Highlights
-
•
The management of the SARS-Cov-2 pandemic in Germany was named a success story.
-
•
A statistically sound estimate of excess mortality has not been made for Germany.
-
•
The excess mortality during the first wave of the pandemic is 8071 cases.
-
•
After age adjustment, there were 4926 fewer deaths than expected.
-
•
Several factors explain the comparatively mild course of the pandemic in Germany.
Keywords: Corona virus, COVID-19, Mortality, Pandemic, Germany
Abstract
Objectives
The first wave of the SARS-CoV-2 pandemic in Germany lasted from week 10 to 23 in 2020. The aim is to provide estimates of excess mortality in Germany during this time.
Methods
We analyzed age-specific numbers of deaths per week from 2016 to week 26 in 2020. We used weekly mean numbers of deaths of 2016–2019 to estimate expected weekly numbers for 2020. We estimated standardized mortality ratios (SMR) and 95% confidence intervals.
Results
During the first wave observed numbers of deaths were higher than expected for age groups 60–69, 80–89, and 90+. The age group 70–79 years did not show excess mortality. The net excess number of deaths for weeks 10–23 was +8,071. The overall SMR was 1•03 (95%CI 1•03–1•04). The largest increase occurred among people aged 80–89 and 90+ (SMR=1•08 and SMR=1•09). A sensitivity analysis that accounts for demographic changes revealed an overall SMR of 0•98 (95%CI 0•98–0•99) and a deficit of 4,926 deaths for week 10–23, 2020.
Conclusions
The excess mortality existed for two months. The favorable course of the first wave may be explained by a younger age at infection at the beginning of the pandemic, lower contact rates, and a more efficient pandemic management.
Introduction
SARS-CoV-2 is transmitted by droplets and likely aerosols. The median incubation period is about 5–6 days (range 1–14 days)1 and the median age at confirmed infection in Germany is 49 years. Typical symptoms include fever, cough, anosmia, ageusia, and pneumonia. The mortality rate of COVID-19 is higher among elderly and among ethnicities other than Caucasians. Furthermore, a markedly higher mortality rate has been observed for several comorbidities including obesity class II (BMI 35•0–39•9 kg/m2) and III (BMI 40•0+ kg/m2), uncontrolled diabetes mellitus, malignancies in the previous year, severely reduced glomerular filtration rate (GFR) (below 30 ml/min/1•73m2), chronic respiratory diseases other than asthma, chronic liver disease, stroke, dementia, organ transplant, and immunosuppression2.
The case-fatality of COVID-19 in Germany below age 60 years is close to zero. However, among elderly, the case-fatality exponentially increases from age 60–64 up to age 80–84 and thereafter slightly levels off3. The first wave of the SARS-CoV-2 pandemic started in Germany at week 10 (March 2, 2020) and ended in week 23 (June 7, 2020). As part of the fight against the pandemic, the federal government banned major events with more than 1000 participants from March 9, 2020. This was followed by a nationwide lockdown on March 23, 2020.
To estimate the mortality burden of SARS-CoV-2 it is possible to study the increase in deaths if SARS-CoV-2 had not occurred. Vestergaard et al. presented pooled estimates of all-cause mortality and estimated excess deaths for 24 European countries together.4 Due to the different course of the SARS-CoV-2 pandemic in European countries, pooling of mortality data masks important national differences. The aim of this paper is to provide estimates of excess mortality in Germany during the SARS-CoV-2 pandemic.
Material & methods
On July 24, 2020, the Federal Bureau of Statistics provided mortality figures by days, weeks and months since 1 January 2016. Whereas data for 2016–2018 are based on the final data of these years, data from January 1, 2019 onwards are preliminary as they are a pure case count of the death notifications received from the registry offices without the usual statistical processing. The last day of mortality data provided is June 28, 2020 (the end of week 26).
We used nationwide daily number of deaths of the years 2016–2020 and focused on the weeks 10–23 of each year as these weeks represent the first pandemic wave of SARS-CoV-2 in Germany in 20205. Furthermore, we used the Robert Koch-Institute COVID-19 dashboard6 to extract the daily number of newly confirmed SARS-CoV-2 infections and the daily number of “SARS-CoV-2 associated” deaths in Germany. Up to now, it is difficult to distinguish between deaths due to versus deaths with SARS-CoV-2.
