Abstract
The COVID-19 pandemic caused by the infection with the novel Coronavirus SARS-CoV-2, revealed individual and global vulnerabilities, in which we highlight the social, economic, and political aspects and the health systems’ organization in the countries. Brazil remains with a high transmission rate and presents a centripetal distribution as observed through a more sustained growth in the number of municipalities affected, outlining a profile of invasion of poor communities. Several vulnerabilities overlap with precarious housing conditions, lack of basic sanitation, malnutrition, and endemicity for neglected chronic diseases such as visceral leishmaniasis (VL). COVID-19 and VL evidently do not share clinical features, but exactly because of the distinct immunopathogenesis between the diseases, patients with VL may present a vulnerability in the immune system against antiviral responses. Considering that VL susceptibility seems to be related to an inefficient and polarized immune response, it is likely that in endemic areas, the overlap of social weaknesses added to individual vulnerability by immune polarization may aggravate the COVID-19 condition. In this sense, we reinforce that possible relationships between endemic neglected diseases such as VL and pandemic SARS-CoV-2 infection need to be further considered and investigated.
Keywords: COVID-19, SARS-CoV-2, Visceral leishmaniasis, Brazil, Immune response
Dear editor,
The COVID-19 pandemic caused by the infection with the novel Coronavirus SARS-CoV-2 [1], revealed individual and global vulnerabilities, in which we highlight the social, economic, and political aspects and the health systems’ organization in the countries. With the advancement of the disease and accumulation of epidemiological data, the world organizations prepared a list of risk groups for COVID-19, including elderly, hypertensive, diabetic, obese, individuals with cardiovascular problems, and more recently these groups were expanded to include pregnant women, asthmatics, conditions that affect their immune system, among others [2].
In countries that still remain with a high transmission rate, COVID-19 presents a centripetal distribution as observed in Brazil through a more sustained growth in the number of municipalities affected, outlining a profile of invasion of poor communities [3], [4]. Several vulnerabilities overlap with precarious housing conditions lack, of basic sanitation, malnutrition, and endemicity for neglected chronic diseases such as visceral leishmaniasis (VL). In 2018, VL lethality in the Americas reached 8%, and among the total of notified cases, 97% (3,466) were reported by Brazil [5]. Interestingly, in the scientific literature on this issue, VL versus COVID-19 is still quite limited, but recently Miotti and co-authors published a first case of COVID-19 in a patient with VL in Italy. In this patient, immunosuppression caused by VL seems to have contributed to the worsening of the clinical course [6]. Despite the well-described report, correlation factors between diseases are not listed.
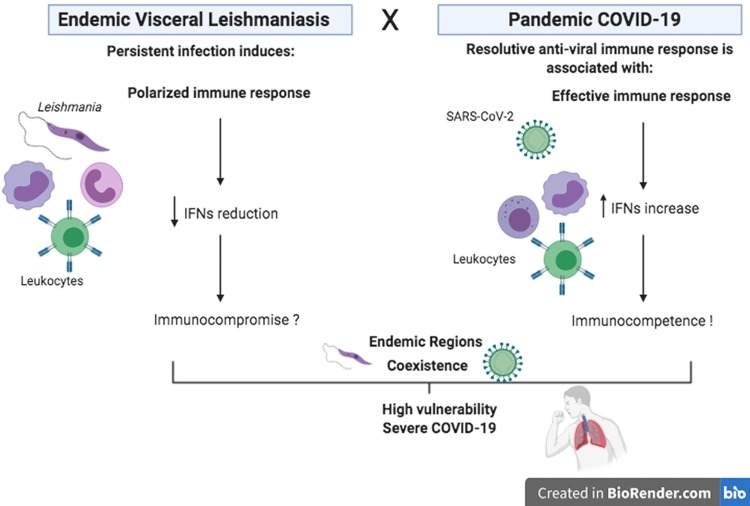
COVID-19 caused by the novel Coronavirus and the VL induced following infection with protozoan Leishmania (Leishmania) infantum, evidently do not share clinical features, but exactly because of the distinct immunopathogenesis between the diseases, patients with VL may present a vulnerability in the immune system against antiviral responses. Protozoan persistence seems to be very frequent in infected individuals, and the development of an immunocompromise, and in some cases an immunosuppressive state, impacts various activities of innate and adaptive immunity [7] in patients with VL as evidenced by the inability of IFN-γ production by peripheral blood mononuclear cells stimulated with leishmanial antigens [8].
