Abstract
Background
Recent changes in the understanding and management of multiple sclerosis (MS) have increased the role of MRI in supporting diagnosis and disease monitoring. However, published guidelines on the use of MRI in MS do not translate easily into different clinical settings and considerable variation in practice remains. Here, informed by published guidelines for the use of MRI in MS, we identified a clinically informative MRI protocol applicable in a variety of clinical settings, from district general hospitals to tertiary centres.
Methods
MS specialists geographically representing the UK National Health Service and with expertise in MRI examined existing guidelines on the use of MRI in MS and identification of challenges in their applications in various clinical settings informed the formulation of a feasible MRI protocol.
Results
We identified a minimum set of MRI information, based on clinical relevance, as well as on applicability to various clinical settings. This informed the selection of MRI acquisitions for scanning protocols, differentiated on the basis of their purpose and stage of the disease, and indication of timing for scans. Advice on standardisation of MRI requests and reporting, and proposed timing and frequency of MRI scans were generated.
Conclusions
The proposed MRI protocol can adapt to a range of clinical settings, aiding the impetus towards standardisation of practice and offering an example of research-informed service improvement to support optimisation of resources. Other neurological conditions, where a gap still exists between published guidelines and their clinical implementation, may benefit from this same approach.
Keywords: Multiple sclerosis, MRI, Clinical practice, Diagnosis, Monitoring, Disease-modifying treatments
Introduction
Magnetic resonance imaging (MRI) is routinely used in clinical practice to detect and monitor inflammatory lesions in patients with multiple sclerosis (MS) [1]. Diagnostic criteria, as well as disease-modifying treatments (DMTs), have more recently increased the demand for MRI scans to allow early diagnosis and monitoring of treatment safety and efficacy [2, 3]. This has increased the burden on equipment and healthcare professionals, requiring rationalisation of resources.
Published guidelines on the use of MRI in MS exist [4, 5]. While these guidelines provide comprehensive recommendations, they do not translate easily into different clinical settings and considerable variation in practice remains [6–8]. Indeed, wide variations exist in the MRI acquisition protocols and timing of scanning, as well as in the reporting of images [9]. This makes within-patient, as well as between-centre comparisons difficult, delaying diagnosis and affecting treatment decisions. This variability underlines the need for further direction on the implementation of published guidelines to harmonise practice through the development of standardised MRI protocols and reports in MS that are informative, yet feasible and adaptable to a range of clinical settings within the National Health Service (NHS).
Here we report the outcome of a workshop that brought together MS specialists geographically representing the UK NHS and with expertise in MRI and that identified clinically informative MRI protocols applicable in a variety of clinical settings, from district general hospitals to tertiary centres.
Methods
The authors of this manuscript are MS specialists geographically representing the UK NHS and with expertise in MRI, either as neurologists with academic interest in neuroimaging or as neuroradiologists with MS as a specialist interest. They work as clinical academics and/or as NHS consultants in specialised MS centres, as well as in district general hospitals (DGH). Prior to the authors’ meeting to plan the present work, a comprehensive literature review and examination of MRI protocols was conducted to identify the points that made implementation of the existing guidelines challenging in the clinical practice across NHS settings. The authors completed a pre-meeting questionnaire to gather information on their experience with MRI protocols in NHS centres and to inform the scope for improvement. Both literature review and the outcome of the questionnaires were discussed in detail during the meeting to assess the need for a standardised MRI protocol applicable across clinical settings and to evaluate between-centre differences that could inform the development of minimum recommended MRI protocol for MS.
Results
Timing of MRI scans for MS diagnosis and monitoring
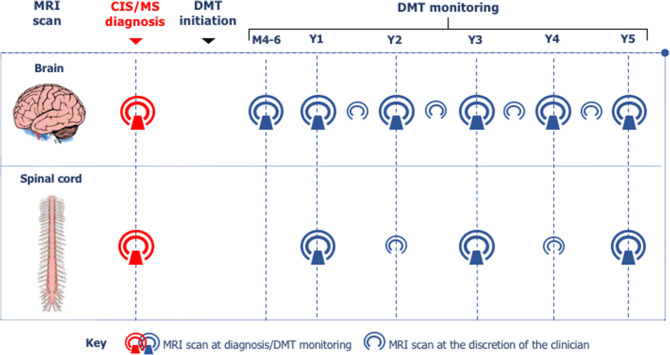
The clinical indications for MRI in MS vary from diagnosis to monitoring, as well as from assessment of treatment efficacy to surveillance for opportunistic infections (Table 1). An overview of the suggested timing for MRI scans in the diagnosis and monitoring of MS patients is reported for a period of 5 years in Fig. 1. This period is crucial for its long-term diagnostic and a prognostic value [10].
Table 1.
Indications for MRI in MS
The indication for MRI scanning in MS ranges from diagnosis to disease or DMTs monitoring, as highlighted below. MRI supports diagnosis, as well as disease monitoring. When a relapse cannot be confirmed purely on clinical grounds, MRI scan can be used to confirm clinical suspicion. Monitoring during DMTs aims to detect disease activity, as well as to characterise the type of damage that appears on the scan to exclude opportunistic infections such as PML
The asterisk indicates that MRI monitoring in patients on DMT is relevant to characterise the type of damage, as well as to assess safety of DMT
DMT disease-modifying treatment, JVC John Cunningham virus, MRI magnetic resonance imaging, MS multiple sclerosis, PML progressive multifocal leukoencephalopathy
Fig. 1.
