Abstract
Introduction
For decades, automatic speech recognition (ASR) has been the subject of research and its range of applications broadened. Presently, ASR among physicians is mainly used to convert speech into text but not to implement instructions in the operating room (OR). This study aimed to evaluate physicians of different surgical professions on their personal experience and posture towards ASR.
Methods
A 16-item survey was distributed electronically to hospitals and outpatient clinics in southern Germany addressing physicians on the potential applications of ASR in the OR.
Results
The survey was responded by 185 of 2693 physicians (response rate: 6.9%) with a mean age of 41.8 ± 9.8 years. ASR is desirable in the OR regardless of the field of speciality (93.7%). While only 2.7% have used ASR, 87.9% evaluate its future potential as high. 91.0% of those working in a university hospital would consider testing ASR, while 67.5% of those in non-university hospitals and practices (p = 0.001). 90.1% of responders of strictly surgical specialities see potential in ASR while 73.7% in non-surgical specialities evaluate its future potential as high (p = 0.01). 58.3% of those over the age of 60 consider the use of ASR without a headset to be imaginable, while 96.3% among those under the age of 60. There were no statistically significant differences regarding sex and professional position.
Conclusion
Foreseeably, ASR is anticipated to be integrated into ORs and valued at a high market potential. Our study provides information about physicians’ individual preferences from various surgical disciplines regarding ASR.
Keywords: Automatic speech recognition, Voice recognition, Speech understanding, Machine learning, Artificial intelligence, Intelligent operating assistance, Operating room of the future
Highlights
-
•
ASR is a desirable tool in the OR regardless of the field of speciality.
-
•
While 90.1% interviewees from surgical specialities see potential in ASR and 73.7% from non-surgical specialities assess its future potential as high.
-
•
There were no statistically significant differences regarding sex and professional position.
-
•
For an ASR system to be implemented in the OR, it needs to be sophisticated and updatable since there are still several technical requirements to be fulfilled.
-
•
Foreseeably, ASR is anticipated to be integrated into the OR and valued at a high market potential.
1. Introduction
Automatic speech recognition (ASR) is the process by which machines automatically decipher and transcribe oral speech. An ASR system receives an acoustic signal via a microphone, which is then analysed and processed in order to generate an output, typically in written form [1]. The roots of the first speech recognition systems date back to the early 1950s [2]. Nowadays, it is indispensable not only for private use but also for various professions [3]. In several medical specialties, ASR has been tested and implemented in speech-language pathology research, diagnostics and therapeutics such as in speech apraxia [4,5]. Among medical professionals, ASR is commonly used to convert speech into text for data entries and has already been sufficiently tested in a mobile environment. Nevertheless, it has not been established as an indispensable tool for command control in the operating room (OR) [6,7] despite the implementation of basic concepts [8] and technical requirements in the OR [9,10].
Presently, surgeons cannot independently control technical equipment outside the sterile area. Therefore, at least one person has to assist during surgeries in the adjustment of lights, the position of the operating table, and the mobility of x-ray equipment.
Current offline voice-control solutions require a headset, which can slip off the face and cause surgical field contamination or might be experienced as uncomfortable altogether. Furthermore, studies have shown that noise levels in modern ORs are heterogeneous and may increase to more than 100 dB [9,11], leading to technical challenges. By now, hands- and headset free solutions with microphone arrays have been developed and tested even under noisy surrounding conditions [10].
In this study, a web-based survey was distributed among surgical-oriented physicians to document their professional background and experience matched with their opinion towards ASR to ascertain the expectations for further innovative development in the future.
2. Materials and methods
The survey was sent electronically to 2693 physicians of different specialities and levels of experience working at university and non-university hospitals as well as in outpatient clinics. We used a web-based survey tool (Survey Monkey Europe, Dublin, Ireland). A German-language survey was electronically sent in June 2018, ran for 6 months, and included one reminder with the objective of understanding physicians' posture towards ASR in a homogenous sample population. Physicians received a 16-item, multiple-choice questionnaire with a cover letter outlining the study's aims. The questionnaire was checked for content validity by three physicians and two scientists having different degrees of training and expertise.
The final version included three domains comprising personal, professional, and occupational information (items 1–6), personal experience and opinion towards ASR (items 7–10), and desired requirements and future outlooks for ASR in the OR (items 11–16). Anonymity was maintained throughout the study.
