Abstract
Objectives
Smoking remains a leading public health issue and health care practitioners (HCPs), who play an important role in supporting and promoting patients’ cessation efforts, need educational initiatives that improve their ability to provide effective clinical care. The objective of this study was to compare patient-reported abstinence from smoking following treatment by HCPs trained in an intensive tobacco cessation program and those trained in less intensive programs.
Methods
A secondary data analysis of two overlapping samples of patients who received most of their treatment from one identifiable HCP (n = 26,590) or all of their treatment from one identifiable HCP (n = 20,986) was assessed. Patients were residents of Ontario, Canada, who enrolled in a publicly funded smoking cessation treatment program between 01 May 2014 and 31 October 2016 and completed the 7-day point prevalence of smoking question at 6-month follow-up. Treatment was provided by HCPs who engaged in the intensive Training Enhancement in Applied Counselling and Health (TEACH) Core course, or those who engaged in one or more other training programs. Generalized estimating equation (GEE) logistic regression was used to compare smoking abstinence between groups.
Results
After adjustment for both patient- and practice-level covariates, a significant association was found between being treated by a TEACH-trained HCP and the likelihood of smoking abstinence at 6-month follow-up in both analytic samples (most care sample: OR = 1.10, 95% CI = 1.01, 1.20; all care sample: OR = 1.12, 95% CI = 1.02, 1.24).
Conclusion
Implementation of comprehensive cessation training to support HCP delivery of smoking cessation treatment should be considered to improve patient outcomes.
Keywords: Smoking cessation, Treatment outcome, Professional education, Tobacco use disorder
Résumé
Objectifs
Le tabagisme demeure l’un des principaux problèmes de santé publique et les praticiens des soins de santé (PSS), qui jouent un rôle important en encourageant et en aidant leurs patients à cesser de fumer, ont besoin de programmes de formation pour améliorer leur capacité à prodiguer des soins cliniques efficaces. La présente étude a pour but de comparer l’abstinence tabagique déclarée par les patients traités par un PSS formé dans le cadre d’un programme intensif d’abandon du tabac et celle déclarée par des patients traités par un PSS formé dans le cadre d’un programme moins intensif.
Méthodes
On a évalué l’analyse de données secondaires portant sur deux échantillons chevauchants de patients ayant reçu la majeure partie de leur traitement d’un seul PSS identifiable (n = 26 590) ou la totalité de leur traitement d’un seul PSS identifiable (n = 20 986). Les patients résidaient en Ontario, au Canada, et s’étaient inscrits à un programme d’abandon du tabac financé à même les deniers publics, entre le 1er mai 2014 et le 31 octobre 2016, et, six mois plus tard, avaient rempli le questionnaire de suivi de sept jours sur la prévalence ponctuelle du tabagisme. Le traitement avait été fourni par des PSS qui avaient suivi le cours intensif de base du programme TEACH (Training Enhancement in Applied Counselling and Health), ou par ceux qui avaient participé à un ou plusieurs autres programmes de formation. Pour comparer l’abstinence tabagique entre les groupes, on s’est servi de la régression logistique à l’aide d’un modèle d’équation d’estimation généralisée (EEG).
Résultats
Après rajustement en fonction des covariantes au niveau des patients et des cabinets, on a observé une association significative entre les patients traités par un PSS ayant participé au programme TEACH et la probabilité d’une abstinence tabagique dans le cadre du suivi de six mois, et ce, dans les deux échantillons analysés (échantillon de patients ayant reçu la majeure partie de leur traitement d’un tel PSS : RC = 1,10, IC à 95 % = 1,01, 1,20; échantillon de patients ayant reçu la totalité de leur traitement d’un tel PSS : RC =1,12, IC à 95% =1,02, 1,24).
Conclusion
On devrait envisager la possibilité d’offrir une formation complète sur l’abandon du tabagisme en vue d’appuyer les PSS qui traitent des patients désireux d’arrêter de fumer et d’améliorer ainsi les résultats pour la santé de ces derniers.
Mots-clés: Abandon du tabagisme, résultats du traitement, formation professionnelle, trouble de l’usage du tabac
Introduction
Smoking remains the second leading risk factor of preventable death and disability worldwide, accounting for 7.1 million deaths and 182 million disability-adjusted life-years (DALYs) in 2017 (Stanaway et al. 2018), with direct or indirect global costs of smoking in 2012 estimated at US$1.4 trillion (Goodchild et al. 2018). In Ontario, Canada, smoking was associated with the highest risk of mortality, compared with other health factors (i.e., alcohol consumption, physical inactivity, and unhealthy body mass index; Rosella et al. 2019). Despite progress in reducing prevalence, 16.2%, or 5 million Canadians, aged 12 years and over reported that they were current daily or occasional smokers in 2017 (Statistics Canada 2017).