Timing of MRI scans in the diagnosis and monitoring of MS patients. The authors advised to perform a brain and spinal cord scan at diagnosis. After the beginning of DMT or after a change in DMT, brain MRI scan was indicated yearly for at least 5 years, with a re-baseline brain scan 4–6 months after initiating or changing DMT. This was to interpret more confidently response to treatment at an early stage of the disease. More frequent scans were left at the discretion of the clinician, based on individual cases. Spinal cord MRI scan was advised every 2 years for at least 5 years after initiation or change of DMT, even in the absence of clear spinal cord signs or symptoms, with more frequent scans left at the discretion of the clinician, based on individual cases. In patients with predominant involvement of the spinal cord, yearly spinal scans may be more appropriate. The initial assessments should be conducted with the use of contrast; subsequent MRI scans for monitoring of disease activity, as well as of DMT efficacy, may include contrast when clinically indicated. The proposed timing assumes the start of DMTs soon after diagnosis. When this is not possible or indicated, monitoring would be left at the discretion of the clinician, but advised to be regular. CIS clinically isolated syndrome, MS multiple sclerosis, DMT disease-modifying treatment, MRI magnetic resonance imaging
Diagnosis
When the suspicion of clinically isolated syndrome (CIS) or of MS is raised, both brain and spinal cord scans should be requested [2, 11]. As well as providing information regarding lesion dissemination in space, spinal cord MRI is also valuable for differential diagnosis, when uncertainty exists over the nature of brain lesions [12, 13]. Although currently not routinely performed, MRI scanning of the optic nerve is important in patients who present with symptoms of visual dysfunction to aid the diagnostic process [2].
The administration of a gadolinium-based contrast agent (Gd) is important in the diagnostic workup to demonstrate dissemination in time of lesions. Therefore, it should be included in the diagnostic MRI protocol, when clinical suspicion of CIS or MS has been raised [2]. Gd highlights focal inflammatory activity during the preceding weeks (typically 6–8 weeks) and thus aids earlier diagnosis. Post-contrast MRI scan is also useful for the purpose of differential diagnosis [14]. Figure 2 offers indications of a minimum set of clinically informative MRI acquisitions that could be considered in a MRI protocol for MS diagnosis. Other sequences, e.g. 3D-T2*echo-planar imaging (EPI) for central vein sign, double inversion recovery (DIR) for cortical lesions, phase-sensitive inversion-recovery (PSIR) for improved detection of spinal cord lesions and MR spectroscopy for atypically looking MS lesions (e.g., tumefactive lesions), may be also considered in addition, if possible and necessary. These sequences are more frequently adopted in specialist centres because they require longer acquisition time and physics expertise for standardisation.
Fig. 2.
Suggested MRI acquisitions for MS diagnosis and monitoring. 3D acquisitions should be preferred as they make head positioning less critical, since readers can electronically re-slice the acquired image. DIS dissemination in space, DIT dissemination in time, MRI magnetic resonance imaging, MS multiple sclerosis, CIS clinically isolated syndrome, 2D 2 dimensional, 3D 3 dimensional, T1WI T1-weighted imaging, T2WI T2-weighted imaging, FLAIR fluid-attenuated inversion recovery, STIR short-TI inversion recovery, DWI diffusion-weighted imaging, SWI susceptibility-weighted imaging, GRE gradient recalled echo, FSE fast spin echo
Detection of disease activity and monitoring of efficacy
Monitoring MRI scans are useful in naïve patients, as well as at the beginning or following initiation or change of DMTs, or if a relapse is suspected, but cannot be confirmed purely on clinical grounds. Indeed, the importance of MRI to confirm stability is highlighted by the role of radiological activity in the evaluation of treatment response [1, 15].
Spinal cord MRI can reveal asymptomatic disease activity, as well as predict disease evolution [16]. Therefore, the authors felt that it should be performed regularly in addition to the brain scans, especially, but not exclusively, in patients in whom a previous involvement of the spinal cord has been demonstrated clinically or radiologically. Indeed, about 58% of new spinal cord lesions can be asymptomatic and 25% of patients with relapsing MS develops at least one asymptomatic spinal cord lesion over 1.5 years [11]; when only patients with stable RRMS are considered, 10% of them show subclinical spinal cord lesion activity alone [11]. Asymptomatic spinal cord lesions can also predict relapses, when combined with asymptomatic brain lesions [11]. Therefore, as spinal cord MRI can disclose subclinical disease activity in otherwise clinically stable MS, the authors supported its routine use in patient’s monitoring throughout the course of the disease and regardless of the clinical manifestation of MS in the cord.
Gd should be considered to aid detection of new inflammatory activity, when this would be too difficult to detect, due to high lesion burden, as well as for its prognostic utility, e.g., brain ring-enhancement patterns may forebode irreversible tissue damage and thus brain volume loss [17]. In the post-partum period, when monitoring is particularly important because of higher risk of relapse [18], the use of contrast enhancement may be limited by breastfeeding.
