Abstract
Objective
In this study, the authors analyzed the status of anxiety depression and insomnia symptoms and influential factors in the work resumption period of Coronavirus disease 2019 (COVID-19).
Methods
A multicenter cross-sectional survey was conducted from March 2, 2020 to March 8, 2020 in Shandong Province, China, using quota sampling combined with snowball sampling. The Generalized Anxiety Disorder-7 (GAD-7), the Patient Health Questionnaire-9 (PHQ-9), and the Insomnia Severity Index (ISI) were used to assess the anxiety, depression, and insomnia symptoms. The multivariate logistic regression analysis was used to explore the influential factors.
Results
A total of 4000 invitations were sent from three centers, 3237 valid questionnaires were received. Based on GAD-7, PHQ-9, and ISI scales, 19.5%–21.7% of the participants had anxiety, depression, or insomnia symptoms; 2.9%–5.6% had severe symptoms. Besides, 2.4%, 4.8%, and 4.5% of the participants had anxiety-depression, anxiety-insomnia, or depression-insomnia combined symptoms. The scores of anxiety and insomnia symptoms, along with scores of depression and insomnia symptoms were positively correlated in these samples. Aged 50–64 years and outside activities once in ≥30 days were risk factors of anxiety, depression, and insomnia symptoms in common. During the epidemic, 17.4% of the participants had received psychological interventions, and only 5.2% had received individual interventions.
Conclusions
The incidence of psychological distress increased during the outbreak of COVID-19 in the work resumption period than the normal period. Current psychological interventions were insufficient; target psychological interventions should be conducted in time.
Keywords: Anxiety, Depression, Insomnia, COVID-19, Cross-sectional study
Highlights
-
•
An analysis of psychological status in the work resumption period of COVID-19.
-
•
A cross-sectional study of people under multiple stress during an epidemic.
-
•
Totally 19.5%–21.7% participants had anxiety, depression, or insomnia symptoms.
-
•
Several factors were found associated with psychological and sleep problems.
-
•
The current psychological interventions were insufficient.
1. Introduction
The outbreak of Coronavirus disease 2019 (COVID-19) became a global health threat in early 2020 [1,2]. The COVID-19 was highly infectious and fatal to some patients [3]. So far, there was no specific remedy [4]. To control the spread of COVID-19, the Chinese government implemented a strict restriction on outdoor activities from the Spring Festival [5]. By the late February 2020, the epidemic was effectively controlled in mainland China [6]. On February 21, 2020, the State Council of the P.R.C. published a guideline for the prevention and control of COVID-19 during the work resumption period, which announced the permission of work resumption [7]. As the epidemic has not been completely resolved [8], the work resumption procedure was gradually conducted and cross-regional activities were still restricted. The panic caused by the epidemic, the communication reduction caused by interpersonal isolation, and the economic impact caused by production suspension can trigger the stress response, which may induce psychological distress even mental illness [[9], [10], [11], [12], [13]]. Previous studies suggested that the Severe Acute Respiratory Syndrome (SARS), the Middle East Respiratory Syndrome (MERS), and the Ebola virus disease (Ebola) epidemics had serious psychological influences to a wide range of people [[14], [15], [16]]. It is necessary to conduct target psychological intervention timely and effectively to prevent psychological distress from worsening.
Although previous studies conducted some investigations of the psychological status during the outbreak of COVID-19, there was limited analysis of the psychological status and influential factors in the work resumption period [10,17,18], and this is a global research gap for COVID-19 research [19]. In the work resumption period, different resumption status and economic pressure may cause different psychological problems. Therefore, we conducted the present study based on multicenter collaboration to analyzed the anxiety, depression, and insomnia symptoms and influential factors in the work resumption period of COVID-19 epidemic, which can provide a reference for further psychological intervention.
2. Material and methods
2.1. Study population and sampling process
The present study was a multicenter cross-sectional study approved by the SanBo Brain Hospital, Capital Medical University ethics committee. Because of the limitation of face-to-face contacts, all participants or their guardians provided informed consent by clicking an “agree to the consent” button online (for online questionnaire) or providing oral consent (for telephone review). A previous study of the research team has been published for the psychological status of China in the outbreak period of COVID-19 [20]. Because of the epidemic situation, a follow-up study was difficult to achieve. The present study is another cross-sectional study to further explore the changes of psychological status and risk factors in the work resumption period of COVID-19.
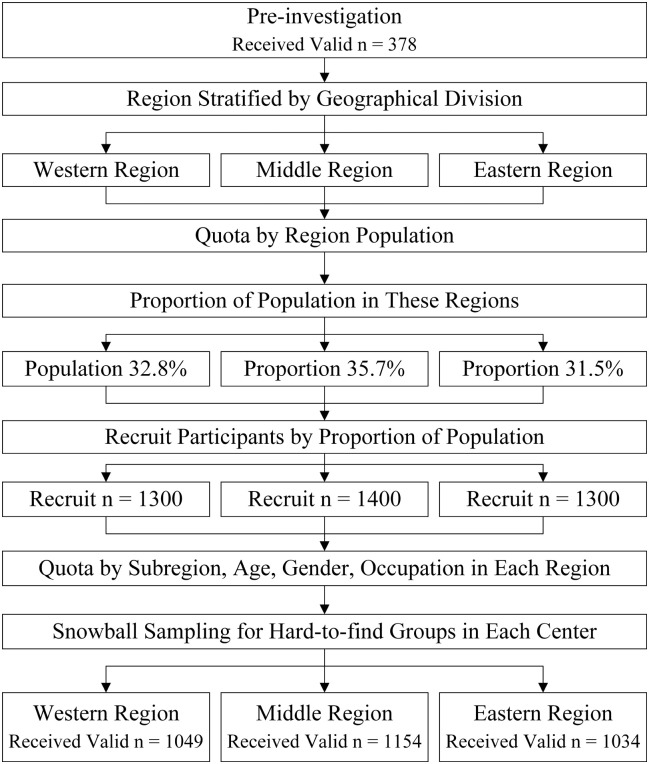
The sampling location was Shandong Province, China. Shandong Province located in eastern China. By the end of 2017, a total of 100.58 million people lived in Shandong Province, accounting for about one-fourteenth of the Chinese population [21]. When the resumption of work began on February 21, 2020, a total of 750 confirmed, 293 cured and 4 died patients were reported in Shandong Province [22]. After established the proposal, we stratified Shandong Province into three regions (western, middle, and eastern) according to the geographical division. We established one collaboration center in each area to conduct investigations (total of three centers). Fig. 1 shows the location of Shandong Province and regional division.