Most smokers want to quit (Hyland et al. 2006), but only 3–5% of untreated smokers who make a quit attempt achieve abstinence (Hughes et al. 2004). There is substantial evidence to support the use of pharmacological (e.g., varenicline, bupropion, or nicotine replacement therapy (NRT)), psychological (e.g., behavioural support), and combined pharmacological and psychological treatment methods to treat tobacco addiction (West et al. 2015; Stead et al. 2016). Even brief interventions, such as advice from a health care practitioner (HCP), have been shown to be effective. This evidence is in line with current clinical guidelines which recommend that HCPs discuss cessation treatment with tobacco users at every clinical visit and incorporate five key behaviour change components into practice (i.e., the 5As: ask, advise, assess, assist, and arrange; Fiore et al. 2008; CAN-ADAPTT 2011). Despite existing guidelines and evidence-based treatments, implementation of these approaches remains inconsistent in clinical settings and HCPs report challenges with implementation in practice, such as lack of perceived knowledge and skills, and training to support the delivery of such interventions is limited (Vogt et al. 2005; Ye et al. 2017; Papadakis et al. 2014). These challenges are reflected in the 2017 Cochrane Tobacco Addiction Group priority-setting report, in which treatment delivery, per se, was ranked as an urgent topic area for future research, and, specifically, questions regarding the training HCPs need to be most effective were recognized as a priority (Lindson et al. 2017).
Training of HCPs to provide tobacco dependence treatment has demonstrated clinically significant effects on patient smoking cessation outcomes (Carson et al. 2012). However, most studies have focused on measuring outcomes at the practitioner level, such as HCP commitment to change behaviours or implementation of newly acquired skills in the clinical setting (Shershneva et al. 2011). Fewer studies report on patient-level smoking cessation outcomes, which reflect the ultimate goal of providing patients with help to quit smoking and may provide a better understanding of the efficacy of any given HCP training program. Given the chronic relapsing nature of tobacco addiction combined with comorbidities that could negatively affect quit outcomes, comprehensive, intensive training programs, which include a focus on how to appropriately modify treatment approaches to specific populations, may be particularly beneficial to increase HCP knowledge and skills (Ye et al. 2017).
The objective of this study was to compare the smoking cessation outcomes of patients treated by HCPs trained in an intensive tobacco cessation training program with those of HCPs trained in other less intensive training programs.
Methods
Study design/setting
We conducted a secondary data analysis within a cohort of people who sought smoking cessation treatment via the Smoking Treatment for Ontario Patients (STOP) program.
Study population and analytic sample
The STOP program is a publicly funded smoking cessation treatment program that provides no-cost NRT in combination with brief behavioural counselling by trained HCPs to approximately 25,000 patients per year in over 300 organizations providing medical care, in Ontario, Canada. The program is offered in four clinical practice settings: family health teams (FHTs), community health centres (CHCs), addiction agencies (AAs), and nurse practitioner-led clinics (NPLCs). FHTs, CHCs, and NPLCs are team-based primary health care organizations that offer health services and programs to communities throughout the province of Ontario, and AAs are centres specializing in providing assessment, treatment, or services for substance use disorders and related problems. Patients are cigarette smokers who primarily want help quitting smoking. There are no age exclusions; minors may enroll with the consent of their parent or legal guardian. It is a real-world, pragmatic, smoking cessation program in which treatment is individually tailored. Clinical care visit frequency can vary according to available resources and treatment may be provided by one or more trained HCPs. As part of the program, patients can receive up to a maximum of 26 weeks of NRT within a 52-week enrollment period.
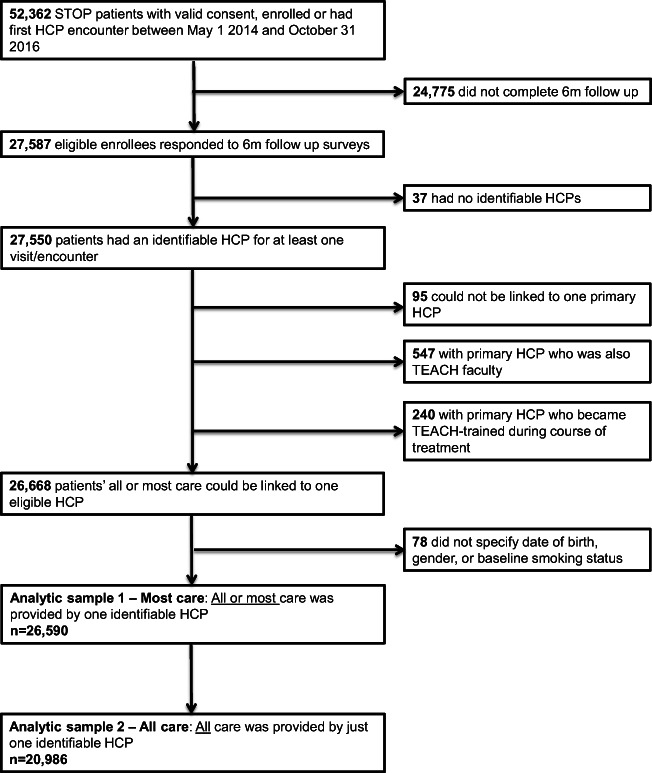
Patients included in the analytic sample (Fig. 1) were residents of Ontario who had enrolled in the STOP program between 01 May 2014 and 31 October 2016 and answered the 7-day point prevalence smoking question in the 6-month follow-up survey. The follow-up survey was completed by 53% of program enrollees. Several exclusion criteria related to the ability to link each patient to their HCP were necessary. We excluded patients for whom no identifiable HCP could be determined for any treatment visit (e.g., those patients for whom the only name noted is that of STOP program non-clinical staff who performed data entry) and those for whom no single identifiable HCP could be determined to have provided most or all treatment (e.g., patients who had an equal number of treatment visits with multiple HCPs, none of whom provided care at the inherently more intensive enrollment visit). Of those patients who were successfully linked to one HCP who provided most or all treatment, two additional exclusions were made: (1) patients whose linked HCP was faculty within the intensive tobacco cessation training program (described below), because although the HCP had advanced skills in particular area(s) included in the training program (e.g., pharmacotherapy), they were not required to complete any additional training to implement the STOP program; and (2) patients whose linked HCP completed the intensive tobacco cessation training program during the course of treatment with the patient in question. Furthermore, patients whose age, gender, or baseline smoking status was unknown were also excluded.