We extracted the daily number of patients treated in intensive care units (ICUs) in Germany from the web page of the German Interdisciplinary Association for Intensive Care and Emergency Medicine (Deutsche Interdisciplinäre Vereinigung für Intensiv- und Notfallmedizin, DIVI)7. Before calendar week 17, the registration of COVID-19 patients treated in ICUs in Germany was incomplete as reporting was not mandatory until week 17, 2020 in Germany. Since week 17, the hospitals in Germany with ICUs are required to report COVID-19 patients being treated in ICUs.
Statistical methods
To dampen the random fluctuation of age-specific mortality figures we aggregated daily numbers to weekly numbers with weeks starting on Mondays. In the main analysis, the reference period are weeks 10–23 of the years 2016–2019 and the index period are weeks 10–23 in 2020. The reference period provides the number of expected deaths in the absence of COVID-19. For each calendar week 10–23, we subtracted the expected number of weekly deaths from the observed number of deaths for the weeks 10–23, 2020.
Furthermore, we estimated standardized mortality ratios (SMRs) and 95% confidence intervals by age groups 0–29, 30–49, 50–59, 60–69, 70–79, 80–89, and 90 years and more. As provided data were not stratified by sex, we were not able to provide sex-specific SMRs. The reference period of 2016–2019, weeks 10–23, includes seasonal influenza waves. The estimated excess mortality due to seasonal influenza as reported by the Robert Koch-Institute in 2015–2016 (week 2–15 of 2016) was 0, in 2016–2017 (week 51 of 2016 to week 11 of 2017) was 22,900 deaths, and in 2017–2018 (week 52 of 2017 up week 14 of 2018) was 25,100 deaths. Excess deaths for the seasons 2018–2019 (week 2–14 of 2019) and 2019–2020 (week 2–12) are not available until now.
Sensitivity analysis
Within the years 2016–2020 there were marked changes in population size, especially in the age group of 80+ years (increase by relative 17•5 percent) where the expected number of COVID-19 deaths is highest (Supplementary Table 1). Not accounting for this increase produces a bias of the SMR away from the reference value to values above 1.
We therefore ran a sensitivity analysis that can only partially address this potential bias because weekly population figures are not available. Instead, we had to use midyear population figures to estimate weekly age-specific mortality rates. We first estimated the age-specific weekly mortality rates for each year 2016 through 2019 using the age-specific midyear populations of these years and thereafter calculated the means of these annual age-specific weekly rates so that we came up with mean mortality rates for the age groups 0–29, 30–49, 50–59, 60–69, 70–79, and 80+ years for each calendar week 1–52.
As for 2016–2019, weekly population figures for 2020 were not available. We used instead the age-specific population figures of December 31, 2019 as a surrogate for the weekly population figures of the weeks 1–26 in 2020. We multiplied these population figures with the weekly age-specific mean rates of 2016–2019 to generate the expected number of deaths per week in 2020 in each age group. Thereafter, we estimated SMRs and corresponding 95% confidence intervals (Supplementary Table 2).
Results
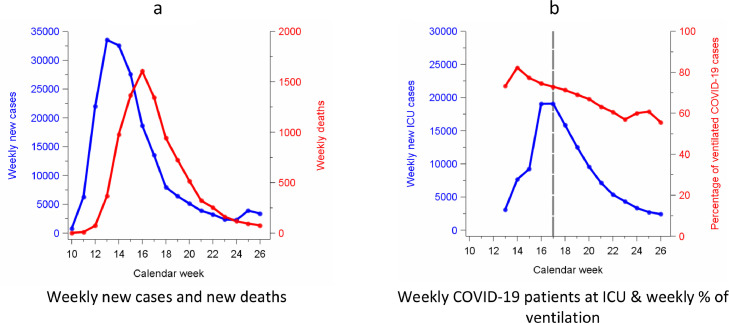
The first wave of SARS-CoV-2 in Germany lasted from week 10 to 23 in 2020. During this period, overall 183,978 SARS-CoV-2 infections were confirmed and 8674 deaths associated with COVID-19 have been registered. The peak of the weekly number of newly confirmed cases and weekly deaths associated with COVID-19 was week 13 (March 23–29, 2020) and 17 (April 20–26) respectively. The peak of the weekly number of COVID-19 patients requiring ICU treatment was also week 17. At week 17, overall 73% of all COVID-19 patients treated at ICUs received artificial ventilation (Fig. 1 ).
