Abstract
Epidemic thunderstorm asthma has been reported to have occurred around twenty times over the past three decades in locations around the world. Thunderstorm asthma events are characterized by a significant increase in asthma presentations, which on occasion can overwhelm local medical services and result in fatalities. This review article presents the epidemiological data underpinning previous thunderstorm asthma events and analyzes what is known about the etiology of this unusual phenomenon. The evidence behind published risk factors, both at the individual and population level, is discussed. Research from the fields of allergy, pulmonology, meteorology, and climatology is drawn together and critically reviewed to surmise future predictions regarding thunderstorm asthma episodes. Finally, evidence-based individual, community, and environmentally targeted preventive strategies are presented.
Keywords: asthma, epidemics, spores, pollen, critical care
Introduction
Thunderstorm asthma refers to an observed increase in acute bronchospasm cases following the occurrence of thunderstorms in the local vicinity,1 although no strict definition based upon the magnitude of increase in asthma presentations has been established. Thunderstorm asthma epidemics are rare, occurring only when specific population, meteorological, and environmental factors coincide. Affected individuals present with classic symptoms of acute asthma such as cough, wheeze, and shortness of breath. These symptoms typically improve with the use of inhaled bronchodilators. However, large numbers of people can be affected, which has the propensity to overwhelm locally available health services. Rarely, thunderstorm asthma can be fatal.
Background
Clear published reports of thunderstorm asthma date back to the early 1980s,2,3 with more than twenty distinct occurrences now recognized.4 Populations across Australia,5,6 Italy,7 North America,8 the Middle East,9 Asia,10 and the United Kingdom11 have been affected, though the number of individuals involved is highly variable (Table 1). Historically, thunderstorm asthma events have been poorly predicted, as they are sporadic and infrequent. However, the majority have occurred during the Spring or early Summer periods, when circulating aeroallergen counts are often higher.
Table 1.
Thunderstorm Asthma Events
| Date | Location | Allergen Trigger(s) | Presentation |
|---|---|---|---|
| 6–7 Jul 1983 | Birmingham, UK4 | Fungal spores | 106 emergency presentations (compared to usual ~20), most with hayfever in the preceding week |
| 20–21 Jun 1984 | Nottingham, UK2 | Fungal spores | 22 emergency presentations (~5-fold increase), 9 with prior hayfever but not asthma |
| 11 Nov 1984 | Melbourne, Australia3 | Not specified | 86 emergency presentations and 16 admissions; 95% having a history of atopy |
| Nov 1987 | Melbourne, Australia14 | Not specified | 154 presentations (5 to 10-fold increase in presentations and admissions); one death |
| 22 Jul 1989 | Leicester, UK32 | Fungal spores | 32 hospital admissions (~7-fold increase) |
| Nov 1989 | Melbourne, Australia14 | Grass pollen | 277 presentations (5 to 10-fold increase) |
| 1–5 Nov 1990 | Tamworth, Australia35 | Grass pollen | 110 emergency presentations and 123 general practitioner presentations (>10-fold increase) |
| 24 Jun 1994 | London, UK24 | Grass pollen | 640 emergency presentations (~10-fold increase), 63% with prior hayfever |
| 1 Dec 1996 | Kuwait City, Kuwait28 | Not identified | 844 presentations (17 near-fatal), 11 deaths |
| 30–31 Oct 1997 | Wagga Wagga, Australia23 | Grass pollen | 215 presentations, 41 admissions, 95% with hayfever and 96% of skin-prick tested cases sensitized to rye grass |
