Abstract
The impact of the COVID-19 pandemic on the incidence of community-acquired pneumonia in elderly people remains uncertain. We compared the number of elderly patients admitted to our hospital for community-acquired pneumonia from January to June 2020 to the numbers from the same period in each of the last three years. The number of patients began decreasing in February 2020, and by April 2020 the number was significantly lower than those from the same period in the three years prior. There is no evidence regarding the impact of general infection control measures, such as wearing a face mask or washing one's hands, on the development of community-acquired pneumonia, because causative bacteria are not believed to be transmitted from human to human. However, these measures might have indirectly contributed to a decreased number of cases through the prevention of common viral infections which could be a trigger of community-acquired pneumonia.
Keywords: Elderly, Pneumonia, Coronavirus, Community-acquired
While a decline in the incidence of a variety of viral diseases, such as influenza, has been reported following the COVID-19 outbreak [1,2], the trend remains uncertain for community-acquired pneumonia in elderly people, with the exception of pneumonia caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
Pneumonia is one of the most common infectious diseases, and can be the primary cause of hospitalization and mortality in older individuals. To assess the impact of the COVID-19 pandemic on the incidence of community-acquired pneumonia in elderly people, we compared in the number of elderly patients (≥65 years old) admitted to our hospital with community-acquired pneumonia from January to June 2020 to those from the same period in 2017, 2018, and 2019. Our facility has the largest capacity to accept elderly patients with community-acquired pneumonia in Oita Prefecture; however, without negative pressure isolation rooms, we have never been able to accept COVID-19 patients.
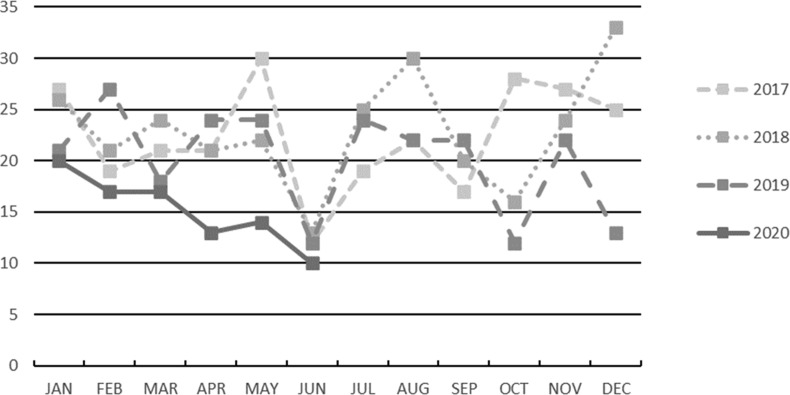
The number of elderly patients with community-acquired pneumonia began to decrease in February 2020, and by April 2020 was significantly lower than in the same period in the three years prior, as seen in Fig. 1 . The number of patients in June 2020 was lower than that from January to May for the three years prior, however, the number was found to be similar to those in June 2017, 2018 and 2019.
Fig. 1.
Number of elderly patients admitted to our hospital for community-acquired pneumonia. The incidence in April differed significantly between the years 2017, 2018, 2019, and 2020 (p < 0.01 for each by chi-square test), and the incidence in 2020 was significantly lower than that in 2019 (p < 0.002 for each by Ryan's multiple comparison test). There were no significant differences noted in the number of patients in May and June, between 2017, 2018, 2019 and 2020.
The COVID-19 pandemic has brought about many lifestyle changes, including the encouragement to wear masks, increased handwashing, maintaining social distance, and the suspension of mass gatherings. These preventive measures may have contributed to a decline in many types of viral diseases which spread through droplet or contact transmission [3]. Pneumonia in elderly people is thought to be caused by the aspiration of oral secretions containing causative pathogens [4]. Aggressive oral care has been proven to reduce the incidence of pneumonia in elderly people [5]; however, there is no evidence regarding the impact of general infection control measures, such as wearing a face mask or washing one's hands, on the development of community-acquired pneumonia. The pathogens responsible for pneumonia in elderly people include Streptococcus pneumoniae, Haemophilus influenzae, Klebsiella pneumoniae, and other bacteria existing inside the oral cavity [6], and these bacteria are not believed to be directly transmitted from human to human.
A primary viral infection, however, can trigger the development of bacterial pneumonia. A previous study found a significant increase in pneumonia-related hospitalizations during the 2009–2010 H1N1 influenza pandemic [7], and virus-mediated effects on the defense of the pulmonary host and a subsequent impairment of bacterial clearance have been revealed [8]. Consequently, the measures for COVID-19 infection control may prevent general viral infections, and subsequently, bacterial pneumonia as well.
The results of the present study showed a decline in the number of elderly patients with pneumonia following the COVID-19 outbreak, specifically in the setting of a hospital that does not accept COVID-19 patients. Measures against droplet and contact transmission might have indirectly contributed to a decreased number of cases through the prevention of common viral infections which can trigger community-acquired pneumonia. Physicians need to be aware of these possibilities, and continue to address measures for infection control.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to thank Ms. Teruyo Torii, Ms. Kyoko Yamanoue, Mr. Masahiko Goto, and Mr. Daichi Suga (Tenshindo Hetsugi Hospital, Oita) for their support and suggestions.
References
- 1.Sakamoto H., Ishikane M., Ueda P. Seasonal influenza activity during the SARS-CoV-2 outbreak in Japan. J Am Med Assoc. 2020;323:1969–1971. doi: 10.1001/jama.2020.6173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Komiya K., Yamasue M., Takahashi O., Hiramatsu K., Kadota J.I., Kato S. The COVID-19 pandemic and the true incidence of tuberculosis in Japan. J Infect. 2020;81:e24–e25. doi: 10.1016/j.jinf.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ministry of Health, Labour and Welfare . vol. 22. 2020. (Infectious diseases weekly report Japan). [Google Scholar]
- 4.Komiya K., Rubin B.K., Kadota J.I., Mukae H., Akaba T., Moro H. Prognostic implications of aspiration pneumonia in patients with community acquired pneumonia: a systematic review with meta-analysis. Sci Rep. 2016;6:38097. doi: 10.1038/srep38097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sjögren P., Wårdh I., Zimmerman M., Almståhl A., Wikström M. Oral care and mortality in older adults with pneumonia in hospitals or nursing homes: systematic review and meta-analysis. J Am Geriatr Soc. 2016;64:2109–2115. doi: 10.1111/jgs.14260. [DOI] [PubMed] [Google Scholar]
- 6.Komiya K., Ishii H., Kadota J. Healthcare-associated pneumonia and aspiration pneumonia. Aging Dis. 2015;6:27–37. doi: 10.14336/AD.2014.0127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weinberger D.M., Simonsen L., Jordan R., Steiner C., Miller M., Viboud C. Impact of the 2009 influenza pandemic on pneumococcal pneumonia hospitalizations in the United States. J Infect Dis. 2012;205:458–465. doi: 10.1093/infdis/jir749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prasso J.E., Deng J.C. Postviral complications: bacterial pneumonia. Clin Chest Med. 2017;38:127–138. doi: 10.1016/j.ccm.2016.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]