Fig. 1.
Weekly confirmed SARS-CoV2 infections, weekly number of deaths associated with COVID-19 (Fig. 1a) daily treated COVID-19 patients in intensive care units and in Germany, week 10–23. 2020 (Fig. 1b).
Legend: weekly new ICU cases were available starting from week 13, 2020; before week 17, 2020, the reported number of weekly new ICU cases may underestimate the true number because of incompleteness of registration.
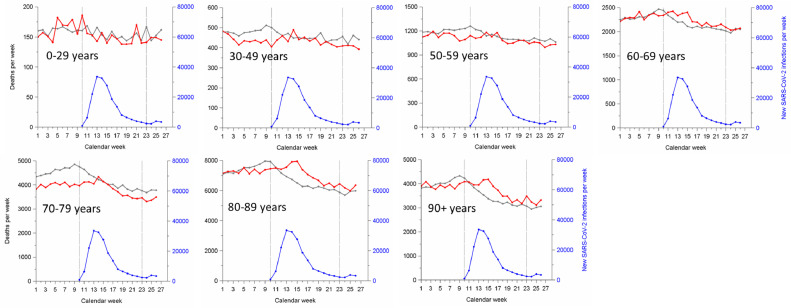
The expected number of weekly deaths based on mean values across the years 2016 through 2019 and the observed number of weekly deaths in 2020 are presented in Fig. 2 . For the age groups 30–49, 50–59, and 70–79 years, the observed number of deaths was lower than the expected number of deaths for the weeks 2–12 in 2020. In contrast, during the first SARS-CoV-2 wave in Germany (week 10–23), the observed number of deaths was higher than the expected number for the age groups 60–69, 80–89, and 90+ years. The age group 70–79 years did not show any excess mortality during the first wave.
Fig. 2.
Average number of weekly deaths in 2016–2019 and number of weekly death in 2020 by age group and weekly number of SARS-CoV-2 confirmed new cases in Germany, week 1–26, 2020.
Legend Fig. 2: gray graph shows the average number of weekly deaths of the years 2016–2019; red graph shows the weekly number of death in 2020; blue graphs shows the weekly number of SARS-CoV-2 confirmed new cases in Germany. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
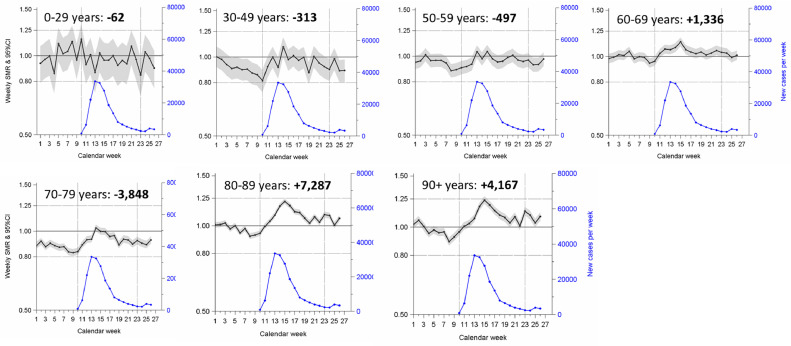
The age-specific SMRs by calendar week 1–26 are shown in Fig. 3 . Between week 7 and 10 (Feb 10 to March 8, 2020) SMRs tended to be below 1 for all age groups except ages 0–29 and 60–69 years. Thereafter, SMRs increased up to 1•25 for the age groups 60–69 years, 80–89, and 90+ years. The excess number of deaths (negative numbers indicate a lower number than expected, positive numbers indicate higher numbers than expected) for the weeks 10–23 were negative for the ages 0–59 years and 70–79 years and positive for all other age groups. The net excess number of deaths for weeks 10–23 was +8071 deaths. This number deviates from the registered number of 8674 deaths associated with COVID-19 as reported by the Robert Koch-Institute for the same time period.
Fig. 3.
Weekly standardized mortality ratios and 95% confidence intervals for overall mortality in Germany, week 1–26 in 2020 and weekly number of newly confirmed SARS-CoV-2 cases weeks 10–26, 2020 in Germany.
Legend Fig. 3: bold negative or positive numbers of death indicate whether during week 10–23 in 2020 there were more or less deaths compared to the average number of deaths in these weeks during 2016–2019; gray bands indicate 95% confidence intervals.