When patients are on specific DMTs, the primary purpose of a follow-up MRI scan is the detection of new inflammatory activity and the exclusion of opportunistic infections for safety of DMT prescription. As DMTs may reach their peak level of activity on MRI months after their initiation [19], a re-baseline scan beyond this time point is advisable. The authors felt that whether this scan should be performed with or without contrast enhancement should depend on clinical considerations such as the level of inflammatory activity at DMT initiation [20], the type of medication started [21] and the age of the patient [22] that all together define a risk for active disease. The presence or persistence of a Gd-active MRI scan at re-baseline could predict subsequent clinical and MRI activity [20, 23] and thus could indicate a subgroup of patients at higher risk of activity during DMTs.
The most recent classification of disease courses places importance on the presence or absence of disease activity also in the progressive forms of MS [24]. Also, with DMTs licenced in these stage (secondary progressive) or form (primary progressive) of the disease to control active inflammation, the authors felt that an approach to monitoring similar to the one used for relapsing MS would be reasonable, at least in the first few years (Fig. 1). MRI in progressive MS is a field in evolution that is likely to benefit from the introduction of methods to measure brain or cord atrophy in clinical practice [25].
Monitoring of DMTs safety
Patients treated with natalizumab or exposed to prolonged periods of lymphopenia with other DMTs may be at greater risk of progressive multifocal leukoencephalopathy (PML) [26]. Patients at risk of PML are typically those with anti-John Cunningham virus (JCV) antibodies, who have had treatment with natalizumab for over 18 months and have been given immunosuppressants before receiving natalizumab [27]. There is evidence to suggest that the management of PML is more successful if the condition is detected in a pre-symptomatic state through MRI [28]. Therefore, the differential diagnosis of new lesions is key: any lesions identified after initiating therapy with natalizumab, especially if more than 18 months, should be treated with suspicion. Any MRI changes consistent with PML that occur in immunocompromised patients should be classified as “radiologically-suspected PML” [29]. An algorithm has been developed to guide the use of MRI to monitor patients treated with natalizumab, based on anti-JCV antibody status and index value [29].
MRI acquisition
The detailed definition of a standardised MRI acquisition protocol was beyond the scope of this work, as the authors felt that such protocol for implementation of MRI sequences in the NHS would be more appropriately defined and endorsed by relevant professional bodies. However, the authors identified some characteristics of the MRI acquisition protocol that would be informative and feasible in any clinical setting.
Scanner strength
Different clinical MRI scanners may use different magnetic fields of strength, with higher strengths yielding greater resolution. Thus, when scanning individual patients, changes in scanner strength may generate an inaccurate representation of disease evolution over time, over- or under-estimating MS lesions. Previous scanner strength should be a primary consideration when deciding about future MRI scans to ensure comparability between studies. When moving to a different scanner strength, especially from lower to higher, re-baseline scan is advisable. A minimum magnet strength of 1.5T (T) is important to preserve an adequate level of detail in the images and facilitate reproducibility between centres.
Sequences
MRI scanning requirements may differ from diagnosis to monitoring (Fig. 2), as well as from assessment of efficacy to surveillance of opportunistic infections. Among the MRI sequences typically helpful to detect MS lesions, some may be of particular help to gain insight into specific aspects of MS pathology, such as perivenular infiltration, cortical damage and tissue loss. Susceptibility weighted imaging (SWI) at diagnosis can demonstrate the perivenular orientation of lesions, which is helpful to distinguish between MS and ischemic lesions [30]. 3D-fluid attenuated inversion recovery (FLAIR) sequence is useful in diagnosis and monitoring of MS due to its ability to increase lesion’s visibility, as well as to detect cortical lesions [31]. The improved detection of posterior fossa lesions with 3D FLAIR might also obviate the need for axial T2 sequences [31]. 3D-T1 acquisition is useful for assessing changes in brain volume over time. While currently this parameter is likely to be qualitative in most of the reports, it may become quantitative, as the use of automated segmentation software becomes more widespread [32].
Head position
3D acquisitions mitigate the variability introduced by changes in head position by enabling readers to electronically re-slice the acquired image. However, this is not possible on all picture archiving and communication systems (PACS). Therefore, in this eventuality and, more importantly, for serial MRI scans using 2D acquisitions, the position of the patient within the magnet bore is important for between-study comparison. Differences in head position between scans can significantly change the orientation of axial images, making comparisons difficult. The use of the anterior commissure–posterior commissure (AC–PC) line, defined as the line passing through the superior edge of the AC and the inferior edge of the PC, for aligning head position remains recommended [33] (Fig. 3).
Fig. 3.