Fig. 1.
A sketch map of the location of Shandong Province (sampling location) and regional division.
Participants were included in the study if they met the following inclusion criteria: (1) lived in Shandong Province, China, during the outbreak of COVID-19; (2) aged no less than 11 years (the scales used are not validated for individuals aged under 11 [23]). People were excluded if they refused to participate. The Generalized Anxiety Disorder-7 scale (GAD-7, Cronbach's α = 0.90) [24], the Patient Health Questionnaire-9 (PHQ-9, Cronbach's α = 0.86) [25], and the Insomnia Severity Index (ISI, Cronbach's α = 0.83) [26] were used to measure anxiety, depression, and insomnia symptoms.
The present study consisted of a pre-investigation and a formal investigation. The pre-investigation was launched from February 24, 2020 (next week after the permission of work resumption [7]) to February 26, 2020. The objectives of the pre-investigation were to foster multicenter collaboration, to assess sampling procedure, to examine the accessibility of the questionnaire, and to determine the sample size of the formal investigation. The three collaboration centers sent a total of 450 invitations (150 for each center) and received 378 (84.0%) valid questionnaires. The proportion of participants with anxiety, depression, or insomnia symptoms was 19.2–21.0%. Based on the pre-investigation, the permissible error was set as 0.03 and the drop-out rate was set as 20.0%. The Clopper-Pearson formula for two-sided confidence intervals for one proportion was used to determine the sample size. After calculation in PASS software (NCSS LLC., Kaysville, Utah, USA; version 15), the desired dropout-inflated enrollment sample size was 3622. The number of invitations sent in the formal investigation was set as 4000.
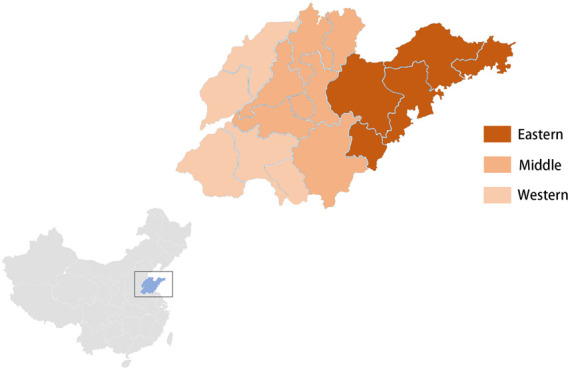
The official investigation was performed from March 2, 2020, to March 8, 2020. As cross-regional outside activities were still restricted, it was impossible to conduct a random sampling procedure by investigating from house to house. A population-based representative quota sampling method combined with a snowball sampling method was designed. First, the proportion of the population in each region was determined according to the census of Shandong Province (published in 2019, data as of the end of 2017) [21]. The quotas for invitations sent was based on the proportion of population in these three regions (western region (western center): n = 1300; middle region (middle center): n = 1400; eastern region (eastern center): n = 1300). Second, a cross-control quota sampling procedure for characteristics of the population (subregion, age, gender, occupation) in each region was conducted. Third, based on the quotas, each center judged the sampling group, sent invitations, and recruited participants who were willing to join. For samples that were so hard to find (such as confirmed patients, the elderly, et al.) that the sampling center could not collect required enough people with the required characteristics, the center then conducted a snowball sampling procedure as a supplement. Participants recruited were given an online unified questionnaire or a telephone survey (for people who cannot answer online, such as elderly; the content is consistent with the online questionnaires). All participants were required to answer only once through one review method. A detailed description of the similar sampling method has been published elsewhere [20]. Fig. 2 shows the sampling process.
Fig. 2.
Flow diagram showing the sampling process.
2.2. Measures
The questionnaire consisted of three parts. The first part collected characteristics, including region, age, gender, education, marriage status, and occupation. The second part concerned the experience related to the COVID-19 epidemic, including similar experience (SARS, an outbreak in 2003; H1N1 flu, an outbreak in 2009), current epidemic status (cured, confirmed, suspected infected, close contacts, frontline medical staff, non-contacts), outside activity during the outbreak of COVID-19 (1–7 days for once, 8–14 days for once, 15–29 days for once, 30 days or more for once), resumption status (on-site, off-site, or no work or study resumption), health education of COVID-19 (public, individual), psychological intervention during the COVID-19 (public, individual). The third part was standardized scales, including GAD-7, PHQ-9, and ISI, to assess anxiety, depression, and insomnia symptoms. Participants were required to respond based on the experiences of the past two weeks. The suitable classification standards of these three scales were determined by the Chinese consensus reviewed by psychologists. The GAD-7, PHQ-9, and ISI score ≥ 10, 10, 15 indicate anxiety, depression, and insomnia symptoms; scores ≥15, 15, 22 indicate severe anxiety, severe depression, and severe insomnia symptoms. For participants aged under 18, total scores ≥11 points in PHQ-9 is consider to have depression symptoms [27]. At the end of the questionnaire, a trust question was set as “did you answer truthfully”. Questionnaires with “No” response in the trust question, the abnormal response time (i.e. less than 1 min or more than 12 h), or incomplete questionnaires would be marked as invalid, which would not be included in the final analysis. Participants accepted recruitment but responded in invalid surveys were viewed as “drop-out samples”.
2.3. Statistical analysis
All statistical analyses were performed using the SPSS software package (IBM, Armonk, New York, USA; version 26). The influential factors of anxiety, depression and insomnia symptoms were analyzed by logistic regression. The division of ages was consistent with the Chinese epidemiology study of mental disorders by Huang et al. [28] in the normal period and the cross-sectional study of psychological status by Wang et al. [20] in the outbreak of COVID-19 to set as contracts. Variables showing a P-value of <0.10 in the univariate analysis (Pearson x 2 or Fisher exact test) were then entered into a multivariate logistic regression analysis with a backward method. The OR value and its 95% confidence interval (95%CI) were given for independent factors, and the OR value >1 indicated risk factors. Besides, after the GAD-7, PHQ-9, and ISI scores of the participants were tested for normality (Kolmogorov-Smirnov test), Pearson's correlation analysis was performed to explorer the correlation of scores. A P value of <0.05 was considered statistically significant.