| 27 Oct 1998 | Newcastle, Australia20 | Grass pollen | 6 presenting patients underwent skin-prick testing; rye grass median wheal 20mm, all had hayfever |
| 31 Jul – 1 Aug 2000 | Calgary, Canada8 | Fungal spores | 157 presentations (9-fold increase) |
| 29–31 Jul 2002 | Cambridge, UK13 | Fungal spores | 57 presentations (~10-fold increase), 1 death |
| Nov 2002 | Al-Ahsa, Saudi Arabia9 | Not identified | Steady influx of acute cases requiring involvement of neighbouring hospitals |
| 20 Nov 2003 | Melbourne, Australia27 | Grass pollen | 70 paediatric emergency presentations (>3-fold increase) |
| 4 Jun 2004 | Naples, Italy26 | Weed pollen | 7 emergency department presentations within half an hour |
| 24 Jun 2005 | South-East England, UK11 | Not identified | 4-fold increase in calls relating to difficulty breathing to a telephone advice line, doubling of out-of-hours attendances |
| 27–28 May, 2010 | Barletta, Italy7 | Olive tree pollen | 20 emergency presentations (~10-fold increase) |
| 25 Nov, 2010 | Melbourne, Australia15 | Grass pollen | 36 emergency presentations (5 to 10-fold increase) |
| 8 Nov, 2011 | Melbourne, Australia6 | Grass pollen | 10 ambulance attendances per hour for breathing difficulties (2-fold increase) |
| 2 Nov, 2013 | Ahvaz, Iran22 | Not identified | >2100 emergency presentations across nine hospitals |
| 26 Oct, 2014 | Canberra, Australia5 | Grass pollen | 15 asthma presentations at a single emergency department (4-fold increase) |
| 21 Nov, 2013 | Melbourne and Geelong, Australia21 | Grass pollen | >3300 more respiratory presentations than expected to emergency departments, 10-fold increase in asthma admissions, 35 to intensive care; 10 deaths |
| 11 Sep, 2018 | Yuling, China10 | Plant pollen | 16-fold increase in paediatric asthma admissions |
Etiology
Thunderstorm asthma epidemics occur when a population sensitized to circulating aeroallergens is exposed to those triggering allergens in a respirable form due to the actions of the storm itself.12 Most commonly, pollens (especially grass pollens) are the predominant allergen involved, although fungal spores have also been implicated.13–15
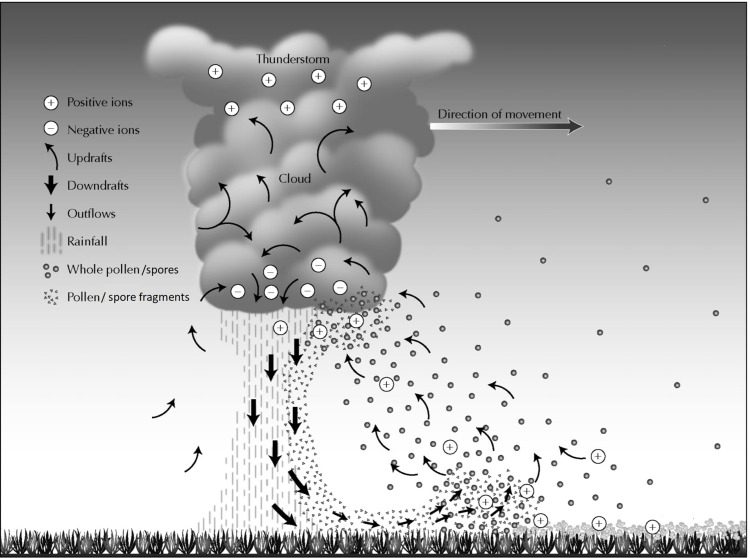
The meteorological activity involved in the generation of thunderstorm asthma is complex (Figure 1). Pollen and/or spores are swept up into the cloud base by warm updrafts, where they are fractured into finer particles either by electrical forces arising with ionic charge differences generated by the storm, or by absorption of moisture leading to swelling and rupture (osmotic shock) of the pollen/spores into smaller fragments.16 As an example, rye grass pollens commencing at >35 µm in size are disrupted into particles <3 µm by this process.17 These multitudinous tiny particles are swept down to ground level by cool downdrafts and gusty wind outflows. Here, if a susceptible population is present, they can be inhaled into the intrathoracic airways, bypassing filtration by the nasopharynx due to their smaller, respirable size. If the individual is sensitized to the triggering allergen, acute bronchospasm is induced, often within minutes. This early asthmatic response is characterized by IgE-mediated mast cell degranulation causing airway smooth muscle contraction, as well as mucosal edema and mucous production.18 This may be followed by ongoing Th2 lymphocyte activation, inflammatory cytokine signaling, and/or eosinophilic infiltration, perpetuating the asthmatic response in the individual.19,20
Figure 1.
Proposed mechanism explaining thunderstorm asthma. Adapted by permission from Springer Nature, Current Allergy and Asthma Reports.16 Taylor PE, Jonsson H. Thunderstorm asthma. Copyright 2004.
