Abstract
Aggressive angiomyxoma is a rare mesenchymal tumor occurring usually in women of reproductive age in pelvic-perineum region. These myofibroblastic tumors rarely affect men and non-pelvic-perineum anatomical sites. There are few literature references for aggressive angiomyxoma in men. We describe a case of a 57-year old male with aggressive angiomyxoma of the scrotum and its management.
INTRODUCTION
Aggressive angiomyxoma is a rare soft tissue tumor affecting the pelvis and perineum predominantly in women. Extremely rare in men, the tumor commonly develops in the scrotum and inguinal area [1]. The exact pathogenesis is not known. We have information only from cases reports and a few case series with clinical cases and follow-up. There are no guidelines for the treatment except one proposition for their treatment [2].
CASE REPORT
A 57-year old male presented to surgery outpatient clinic of the hospital with scrotal mass. His initial review of systems was negative for any complaints except a feeling of heaviness at the scrotum. On clinical examination, the mass was mobile and did not transilluminate. The lesion had gradually increased in size during the last 2 years. The overlying skin was normal. The patient’s medical history like his family was normal. Ultrasound revealed a weak and heterogeneous echogenic mass (Fig. 1), and after the imaging with computed tomography (CT) and magnetic resonance imaging (MRI) (Figs 2 and 3) of the pelvis, we proposed surgical excision of the mass. Preoperatively, there was no suspicion of the diagnosis of aggressive angiomyxoma. Moreover, the differential diagnosis was between lipoma and testicular malignances. We preferred a perineal procedure with patient in lithotomy position; also the team was composed of a general surgeon and an urologist. We extracted a mucoid mass en bloc with free macroscopic margins. The mass was 11 cm in its max diameter, this was extended to the pubic symphysis and displaced the urethra without infiltrated it. The histological examination revealed small spindle-shaped cells without atypia or mitosis proliferating in an edematous to fibrous stroma and numerous small- to medium-sized thick-walled vessels. Around the mass was a smooth muscle integument. The neoplasmatic cells had the expression of desmin, CD34, S100, vimentin, smooth muscle antibody, estrogen receptor 40%, progesteron receptor 20% and Ki67-5%. Postoperatively, our patient had an uneventful recovery. A postoperative SPECT was negative for metastatic disease, and the 2-year follow-up is negative for recurrence of the disease.
Figure 1.

Ultrasound of scrotum
Figure 2.

MRI of the scrotum T2
Figure 3.
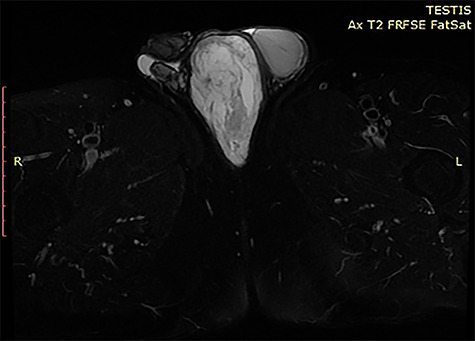
MRI of the scrotum T2 FatSat
DISCUSSION
Aggressive angiomyxoma is a rare entity most frequently between reproductive age women (male/female: 1/7) [3]. Aggressive angiomyxoma or deep angiomyxoma as referred by the world health organization is a mesenchymal malignancy first described in 1983 by Steeper and Rosai. This tumor most commonly derived from the female vulvar region, pelvis and perineum and male scrotum and inguinal region, but there are a few cases with non-pelvic invasion [4, 5]. At the most cases, angiomyxoma is an asymptomatic gradually enlargement mass, the symptoms in most patients are swelling without pain, abdominal distention, hematuria or vaginal hemorrhage in women. In our case, the only symptom was the palpable mass of the scrotum [1, 6]. The differential diagnosis of the palpable mass of scrotum in men patients is between perineal cyst, inguinal hernia, hydrocele, lipoma, abscess, leiomyoma, leiomyosarcoma, liposarcoma, testicular tumors or unidentified masses. The examination of the mass should begin with ultrasound tomography, which demonstrates a hypoechoic, well-demarcated mass with multiple thin echogenic internal septa, and for more detailed imaging, we can use computed tomography or magnetic resonance imaging, which on T2 weighted image has high signal intensities, or digital subtraction angiography to recognize the details of mass structure, to identify the relations between the near anatomical structures in order to organize the operation. Aggressive angiomyxoma has a distinctive imaging appearance of swirled or layered pattern in the tumor after enhancement on CT and MRI [7–9] with intravenous contrast injection. Preoperative diagnoses require high degree of suspicion. There are a few cases with preoperative histological diagnoses with CT assisted biopsy, but in most described cases the diagnosis was made postoperatively with the histological examination of the mass. Histologically, the typical findings include stellate to spindle-shaped tumor cells with fibromyxoid stroma and hyalinized thin-to-thick wall vessels and no necrosis or cystic changes, and the immunohistochemical studies show the expression of vimentin, smooth-muscle actin and CD34 to be strongly positive, the desmin, estrogen receptors and progestin receptors to be median positive, but mostly negative for S-100 and CD68 [3]. The more effective treatment for aggressive angiomyxoma is the radical free margin surgical excision. However, the risk of local recurrence is high especially within 2–3 years after the first operation. A reason for local recurrence is the incomplete surgical excision; however; Chan et al. [6] report no difference in recurrence in patients with negative margins compared with those with positive margins. In general, aggressive angiomyxoma has no tendency for distal metastases, but there was a report of a case with lung and mediastinum metastases. Radiation therapy has proposed as a monotherapy or as control of multiple recurrences after surgical excision, with poor results [10]. Chemotherapy has poor results in aggressive angiomyxoma because of the slow progress of the disease. Monotherapy may has a role in control of these tumors because of the expression of ER and PR receptors.