3. Results
3.1. Characteristics of the participants
A total of 3237 valid questionnaires were received (western region: n = 1049, middle region: n = 1154, eastern region: n = 1034) from 4000 invitations. The actual drop-out rate was 19.1%. Of the drop-out samples, 267 did not provide consent, 181 did not complete the full questionnaire, 193 did not pass the trust question, and 122 answered in too short or too long response times. The included participants were aged 11–83 years with a median of 37 (IQR 22–55); 52.9% (1713) of them were male and 47.1% (1524) were female. The basic characteristic of participants (gender, age, regional sample size) did not have a significant statistical difference with the proposal and the census of Shandong Province [21] (P > 0.05). A total of 76 (2.4%) cured patients, 15 (0.5%) confirmed patients, 218 (6.7%) close contacts, 269 (8.3%) frontline medical staff, and 2659 (82.1%) non-contacts completed valid questionnaires. No sample of the suspected case was collected because there was no existing or new suspected case in the sampling area during the investigation. The overall work or study resumption proportion was 69.9% (2263), 31.5% (1019) resumed work on-site. Because all schools in the sampling area were not allowed to resume on-site study during the investigation, no on-site study resumption sample was collected. During the outbreak of COVID-19, 94.7% (3065) of the participants had received health education about the epidemic. However, only 17.4% (562) of the participants had received psychological interventions, 5.2% had received individual psychological interventions. Table 1 shows the participants' characteristics and experiences related to the COVID-19 epidemic.
Table 1.
Participants' characteristics and experiences (n = 3237).
| Subject | n | % |
|---|---|---|
| Region | ||
| Western | 1049 | 32.4 |
| Middle | 1154 | 35.7 |
| Eastern | 1034 | 31.9 |
| Gender | ||
| Male | 1713 | 52.9 |
| Female | 1524 | 47.1 |
| Age, y | ||
| <18 | 597 | 18.4 |
| 18–34 | 823 | 25.4 |
| 35–49 | 739 | 22.8 |
| 50–64 | 651 | 20.1 |
| >64 | 427 | 13.2 |
| Education | ||
| Junior and lower | 1106 | 34.2 |
| Senior | 1089 | 33.6 |
| University and higher | 1042 | 32.2 |
| Marriage | ||
| Unmarried | 994 | 30.7 |
| Married | 2031 | 62.7 |
| Divorced | 212 | 6.6 |
| Current location | ||
| City | 2305 | 71.2 |
| Rural | 932 | 28.8 |
| Occupation | ||
| Student | 849 | 26.2 |
| Public institutions | 583 | 18.0 |
| Business and industry | 729 | 22.5 |
| Farmer | 561 | 17.3 |
| Freelance, part-time, or no occupation | 515 | 15.9 |
| Similar memory | ||
| SARS | 891 | 27.5 |
| H1N1 | 703 | 21.7 |
| Both | 765 | 23.6 |
| None | 878 | 27.1 |
| Epidemic status* | ||
| Cured | 76 | 2.4 |
| Confirmed | 15 | 0.5 |
| Close contacts | 218 | 6.7 |
| Frontline medical staff | 269 | 8.3 |
| Non contacts | 2659 | 82.1 |
| Outside activity/ once | ||
| 1–7 days | 1285 | 39.7 |
| 8–14 days | 795 | 24.6 |
| 15–29 days | 672 | 20.8 |
| ≥ 30 days | 485 | 15.0 |
| Resumption status** | ||
| On-site work resumption | 1019 | 31.5 |
| Off-site work resumption | 630 | 19.5 |
| Off-site study resumption | 614 | 19.0 |
| No work resumption | 739 | 22.8 |
| No study resumption | 235 | 7.3 |
| Health education | ||
| Public | 1504 | 46.5 |
| Individual | 465 | 14.4 |
| Both | 1096 | 33.9 |
| None | 172 | 5.3 |
| Psychological intervention | ||
| Public | 393 | 12.1 |
| Individual | 42 | 1.3 |
| Both | 127 | 3.9 |
| None | 2675 | 82.6 |
SARS: Severe Acute Respiratory Syndrome, an outbreak in 2003; H1N1: H1N1 Flu, an outbreak in 2009; ⁎No sample of the suspected case was collected because there was no existing or new suspected case in the sampling area during the investigation; ⁎⁎Because all schools in the sampling area were not allowed to conduct on-site study resumption during the investigation, no on-site study resumption sample was collected.
3.2. Anxiety, depression, and insomnia symptoms
According to the GAD-7, PHQ-9, and ISI scales, 20.8% (674) of the participants had anxiety symptoms, 19.5% (631) had depression symptoms, and 21.7% (702) had insomnia symptoms. The proportions of participants with severe anxiety, severe depression, or severe insomnia symptoms were 4.4% (143), 2.9% (95), and 5.6% (182). Besides, 2.4% (78), 4.8% (155), and 4.5% (146) of participants had anxiety-depression, anxiety-insomnia, or depression-insomnia combined symptoms. After Pearson's correlation analysis, the scores of anxiety and insomnia symptoms, along with scores of depression and insomnia symptoms were positively correlated in these samples (r = 0.719, P = 0.001; r = 0.698, P = 0.003). The correlation between scores of anxiety and depression symptoms did not reach statistical significance (r = 0.621, P = 0.06).
3.3. Influential factors
For exploration of factors associated with anxiety symptoms, univariate analysis revealed that age, occupation, outside activities and resumption status had P values <0.10. These subjects were entered into multivariate analysis. After multivariate analysis, aged 50–64 years (OR = 2.21, 95%CI: 1.41–2.76, P = 0.01), public institution occupations (OR = 1.87, 95%CI: 1.29–2.92, P = 0.01), business and industry occupations (OR = 2.63, 95%CI: 1.71–3.85, P = 0.008), outside activities once in ≥30 days (OR = 3.18, 95%CI: 1.82–4.51, P < 0.001) and off-site work resumption (OR = 2.26, 95%CI: 1.44–2.96, P = 0.03) were independent risk factors of anxiety symptoms (Table 2 ).
Table 2.