Presentation
The clinical presentation of thunderstorm asthma is characterized by acute onset coughing, shortness of breath, wheezing, and respiratory distress due to airway irritation, inflammation, and obstruction. Although inhaled bronchodilators are often effective, hypoxia and respiratory failure can develop, with death a rare but possible complication.21 Thunderstorm asthma affects not just single individuals but groups of people who are in proximity to each other and the associated storm front. Those who are not sensitized or exposed to the offending allergen, including people who remain indoors with windows and doors shut, are almost universally unaffected.1 These features differentiate thunderstorm asthma from non-thunderstorm asthma and other respiratory conditions. Prior history of asthma is not a defining feature, as 36–56% presenting with thunderstorm asthma do not have an established diagnosis of asthma.21–24 However, they may well have hay fever as a manifestation of their allergy to the triggering pollen or spore.23
On a broader community level, the presentation of a thunderstorm asthma event may be characterized by high demand for and possible overwhelming of local health resources when large numbers of people are affected.24 For example, in the largest reported thunderstorm asthma event, which occurred on 21st November 2016 in Melbourne, Australia, there was a ten-fold increase in asthma admissions and a similar increase in emergency department presentations. Thirty-five patients were admitted to intensive care and five died in hospital; a further five died whilst awaiting (or could not be resuscitated by) the attention of paramedics and ambulance officers, who faced a momentous increase in callout requests.21 A comparably large event in Iran similarly required the resources of multiple hospitals and emergency departments to cope with thousands of thunderstorm asthma sufferers.22
Risk Factors
There are several risk factors that predispose individuals and populations to experience thunderstorm asthma. The greatest risk factor for individuals appears to be a history of allergic rhinitis, which embodies a clinical manifestation of sensitization to an environmental allergen. In almost all episodes of thunderstorm asthma where allergic rhinitis and/or skin-prick test sensitization to the suspected offending allergen was reported, it was present in more than 90% of affected cases,19 which is well above population norms. Furthermore, the ages of patients affected by thunderstorm asthma, which is predominantly 20–50 years, closely matches the age distribution of allergic rhinitis.25 People exposed to the outdoor environment are also much more likely to suffer from thunderstorm asthma compared to those who are not.26 Though the incidence of thunderstorm asthma in children is variable in studies reporting pediatric data,10 children are proportionally underrepresented (but not universally spared27) in thunderstorm asthma diagnoses when compared to their rate of non-thunderstorm asthma diagnosis. Males are more likely to be affected than females,10 and in one epidemic, Asian or Indian ethnicity was a significant risk factor for having thunderstorm asthma and increased severity of it.21
For individuals who suffer from severe thunderstorm asthma that results in intensive care admission or death, a pre-existing diagnosis of asthma is highly likely.19,28 In fact, all 35 thunderstorm asthma-related intensive care unit admissions during the 2016 Melbourne epidemic event (as well as all deaths) were in people previously diagnosed with asthma.21
On a population level, risk factors for thunderstorm asthma epidemics include the circulating triggering aeroallergen load, propensity for storm activity coinciding with this, and presence and size of a sensitized and susceptible population. All factors are needed for a significant thunderstorm asthma event (Figure 2). Geographical areas where all these factors are likely to coexist are therefore more likely to experience a thunderstorm asthma epidemic. Other air pollutants may also play a role.22
Figure 2.
Picture of all elements required for a thunderstorm asthma epidemic: storm activity, presence of aeroallergen (in this case grass pollen), and human presence as shown by building.
Future Predictions
Thunderstorm asthma is an emerging threat to the health of vulnerable populations. Episodes may become more frequent in the setting of changes to climate.29 Furthermore, air pollution is an important co-factor in the development of pollen-related allergic disease,30 so increasing pollution levels may potentiate more severe outbreaks of thunderstorm asthma. Changes to climate are likely to lead to more frequent and widespread episodes of thunderstorm asthma by a variety of mechanisms. Firstly, storm events may increase in frequency and severity due to ocean and near-surface air warming effects.31 Secondly, changes to climate alter the growth patterns of allergen-producing plants and the production and dispersion of triggering pollens; with increasing atmospheric carbon dioxide levels predisposing plants to produce more pollen, this could substantially increase the risk of severe thunderstorm asthma events.29 Thunderstorm asthma events are also more likely to occur in previously unaffected regions and outside of usual seasons due to these changes.