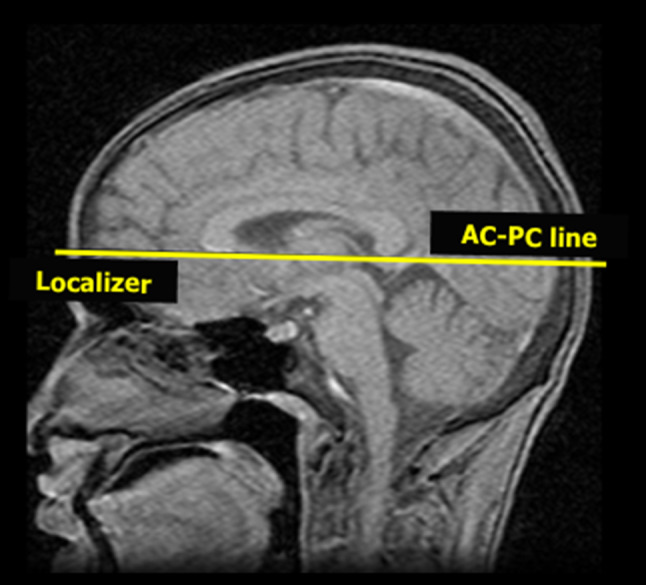
Head position during MRI acquisition. The anterior commissure–posterior commissure (AC–PC) line should be used to align head position to allow scan comparison, when only 2D acquisitions are possible. This line is typically ~ 9° steeper than the orbito-meatal line, traditionally used in computerised tomography (CT) scans. MRI magnetic resonance imaging, 2D 2 dimensional
Use of contrast agent
Gd is frequently used for its ability to highlight regions of altered blood–brain barrier and thus areas of active inflammation, thereby providing an indicator of current disease activity and a means to assess DMTs efficacy and safety in PML surveillance [1, 34]. However, evidence suggests a retention of Gd in the body, following a scan [35]. Therefore, the Gd for routine MRI scans should be used when necessary, with specific macrocyclic Gd agents being recommended over linear agents for safety reasons [36, 37]. Since Gd may be used both at diagnosis and during DMTs or natural history monitoring, the authors felt that, in line with published recommendation, Gd should be used only when deemed to be clinically necessary: (1) at diagnosis, (2) in cases of high lesion burden to identify new lesions, (3) to confirm the clinical suspicion of disease activity (e.g., worsening in disability, for which a relapse is suspected, but no clear episode is identifiable), and (4) where it may critically inform treatment decisions (e.g., assessment of treatment efficacy [21] or safety [38]).
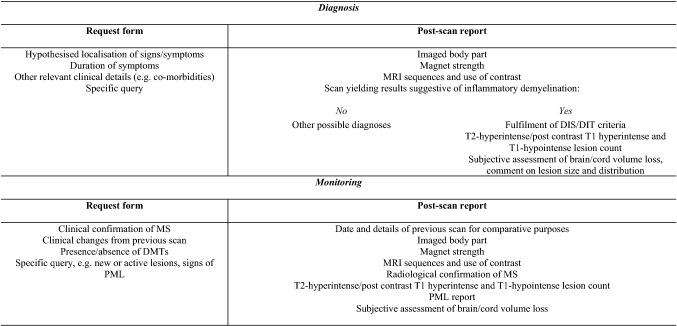
MRI scan requests and reports
With an increasing number of scans being performed for MS diagnosis and management, there is further need to streamline scan requests and reports. Table 2 reports the proposed essential components of request forms and post-scan reports identified by the authors. Reports should be prepared with sufficient detail to stand alone, should the MRI images be unavailable. The use of the term “progression” on radiological reports was felt by the authors to be inaccurate and thus to be discouraged, with “evidence of radiologically active disease” or “radiological evolution” proposed as alternative terminology.
Table 2.
MRI request forms and post-scan reports
The authors suggested that the clinician provides the neuroradiologist with relevant information about the individual patient and his history (left). The post-scan reports should contain information that would allow interpretability of the results (right)
DIT duration in time, DIS duration in space, MS multiple sclerosis, PML progressive multifocal leukoencephalopathy, DMTs disease-modifying treatments, MRI magnetic resonance imaging
MS lesion count
Whenever possible, absolute lesion counts should be reported, i.e., information about the number of T2-hyperintense, T1-hypointense and T1-hyperintense lesions in the post-contrast T1-weighted scans. This is relevant for both diagnostic, as well as monitoring scans [1]. Where there is high lesion load, especially if lesions are confluent, the authors felt that, although not ideal, a categorical approach to the number of T2-hyperintense lesions would be acceptable (e.g., less than 9 T2-hyperintense lesions, between 10 and 20 hyperintense lesions etc.). For monitoring scans, the detection of new lesions and/or changes in the size of pre-existing lesions should be indicated. Lesion number should be indicated separately for the brain and the spinal cord. Indication of lesion location should be given to support the diagnostic process, as well as to provide clinically meaningful indications on the current or future patients’ disability [39].
Brain and spinal cord volume
Comments on brain or spinal cord volumes should be provided in the report, at least as qualitative evaluation of the presence of MS-related tissue loss, by comparing the last scan with what expected in the normal, age-matched population, or as an assessment of the rate of volume reduction over time, by comparing the last scan with the first (or the most meaningful) available scan for the same patient.