Multivariate logistic regression to identify independent factors associated with anxiety symptoms (GAD-7 scale).
| Subject | Variable | OR | 95% CI | P |
|---|---|---|---|---|
| Age, y | <18 | 1 | – | – |
| 18–34 | 1.03 | 0.52–1.82 | 0.33 | |
| 35–49 | 1.37 | 0.73–1.92 | 0.12 | |
| 50–64 | 2.21 | 1.41–2.76 | 0.01* | |
| >64 | 1.60 | 0.91–2.87 | 0.08 | |
| Occupation | Student | 1 | – | – |
| Public institutions | 1.87 | 1.29–2.92 | 0.01* | |
| Business and industry | 2.63 | 1.71–3.85 | 0.008** | |
| Farmer | 1.41 | 0.85–2.27 | 0.06 | |
| Freelance, part-time, or no occupation | 1.54 | 0.97–2.06 | 0.06 | |
| Outside activity/ once | 1–7 days | 1 | – | – |
| 8–14 days | 1.18 | 0.73–1.86 | 0.20 | |
| 15–29 days | 1.91 | 0.93–3.11 | 0.05 | |
| ≥ 30 days | 3.18 | 1.82–4.51 | <0.001** | |
| Resumption status | On-site work resumption | 1 | – | – |
| Off-site work resumption | 2.26 | 1.44–2.96 | 0.03* | |
| Off-site study resumption | 0.74 | 0.50–1.49 | 0.11 | |
| No work resumption | 1.46 | 0.93–2.09 | 0.19 | |
| No study resumption | 1.55 | 0.96–2.28 | 0.15 |
Adjusted for all other variables. GAD-7: the Generalized Anxiety Disorder-7 scale; ⁎P < 0.05 (Multivariate logistic regression); ⁎⁎P < 0.01 (Multivariate logistic regression).
Age, gender, occupation, outside activities and resumption status had P values <0.10 in the univariate analysis of factors associated with depression symptoms. Multivariate analysis revealed that aged 50–64 years (OR = 2.65, 95%CI: 1.76–3.72, P = 0.002), aged >64 years (OR = 1.79, 95%CI: 1.19–2.55, P = 0.02), outside activities once in 15–29 days (OR = 2.12, 95%CI: 1.33–3.23, P = 0.02), and outside activities once in ≥30 days (OR = 3.37, 95%CI: 2.03–4.98, P < 0.001) were independent risk factors of depression symptoms (Table 3 .).
Table 3.
Multivariate logistic regression to identify independent factors associated with depression symptoms (PHQ-9 scale).
| Subject | Variable | OR | 95% CI | P |
|---|---|---|---|---|
| Age, y | <18 | 1 | – | – |
| 18–34 | 1.46 | 0.92–2.89 | 0.06 | |
| 35–49 | 1.72 | 0.94–2.96 | 0.05 | |
| 50–64 | 2.65 | 1.76–3.72 | 0.002** | |
| >64 | 1.79 | 1.19–2.55 | 0.02* | |
| Gender | Male | 1 | – | – |
| Female | 0.85 | 0.58–1.74 | 0.13 | |
| Occupation | Student | 1 | – | – |
| Public institutions | 1.78 | 0.93–2.85 | 0.13 | |
| Business and industry | 1.89 | 0.97–2.90 | 0.06 | |
| Farmer | 1.44 | 0.84–1.92 | 0.20 | |
| Freelance, part-time, or no occupation | 1.77 | 0.94–2.81 | 0.06 | |
| Outside activity/ once | 1–7 days | 1 | – | – |
| 8–14 days | 1.85 | 0.90–2.42 | 0.17 | |
| 15–29 days | 2.12 | 1.33–3.23 | 0.02* | |
| ≥ 30 days | 3.37 | 2.03–4.98 | <0.001** | |
| Resumption status | On-site work resumption | 1 | – | – |
| Off-site work resumption | 1.67 | 0.92–2.73 | 0.07 | |
| Off-site study resumption | 0.74 | 0.47–1.33 | 0.16 | |
| No work resumption | 2.13 | 0.93–3.70 | 0.06 | |
| No study resumption | 0.89 | 0.62–1.91 | 0.19 |
Adjusted for all other variables. PHQ-9: the Patient Health Questionnaire-9; ⁎P < 0.05 (Multivariate logistic regression); ⁎⁎P < 0.01 (Multivariate logistic regression).
The univariate analysis of factors associated with insomnia symptoms showed that age, occupation, outside activities, resumption status, and psychological intervention had P values <0.10. The multivariate analysis showed that aged 50–64 years (OR = 2.46, 95%CI: 1.45–3.64, P = 0.009), business and industry occupations (OR = 2.62, 95%CI: 1.56–3.76, P = 0.005), outside activities once in ≥30 days (OR = 3.13, 95%CI: 1.84–4.80, P < 0.001), and off-site work resumption (OR = 2.29, 95%CI: 1.32–3.38, P = 0.01) were independent risk factors of insomnia symptoms (Table 4 .).
Table 4.
Multivariate logistic regression to identify independent factors associated with insomnia symptoms (ISI scale).
| Subject | Variable | OR | 95% CI | P |
|---|---|---|---|---|
| Age, y | <18 | 1 | – | – |
| 18–34 | 1.34 | 0.89–2.20 | 0.10 | |
| 35–49 | 1.57 | 0.92–2.41 | 0.08 | |
| 50–64 | 2.46 | 1.45–3.64 | 0.009** | |
| >64 | 1.83 | 0.97–2.92 | 0.06 | |
| Occupation | Student | 1 | – | – |
| Public institutions | 1.74 | 0.98–3.26 | 0.05 | |
| Business and industry | 2.62 | 1.56–3.76 | 0.005** | |
| Farmer | 1.23 | 0.80–1.83 | 0.22 | |
| Freelance, part-time, or no occupation | 1.61 | 0.86–2.60 | 0.17 | |
| Outside activity/ once | 1–7 days | 1 | – | – |
| 8–14 days | 1.35 | 0.93–1.91 | 0.07 | |
| 15–29 days | 2.06 | 0.95–3.73 | 0.06 | |
| ≥ 30 days | 3.13 | 1.84–4.80 | <0.001** | |
| Resumption status | On-site work resumption | 1 | – | – |
| Off-site work resumption | 2.29 | 1.32–3.38 | 0.01* | |
| Off-site study resumption | 0.82 | 0.42–1.45 | 0.14 | |
| No work resumption | 1.83 | 0.98–2.75 | 0.05 | |
| No study resumption | 1.27 | 0.79–1.92 | 0.25 | |
| Psychological intervention | Public | 1 | ||
| Individual | 1.57 | 0.90–2.94 | 0.13 | |
| Both | 1.20 | 0.73–1.92 | 0.28 | |
| None | 1.89 | 0.98–2.83 | 0.06 |
Adjusted for all other variables. ISI: the Insomnia Severity Index; ⁎P < 0.05 (Multivariate logistic regression); ⁎⁎P < 0.01 (Multivariate logistic regression).