Predicting a future thunderstorm asthma event is challenging due to the unique combination of meteorological, aerobiological, and population factors involved.32 However, prediction is an important goal.21 Unfortunately, current predictive models tested to predict high-risk asthma admission days do not seem to have the ability to accurately identify these days primarily due to low specificity, and furthermore cannot reliably predict the magnitude of events.32
Prevention Strategies
Due to the potential for more severe and frequent thunderstorm asthma events in the future, enacting preventative strategies has the potential to significantly reduce morbidity and mortality. Individual, population and environmental factors should be addressed. Individuals with existing asthma are at higher risk of having severe and life-threatening thunderstorm asthma exacerbations.33 However, for these individuals, inhaled corticosteroids may be effective in preventing severe attacks during storms.23 Therefore, promotion of good asthma management and control with medical therapy is an important preventive strategy.32 A larger set of susceptible patients tend to have pollen sensitization manifesting as a history of allergic rhinitis, often without a pre-existing history of asthma. For these individuals, education on their susceptibility to thunderstorm asthma may be useful, especially if coupled with provision of emergency medication for them to have available should thunderstorm asthma eventuate. The role masks could play in reducing pollen inhalation and thereby potentially reducing thunderstorm asthma incidence and severity has not been explored. Although accurately identifying which patients with pollen sensitization will develop thunderstorm asthma is currently not possible, treating their pollen allergy with sublingual immunotherapy has been shown to decrease their susceptibility to storm-related asthma.34 The corresponding decrease in exhaled nitric oxide levels demonstrated in these protected patients is intriguing and suggests that it could be a relevant biomarker to predict thunderstorm asthma risk.
On a population level, public health messages about thunderstorm asthma should be delivered in a timely, targeted, and evidence-based manner in order to maximize benefit.35 Utilizing local media may be useful.36 Messages should include information on who is at risk, how they can be prepared for an event, and steps to take in a thunderstorm asthma outbreak, such as having asthma medication ready and remaining indoors with windows and doors closed.37 Although predictive models may not be entirely accurate, with refinement they may serve as useful warning systems in the future. As one example, an online warning system combining pollen count and meteorological data has been deployed in Australia following the 2016 Melbourne thunderstorm asthma epidemic.38 Population-level approaches to address the issue of sub-optimally controlled asthma in the community at large are necessary, with education of clinicians and patients alike warranted.19
Finally, efforts to better understand and modify the environmental risk factors for thunderstorm asthma are challenging to pursue but worthwhile. Further research investigating the interplay between weather and pollen/spore dissemination may lead to better thunderstorm asthma warning systems. Individuals, companies, and governments can all contribute to both climate changes and air pollution that increase the chance of thunderstorm asthma occurring. Behavior modification of these stakeholders to minimize these detrimental environmental effects is required to improve pulmonary health for citizens.39
Conclusion
Thunderstorm asthma events are sporadic occurrences that arise when large groups of sensitized individuals are exposed to triggering aeroallergens due to the actions of a storm. These epidemic events result in higher than average asthma exacerbations and presentations, which can overwhelm healthcare services. Rarely, thunderstorm asthma can lead to death of the affected person. Individual patient, population and environmental factors both predispose to and can be targeted to prevent thunderstorm asthma. Further research into the complex interactions between climate, weather, and aerobiological phenomena that lead to thunderstorm asthma is needed, so as to best prepare for this unpredictable, significant public health threat.
Disclosure
The author reports no funding and no conflicts of interest for this work.
References
- 1.D’Amato G, Vitale C, D’Amato M, et al. Thunderstorm-related asthma: what happens and why. Clin Exp Allergy. 2016;46(3):390–396. doi: 10.1111/cea.12709 [DOI] [PubMed] [Google Scholar]
- 2.Alderman P, Sloan J, Basran G. Asthma and thunderstorms. Arch Emerg Med. 1986;3(4):260–262. doi: 10.1136/emj.3.4.260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Egan P. Weather or not. Med J Aust. 1985;142(5):330. doi: 10.5694/j.1326-5377.1985.tb113389.x [DOI] [PubMed] [Google Scholar]
- 4.Packe GE, Ayres JG. Asthma outbreak during a thunderstorm. Lancet. 1985;326(8448):199–204. doi: 10.1016/S0140-6736(85)91510-7 [DOI] [PubMed] [Google Scholar]
- 5.Colley C Canberra sneezes through worst hay fever season in years. Canberra Times [Internet] 2014. November 7 Available from: www.canberratimes.com.au/act-news/canberra-sneezes-through-worst-hay-fever-season-in-years-20141105-11h3xk.html. Accessed August10, 2020.
- 6.Murnane M. Storms trigger asthma explosion as pollen fills the air. Sydney Morning Herald [Internet] 2011. November 8 Available from: www.smh.com.au/environment/weather/storms-trigger-asthma-explosion-as-pollen-fills-the-air-20111108-1n4qw.html. Accessed August10, 2020.