For the period of the first SARS-CoV-2 pandemic in Germany (week 10–23, 2020), the overall SMR was 1•03 (95%CI 1•03–1•04). SMRs were increased for the age groups 60–69, 80–89, and 90+ years. The largest increase occurred among people of the age groups 80–89 and 90+ years (SMR=1•08 and SMR=1•09 respectively) (Table 1).
Our sensitivity analysis reveals that the overall SMR for the week 10–23, 2020, is 0•98 (95%CI 0•98–0•99). With the exception of the age group 60–69 years, SMRs were below 1. According to this sensitivity analysis, there is a deficit of overall 4926 deaths during week 10–23, 2020. For age groups 60–69, 70–79, and 80+ years, weekly SMRs showed a peak at week 14–15 and were above 1 (60–69 years: SMR=1•09, 70–79 years: 1•07, 80+ years: 1•12) (Supplementary Figs. 1 & 2).
Discussion
The SARS-CoV-2 pandemic in Germany produced excess mortality during its first wave from week 10–23 in 2020. The estimated excess number of deaths during this period (+8071 deaths) is to some extent lower than the reported figures of deaths (8674 deaths) associated with COVID-19 by the Robert Koch-Institute (RKI). The gap between reported COVID-19 deaths and estimated excess deaths (overall 603 deaths) is influenced by several factors including the filling and coding quality of death certificates, the SARS-CoV-2 test capacity in Germany at that time and the location of death (hospital, nursing home, or unattended death at home)8. The RKI counts all deaths that are "associated with COVID-19″, which includes deaths that are potentially not attributable to COVID-19. According to the RKI report of July 26, 2020, about 12% of all SARS-CoV-2 positive cases were placed in nursing homes and other mass accommodations and 46% of COVID-19 deaths occurred in these facilities. The median age at COVID-19 death was 82 years in Germany9.
The influenza season 2017/2018 (week 52 of 2017 up week 14 of 2018) was the worst influenza season in Germany of the last 30 years with an estimated excess number of deaths of overall 25,100.10 However, also the influenza season 2016/2017 resulted in an excess number of deaths of overall 22,900 deaths in Germany. Excess deaths for the influenza seasons 2018–2019 (week 2–14 of 2018) and 2019–2020 (week 2–12 of 2020) have not been provided by the Robert Koch-Institute until now. Our estimated SMRs below 1 during the weeks 2–12 in 2020 may be explainable by a shorter interval of the influenza season 2019–2020 (11 weeks) compared to the previous five influenza seasons (13–15 weeks) and by a milder course.11 Compared to seasonal influenza, Germany has apparently got off lightly so far with COVID-19.
Germany has also come through the first wave well in international comparison. The estimated excess deaths due to COVID-19 are markedly higher in countries such as Spain, Italy, United Kingdom, Brazil and the United States. Many factors may explain why Germany was so far successful in combating the pandemic in terms of excess mortality. First, the SARS-CoV-2 pandemic started in Germany predominantly among younger people (median age of 40 years until March 4, 2020)12 typically coming back from skiing holidays in the alps and only thereafter the pandemic also spread among older people. Since March 2020, the median age of all confirmed SARS-CoV-2 cases which were reported to the Robert Koch-Institute changed to 48 years in July 26, 20209. Low age at infection is one of the most important factors that prevents COVID-19 deaths2. In contrast to Japan where a substantial proportion of SARS-CoV-2 infections were acquired in hospitals and nursing homes13, only about 15% of SARS-CoV-2 infections were acquired by typically more vulnerable and elderly patients in hospitals or nursing homes up to the end of the first SARS-CoV-2 pandemic wave in Germany.14 Second, the daily mean number of social contacts defined as either skin-to-skin contact (kiss or handshake) or a two-way conversation with three or more words in the physical presence of another person was considerably lower in Germany (8•0) than in any other country that was included in this study. Italy had the highest mean value of 20. Furthermore, the difference of mean contacts in Germany and Italy is particularly prominent for contacts of children to persons aged 65 years or more15. The considerably lower amount of social mixing in Germany may have prevented especially infections among the elderly who have a considerably higher case-fatality than younger people. Third, factors related to the health care system including the number of general practitioners, hospital beds and especially ICU bed capacity may have played a beneficial role in Germany. Fourth, the early pandemic management may have differed compared to other countries. In response to the pandemic, local public health authorities were strengthened and extra staff was employed to support local contact tracing16. Subjects with a potential infection or contact to other infected subjects and people coming from risk territories were strongly encouraged to stay at home. Furthermore, these people were advised not to see a doctor if possible. If general practitioners (GPs) or the local health authority was asked for help and advice much of this counselling was done via telephone hotlines. The indication for a SARS-CoV-2 test was examined by the local health authorities (Public Health offices) because of the initial bottlenecks in testing capacity. A SARS-CoV-2 PCR test was performed in case of symptoms, contact to infected persons, or persons from risk areas. This approach was possible because Germany was in addition to some Asian countries one of the first in the world to establish meaningful test capacities. As a consequence, many contacts to infected people could be prevented and it was possible to prevent increasing numbers of infected persons and thus also in some cases persons requiring intensive care treatment.17 Further research is needed to find out why the pandemic has been so relatively mild in Germany.