4. Discussion
4.1. Anxiety, depression, and insomnia symptoms
The wildly spread COVID-19 epidemic and strict interpersonal isolation can trigger stress response [29]. The occurrence of stressful life events is a risk factor for psychopathology, and environmental stressors also induce stable changes in gene expression within the brain that may lead to mental illnesses [30,31]. Coming into the work resumption period, many factors can become stressors of a wide range of people in a comprehensive effect, including epidemical panic, interpersonal isolation, economic volatility, and resumption status. The present study revealed that 19.5%–21.7% of the participants had anxiety, depression, or insomnia symptoms; 2.9%–5.6% had severe symptoms. According to the epidemiological report of Huang et al. on the prevalence of mental disorders in China in the normal period, the lifetime prevalence of anxiety disorders and depression disorders were 6.8% and 7.6%, which indicates the prevalence of psychological distress may get increased in the work resumption period than the normal period. An online survey [17] and another study on Chinese web users [18] suggested that one-third of people had anxiety symptoms during the outbreak of COVID-19 and the negative emotion increased. But they only focused on web users, which might limit their overall representation. A previous nationwide cross-sectional study of the research team was conducted from February 10, 2020 to February 17, 2020 (during the outbreak of COVID-19) in China with a similar design of the present study. They proposed 12.2%, 11.0%, and 13.3% of the participants had anxiety, depression, or insomnia symptoms. The proportion of anxiety, depression, and insomnia symptoms got increased the present study [20]. Wang et al. conducted a longitudinal study surveyed the general population during the initial outbreak and the epidemic's peak. They found moderate-to-severe stress, anxiety and depression were noted in 8.1%, 28.8% and 16.5% and no significant longitudinal changes [9]. Previous cross-sectional studies suggested the incidence of psychological distress might increase during the outbreak of COVID-19 in the work resumption period than the outbreak period, but current random sampling studies on psychological health during the outbreak of COVID-19 were still lacking and the sampling design and population were various. The changes in psychological distress from the outbreak of the epidemic to the work resumption period still cannot be concluded for sure, which requires further follow-up studies. Tan et al. analyzed the psychological effects of a workforce returning to work during the COVID-19 epidemic. They found 10.8% of respondents met the diagnosis of post-traumatic stress disorder (PTSD) and reported a lower prevalence of anxiety (3.8%), depression (3.7%), stress (1.5%) and insomnia (2.3%). They suggested returning to work had not caused a high level of psychiatric symptoms in the workforce and assumed it was the effects of psychological measures [10]. In the present studies, we analyzed people who had different occupations and found occupations with high-risk of psychological distress. We also found people who had different occupations accepted similar proportion of psychological interventions (p = 0.33), suggesting these differences in psychological distress might relate to the characteristics of different occupations, which needs further explorations. As the purpose of the present study was to explore the psychological status of general population, we included some samples who did not belong to workforce (e.g. 26.2% were students). This might introduce heterogeneity when comparing to studies focus on Chinese workforce or other particular groups and influence the comparability.
Besides, the present study also showed that 2.4%, 4.8%, and 4.5% of participants had anxiety-depression, anxiety-insomnia, or depression-insomnia combined symptoms. The scores of anxiety and insomnia symptoms (r = 0.719), along with scores of depression and insomnia symptoms (r = 0.698) were positively correlated in these samples. Previous studies suggested that environmental stressors or physiological disease might cause the comorbidity of anxiety, depression, or insomnia, which could provide a great challenge in the diagnosis and intervention [32,33]. The comorbidity of anxiety and depression could make psychological distress worse and reduce treatment response, which should be considered [34]. Sleep disturbance is a common manifestation of anxiety and depression. Insomnia has been identified as a predictor of multiple mental disorders and could increase the risk for psychopathology [35]. Efforts should be made to strengthen interventions for sleep problems such as cognitive behavior therapy and mindfulness-based therapy [36].
4.2. Influential factors
This study also analyzed the risk factors for anxiety, depression, and insomnia symptoms, which could indicate the target group for interventions. After multivariate analysis, aged 50–64 years (OR = 2.21), public institution occupations (OR = 1.87), business and industry occupations (OR = 2.63), outside activities once in ≥30 days (OR = 3.18) and off-site work resumption (OR = 2.26) were independent risk factors of anxiety symptoms; aged 50–64 years (OR = 2.65), aged >64 years (OR = 1.79), outside activities once in 15–29 days (OR = 2.12), and outside activities once in ≥30 days (OR = 3.37) were independent risk factors of depression symptoms; aged 50–64 years (OR = 2.46), business and industry occupations (OR = 2.62), outside activities once in ≥30 days (OR = 3.13), and off-site work resumption (OR = 2.29) were independent risk factors of insomnia symptoms. Generally, aged 50–64 years and outside activities once in ≥30 days were risk factors of anxiety, depression, and insomnia symptoms in common.
According to an epidemiological study of mental disorders, Chinese aged 50–64 years had a higher incidence of mental illness than the other age groups [28], which may explain the higher prevalence of anxiety, depression, and insomnia symptoms in participants aged 50–64 years in the present study. Furthermore, in China, many middle-aged and elderly people are in leadership positions in companies and families. The economic stress caused by the epidemic and work resumption could influence their mental health [37]. Therefore, middle-aged and elderly people, especially aged 50–64 years, are easier to have psychological distress that needs interventions. In addition, the previous study of Wang et al. suggested participants aged 35–49 years had more severe anxiety, depression, and insomnia symptoms during the outbreak of COVID-19 [20]. This change in the high-risk age groups might be the combined influence of economic and epidemic pressure changes with time, which needs further exploration. Affected by the COVID-19 epidemic, a wide range of people reduced unnecessary outside activities and interpersonal communication, some of them even stayed home alone for a long time. In the present study, 15.0% of the participants had outside activities once in ≥30 days. Previous studies suggested that the interpersonal isolation of patients had a significant impact on mental health [38]. With further control of COVID-19, more and more people can restore interpersonal contacts and resume normal work in the future. The psychological distress may get released in some people. However, interpersonal isolation has a long-term influence on mental health, some people with psychological distress cannot relieve by himself, even after resuming interpersonal contacts [38]. Target psychological interventions should be performed in time to people under long-term interpersonal isolation before and after work resumption. In addition, several previous studies concerned the healthcare workers had a higher risk of psychological symptoms [12,13,20]. The present study did not find being frontline medical staff was a risk factor of psychological distress, which might relate to the effectively control of the epidemic, lower proportion of confirmed patients, higher proportion of accepting psychological interventions for these group, and higher proportion of recovering patients. However, more attention should also be paid to timely identification and intervention of PTSD for healthcare workers [10].