Contributor Information
George Kirkilessis, Department of Surgery, General Hospital AttiKon, Athens, Greece.
Kyriaki Kakavia, Department of Vascular Surgery, General Hospital of Athens Laiko, Athens, Greece.
Dimitrios Bougiouklis, Department of Surgery, General Hospital of Pyrgos, Pyrgos, Greece.
Anestis Papadopoulos, Department of Surgery, General Hospital of Pyrgos, Pyrgos, Greece.
Charalampos Lampropoulos, Department of Surgery, General Hospital of Pyrgos, Pyrgos, Greece.
Ioannis Kirkilessis, Department of Surgery, General Hospital of Pyrgos, Pyrgos, Greece.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
- 1. Draeger DL, Protzel C, Hakenberg OW. Aggressive angiomyxoma as a rare differential diagnosis of enlargement of the scrotum. Clin Genitourin Cancer 2016;14:e237–9. [DOI] [PubMed] [Google Scholar]
- 2. Schwartz PE, Hui P, McCarthy S. Hormonal therapy for aggressive Angiomyxoma: a case report and proposed management algorithm. J Low Genit Tract Dis 2014;18:E55–61. [DOI] [PubMed] [Google Scholar]
- 3. Jingping Z, Chunfu Z. Clinical experiences on aggressive angiomyxoma in China (report of 93 cases). Int J Gynecol Cancer 2010;20:303–7. [DOI] [PubMed] [Google Scholar]
- 4. Bajaj MS, Mehta M, Kashyap S, Pushker N, Lohia P, Chawla B, et al. Clinical and pathologic profile of angiomyxomas of the orbit. Ophthal Plast Reconstr Surg 2011;27:76–80. [DOI] [PubMed] [Google Scholar]
- 5. Wang Z, Liu Y, Yang L, Gu L, He Y, Huang D, et al. Maxillary aggressive angiomyxoma showing ineffective to radiotherapy: a rare case report and review of literature. Int J Clin Exp Pathol 2015;8:1063–7. [PMC free article] [PubMed] [Google Scholar]
- 6. Gaunay GS, Barazani Y, Kagen AC, Stember DS. Aggressive angiomyxoma of the scrotum. Clin Imaging 2013;37:1122–4. [DOI] [PubMed] [Google Scholar]
- 7. Tariq R, Hasnain S, Siddiqui MT, Ahmed R. Aggressive angiomyxoma: swirled configuration on ultrasound and MR imaging. J Pak Med Assoc 2014;64:345–8. [PubMed] [Google Scholar]
- 8. Idrus Alhabshi SM, Abd Rashid M. Large perineal and gluteal angiomyxoma: the role of diagnostic imaging and literature review. Case Rep Dermatol 2013;2013: bcr2013008680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Karwacki GM, Stöckli M, Kettelhack C, Mengiardi B, Studler U. Radiographic diagnosis and differentiation of an aggressive angiomyxoma in a male patient. Radiology Case 2013;7:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bhandari RN, Dragun AE, Aguero EG, Sharma AK. External beam radiotherapy for perirectal Angiomyxoma results in a dramatic clinical response and allows a patient to avoid abdominoperineal resection. Am J Clin Oncol 2006;29:318–9. [DOI] [PubMed] [Google Scholar]