- 7.Losappio L, Heffler E, Contento F, Cannito C, Rolla G. Thunderstorm-related asthma epidemic owing to Olea Europaea pollen sensitization. Allergy Eur J Allergy Clin Immunol. 2011;66(11):1510–1511. [DOI] [PubMed] [Google Scholar]
- 8.Wardman AD, Stefani D, MacDonald JC. Thunderstorm-associated asthma or shortness of breath epidemic: a Canadian case report. Can Respir J. 2002;9(4):267–270. doi: 10.1155/2002/728257 [DOI] [PubMed] [Google Scholar]
- 9.Al-Rubaish AM. Thunderstorm-associated bronchial asthma: a forgotten but very present epidemic. J Family Community Med. 2007;14(2):47–51. [PMC free article] [PubMed] [Google Scholar]
- 10.Xu Y, Xue T, Li H, Guan K. Retrospective analysis of epidemic thunderstorm asthma in children in Yulin, northwest China. Pediatr Res. 2020. [DOI] [PubMed] [Google Scholar]
- 11.Levy M, Bryden C. Thunderstorm asthma. Brit J Prim Care Nurs. 2007;1:69–71. [Google Scholar]
- 12.Marks GB, Bush RK. It’s blowing in the wind: new insights into thunderstorm-related asthma. J Allergy Clin Immunol. 2007;120(3):530–532. doi: 10.1016/j.jaci.2007.07.012 [DOI] [PubMed] [Google Scholar]
- 13.Pulimood TB, Corden JM, Bryden C, Sharples L, Nasser SM. Epidemic asthma and the role of the fungal mold Alternaria alternata. J Allergy Clin Immunol. 2007;120(3):610–617. doi: 10.1016/j.jaci.2007.04.045 [DOI] [PubMed] [Google Scholar]
- 14.Bellomo R, Gigliotti P, Treloar A, et al. Two consecutive thunderstorm associated epidemics of asthma in the city of Melbourne: the possible role of rye grass pollen. Med J Aust. 1992;156(12):834–837. doi: 10.5694/j.1326-5377.1992.tb136994.x [DOI] [PubMed] [Google Scholar]
- 15.Howden ML, McDonald CF, Sutherland MF. Thunderstorm asthma - a timely reminder. Med J Aust. 2011;195(9):512–513. doi: 10.5694/mja11.11044 [DOI] [PubMed] [Google Scholar]
- 16.Taylor PE, Jonsson H. Thunderstorm asthma. Curr Allergy Asthma Rep. 2004;4(5):409–413. doi: 10.1007/s11882-004-0092-3 [DOI] [PubMed] [Google Scholar]
- 17.Suphioglu C, Singh MB, Taylor P, et al. Mechanism of grass-pollen-induced asthma. Lancet. 1992;339(8793):569–572. doi: 10.1016/0140-6736(92)90864-Y [DOI] [PubMed] [Google Scholar]
- 18.Cockcroft DW, Davis BE, Blais CM. Thunderstorm asthma: an allergen-induced early asthmatic response. Ann Allergy, Asthma Immunol. 2018;120(2):120–123. doi: 10.1016/j.anai.2017.12.002 [DOI] [PubMed] [Google Scholar]
- 19.Harun N, Lachapelle P, Douglass J. Thunderstorm-triggered asthma: what we know so far. J Asthma Allergy. 2019;12:101–108. doi: 10.2147/JAA.S175155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wark PAB, Simpson J, Hensley MJ, Gibson PG. Airway inflammation in thunderstorm asthma. Clin Exp Allergy. 2002;32(12):1750–1756. doi: 10.1046/j.1365-2222.2002.01556.x [DOI] [PubMed] [Google Scholar]
- 21.Thien F, Beggs PJ, Csutoros D, et al. The Melbourne epidemic thunderstorm asthma event 2016: an investigation of environmental triggers, effect on health services, and patient risk factors. Lancet Planet Health. 2018;2(6):e255–63. doi: 10.1016/S2542-5196(18)30120-7 [DOI] [PubMed] [Google Scholar]
- 22.Forouzan A, Masoumi K, Haddadzadeh Shoushtari M, et al. An overview of thunderstorm-associated asthma outbreak in southwest of Iran. J Environ Public Health. 2014;2014:1–4. doi: 10.1155/2014/504017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Girgis ST, Marks GB, Downs SH, Kolbe A, Car GN, Paton R. Thunderstorm-associated asthma in an inland town in south-eastern Australia. Who is at risk? Eur Respir J. 2000;16(1):3–8. doi: 10.1034/j.1399-3003.2000.16a02.x [DOI] [PubMed] [Google Scholar]