4.3. Psychological interventions
In the present study, only 17.4% of current participants had received psychological interventions, 5.2% had received individual psychological interventions during the outbreak of COVID-19. Compared with a previous study (1.9% received counseling during the outbreak) [20], the proportion of people received psychological interventions was higher. But it was still insufficient for the potential proportion of people with psychological distress. The outbreak of COVID-19 limited face-to-face counseling and individualized psychological interventions, which was a serious challenge to the mental health service. Besides, there were still many people who did not pay enough attention to mental health [39]. Irvine et al. suggested that there was no significant difference between online or telephone psychological therapy and face-to-face psychological intervention in efficacy and detrimental effects [40]. Besides, community interventions by Internet or telephone and app-supported smartphone interventions also showed advantages in promoting mental health [41,42] such as Internet-based cognitive behavior therapy [43]. However, some studies concerned that non-face-to-face psychological interventions might have defects in reliability and individualized treatment [40,44]. We suggest that under the current circumstances, individualized psychological interventions are still important for high-risk groups, and the others should adopt public psychological education. As the outbreak of COVID-19 has not been completely resolved, online or telephone interventions can be chosen as preferred. When the epidemic is under control, individualized face-to-face psychological interventions should be resumed in time to improve people's mental health and prevent psychological distress from worsening. Furthermore, providing accurate health information is important for epidemic control, health education, and psychological interventions [17]. It is essential to mobilize existing resources and provide accurate health information to satisfy demand [45,46], as well as effective management for at-risk workplaces to efficiently detect early signs of localized transmissions [47], identify infected areas and effectively quarantine them [48].
4.4. Limitations
As cross-regional outside activities were still restricted, it was impossible to conduct a random sampling procedure by investigating from house to house. Although the present study designed a population-based representative quota sampling method combined with a snowball sampling method, nonprobability sampling has inherent limitations in representing the entire population. The present study was to explore the psychological status of general population, we included some samples who did not belong to workforce (e.g. 26.2% were students). Because the sampling design and population were various, the comparation of previous cross-sectional studies might introduce heterogeneity. After the epidemic is under control, further researches with random sampling and follow-up studies should be carried out. Besides, the scales used in the present study were only screening assessments and the further diagnosis of mental illness should be made by qualified psychiatrists.
5. Conclusions
The present study suggested that 19.5%–21.7% of the participants had anxiety, depression, or insomnia symptoms; 2.9%–5.6% had severe symptoms. The incidence of psychological distress increased in the work resumption period of COVID-19 epidemic than the normal period. Besides, 2.4%, 4.8%, and 4.5% of participants had anxiety-depression, anxiety-insomnia, or depression-insomnia combined symptoms. The scores of anxiety and insomnia symptoms, along with scores of depression and insomnia symptoms were positively correlated in these samples. Aged 50–64 years and outside activities once in ≥30 days were risk factors of anxiety, depression, and insomnia symptoms in common. During the epidemic, 17.4% of the participants had received psychological interventions, and only 5.2% had received individual interventions. Current psychological interventions were not sufficient; target psychological interventions should be conducted in time.
Declarations of Competing Interest
None.
Research ethics
The SanBo Brain Hospital, Capital Medical University ethics committee approved this study. Because of the limitation of face-to-face contacts, all participants or their guardians provided informed consent by clicking an “agree to the consent” button online (for online questionnaire) or providing oral consent (for telephone review). This study was conducted following the 1964 Helsinki Declaration and its later amendments.
Funding
No funding was received for this study.
Author contributions
Collecting data: Yuan Zhang, Shu Wang, Wei Ding, Yao Meng, Huiting Hu, Zhenhua Liu, Xianwei Zeng, Yuguang Guan, Minzhong Wang.
Mathematical calculation: Yuan Zhang, Shu Wang, Minzhong Wang.
Preparing manuscript: Yuan Zhang, Shu Wang, Wei Ding, Yao Meng, Huiting Hu, Yuguang Guan.
Revision manuscript: Zhenhua Liu, Xianwei Zeng, Yuguang Guan, Minzhong Wang.
Supervision: Minzhong Wang.
Acknowledgments
None.
References
- 1.Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y., Qiu Y., Wang J., Liu Y., Wei Y., Xia J.A., Yu T., Zhang X., Zhang L. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395(10223):507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tian S., Hu N., Lou J., Chen K., Kang X., Xiang Z., Chen H., Wang D., Liu N., Liu D., Chen G., Zhang Y., Li D., Li J., Lian H., Niu S., Zhang L., Zhang J. Characteristics of COVID-19 infection in Beijing. J. Inf. Secur. 2020;80(4):401–406. doi: 10.1016/j.jinf.2020.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rothan H.A., Byrareddy S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020;109 doi: 10.1016/j.jaut.2020.102433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55(3) doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National-Health-Commission-of-the-P.R.C Notice on strengthening community prevention and control of Coronavirus disease (in Chinese) 2020. 2020. http://www.nhc.gov.cn/xcs/zhengcwj/202001/dd1e502534004a8d88b6a10f329a3369.shtml
- 6.Kraemer M.U.G., Yang C.H., Gutierrez B., Wu C.H., Klein B., Pigott D.M., du Plessis L., Faria N.R., Li R., Hanage W.P., Brownstein J.S., Layan M., Vespignani A., Tian H., Dye C., Pybus O.G., Scarpino S.V. The effect of human mobility and control measures on the COVID-19 epidemic in China. Science. 2020;368(6490):493–497. doi: 10.1126/science.abb4218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The-State-Council-of-the-P.R.C., Guidelines for the prevention and control of Coronavirus disease during in the work resumption period (in Chinese), 2020. http://www.gov.cn/gongbao/content/2020/content_5488911.htm. (Accessed February 22 2020).