Fig. 1.
Analytic sample derivation
We undertook analyses of two overlapping patient samples: (1) most care sample: patients who received most of their treatment from one identifiable HCP (n = 26,590); and (2) all care sample: the subsample of patients who received all of their treatment from just one identifiable HCP (n = 20,986). Most treatment by a HCP was defined as care provided by one identifiable HCP at more clinical encounters than any other HCP. If a patient had the same number of encounters with an equal number of HCPs, the HCP providing most treatment was designated as the HCP who conducted the patient’s baseline enrollment, as those visits inherently included more clinical interaction. A flowchart with details of derivation of the two analytic samples is presented in Fig. 1.
Exposure
The comparison of interest was between patients treated by Training Enhancement in Applied Counselling and Health (TEACH)-trained HCPs and those who were treated by HCPs who received other training as described below.
In order to provide cessation interventions to their patients, all HCPs implementing the STOP program are required to complete at least one of the following training programs, or others that may be approved on an ad hoc basis: TEACH (Herie et al. 2012) Core course: An Interprofessional Comprehensive Course on Treating Tobacco Use Disorder; Fundamentals of Tobacco Intervention (FTI; Selby et al. 2012); Ottawa Model for Smoking Cessation (OMSC; Reid et al. 2010); Best Practice Champions (Registered Nurses’ Association of Ontario 2012); or Quit Using and Inhaling Tobacco (QUIT; Canadian Pharmacists Association 2006). Of all HCPs implementing STOP, 58%, 37%, 17%, 10%, and 2% reported completion of the TEACH Core course, FTI, OMSC, Best Practice Champions, and QUIT trainings, respectively; 11% of HCPs reported completion of other trainings and 33.3% reported completion of more than one training.
These training programs vary in terms of content, delivery format, time commitment, level of engagement, and evaluation. The TEACH Core course fosters skills in intensive tobacco cessation interventions in the areas of screening, assessment, and treatment methods. HCP participants proceed through key content areas in tobacco cessation, engage in interdisciplinary group discussions, and complete assessments over 19.5 university-accredited course hours. The course was offered in person over 3 days from 2007 to 2016 or online over 5 weeks from 2015 to the present time. Participants must achieve a score of at least 70% on a final examination to complete the course. Given this interdisciplinary approach to learning, detailed presentation of evidence-based treatment strategies, opportunities to practise the application of these strategies, and methods of evaluation, this program presents a comprehensive training opportunity. FTI is a self-study course adapted from the Core course, which includes three brief online modules on tobacco cessation counselling and pre- and post-course learning self-assessments. While covering content similar to the FTI, OMSC offers optional training in different formats: a 3-day conference, 1-day workshop, or five brief online courses. Best Practice Champions offered by the Registered Nurses’ Association of Ontario (RNAO) does not focus on tobacco cessation specifically, but centres on how to implement evidence-based practices in a variety of clinical practice settings, and may include completion of one of three trainings: a 1-day workshop, brief online module, or single session webinar. QUIT is an accredited, self-directed online program offered by the Canadian Pharmacists Association (CPhA) in order to enhance delivery of both behavioural and pharmacological smoking cessation services in pharmacy settings. Completion of this program involves six modules, assessment activities, and earning a score of at least 70% on a final test.
Of note, all HCPs implementing the STOP program have access to multiple avenues of support, including one-on-one communications with STOP program staff, and group communication with STOP program staff and other implementing HCPs during twice-monthly program teleconferences. Additionally, TEACH offers participation in continuing professional development through monthly webinars and a community of practice listserv available to all HCPs implementing the STOP program.
Outcome measure
The study outcome was self-reported past 7-day point prevalence of abstinence from smoking, measured at the 6-month follow-up survey by the question, “Have you had a cigarette, even a puff, in the last seven days?” with possible responses of “yes” or “no.” There is evidence to support the validity of self-reported survey items to approximate biochemical measures of abstinence from smoking (Wong et al. 2012). Attempts to follow up with all STOP patients were made, except for those who had died or withdrew from the study prior to the 6-month follow-up period. Follow-ups were conducted via emailed surveys, over the phone, or in person during clinical visits. The 6-month follow-up was chosen as our outcome, despite the program enrollment eligibility being 12 months, to reflect the recommended reporting standard (Piper et al. 2019). Furthermore, as the program allows for 26 weeks of medication, even patients who use this entire supply would complete treatment within 6 months of enrollment, and unpublished STOP program data show that few patients continue their treatment trajectory beyond the first 6 months.
