Introduction
While the safety of healthcare workers during this pandemic has been of primary concern, emergency responders deserve special and unique considerations. Chronic diseases associated with increased risk of COVID-related mortality are common among the >2 million US firefighters, police officers, and emergency medical services (EMS) personnel 1, 2, 3. More importantly, nearly a quarter of EMS personnel are >50 years old and seven percent are >60 years old 1.
Strategies to protect first responders
While the following policies are not prescriptive, they may be useful in guiding organizations to develop safety protocols for emergency responders. Based on a limited understanding of the disease, it may be reasonable to restrict first responders older than 65 years from direct community engagement. Partial work restrictions may be considered for emergency responders over 60 years with cardiovascular disease, poorly controlled hypertension (e.g. BP > 130/80), diabetes (HbA1c >8%), obesity, and chronic pulmonary conditions. This restriction may also extend to younger individuals with unrevascularized obstructive coronary artery disease, moderate-severe valvular disease, history of ventricular arrhythmias or heart failure. Those below 60 years with low risk cardiovascular disease may be allowed to work without restriction. This includes individuals with well-controlled hypertension, dyslipidemia, diabetes, revascularized coronary artery disease and no evidence of inducible ischemia, mild valvular disease and paroxysmal atrial fibrillation.
While we recognize these recommendations may result in staffing shortages, partial restrictions may offset some of these logistical concerns. For example, it may be possible to restrict many with underlying chronic conditions to office, rather than field work.
Returning to work after COVID-19 infection
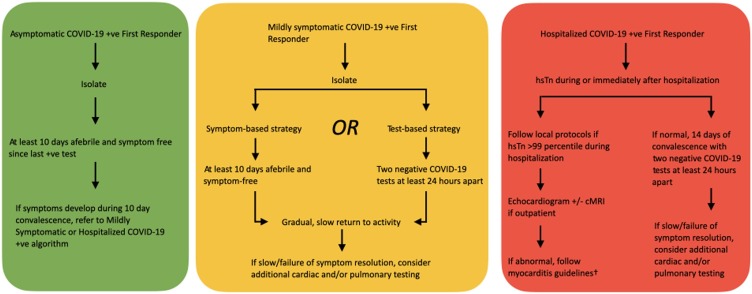
For first responders, this decision should be centered not only on the potential of an individual to infect others but also whether it is safe to perform high levels of physical activity. It is possible that silent myocardial and coronary inflammation persists long after symptom resolution, and may act as a harbinger for an adverse cardiac event especially while performing high levels of physical activity 4. Therefore, we suggest a strategy that includes a period of convalescence, followed by a symptom-based or test-based screen to determine eligibility to return-to-work (Fig. 1 ).
Fig. 1.
Title: Cardiovascular Considerations to Return to Work for First Responders in the COVID-19 Era. †We recommend the American College of Cardiology/American Heart Association Athlete myocarditis guidelines 5. hsTn: high-sensitivity troponin-I; cMRI: cardiac MRI; COVID-19: Coronavirus Disease of 2019.
Symptomatic first responders who have a positive COVID-19 test should self-isolate for at least 10–14 days from the date of positive test. Prior to resuming work, they should be carefully evaluated for ongoing symptoms and a subsequent slow resumption of activity. A resting 12-lead electrocardiogram and a high-sensitivity troponin test should be considered for those with COVID-19 related hospitalization. An echocardiogram should be performed based on a concerning initial evaluation with additional testing such as cardiac magnetic resonance imaging and ambulatory rhythm monitoring when appropriate. If there remains a concern for cardiac involvement, the American Heart Association/American College of Cardiology return-to-play document for athletes with myocarditis provides a useful reference 5.
Conclusion
Emergency responders present distinct challenges due to the unpredictable nature of their work environments. Introducing restrictions for the most vulnerable, adopting widespread testing and return to work evaluations may help protect emergency responders during the pandemic.
Consent
N/A
Author contributions
P.R, E.F, E.H.C, B.D.L and S.M.I made substantial contributions to the conception or design of the research or the acquisition and analysis of data. P.R, E.F, E.H.C, B.D.L and S.M.I all contributed to the drafting of the work or revising it critically for important intellectual content.
Funding
None.
Ethical approval
N/A.
Registry and the registration No. Of the study/Trial
N/A.
Animal studies
N/A.
Disclosures
S.M.I is the Medical Director of the University of Texas Southwestern/Parkland BioTel Emergency Medical Services System and the Medical Director of the Dallas Fire-Rescue Department.
References
- 1.National Association of State EMS Officials . 2020. 2020 National Emergency Medical Services Assessment. [Google Scholar]
- 2.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Soteriades E.S., Hauser R., Kawachi I., Liarokapis D., Christiani D.C., Kales S.N. Obesity and cardiovascular disease risk factors in firefighters: a prospective cohort study. Obes Res. 2005;13:1756–1763. doi: 10.1038/oby.2005.214. [DOI] [PubMed] [Google Scholar]
- 4.Puntmann V.O., Carerj M.L., Wieters I., Fahim M., Arendt C., Hoffmann J. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19) JAMA Cardiol. 2020 doi: 10.1001/jamacardio.2020.3557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maron B.J., Udelson J.E., Bonow R.O., Nishimura R.A., Ackerman M.J., Estes N.A.M., 3rd Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities: Task Force 3: Hypertrophic Cardiomyopathy, Arrhythmogenic Right Ventricular Cardiomyopathy and Other Cardiomyopathies, and Myocarditis: A Scientif. J Am Coll Cardiol. 2015;66:2362–2371. doi: 10.1016/j.jacc.2015.09.035. [DOI] [PubMed] [Google Scholar]