Based on our results we cannot answer whether the rigorous lockdown in Germany was the reason for the relatively low numbers of fatal cases during the first wave of SARS-CoV-2 infections. With 2922 COVID-19 patients at intensive care units on April 18, 2020, the first SARS-CoV-2 wave had reached the maximum COVID-19-related utilization of the ICUs. At that time, the German Interdisciplinary Association for Intensive Care and Emergency Medicine, which did not completely register all hospitals with ICU beds at the time, registered about 16,700 available ICU beds17 so that debates on triage of patients did not seem to be indicated. In the meanwhile, the intensive care bed capacity has been increased to 30,000 beds. As long as the intensive care bed capacity is not too heavily burdened by COVID-19, risk-based lockdown relaxation measures seem possible, especially for younger people (under 60 years) in Germany.18 However, relaxation measures should be accompanied by close monitoring of the development of COVID-19 case numbers. According to Dehning et al., effects of lockdown relaxation on the number of confirmed new infections occur with a delay of about 11 days in Germany1.
There are several factors that limit our results. First, we were not able to provide sex-specific estimates of excess mortality because the Federal Bureau of Statistics did not provide these data until now. We expect that men will show a higher excess mortality than women. In their cohort study based on national primary care electronic health record data linked to COVID-19 death data, Williamson et al. found a 59% (95%CI 53–65%) higher COVID-19 mortality rate among men than women after multiple adjustment for several confounders2. Second, the years 2016–2019 were used to estimate the COVID-19 excess mortality. However, these years were affected to varying degrees by the seasonal influenza excess mortality. Depending on the inclusion or exclusion of single years of the period 2016–2019 estimates of excess mortality vary. We therefore used the average number of deaths of the weeks 1–23 for the years 2016–2019 to reduce the influence of a single year. Third, we could only partially address the change in age distribution of the German population from 2016 to 2020. This imperfect sensitivity analysis showed that there was no excess mortality during the first pandemic wave in Germany but a deficit of deaths (overall 4926 deaths). It is difficult to decide whether the main or sensitivity analysis is more valid. Both forms of analysis suffer from limitations. While the main analysis did not take into account the change in age structure in the reference period, the sensitivity analysis did not take into account the weekly change in the underlying population figures during the reference and index period. The advantage of our main analysis is the predictability of the direction of potential bias: estimated SMRs tend to be farer away from the reference value. It is hard to speculate about the direction of the bias in our sensitivity analysis. Fourth, number of deaths may be influenced by other factors than influenza and COVID-19. For example, the lockdown was accompanied by a marked decrease of car, train, and air traffic and a reduction of contact rates, which was also most likely accompanied by a reduced risk of other infectious diseases. Furthermore, the lockdown was accompanied by a marked decrease in hospital bed occupancy, as hospitals were required by decree to maintain most of the capacity to treat expected COVID-19 cases. This was accompanied by a marked decrease in the hospitalization rate of the population and thus a reduction in the risk of SARS-CoV-2 infection in hospitals.
Declaration of Competing Interest
None of the authors declares a competing interest.
Acknowledgments
Acknowledgment
We thank Eva Bock and Hildegard Lax for their support in data management.
Funding
This work was supported by the German Federal Ministry of Education and Science (BMBF) [grant number 01ER1305].
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jinf.2020.09.012.