Covariates
The following covariates were treated as potential confounders: patient’s age, gender, household income, educational attainment, current employment, baseline daily smoking status, willingness to set a quit date within the next 30 days, past year quit attempt, marijuana use in the past 30 days, opioid use in the past 30 days, alcohol consumption in the past year, lifetime self-reported history of heart disease or heart problems, diabetes, chronic bronchitis, emphysema, or chronic obstructive pulmonary disease (COPD), cancer (any type), depression, anxiety, schizophrenia, bipolar disorder, depression score as measured by the Patient Health Questionnaire (PHQ-9; Spitzer et al. 1999), practice setting type, cumulative duration of clinic STOP program operations at the time of patient enrollment, and cumulative number of STOP program patients ever enrolled at that clinic at the time of patient enrollment. Information on all patient-level covariates was collected via a self-reported survey at the time of enrollment into the STOP program. Practice setting covariates were derived from STOP program administrative data. Excluding age, gender, and baseline smoking status, all missing covariate data were assigned the same value (i.e., the lowest exposure level).
Summary of smoking cessation treatment
Summary of treatment variables examined included total number of treatment visits, total number of long-acting NRT boxes dispensed (which included patches of 7 mg, 14 mg, and 21 mg variety), total number of short-acting NRT boxes dispensed (which included lozenge, inhaler, gum, or mouth spray), type of NRT received during cumulative treatment, cumulative weeks of NRT dispensed, and amount of NRT dispensed in milligrams (calculated based on number of boxes dispensed). Treatment information was summarized from the first 6 months of treatment following enrollment because the study outcome was assessed at 6-month follow-up.
Statistical analysis
The statistical analysis for each of the two analytic samples followed the same procedures. To determine whether exposure to a TEACH-trained HCP was associated with the likelihood of smoking abstinence at the 6-month follow-up, we employed generalized estimating equation (GEE) logistic regression to account for clustering of patients within clinics and specified an exchangeable correlation matrix and robust standard errors. All covariates were determined a priori and were included in the model to account for possible confounding. Summary of treatment received, separated for each sample, by exposure, is presented for descriptive purposes only; treatment characteristics were not treated as potential confounders of the association between being treated by a comprehensively trained HCP and smoking abstinence because they may, in fact, be at least partial mediators of that relationship. All analyses were conducted in 2018 using Stata, version 14.2.
Results
Descriptive characteristics of the patients in each sample, by HCP TEACH training status, are presented in Table 1. Patients of TEACH-trained and non-TEACH-trained HCPs were similar in both samples, with a few exceptions. Patients of TEACH-trained HCPs were more likely to have completed high school and have a lifetime history of emphysema or COPD diagnosis. In the most care sample, practice settings with TEACH-trained HCPs had enrolled slightly fewer patients over their duration of operations overall, compared with settings with non-TEACH-trained HCPs. However, practice settings with TEACH-trained HCPs had been implementing the STOP program longer in both care samples.
Table 1.
Sample characteristics at enrollment, separated by analytic sample
| Sample 1: One practitioner conducted most of the visits (n = 26,590) |
Sample 2: One practitioner conducted all of the visits (n = 20,986) |
|||
|---|---|---|---|---|
| Not TEACH | Yes TEACH | Not TEACH | Yes TEACH | |
| n = 8869 | n = 17,721 | n = 6568 | n = 14,418 | |
| Patient-level characteristics | ||||
| Age in years (mean (sd)) | 52.2 (13.3) | 52.8 (13.3) | 52.0 (13.4) | 52.7 (13.4) |
| Male (n (%)) | 4166 (47.0%) | 8166 (46.1%) | 3058 (46.6%) | 6581 (45.6%) |
| Completed high school or less (n (%)) | 4041 (45.6%) | 8538 (48.2%) | 3054 (46.5%) | 7037 (48.8%) |
| Household income $40k or less (n (%)) | 3651 (41.2%) | 7445 (42.0%) | 2574 (39.2%) | 5874 (40.7%) |
| Currently employed (n (%)) | 3552 (40.0%) | 6959 (39.3%) | 2743 (41.8%) | 5863 (40.7%) |
| Daily smoking status (n (%)) | 8165 (92.1%) | 16,191 (91.4%) | 6090 (92.7%) | 13,247 (91.9%) |
| Had a past year quit attempt (n (%)) | 4633 (52.2%) | 9339 (52.7%) | 3377 (51.4%) | 7555 (52.4%) |