- 8.Remuzzi A., Remuzzi G. COVID-19 and Italy: what next? Lancet. 2020;395(10231):1225–1228. doi: 10.1016/S0140-6736(20)30627-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K., Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tan W., Hao F., McIntyre R.S., Jiang L., Jiang X., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Zhang Z., Lai A., Ho R., Tran B., Ho C., Tam W. Is returning to work during the COVID-19 pandemic stressful? A study on immediate mental health status and psychoneuroimmunity prevention measures of Chinese workforce. Brain Behav. Immun. 2020;87:84–92. doi: 10.1016/j.bbi.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Jiang X., McIntyre R.S., Tran B., Sun J., Zhang Z., Ho R., Ho C., Tam W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020;87:100–106. doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chew N.W.S., Lee G.K.H., Tan B.Y.Q., Jing M., Goh Y., Ngiam N.J.H., Yeo L.L.L., Ahmad A., Ahmed Khan F., Napolean Shanmugam G., Sharma A.K., Komalkumar R.N., Meenakshi P.V., Shah K., Patel B., Chan B.P.L., Sunny S., Chandra B., Ong J.J.Y., Paliwal P.R., Wong L.Y.H., Sagayanathan R., Chen J.T., Ying Ng A.Y., Teoh H.L., Tsivgoulis G., Ho C.S., Ho R.C., Sharma V.K. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tan B.Y.Q., Chew N.W.S., Lee G.K.H., Jing M., Goh Y., Yeo L.L.L., Zhang K., Chin H.K., Ahmad A., Khan F.A., Shanmugam G.N., Chan B.P.L., Sunny S., Chandra B., Ong J.J.Y., Paliwal P.R., Wong L.Y.H., Sagayanathan R., Chen J.T., Ng A.Y.Y., Teoh H.L., Ho C.S., Ho R.C., Sharma V.K. Psychological impact of the COVID-19 pandemic on health Care Workers in Singapore. Ann. Intern. Med. 2020;173(4):317–320. doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chua S.E., Cheung V., McAlonan G.M., Cheung C., Wong J.W.S., Cheung E.P.T., Chan M.T.Y., Wong T.K.W., Choy K.M., Chu C.M., Lee P.W.H., Tsang K.W.T. Stress and psychological impact on SARS patients during the outbreak. Can. J. Psychiatry. 2016;49(6):385–390. doi: 10.1177/070674370404900607. [DOI] [PubMed] [Google Scholar]
- 15.Kim H.-C., Yoo S.-Y., Lee B.-H., Lee S.H., Shin H.-S. Psychiatric findings in suspected and confirmed Middle East respiratory syndrome patients quarantined in hospital: a retrospective chart analysis. Psychiatry Investig. 2018;15(4):355–360. doi: 10.30773/pi.2017.10.25.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kelly J.D., Hoff N.A., Spencer D.A., Musene K., Bramble M.S., McIlwain D., Okitundu D., Porco T.C., Rutherford G.W., Glymour M.M., Bjornson Z., Mukadi P., Okitolonda-Wemakoy E., Nolan G.P., Muyembe-Tamfum J.J., Rimoin A.W. Neurological, cognitive, and psychological findings among survivors of Ebola virus disease from the 1995 Ebola outbreak in Kikwit, Democratic Republic of Congo: a cross-sectional study. Clin. Infect. Dis. 2019;68(8):1388–1393. doi: 10.1093/cid/ciy677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li S., Wang Y., Xue J., Zhao N., Zhu T. The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. Int. J. Environ. Res. Public Health. 2020;17(6) doi: 10.3390/ijerph17062032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tran B.X., Ha G.H., Nguyen L.H., Vu G.T., Hoang M.T., Le H.T., Latkin C.A., Ho C.S.H., Ho R.C.M. Studies of novel coronavirus disease 19 (COVID-19) pandemic: a global analysis of literature. Int. J. Environ. Res. Public Health. 2020;17(11) doi: 10.3390/ijerph17114095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wang S., Zhang Y., Ding W., Meng Y., Hu H., Liu Z., Zeng X., Wang M. Psychological distress and sleep problems when people are under interpersonal isolation during an epidemic: a nationwide multicenter cross-sectional study. Eur Psychiatry. 2020;63(1):e77. doi: 10.1192/j.eurpsy.2020.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shandong-Provincial-Bureau-of-Statistics . China Statistics Press; Beijing, China: 2019. Shandong-Investigation-Team-of-National-Bureau-of-Statistics, Shandong Statistical Yearbook 2019 (in Chinese) [Google Scholar]
- 22.Health-Commission-of-the-Shandong-Province Epidemic status of Coronavirus disease in Shandong Province on February 21, 2020 (in Chinese) 2020. http://wsjkw.shandong.gov.cn/ztzl/rdzt/qlzhfkgz/tzgg/202002/t20200222_2582373.html (Accessed February 21 2020)
- 23.Moyer D.N., Connelly K.J., Holley A.L. Using the PHQ-9 and GAD-7 to screen for acute distress in transgender youth: findings from a pediatric endocrinology clinic. J. Pediatr. Endocrinol. Metab. 2019;32(1):71–74. doi: 10.1515/jpem-2018-0408. [DOI] [PubMed] [Google Scholar]
- 24.He X.Y., Li C., Qian J., Cui H.S., Wu W.Y. Reliability and validity of a generalized anxiety scale in general hospital outpatients. Shanghai Arch. Psychiatry. 2010;22:200–203. [Google Scholar]
- 25.Wang W., Bian Q., Zhao Y., Li X., Wang W., Du J., Zhang G., Zhou Q., Zhao M. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry. 2014;36(5):539–544. doi: 10.1016/j.genhosppsych.2014.05.021. [DOI] [PubMed] [Google Scholar]
- 26.Chung K.-F., Kan K.K.-K., Yeung W.-F. Assessing insomnia in adolescents: comparison of insomnia severity index, Athens insomnia scale and sleep quality index. Sleep Med. 2011;12(5):463–470. doi: 10.1016/j.sleep.2010.09.019. [DOI] [PubMed] [Google Scholar]
- 27.Richardson L.P., McCauley E., Grossman D.C., McCarty C.A., Richards J., Russo J.E., Rockhill C., Katon W. Evaluation of the Patient Health Questionnaire-9 item for detecting major depression among adolescents. Pediatrics. 2010;126(6):1117–1123. doi: 10.1542/peds.2010-0852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huang Y., Wang Y., Wang H., Liu Z., Yu X., Yan J., Yu Y., Kou C., Xu X., Lu J., Wang Z., He S., Xu Y., He Y., Li T., Guo W., Tian H., Xu G., Xu X., Ma Y., Wang L., Wang L., Yan Y., Wang B., Xiao S., Zhou L., Li L., Tan L., Zhang T., Ma C., Li Q., Ding H., Geng H., Jia F., Shi J., Wang S., Zhang N., Du X., Du X., Wu Y. Prevalence of mental disorders in China: a cross-sectional epidemiological study. Lancet Psychiatry. 2019;6(3):211–224. doi: 10.1016/S2215-0366(18)30511-X. [DOI] [PubMed] [Google Scholar]