- 24.Davidson AC, Emberlin J, Cook AD, et al. A major outbreak of asthma associated with a thunderstorm: experience of accident and emergency departments and patients’ characteristics. Br Med J. 1996;312(7031):601–604. doi: 10.1136/bmj.312.7031.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Australian Institute of Health and Welfare. Allergic rhinitis [Internet]. Vol. 25 2019. [cited March15, 2020]. Available from: https://www.aihw.gov.au/reports/chronic-respiratory-conditions/allergic-rhinitis-hay-fever/contents/allergic-rhinitis. [Google Scholar]
- 26.D’Amato G, Cecchi L, Liccardi G. Thunderstorm-related asthma: not only grass pollen and spores. J Allergy Clin Immunol. 2008;121(2):537–538. doi: 10.1016/j.jaci.2007.10.046 [DOI] [PubMed] [Google Scholar]
- 27.Erbas B, Akram M, Dharmage SC, et al. The role of seasonal grass pollen on childhood asthma emergency department presentations. Clin Exp Allergy. 2012;42(5):799–805. doi: 10.1111/j.1365-2222.2012.03995.x [DOI] [PubMed] [Google Scholar]
- 28.Ali F, Behbehani N, Alomair N, Taher A. Fatal and near-fatal thunderstorm asthma epidemic in a desert country. Ann Thorac Med. 2019;14:155–160. doi: 10.4103/atm.ATM_258_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.D’Amato G, Vitale C, Lanza M, Molino A, D’Amato M. Climate change, air pollution, and allergic respiratory diseases: an update. Curr Opin Allergy Clin Immunol. 2016;16(5):434–440. doi: 10.1097/ACI.0000000000000301 [DOI] [PubMed] [Google Scholar]
- 30.Chung HY, Hsieh CJ, Tseng CC, Yiin LM. Association between the first occurrence of allergic rhinitis in preschool children and air pollution in taiwan. Int J Environ Res Public Health. 2016;13(3):6–12. doi: 10.3390/ijerph13030268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Allen JT. Climate change and severe thunderstorms In: Oxford Research Encyclopedia of Climate Science. 2018. [Google Scholar]
- 32.Silver JD, Sutherland MF, Johnston FH, et al. Seasonal asthma in Melbourne, Australia, and some observations on the occurrence of thunderstorm asthma and its predictability. PLoS One. 2018;13(4):1–24. doi: 10.1371/journal.pone.0194929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Queensland University of Technology. Literature review on thunderstorm asthma and its implications for public health advice. Department of Health and Human Services 2017.
- 34.O’Hehir RE, Varese NP, Deckert K, et al. Epidemic thunderstorm asthma protection with five-grass pollen tablet sublingual immunotherapy: a clinical trial. Am J Respir Crit Care Med. 2018;198(1):126–128. doi: 10.1164/rccm.201711-2337LE [DOI] [PubMed] [Google Scholar]
- 35.Lindstrom SJ, Silver JD, Sutherland MF, et al. Thunderstorm asthma outbreak of november 2016: a natural disaster requiring planning. Med J Aust. 2017;207(6):235–237.e1. doi: 10.5694/mja17.00285 [DOI] [PubMed] [Google Scholar]
- 36.Waters J, Corbett S, Gibson P, Hensley M, Wlodarczyk J. Epidemic asthma surveillance in the New England region 1990–1992. NSW Public Health Bull. 1993;4(9):100. doi: 10.1071/NB93049 [DOI] [Google Scholar]
- 37.Cockcroft DW. Epidemic thunderstorm asthma. Lancet Planet Health. 2018;2(6):e236–7. doi: 10.1016/S2542-5196(18)30123-2 [DOI] [PubMed] [Google Scholar]
- 38.Doyle K, Deacon B, Locke S. Thunderstorm asthma alert system launched in Victoria to prevent repeat of disaster [Internet]. Australian Broadcasting Corporation News. 2017. [cited March14, 2020]. Available from: https://www.abc.net.au/news/2017-10-01/thunderstorm-asthma/9000320.
- 39.Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014;383(9928):1581–1592. doi: 10.1016/S0140-6736(14)60617-6 [DOI] [PMC free article] [PubMed] [Google Scholar]