Conclusions
In this report, we address the need for a standardisation of practice in the use of MRI for MS across clinical settings within the NHS. We suggest MRI scanning protocols and templates for MRI requests and post-scan reports in the attempt to facilitate diagnosis and optimise management of patients with MS, while considering the heterogeneity of resources and expertise that different clinical settings may present. The role of optic nerve imaging in MS was not discussed, as this is not currently included in the imaging diagnostic criteria for MS and, in MS monitoring, its informativeness is established by the clinician in each individual case [2].
Our proposed protocol aims to strike a balance between the need for frequent and accurate radiological information and the availability of equipment and staffing resources. The timing of MRI scans aims to capture, as early as possible, MS or its evolution that can be amenable to the starting or the changing of DMTs. The MRI acquisition protocol proposes a minimum, standardised set of meaningful information that can be used to manage MS. Indeed, published international guidelines offer guidance on MRI features that are most relevant to the diagnosis of MS [4]. Their implementation in clinical practice, however, has proven to be challenging across clinical settings, especially when the care of MS patients is outside specialist centres. Our proposed application of MRI for MS in clinical practice balances the specialist requirements with practical limitations imposed by limited resources by streamlining acquisition protocols and by standardising the timing of scans to integrate MRI findings in the clinical decision-making process. This effort can aid the impetus towards standardisation of practice and offer an example of research-informed service improvement to support optimisation of resources.
The authors also tackled the issue of effective communication between specialists, i.e., clinicians and radiologists, that is paramount in a multi-disciplinary context. We tailored our suggestions regarding the format of requests and reports for MRI scanning so that they can be used as a standardised, time-sparing tool for obtaining clinically relevant MRI information about MS patients. Indeed, the authors felt that clear, minimal information about the reason for the MRI scan was essential for the radiologist to correctly address the clinician’s question. Similarly, quantitative information about the MRI scan was felt to be necessary to manage MS effectively and promptly by clinicians. This quantitative, rather than merely descriptive, approach to MRI scan reporting for diagnostic, as well as for MRI monitoring scans, can contribute to an improved integration of MRI information in the clinical management of patients.
Acknowledgements
The London workshop in 2017 was funded by Novartis. The views expressed in this manuscript are those of the authors and not necessarily those of Novartis.
Author contributions
All the authors attended the workshop and provided intellectual contribution. All authors read and approved the final version of the manuscript.
Funding
The authors have no financial relationship with Novartis that sponsored a workshop leading to this publication and that supported further teleconferences between the authors.
Compliance with ethical standards
Conflicts of interest
Dr. Tomassini received honoraria to attend advisory boards and for lectures from Biogen, Novartis, Genzyme Sanofi. Dr. Sinclair received support for attending scientific meetings and speakers’ fees from Merck and Biogen. Dr Sawlani received honoraria to attend advisory boards and speaker fees from Novartis. Dr. Pearson received honoraria and support to attend scientific meetings, speakers’ fees and advisory boards from Biogen, Genzyme, Merck Serono, Novartis, Roche and Teva. Dr. Overell has received honoraria for speaking engagements and attendance at advisory boards, and conference travel support from Teva, Novartis, Merck Serono, Genzyme, Hoffmann-La Roche, Allergan, WebMD Global and Biogen. His Department has received educational funds, research support and funds to provide nursing and administrative staff from Novartis, Genzyme, Roche and Biogen. Since March 2019, he has been an employee and shareholder of F. Hoffmann-La Roche Ltd.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Footnotes
Valentina Tomassini and Audrey Sinclair have contributed equally to this work. Given their different expertise that is relevant to this work, they also share correspondence for this manuscript.
Contributor Information
Valentina Tomassini, Email: valentina.tomassini@unich.it.