- 29.Li W., Yang Y., Liu Z.H., Zhao Y.J., Zhang Q., Zhang L., Cheung T., Xiang Y.T. Progression of mental health services during the COVID-19 outbreak in China. Int. J. Biol. Sci. 2020;16(10):1732–1738. doi: 10.7150/ijbs.45120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Aliri J., Muela A., Gorostiaga A., Balluerka N., Aritzeta A., Soroa G. Stressful life events and depressive symptomatology among Basque adolescents: the mediating role of attachment representations. Psychol. Rep. 2019;122(3):789–808. doi: 10.1177/0033294118771970. [DOI] [PubMed] [Google Scholar]
- 31.Uchida S., Yamagata H., Seki T., Watanabe Y. Epigenetic mechanisms of major depression: targeting neuronal plasticity. Psychiatry Clin. Neurosci. 2018;72(4):212–227. doi: 10.1111/pcn.12621. [DOI] [PubMed] [Google Scholar]
- 32.Marthoenis M., Ilyas A., Sofyan H., Schouler-Ocak M. Prevalence, comorbidity and predictors of post-traumatic stress disorder, depression, and anxiety in adolescents following an earthquake. Asian J. Psychiatr. 2019;43:154–159. doi: 10.1016/j.ajp.2019.05.030. [DOI] [PubMed] [Google Scholar]
- 33.Ngocho J.S., Watt M.H., Minja L., Knettel B.A., Mmbaga B.T., Williams P.P., Sorsdahl K. Depression and anxiety among pregnant women living with HIV in Kilimanjaro region, Tanzania. PLoS One. 2019;14(10) doi: 10.1371/journal.pone.0224515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Paavonen V., Luoto K., Lassila A., Leinonen E., Kampman O. Temperament clusters associate with anxiety disorder comorbidity in depression. J. Affect. Disord. 2018;236:252–258. doi: 10.1016/j.jad.2018.04.084. [DOI] [PubMed] [Google Scholar]
- 35.Hertenstein E., Feige B., Gmeiner T., Kienzler C., Spiegelhalder K., Johann A., Jansson-Fröjmark M., Palagini L., Rücker G., Riemann D., Baglioni C. Insomnia as a predictor of mental disorders: a systematic review and meta-analysis. Sleep Med. Rev. 2019;43:96–105. doi: 10.1016/j.smrv.2018.10.006. [DOI] [PubMed] [Google Scholar]
- 36.Ho C.S., Chee C.Y., Ho R.C. Mental health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann. Acad. Med. Singap. 2020;49(3):155–160. [PubMed] [Google Scholar]
- 37.Ouyang P., Sun W. Depression and sleep duration: findings from middle-aged and elderly people in China. Public Health. 2019;166:148–154. doi: 10.1016/j.puhe.2018.10.007. [DOI] [PubMed] [Google Scholar]
- 38.Purssell E., Gould D., Chudleigh J. Impact of isolation on hospitalised patients who are infectious: systematic review with meta-analysis. BMJ Open. 2020;10(2) doi: 10.1136/bmjopen-2019-030371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.De Sousa A., Mohandas E., Javed A. Psychological interventions during COVID-19: challenges for low and middle income countries. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Irvine A., Drew P., Bower P., Brooks H., Gellatly J., Armitage C.J., Barkham M., McMillan D., Bee P. Are there interactional differences between telephone and face-to-face psychological therapy? A systematic review of comparative studies. J. Affect. Disord. 2020;265:120–131. doi: 10.1016/j.jad.2020.01.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Castillo E.G., Ijadi-Maghsoodi R., Shadravan S., Moore E., Mensah M.O.R., Docherty M., Aguilera N.M.G., Barcelo N., Goodsmith N., Halpin L.E., Morton I., Mango J., Montero A.E., Rahmanian K.S., Bromley E., Chung B., Jones F., Gabrielian S., Gelberg L., Greenberg J.M., Kalofonos I., Kataoka S.H., Miranda J., Pincus H.A., Zima B.T., Wells K.B. Community interventions to promote mental health and social equity. Curr Psychiatry Rep. 2019;21(5):35. doi: 10.1007/s11920-019-1017-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Linardon J., Cuijpers P., Carlbring P., Messer M., Fuller-Tyszkiewicz M. The efficacy of app-supported smartphone interventions for mental health problems: a meta-analysis of randomized controlled trials. World Psychiatry. 2019;18(3):325–336. doi: 10.1002/wps.20673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhang M.W., Ho R.C. Moodle: the cost effective solution for internet cognitive behavioral therapy (I-CBT) interventions. Technol. Health Care. 2017;25(1):163–165. doi: 10.3233/THC-161261. [DOI] [PubMed] [Google Scholar]
- 44.Savic M., Dilkes-Frayne E., Carter A., Kokanovic R., Manning V., Rodda S.N., Lubman D.I. Making multiple 'online counsellings' through policy and practice: an evidence-making intervention approach. Int J Drug Policy. 2018;53:73–82. doi: 10.1016/j.drugpo.2017.12.008. [DOI] [PubMed] [Google Scholar]
- 45.Tran B.X., Dang A.K., Thai P.K., Le H.T., Le X.T.T., Do T.T.T., Nguyen T.H., Pham H.Q., Phan H.T., Vu G.T., Phung D.T., Nghiem S.H., Nguyen T.H., Tran T.D., Do K.N., Truong D.V., Vu G.V., Latkin C.A., Ho R.C.M., Ho C.S.H. Coverage of health information by different sources in communities: implication for COVID-19 epidemic response. Int. J. Environ. Res. Public Health. 2020;17(10) doi: 10.3390/ijerph17103577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Le H.T., Nguyen D.N., Beydoun A.S., Le X.T.T., Nguyen T.T., Pham Q.T., Ta N.T.K., Nguyen Q.T., Nguyen A.N., Hoang M.T., Vu L.G., Tran B.X., Latkin C.A., Ho C.S.H., Ho R.C.M. Demand for health information on COVID-19 among Vietnamese. Int. J. Environ. Res. Public Health. 2020;17(12) doi: 10.3390/ijerph17124377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tran B.X., Vu G.T., Latkin C.A., Pham H.Q., Phan H.T., Le H.T., Ho R.C.M. Characterize health and economic vulnerabilities of workers to control the emergence of COVID-19 in an industrial zone in Vietnam. Saf. Sci. 2020;129 doi: 10.1016/j.ssci.2020.104811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tran B.X., Phan H.T., Nguyen T.P.T., Hoang M.T., Vu G.T., Lei H. Thi, Latkin C.A., Ho C.S., Ho R.C. Reaching further by Village Health Collaborators: the informal health taskforce of Vietnam for COVID-19 responses. J. Glob. Health. 2020;10(1) doi: 10.7189/jogh.10.010354. [DOI] [PMC free article] [PubMed] [Google Scholar]