Appendix. Supplementary materials
References
- 1.Dehning J., Zierenberg J., Spitzner F.P. Inferring change points in the spread of COVID-19 reveals the effectiveness of interventions. Science. 2020;369(6500) doi: 10.1126/science.abb9789. eabb9789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Williamson E.J., Walker A.J., Bhaskaran K. Factors associated with COVID-19-related death using OpenSAFELY. Nature. 2020 doi: 10.1038/s41586-020-2521-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stang A., Standl F., Jöckel K.-.H. Characteristics of COVID-19 pandemic and public health consequences. Herz. 2020;45(4):313–315. doi: 10.1007/s00059-020-04932-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vestergaard L.S., Nielsen J., Richter L. Excess all-cause mortality during the COVID-19 pandemic in Europe – preliminary pooled estimates from the EuroMOMO network, March to April 2020. Eurosurveillance. 2020;25(26) doi: 10.2807/1560-7917.ES.2020.25.26.2001214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Statistisches Bundesamt. Sterbefälle - Fallzahlen nach Tagen, Wochen, Monaten, Altersgruppen und Bundesländern für Deutschland 2016 – 2020. https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Bevoelkerung/Sterbefaelle-Lebenserwartung/Tabellen/sonderauswertung-sterbefaelle.html?nn=375478 (accessed 24.07 2020).
- 6.Robert Koch-Institute. COVID-19 Dashboard. https://experience.arcgis.com/experience/478220a4c454480e823b17327b2bf1d4 (accessed 24.07 2020).
- 7.Deutsche Interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin D. Tagesreport - DIVI-Intensivregister. https://www.divi.de/register/tagesreport (accessed 24.07 2020).
- 8.Weinberger D.M., Chen J., Cohen T. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern Med. 2020 doi: 10.1001/jamainternmed.2020.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Robert Koch-Institute . Robert Koch-Institute; 2020. Täglicher Lagebericht des RKI zur Coronavirus-Krankheit-2019 (COVID-19). 26.7.2020 Aktualisierter Stand für Deutschland.https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/Gesamt.html accessed 27.07 2020. [Google Scholar]
- 10.Robert Koch-Institute . Robert Koch-Institute; 2020. Pommes für die Grippeschutzimpfung? Neuer Influenza-Saisonbericht erschienen.https://www.rki.de/DE/Content/Service/Presse/Pressemitteilungen/2019/10_2019.html accessed 24.07 2020. [Google Scholar]
- 11.Robert Koch-Institute. Kürzere Dauer der Grippewelle 2019/20 sowie abrupter Rückgang der Raten an Atemwegserkrankungen. Epidemiologisches Bulletin: Robert Koch-Institut; 16/2020. https://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2020/Ausgaben/16_20.html (accessed 24.07 2020).
- 12.Robert Koch-Institute . Robert Koch-Institute; 2020. Täglicher Lagebericht des RKI zur Coronavirus-Krankheit-2019 (COVID-19). 04.03.2020 Aktualisierter Stand für Deutschland.https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/Gesamt.html accessed 27.07 2020. [Google Scholar]
- 13.Furuse Y., Sando E., Tsuchiya N. Clusters of coronavirus disease in communities, Japan. Emerg Infect Disease J. 2020;26(9) doi: 10.3201/eid2609.202272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robert Koch-Institute . Robert Koch-Institute; 2020. Täglicher Lagebericht des RKI zur Coronavirus-Krankheit-2019 (COVID-19). 07.06.2020 Aktualisierter Stand für Deutschland.https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Situationsberichte/Gesamt.html accessed 27.07 2020. [Google Scholar]
- 15.Mossong J., Hens N., Jit M. Social contacts and mixing patterns relevant to the spread of infectious diseases. PLoS Med. 2008;5(3):e74. doi: 10.1371/journal.pmed.0050074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Reintjes R. Lessons in contact tracing from Germany. BMJ. 2020;369:m2522. doi: 10.1136/bmj.m2522. [DOI] [PubMed] [Google Scholar]
- 17.Stang A., Stang M., Jöckel K.-.H. Estimated use of intensive care beds due to COVID-19 in Germany over time. Dtsch Arztebl Int. 2020;117(19):329–335. doi: 10.3238/arztebl.2020.0329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Standl F., Jöckel K., Stang A. COVID-19 and the need of targeted inverse quarantine. Eur J Epidemiol. 2020;35(4):339–340. doi: 10.1007/s10654-020-00629-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.