Regarding COVID-19, studies point out that a resolutive anti-viral immune response is associated with an effective inflammation related to IFNs production, activation of cellular immunity by CD8 T lymphocytes and NK cells, and counterbalanced by a modulated anti-inflammatory response [9]. Considering that VL susceptibility seems to be related to an inefficient and polarized immune response, it is likely that in endemic areas, the overlap of social weaknesses added to individual vulnerability by immune polarization may aggravate the COVID-19 condition (Fig. 1 ), contributing to maintenance of sustained high levels of the number of cases, or even by an unfavorable impact on the outcome, leading to mortality.
Fig. 1.
A brief scheme of the immunological intersection between endemic VL and pandemic COVID-19.
The COVID-19 pandemic has revealed many vulnerability relational aspects in the individual and collective domain. In this sense, we reinforce that possible relationships between endemic neglected diseases such as VL and pandemic SARS-CoV-2 infection need to be further considered and investigated.
Acknowledgments
Acknowledgment
FAPEMIG (Minas Gerais State Research Foundation, Minas Gerais, Brazil); CAPES (Coordination of Training of Higher Education Graduate Foundation, Brasilia, Brazil); and CNPq (National Council for Scientific and Technological Development, Brazil).
Authors’ contributions
S.F.G. Carvalho and M.C. Andrade contributed to conception, design, data acquisition, and interpretation, and drafted and critically revised the manuscript. T.M. Vieira and A.P.V. Moura contributed to interpretation and critically revised the manuscript. All authors gave their final approval and agree to be accountable for all aspects of the work.
Declaration of Competing Interest
The author declares no competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Singhal T. A review of coronavirus disease-2019 (COVID-19) Indian J Pediatr. 2020;87(4):281–286. doi: 10.1007/s12098-020-03263-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Evidence used to update the list of underlying medical conditions that increase a person’s risk of severe illness from COVID-19. [Internet; updated July 28, 2020; cited 02 Sep 2020]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/evidence-table.html.
- 3.Carmo R.F., Nunes B.E.B.R., Machado M.F., Armstrong A.C., Souza C.D.F. Expansion of COVID-19 within Brazil: the importance of highways. J Travel Med. 2020;27(5) doi: 10.1093/jtm/taaa106. taaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pessoa ZS, Teixeira RLP, Clementino MLM. Interfaces between Vulnerabilities, Governance, Innovation and Capacity of Response to COVID-19 in Brazilian Northeast. Ambient Soc. [cited 2020 Sep 02]; 23:e0110. Available from: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1414753X2020000100903&lng=en. Epub July 03, 2020. doi:http://dx.doi.org/10.1590/1809-4422asoc20200110vu2020l3id.
- 5.Organização Pan-Americana da Saúde [homepage on the internet]. Leishmanioses: Informe Epidemiológico nas Américas. Washington, D.C.: OPAS; 2019 [update 13 Dec 2020; cited 02 Sep 2020];Available from: http://iris.paho.org/xmlui/handle/123456789/50505.
- 6.Miotti A.M., Patacca A., Grosso C., Cristini F. COVID-19 in a patient with visceral leishmaniasis. J Infect Dis Ther. 2020;8:430. [Google Scholar]
- 7.Conceição-Silva F., Morgado F.N. Leishmania Spp-host interaction: there is always an onset, but is there an end? Front Cell Infect Microbiol. 2019;19(9):330. doi: 10.3389/fcimb.2019.00330. doi: .3389/fcimb.2019.00330. PMID: 31608245; PMCID: PMC6761226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gardinassi L.G., Garcia G.R., Costa C.H., Costa Silva V., de Miranda Santos I.K. Blood transcriptional profiling reveals immunological signatures of distinct states of infection of humans with Leishmania infantum. PLoS Negl Trop Dis. 2016;10(11) doi: 10.1371/journal.pntd.0005123. PMID: 27828962; PMCID: PMC5102635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vabret N., Britton G.J., Gruber C., Hegde S., Kim J., Kuksin M. Immunology of COVID-19: current state of the science. Immunity. 2020;52(16):910–941. doi: 10.1016/j.immuni.2020.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]