| Willing to set quit date within the next 30 days (n (%)) | 6569 (74.1%) | 13,074 (73.8%) | 4848 (73.8%) | 10,627 (73.7%) |
| Marijuana use in the past 30 days (any) (n (%)) | 1728 (19.5%) | 3299 (18.6%) | 1258 (19.2%) | 2675 (18.6%) |
| Opioid use in the past 30 days (any) (n (%)) | 1506 (17.0%) | 3161 (17.8%) | 1126 (17.1%) | 2497 (17.3%) |
| Consumed alcohol in the past year (n (%)) | 6169 (69.6%) | 12,653 (71.4%) | 4631 (70.5%) | 10,360 (71.8%) |
| Heart disease or heart problemsa (n (%)) | 1221 (13.8%) | 2498 (14.1%) | 925 (14.1%) | 1981 (13.7%) |
| Diabetesa (n (%)) | 1315 (14.8%) | 2717 (15.3%) | 958 (14.6%) | 2220 (15.4%) |
| Chronic bronchitis, emphysema, or COPDa (n (%)) | 2099 (23.7%) | 4562 (25.7%) | 1557 (23.7%) | 3674 (25.5%) |
| Cancer (any type)a (n (%)) | 660 (7.4%) | 1424 (8.0%) | 483 (7.4%) | 1160 (8.0%) |
| Depressiona (n (%)) | 3393 (38.3%) | 6952 (39.2%) | 2456 (37.4%) | 5537 (38.4%) |
| Anxietya (n (%)) | 3161 (35.6%) | 6361 (35.9%) | 2288 (34.8%) | 5094 (35.3%) |
| Schizophreniaa (n (%)) | 306 (3.4%) | 634 (3.6%) | 187 (2.8%) | 480 (3.3%) |
| Bipolar disordera (n (%)) | 551 (6.2%) | 1246 (7.0%) | 371 (5.6%) | 937 (6.5%) |
| PHQ-9 depression score (Mdn (IQR)) | 0 (0–2) | 0 (0–2) | 0 (0–2) | 0 (0–2) |
| Practice setting characteristics | ||||
| Organization type (n (%)) | ||||
| AA | 1201 (13.5%) | 2061 (11.6%) | 781 (11.9%) | 1412 (9.8%) |
| CHC | 1021 (11.5%) | 2975 (16.8%) | 693 (10.6%) | 2414 (16.7%) |
| FHT | 6302 (71.1%) | 12,404 (70.0%) | 4847 (73.8%) | 10,357 (71.8%) |
| NPLC | 345 (3.9%) | 281 (1.6%) | 247 (3.8%) | 235 (1.6%) |
| Total months since organization implemented STOP programb (Mdn (IQR)) | 39.4 (26.2–49.4) | 41.5 (29.4–51.2) | 40.1 (26.7–50.0) | 41.9 (30.5–51.5) |
| Cumulative number of patients enrolled at clinicb (Mdn (IQR)) | 359 (174–885) | 355 (167–654) | 372 (169–940) | 356 (167–680) |
aPatients were asked if they had ever been diagnosed by a health professional
bAt time of enrollment of each patient
AA, addiction agency; CHC, community health centre; COPD, chronic obstructive pulmonary disease; FHT, family health team; IQR, interquartile range; Mdn, median; NPLC, nurse practitioner-led clinic; PHQ-9, Patient Health Questionnaire
Summary of smoking treatment, separated by analytic sample and TEACH training status, is presented in Table 2. Patients of TEACH-trained HCPs had more clinical visits and received more cumulative milligrams of NRT (both samples). In the all care sample only, patients of TEACH-trained HCPs had more cumulative weeks of NRT and boxes of long-acting NRT.
Table 2.
Summary of treatment received in the first 6 months following enrollment
| Sample 1: One practitioner conducted most of the visits (n = 26,590) |
Sample 2: One practitioner conducted all of the visits (n = 20,986) |
|||
|---|---|---|---|---|
| Not TEACH | Yes TEACH | Not TEACH | Yes TEACH | |
| n = 8869 | n = 17,721 | n = 6568 | n = 14,418 | |
| Total number of visits/clinical encounters (Mdn (IQR)) | 3 (1–5) | 4 (2–6) | 2 (1–5) | 3 (2–6) |
| Total number of patches (long-acting) boxes dispensed (Mdn (IQR)) | 8 (3–15) | 8 (3–16) | 6 (2–12) | 7 (3–15) |
| Total number of short-acting boxes dispensed (Mdn (IQR)) | 3 (1–5) | 3 (1–6) | 2 (1–4) | 2 (1–5) |
| Total number of cumulative weeks of NRT dispensed (Mdn (IQR)) | 8 (4–15) | 8 (4–16) | 6 (3–12) | 7 (4–15) |
| Type of NRT received (n (%)) | ||||
| Patches | 647 (7.3%) | 1571 (8.9%) | 521 (8.0%) | 1334 (9.2%) |
| Short acting | 963 (10.9%) | 1988 (11.2%) | 784 (12.0%) | 1749 (12.1%) |
| Patches+short acting | 7135 (80.4%) | 14,004 (79.0%) | 5143 (78.3%) | 11,180 (77.5%) |
| None | 124 (1.4%) | 158 (0.9%) | 120 (1.8%) | 155 (1.1%) |
| Total mg of NRT dispensed (Mdn (IQR)) | 1358 (688–2675) | 1519 (756–2964) | 1148 (588–2253) | 1316 (646–2611) |
IQR, interquartile range; Mdn, median; NRT, nicotine replacement therapy
Crude and adjusted logistic regression models are presented in Table 3. In unadjusted analyses, we found a significant positive association between having a TEACH-trained HCP and the likelihood of smoking abstinence at 6-month follow-up in both analytic samples (most care sample: OR = 1.09, 95% CI = 1.00, 1.19; all care sample: OR = 1.11, 95% CI = 1.01, 1.23). When adjusted for patient-level covariates, the association in the all care sample remained significant (OR = 1.10, 95% CI = 1.00, 1.23), while the association in the most care sample did not. Finally, when both patient- and practice-level covariates were adjusted for, a significant association between having a TEACH-trained HCP and the likelihood of smoking abstinence at 6 months was observed in both analytic samples (most care sample: OR = 1.10, 95% CI = 1.01, 1.20; all care sample: OR = 1.12, 95% CI = 1.02, 1.24).