Audrey Sinclair, Email: Audrey.Sinclair@stgeorges.nhs.uk.
References
- 1.Tomassini V, Palace J. Multiple sclerosis lesions: insights from imaging techniques. Expert Rev Neurother. 2009;9:1341–1359. doi: 10.1586/ern.09.83. [DOI] [PubMed] [Google Scholar]
- 2.Thompson AJ, Banwell BL, Barkhof F, Carroll WM, Coetzee T, Comi G, Correale J, Fazekas F, Filippi M, Freedman MS, Fujihara K, Galetta SL, Hartung HP, Kappos L, Lublin FD, Marrie RA, Miller AE, Miller DH, Montalban X, Mowry EM, Sorensen PS, Tintore M, Traboulsee AL, Trojano M, Uitdehaag BMJ, Vukusic S, Waubant E, Weinshenker BG, Reingold SC, Cohen JA. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018;17:162–173. doi: 10.1016/S1474-4422(17)30470-2. [DOI] [PubMed] [Google Scholar]
- 3.Wattjes MP, Rovira A, Miller D, Yousry TA, Sormani MP, de Stefano MP, Tintore M, Auger C, Tur C, Filippi M, Rocca MA, Fazekas F, Kappos L, Polman C, Frederik B, Xavier M. Evidence-based guidelines: MAGNIMS consensus guidelines on the use of MRI in multiple sclerosis–establishing disease prognosis and monitoring patients. Nat Rev Neurol. 2015;11:597–606. doi: 10.1038/nrneurol.2015.157. [DOI] [PubMed] [Google Scholar]
- 4.Filippi M, Rocca MA, Ciccarelli O, De Stefano N, Evangelou N, Kappos L, Rovira A, Sastre-Garriga J, Tintore M, Frederiksen JL, Gasperini C, Palace J, Reich DS, Banwell B, Montalban X, Barkhof F. MRI criteria for the diagnosis of multiple sclerosis: MAGNIMS consensus guidelines. Lancet Neurol. 2016;15:292–303. doi: 10.1016/S1474-4422(15)00393-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Traboulsee A, Simon JH, Stone L, Fisher E, Jones DE, Malhotra A, Newsome SD, Oh J, Reich DS, Richert N, Rammohan K, Khan O, Radue EW, Ford C, Halper J, Li D. Revised recommendations of the consortium of MS centers task force for a standardized MRI protocol and clinical guidelines for the diagnosis and follow-up of multiple sclerosis. AJNR Am J Neuroradiol. 2016;37:394–401. doi: 10.3174/ajnr.A4539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Filippi M, Rocca MA, Bastianello S, Comi G, Gallo P, Gallucci M, Ghezzi A, Marrosu MG, Minonzio G, Pantano P, Pozzilli C, Tedeschi G, Trojano M, Falini A, De Stefano N. Guidelines from The Italian Neurological and Neuroradiological Societies for the use of magnetic resonance imaging in daily life clinical practice of multiple sclerosis patients. Neurol Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol. 2013;34:2085–2093. doi: 10.1007/s10072-013-1485-7. [DOI] [PubMed] [Google Scholar]
- 7.Traboulsee A, Letourneau-Guillon L, Freedman MS, O'Connor PW, Bharatha A, Chakraborty S, Girard JM, Giuliani F, Lysack JT, Marriott JJ, Metz LM, Morrow SA, Oh J, Sharma M, Vandorpe RA, Vertinsky TA, Wadhwa VS, von Riedemann S, Li DK. Canadian Expert Panel recommendations for MRI use in MS diagnosis and monitoring. Can J Neurol Sci J Can Sci Neurol. 2015;42:159–167. doi: 10.1017/cjn.2015.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vagberg M, Axelsson M, Birgander R, Burman J, Cananau C, Forslin Y, Granberg T, Gunnarsson M, von Heijne A, Jonsson L, Karrenbauer VD, Larsson EM, Lindqvist T, Lycke J, Lonn L, Mentesidou E, Muller S, Nilsson P, Piehl F, Svenningsson A, Vrethem M, Wikstrom J. Guidelines for the use of magnetic resonance imaging in diagnosing and monitoring the treatment of multiple sclerosis: recommendations of the Swedish Multiple Sclerosis Association and the Swedish Neuroradiological Society. Acta Neurol Scand. 2017;135:17–24. doi: 10.1111/ane.12667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmierer K, Campion T, Sinclair A, van Hecke W, Matthews PM, Wattjes MP. Towards a standard MRI protocol for multiple sclerosis across the UK. Br J Radiol. 2019;92(1101):20180926. doi: 10.1259/bjr.20180926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fisniku LK, Brex PA, Altmann DR, Miszkiel KA, Benton CE, Lanyon R, Thompson AJ, Miller DH. Disability and T2 MRI lesions: a 20-year follow-up of patients with relapse onset of multiple sclerosis. Brain. 2008;131:808–817. doi: 10.1093/brain/awm329. [DOI] [PubMed] [Google Scholar]
- 11.Moccia M, Ruggieri S, Ianniello A, Toosy A, Pozzilli C, Ciccarelli O. Advances in spinal cord imaging in multiple sclerosis. Ther Adv Neurol Disord. 2019;12:1756286419840593. doi: 10.1177/1756286419840593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bot JC, Barkhof F, Nijeholt GLA, van Schaardenburg D, Voskuyl AE, Ader HJ, Pijnenburg JA, Polman CH, Uitdehaag BM, Vermeulen EG, Castelijns JA. Differentiation of multiple sclerosis from other inflammatory disorders and cerebrovascular disease: value of spinal MR imaging. Radiology. 2002;223:46–56. doi: 10.1148/radiol.2231010707. [DOI] [PubMed] [Google Scholar]
