10.1111/acem.12654 [DOI] [PubMed] [Google Scholar]
- 49.Gannon B, Jones C, McCabe A, et al. An economic cost analysis of emergency department key performance indicators in Ireland. Eur J Emerg Med 2017;24:196–201. 10.1097/MEJ.0000000000000347 [DOI] [PubMed] [Google Scholar]
- 50.Heuschmann PU, Biegler MK, Busse O, et al. Development and implementation of evidence-based indicators for measuring quality of acute stroke care. Stroke 2006;37:2573–2551. 10.1161/01.STR.0000241086.92084.c0 [DOI] [PubMed] [Google Scholar]
- 51.Griffey RT, Pines JM, Farley HL, et al. Chief complaint-based performance measures: a new focus for acute care quality measurement. Ann Emerg Med 2015;65:387–95. 10.1016/j.annemergmed.2014.07.453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Birnbaum LA, Rodriguez JS, Topel CH, et al. Older stroke patients with high stroke scores have delayed Door-To-Needle times. J Stroke Cerebrovasc Dis 2016;25:2668–72. 10.1016/j.jstrokecerebrovasdis.2016.07.013 [DOI] [PubMed] [Google Scholar]
- 53.NQF quality forum. Available: http://www.qualityforum.org/Measures_Reports_Tools.aspx
- 54.McClelland MS, Jones K, Siegel B, et al. A field test of time-based emergency department quality measures. Ann Emerg Med 2012;59:1–10. 10.1016/j.annemergmed.2011.06.013 [DOI] [PubMed] [Google Scholar]
- 55.IQTIG Beschreibung Der Qualitätsindikatoren für das Erfassungsjahr 2017 2018.
- 56.Jones P, Harper A, Wells S, et al. Selection and validation of quality indicators for the shorter stays in emergency departments national research project. Emerg Med Australas 2012;24:303–12. 10.1111/j.1742-6723.2012.01546.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.