Table 3.
Regression outcome of HCP TEACH training status on patient quitting at 6-month follow-up
| Unadjusted | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | |
| Sample 1: TEACH-trained HCP, most care provided by one HCP sample (n = 26,590) | 1.09 (1.00–1.19) | 0.046 | 1.08 (0.99–1.18) | 0.067 | 1.10 (1.01–1.20) | 0.026 |
| Sample 2: TEACH-trained HCP, all care provided by one HCP sample (n = 20,986) | 1.11 (1.01–1.23) | 0.033 | 1.11 (1.00–1.23) | 0.042 | 1.12 (1.02–1.24) | 0.020 |
Italicized values indicate statistical significance (p < 0.05)
Model 1 adjusted for baseline patient level covariates: age; gender; education; income; employment status; baseline daily smoking status; willingness to set quit date within the next 30 days; past year quit attempt; marijuana use; opioid use; alcohol use; lifetime history of heart disease, diabetes, chronic obstructive pulmonary disease (COPD), cancer, depression, anxiety, schizophrenia, bipolar disorder; and patient health questionnaire (PHQ-9) score
Model 2 adjusted for baseline patient-level covariates from Model 1 and also practice-level covariates: practice setting, type, and duration of STOP implementation and clinic size at time of patient enrollment
HCP, health care practitioner; TEACH, Training Enhancement in Applied Counselling and Health
Discussion
In this study, a significant association was found between patient smoking abstinence at 6-month follow-up and having been treated by a HCP trained in an intensive tobacco cessation program compared with other less intensive training, even after adjustment for patient- and practice-level covariates.
Our findings are in line with previous individual studies (e.g., Brose et al. 2014; Olano-Espinosa et al. 2013) and a meta-analysis of 14 randomized trials that found a significant effect of practitioner training on patients’ point prevalence of abstinence at 6 months or more following the start of training (OR = 1.36, 95% CI = 1.20–1.55, p = 0.004; Carson et al. 2012). However, in these previous individual studies and meta-analyses, the comparison group was patients treated by untrained practitioners and the trainings varied substantially in terms of intensity of training provided to HCPs (i.e., durations ranged from one 40-min session (Unrod et al. 2007) to five day-long sessions (Joseph et al. 2004)) and content covered in training. One study did assess the effect of a comprehensive training intervention on continuous abstinence at 6-month follow-up (OR = 6.5, 95% CI = 3.3–12.7, p < 0.0001), but again, the comparison was with a control group that did not receive any training (Olano-Espinosa et al. 2013).
Our analysis takes this line of enquiry further by not simply comparing patient outcomes between trained HCPs and untrained HCPs, where one may more reasonably hypothesize a measurable effect, but by focusing among trained HCPs and comparing the type of training undertaken. As clinical guidelines recommend training that incorporates specific competencies, such as providing patient-centred approaches to treatment and offering behavioural and pharmacological interventions (Fiore et al. 2008; CAN-ADAPTT 2011), training programs that include these components are of most relevance to practitioners, and studies that distinguish between training options are of most relevance to decision makers interested in educational initiatives that optimize the ability of HCPs to provide effective prevention services.
Growing the understanding of the most effective smoking cessation treatments, providers to deliver treatments, and training to prepare providers to deliver treatments is an underdeveloped area of research with scientific importance. Indeed, in their 2017 report, the Cochrane Tobacco Addiction Group identified delivery, per se, of evidence-based, safe, and cost-effective smoking cessation treatment as a key area of priority for both clinicians and researchers (Lindson et al. 2017). Evidence suggests that HCPs may not have adequate training to provide comprehensive cessation support to their patients; if such training exists and is made available, knowledge and skills gained may be implemented in practice (Carson et al. 2012). HCPs in primary care settings have a unique opportunity to impact smoking behaviour change given relationships with patients, diversity of patients seen, and opportunities for continuity of care (Doyle et al. 2013). Applying behavioural interventions for modifiable health conditions into everyday practice has demonstrated population health implications (e.g., West et al. 2015).
Limitations
This study has several limitations. Because this was a secondary analysis of observational data, exposure to TEACH training was not allocated randomly, and analyses were restricted to available measures. As such, possible bias may have been introduced due to residual and unmeasured confounding factors, including practitioner-level variables, such as HCP years of experience or engagement in other professional trainings. It is also possible that the time and travel commitment associated with the TEACH training program may have been a deterrent to some interested clinicians. To overcome this barrier, TEACH developed and offers a facilitated online version of the training course, which can be completed over several weeks. Internal evaluation data show that both in-person and online training modalities have been well subscribed and well attended, and are associated with improvements in self-reported participant competencies, indicating that despite the time commitment, the course is a valuable offering to HCPs interested in obtaining training for conducting smoking cessation treatment. Ultimately, due to this study’s flexible design, combined with the multidisciplinary sample of HCPs trained and variety of clinical practice settings, our findings may more accurately reflect outcomes from real-world cessation intervention settings. A second limitation of this study is that despite inclusion of a range of patient- and practice-level variables as potential confounders in our analyses, we do not know what aspect of TEACH training led to improved patient outcomes. Evidence from previous program analyses suggest that intensive training on assessment, quit plan development, and applying strategies for relapse prevention, delivered through multidisciplinary and experiential learning methods, may be associated with changes in HCP performance in those areas. These learning methods applied in the context of offering pharmacological interventions may be particularly useful for HCPs in real-world settings, like that of the STOP program. Further consideration of what specific aspects of comprehensive smoking cessation training may lead to improved outcomes is an important area for future research. Another limitation of this work is that in order to capture most patients who had completed active treatment, and as per recommended guidelines (Piper et al. 2019), smoking outcomes were assessed at 6 months following enrollment. Although we expected to capture most individuals who experienced smoking relapse within our reporting period (Hughes et al. 2004), future studies that examine long-term abstinence would be beneficial. Finally, as the follow-up rate was 53%, non-response bias may have impacted our findings.