- 13.Bot JC, Barkhof F, Polman CH, Nijeholt GJLA, de Groot V, Bergers E, Ader HJ, Castelijns JA. Spinal cord abnormalities in recently diagnosed MS patients: added value of spinal MRI examination. Neurology. 2004;62:226–233. doi: 10.1212/WNL.62.2.226. [DOI] [PubMed] [Google Scholar]
- 14.Absinta M, Cortese IC, Vuolo L, Nair G, de Alwis MP, Ohayon J, Meani A, Martinelli V, Scotti R, Falini A, Smith BR, Nath A, Jacobson S, Filippi M, Reich DS. Leptomeningeal gadolinium enhancement across the spectrum of chronic neuroinflammatory diseases. Neurology. 2017;88:1439–1444. doi: 10.1212/WNL.0000000000003820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rotstein DL, Healy BC, Malik MT, Chitnis T, Weiner HL. Evaluation of no evidence of disease activity in a 7-year longitudinal multiple sclerosis cohort. JAMA Neurol. 2015;72:152–158. doi: 10.1001/jamaneurol.2014.3537. [DOI] [PubMed] [Google Scholar]
- 16.Sombekke MH, Wattjes MP, Balk LJ, Nielsen JM, Vrenken H, Uitdehaag BM, Polman CH, Barkhof F. Spinal cord lesions in patients with clinically isolated syndrome: a powerful tool in diagnosis and prognosis. Neurology. 2013;80:69–75. doi: 10.1212/WNL.0b013e31827b1a67. [DOI] [PubMed] [Google Scholar]
- 17.Paolillo A, Pozzilli C, Gasperini C, Giugni E, Mainero C, Giuliani S, Tomassini V, Millefiorini E, Bastianello S. Brain atrophy in relapsing-remitting multiple sclerosis: relationship with 'black holes', disease duration and clinical disability. J Neurol Sci. 2000;174:85–91. doi: 10.1016/S0022-510X(00)00259-8. [DOI] [PubMed] [Google Scholar]
- 18.Confavreux C, Hutchinson M, Hours MM, Cortinovis-Tourniaire P, Moreau T. Rate of pregnancy-related relapse in multiple sclerosis. Pregnancy in multiple sclerosis group. N Engl J Med. 1998;339:285–291. doi: 10.1056/NEJM199807303390501. [DOI] [PubMed] [Google Scholar]
- 19.Comi G, Filippi M, Wolinsky JS. European/Canadian multicenter, double-blind, randomized, placebo-controlled study of the effects of glatiramer acetate on magnetic resonance imaging–measured disease activity and burden in patients with relapsing multiple sclerosis. European/Canadian Glatiramer Acetate Study Group. Ann Neurol. 2001;49:290–297. doi: 10.1002/ana.64. [DOI] [PubMed] [Google Scholar]
- 20.Tomassini V, Paolillo A, Russo P, Giugni E, Prosperini L, Gasperini C, Antonelli G, Bastianello S, Pozzilli C. Predictors of long-term clinical response to interferon beta therapy in relapsing multiple sclerosis. J Neurol. 2006;253:287–293. doi: 10.1007/s00415-005-0979-5. [DOI] [PubMed] [Google Scholar]
- 21.Prosperini L, Gianni C, Barletta V, Mancinelli C, Fubelli F, Borriello G, Pozzilli C. Predictors of freedom from disease activity in natalizumab treated-patients with multiple sclerosis. J Neurol Sci. 2012;323:104–112. doi: 10.1016/j.jns.2012.08.027. [DOI] [PubMed] [Google Scholar]
- 22.Tortorella C, Bellacosa A, Paolicelli D, Fuiani A, Di Monte E, Simone IL, Giaquinto P, Livrea P, Trojano M. Age-related gadolinium-enhancement of MRI brain lesions in multiple sclerosis. J Neurol Sci. 2005;239:95–99. doi: 10.1016/j.jns.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 23.Sbardella E, Tomassini V, Stromillo ML, Filippini N, Battaglini M, Ruggieri S, Ausili Cefaro L, Raz E, Gasperini C, Sormani MP, Pantano P, Pozzilli C, De Stefano N. Pronounced focal and diffuse brain damage predicts short-term disease evolution in patients with clinically isolated syndrome suggestive of multiple sclerosis. Mult Scler. 2011;17:1432–1440. doi: 10.1177/1352458511414602. [DOI] [PubMed] [Google Scholar]
- 24.Lublin FD, Reingold SC, Cohen JA, Cutter GR, Sorensen PS, Thompson AJ, Wolinsky JS, Balcer LJ, Banwell B, Barkhof F, Bebo B, Jr, Calabresi PA, Clanet M, Comi G, Fox RJ, Freedman MS, Goodman AD, Inglese M, Kappos L, Kieseier BC, Lincoln JA, Lubetzki C, Miller AE, Montalban X, O'Connor PW, Petkau J, Pozzilli C, Rudick RA, Sormani MP, Stuve O, Waubant E, Polman CH. Defining the clinical course of multiple sclerosis: the 2013 revisions. Neurology. 2014;83:278–286. doi: 10.1212/WNL.0000000000000560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Losseff NA, Webb SL, Oriordan JI, Page R, Wang L, Barker GJ, Tofts PS, McDonald WI, Miller DH, Thompson AJ. Spinal cord atrophy and disability in multiple sclerosis. A new reproducible and sensitive MRI method with potential to monitor disease progression. Brain. 1996;119(Pt 3):701–708. doi: 10.1093/brain/119.3.701. [DOI] [PubMed] [Google Scholar]