Conclusions
These findings suggest that comprehensive training, specifically of HCPs to provide tobacco cessation interventions, may contribute to improved patient smoking outcomes in both primary care and addiction service settings. This study supports the implementation of training that incorporates screening, assessment, and treatment methods to support comprehensive, intensive tobacco cessation interventions. Given the impact of smoking on morbidity and mortality and potential patient reach of HCPs, comprehensive cessation training is a promising intervention that may be implemented to reduce the public health burden of smoking, and ultimately to mitigate risks associated with smoking for the patient.
Acknowledgements
The authors thank Arezoo Ebnahmady who contributed to initial discussions of the study design and Ahmad Mobin who performed preliminary data cleaning. Peter Selby would like to acknowledge salary support for his clinician-scientist position from the Centre for Addiction and Mental Health and the Department of Family and Community Medicine at the University of Toronto.
Funding information
Funding for the Smoking Treatment for Ontario Patients (STOP) and Training Enhancement in Applied Counselling and Health (TEACH) programs was provided by the Ministry of Health and Long-Term Care (MOHLTC), as part of the Smoke Free Ontario Strategy. The findings in and conclusions of this study are those of the authors and do not necessarily represent the official position of the MOHLTC. This study did not receive any external funding.
Compliance with ethical standards
This study was approved by the Research Ethics Board of the Centre for Addiction and Mental Health (CAMH). Informed consent was obtained from all individual participants prior to collection of any study data.
Conflict of interest
Dolly Baliunas and Peter Selby report grants from Pfizer Inc. through the Global Research Awards in Nicotine Dependence (GRAND) program. In the last 5 years, Peter Selby additionally reports grants from Pfizer Inc./Pfizer Canada, Bhasin Consulting Fund, Shoppers Drug Mart, and Patient-Centered Outcomes Research Institute; has received honoraria for speaking engagements from Pfizer Canada Inc., ABBVie, and Bristol-Myers Squibb; and has also received consulting fees from Pfizer Inc./Pfizer Canada, Evidera Inc., Johnson & Johnson Group of Companies, Medcan Clinic, Miller Medical Communications, MedPlan Communications, NVision Insight Group, Inflexxion Inc., Kataka Medical Communications, Sun Life Financial, and Myelin & Associates. Through an open tender process, Johnson & Johnson, Novartis, and Pfizer Inc. are vendors of record for providing smoking cessation pharmacotherapy, free or discounted, for research studies in which Peter Selby is the principal investigator or co-investigator. Anna Ivanova, Elise Tanzini, and Rosa Dragonetti declare that they have no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Brose LS, West R, Michie S, McEwen A. Changes in success rates of smoking cessation treatment associated with take up of a national evidence based training programme. Preventive Medicine. 2014;69:1–4. doi: 10.1016/j.ypmed.2014.08.021. [DOI] [PubMed] [Google Scholar]
- CAN-ADAPTT. (2011). Canadian smoking cessation clinical practice guideline. In Canadian Action Network for the Advancement, Dissemination and Adoption of Practice-informed Tobacco Treatment. Toronto, ON: Centre for Addiction and Mental Health.
- Canadian Pharmacists Association. (2006). QUIT: quit using and inhaling tobacco. Ottawa, ON: Canadian Pharmacists Association.
- Carson KV, Verbiest ME, Crone MR, Brinn MP, Esterman AJ, Assendelft WJ, et al. Training health professionals in smoking cessation. Cochrane Database of Systematic Reviews. 2012;5:CD000214. doi: 10.1002/14651858.CD000214.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3(1):e001570. doi: 10.1136/bmjopen-2012-001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Jaen CR, Baker TB, Bailey WC, Bennett G, Benowitz NL, et al. A clinical practice guideline for treating tobacco use and dependence: 2008 update - a US Public Health Service report. American Journal of Preventive Medicine. 2008;35(2):158–176. doi: 10.1016/j.amepre.2008.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodchild M, Nargis N, Tursan d'Espaignet E. Global economic cost of smoking-attributable diseases. Tobacco Control. 2018;27(1):58–64. doi: 10.1136/tobaccocontrol-2016-053305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herie M, Connolly H, Voci S, Dragonetti R, Selby P. Changing practitioner behavior and building capacity in tobacco cessation treatment: the TEACH project. Patient Education and Counseling. 2012;86(1):49–56. doi: 10.1016/j.pec.2011.04.018. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99(1):29–38. doi: 10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- Hyland A, Borland R, Li Q, Yong HH, McNeill A, Fong GT, et al. Individual-level predictors of cessation behaviours among participants in the International Tobacco Control (ITC) Four Country Survey. Tobacco Control. 2006;15(suppl 3):83–94. doi: 10.1136/tc.2005.013516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph AM, Arikian NJ, An LC, Nugent SM, Sloan RJ, Pieper CF, et al. Results of a randomized controlled trial of intervention to implement smoking guidelines in veterans affairs medical centers: increased use of medications without cessation benefit. Medical Care. 2004;42(11):1100–1110. doi: 10.1097/00005650-200411000-00009. [DOI] [PubMed] [Google Scholar]
- Lindson N, Richards-Doran D, Heath L, Hartmann-Boyce J. Setting research priorities in tobacco control: a stakeholder engagement project. Addiction. 2017;112(12):2257–2271. doi: 10.1111/add.13940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olano-Espinosa E, Matilla-Pardo B, Minue C, Anton E, Gomez-Gascon T, Ayesta FJ. Effectiveness of a health professional training program for treatment of tobacco addiction. Nicotine & Tobacco Research. 2013;15(10):1682–1689. doi: 10.1093/ntr/ntt040. [DOI] [PubMed] [Google Scholar]
- Papadakis S, Gharib M, Hambleton J, Reid RD, Assi R, Pipe AL. Delivering evidence-based smoking cessation treatment in primary care practice: experience of Ontario family health teams. Canadian Family Physician. 2014;60(7):e362–e371. [PMC free article] [PubMed] [Google Scholar]
- Piper, M. E., Bullen, C., Krishnan-Sarin, S., Rigotti, N. A., Steinberg, M. L., Streck, J. M., et al. (2019). Defining and measuring abstinence in clinical trials of smoking cessation interventions: an updated review. Nicotine & Tobacco Research. 10.1093/ntr/ntz110. [DOI] [PMC free article] [PubMed]
- Registered Nurses' Association of Ontario. (2012). Toolkit: implementation of best practice guidelines (2nd ed.). Toronto, ON: Registered Nurses' Association of Ontario.
- Reid RD, Mullen K-A, Slovinec D'Angelo ME, Aitken DA, Papadakis S, Haley PM, et al. Smoking cessation for hospitalized smokers: an evaluation of the “Ottawa Model”. Nicotine & Tobacco Research. 2010;12(1):11–18. doi: 10.1093/ntr/ntp165. [DOI] [PubMed] [Google Scholar]
- Rosella LC, Kornas K, Huang A, Grant L, Bornbaum C, Henry D. Population risk and burden of health behavioural related all-cause, premature, and amenable deaths in Ontario, Canada: Canadian Community Health Survey linked Mortality Files. Annals of Epidemiology. 2019;32:49–57. doi: 10.1016/j.annepidem.2019.01.009. [DOI] [PubMed] [Google Scholar]
- Selby, P., Herie, M., Dragonetti, R., Barker, M., Chapchuk, R., Fahim, M., et al. (2012). Fundamentals of tobacco interventions: a comprehensive training toolkit. Toronto, ON: Centre for Addiction and Mental Health.
- Shershneva MB, Larrison C, Robertson S, Speight M. Evaluation of a collaborative program on smoking cessation: translating outcomes framework into practice. Journal of Continuing Education in the Health Professions. 2011;31(S1):S28–S36. doi: 10.1002/chp.20146. [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L., Kroenke, K., & Williams, J. B. (1999). Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study., 282(18), 1737–1744. 10.1001/jama.282.18.1737. [DOI] [PubMed]
- Stanaway JD, Afshin A, Gakidou E, Lim SS, Abate D, Abate KH, et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1923–1994. doi: 10.1016/s0140-6736(18)32225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada (2017). Table 13-10-0096-01 Health characteristics, annual estimates. https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310009601. Accessed April 11, 2019.
- Stead LF, Koilpillai P, Fanshawe TR, Lancaster T. Combined pharmacotherapy and behavioural interventions for smoking cessation. Cochrane Database Syst Rev. 2016;3(3):CD008286. doi: 10.1002/14651858.CD008286.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unrod M, Smith M, Spring B, DePue J, Redd W, Winkel G. Randomized controlled trial of a computer-based, tailored intervention to increase smoking cessation counseling by primary care physicians. Journal of General Internal Medicine. 2007;22(4):478–484. doi: 10.1007/s11606-006-0069-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt F, Hall S, Marteau TM. General practitioners’ and family physicians’ negative beliefs and attitudes towards discussing smoking cessation with patients: a systematic review. Addiction. 2005;100(10):1423–1431. doi: 10.1111/j.1360-0443.2005.01221.x. [DOI] [PubMed] [Google Scholar]
- West R, Raw M, McNeill A, Stead L, Aveyard P, Bitton J, et al. Health-care interventions to promote and assist tobacco cessation: a review of efficacy, effectiveness and affordability for use in national guideline development. Addiction. 2015;110(9):1388–1403. doi: 10.1111/add.12998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong SL, Shields M, Leatherdale S, Malaison E, Hammond D. Assessment of validity of self-reported smoking status. Health Reports. 2012;23(1):47–53. [PubMed] [Google Scholar]
- Ye L, Goldie C, Sharma T, John S, Bamford M, Smith PM, et al. Tobacco-nicotine education and training for health-care professional students and practitioners: a systematic review. Nicotine & Tobacco Research. 2017;20(5):531–542. doi: 10.1093/ntr/ntx072. [DOI] [PubMed] [Google Scholar]