- 26.Oshima Y, Tanimoto T, Yuji K, Tojo A. Drug-associated progressive multifocal leukoencephalopathy in multiple sclerosis patients. Mult Scler. 2019;25:1141–1149. doi: 10.1177/1352458518786075. [DOI] [PubMed] [Google Scholar]
- 27.Plavina T, Subramanyam M, Bloomgren G, Richman S, Pace A, Lee S, Schlain B, Campagnolo D, Belachew S, Ticho B. Anti-JC virus antibody levels in serum or plasma further define risk of natalizumab-associated progressive multifocal leukoencephalopathy. Ann Neurol. 2014;76:802–812. doi: 10.1002/ana.24286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kappos L, Bates D, Edan G, Eraksoy M, Garcia-Merino A, Grigoriadis N, Hartung HP, Havrdova E, Hillert J, Hohlfeld R, Kremenchutzky M, Lyon-Caen O, Miller A, Pozzilli C, Ravnborg M, Saida T, Sindic C, Vass K, Clifford DB, Hauser S, Major EO, O'Connor PW, Weiner HL, Clanet M, Gold R, Hirsch HH, Radu EW, Sorensen PS, King J. Natalizumab treatment for multiple sclerosis: updated recommendations for patient selection and monitoring. Lancet Neurol. 2011;10:745–758. doi: 10.1016/S1474-4422(11)70149-1. [DOI] [PubMed] [Google Scholar]
- 29.McGuigan C, Craner M, Guadagno J, Kapoor R, Mazibrada G, Molyneux P, Nicholas R, Palace J, Pearson OR, Rog D, Young CA. Stratification and monitoring of natalizumab-associated progressive multifocal leukoencephalopathy risk: recommendations from an expert group. J Neurol Neurosurg Psychiatry. 2016;87:117–125. doi: 10.1136/jnnp-2016-315106.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sati P, Oh J, Constable RT, Evangelou N, Guttmann CR, Henry RG, Klawiter EC, Mainero C, Massacesi L, McFarland H, Nelson F, Ontaneda D, Rauscher A, Rooney WD, Samaraweera AP, Shinohara RT, Sobel RA, Solomon AJ, Treaba CA, Wuerfel J, Zivadinov R, Sicotte NL, Pelletier D, Reich DS. The central vein sign and its clinical evaluation for the diagnosis of multiple sclerosis: a consensus statement from the North American Imaging in Multiple Sclerosis Cooperative. Nat Rev Neurol. 2016;12:714–722. doi: 10.1038/nrneurol.2016.166. [DOI] [PubMed] [Google Scholar]
- 31.Patzig M, Burke M, Bruckmann H, Fesl G. Comparison of 3D cube FLAIR with 2D FLAIR for multiple sclerosis imaging at 3 Tesla. RoFo Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin. 2014;186:484–488. doi: 10.1055/s-0033-1355896. [DOI] [PubMed] [Google Scholar]
- 32.Lysandropoulos AP, Absil J, Metens T, Mavroudakis N, Guisset F, Van Vlierberghe E, Smeets D, David P, Maertens A, Van Hecke W. Quantifying brain volumes for multiple sclerosis patients follow-up in clinical practice—comparison of 1.5 and 3 Tesla magnetic resonance imaging. Brain Behav. 2016;6:e00422. doi: 10.1002/brb3.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weiss KL, Pan H, Storrs J, Strub W, Weiss JL, Jia L, Eldevik OP. Clinical brain MR imaging prescriptions in Talairach space: technologist- and computer-driven methods. AJNR Am J Neuroradiol. 2003;24:922–929. [PMC free article] [PubMed] [Google Scholar]
- 34.Wijburg MT, Witte BI, Vennegoor A, Roosendaal SD, Sanchez E, Liu Y, Martins Jarnalo CO, Uitdehaag BM, Barkhof F, Killestein J, Wattjes MP. MRI criteria differentiating asymptomatic PML from new MS lesions during natalizumab pharmacovigilance. J Neurol Neurosurg Psychiatry. 2016;87:1138–1145. doi: 10.1136/jnnp-2016-313772. [DOI] [PubMed] [Google Scholar]
- 35.McDonald RJ, McDonald JS, Kallmes DF, Jentoft ME, Paolini MA, Murray DL, Williamson EE, Eckel LJ. Gadolinium deposition in human brain tissues after contrast-enhanced MR imaging in adult patients without intracranial abnormalities. Radiology. 2017;285:546–554. doi: 10.1148/radiol.2017161595. [DOI] [PubMed] [Google Scholar]
- 36.European Medicine Agency (2017) EMA's final opinion confirms restrictions on use of linear gadolinium agents in body scans. In: https://www.ema.europa.eu/en/medicines/human/referrals/gadolinium-containing-contrast-agents. Accessed 27 May 2020
- 37.US Food and Drug Administration (2017). FDA warns that gadolinium-based contrast agents (GBCAs) are retained in the body. In: https://www.fda.gov/drugs/drug-safety-and-availability/fda-drug-safety-communication-fda-warns-gadolinium-based-contrast-agents-gbcas-are-retained-body. Accessed 27 May 2020
- 38.Wattjes MP, Barkhof F. Diagnosis of natalizumab-associated progressive multifocal leukoencephalopathy using MRI. Curr Opin Neurol. 2014;27:260–270. doi: 10.1097/WCO.0000000000000099. [DOI] [PubMed] [Google Scholar]
- 39.Prosperini L, Kouleridou A, Petsas N, Leonardi L, Tona F, Pantano P, Pozzilli C. The relationship between infratentorial lesions, balance deficit and accidental falls in multiple sclerosis. J Neurol Sci. 2011;304:55–60. doi: 10.1016/j.jns.2011.02.014. [DOI] [PubMed] [Google Scholar]