The inclusion criteria were for physicians to be practicing in the outpatient sector or a hospital.
Quantitative data was collected and respectively presented using descriptive statistics. Categorical variables were given as absolute numbers and percentages. Comparisons between independent groups were performed using the Chi-squared test. Statistically significant group differences were considered at p < 0.05. Multivariate analysis was performed by the means of logistic regression. Multiple testing was accounted for by using the Bonferroni correction.
Descriptive statistical calculations were performed using Microsoft Excel 2010 (Microsoft Corporation, Redmond, WA, USA). Statistical calculations were performed using R (Version 3.6.2) and R Studio (Version 1.1.453).
The work is in line with the Consolidated criteria for Reporting Qualitative Research (COREQ) criteria.
3. Results
Responses to the questionnaire were received from 185 of 2693 (response rate: 6.9%) physicians. The mean age of participants was 41.8 ± 9.8 years of which 21.2% were female and 78.8% male.
3.1. Professional and occupational information
A minority of participants practice in an outpatient or ambulatory setting (2.2%), while most work in university hospitals (76.5%), followed by non-university hospitals (21.3%). The survey was responded by professionals with varying levels of experience in the following proportions: 6.0% heads of department, 57.1% consultants, 12.6% board-certified doctors and 24.2% residents in training.
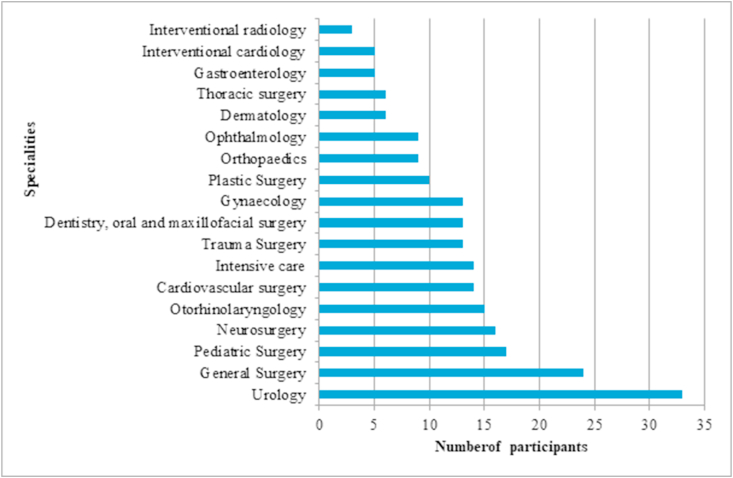
Sixty-six percent of participants had more than 10 years of experience in conducting surgery. Of 185 participants, 33 were urologists, 24 general surgeons, 17 paediatric surgeons, 16 neurosurgeons, 15 otorhinolaryngologists, 14 cardiac surgeons, 14 intensive care specialists, 13 traumatologists, 13 oral and maxillofacial surgeons, and 13 gynaecologists. Also involved were 10 plastic surgeons, 9 orthopaedic surgeons, 9 ophthalmologists, 6 dermatologists, 6 thoracic surgeons, 5 gastroenterologists, 5 interventional cardiologists and 3 interventional radiologists. Although not all participants strictly belonged to surgical disciplines, others such as gastroenterologists, interventional radiologists, and hemodynamic internists frequently perform surgical procedures that may benefit from ASR and which is why they were considered for inclusion. Multiple answers were possible regarding the surgical specialty (Fig. 1).
Fig. 1.
Number of participants of the different specialities.
3.2. Personal experience and opinions toward ASR
Ninety-nine percent of participants consider the introduction of new technologies into ORs to be of relevance and 87.9% see potential in controlling medical devices in the OR by voice alone.
Personal experience in the professional use of an automatic speech control system only applied to 2.7%. Of the participants with personal ASR experience, 66.7% rated it as sufficient, 16.7% as neutral, and 16.7% as insufficient.
There is a lack of experience regarding ASR systems as only 12.6% are familiar speech control systems in the OR at all. Nonetheless, 85.1% of respondents are open to test a system that suits their individual needs.
Furthermore, participants were inquired which technical equipment they would prefer to control which was in the following order: position of the operating table (83.7%), video and documentation system (80.2%), room lighting (73.3%), setup menu of the endoscope's light source (65.7%), X-ray apparatus (33.7%), suction pump and air-conditioning (each 30.2%), insufflator (21.5%), and intravenous (IV) stand (9.3%).
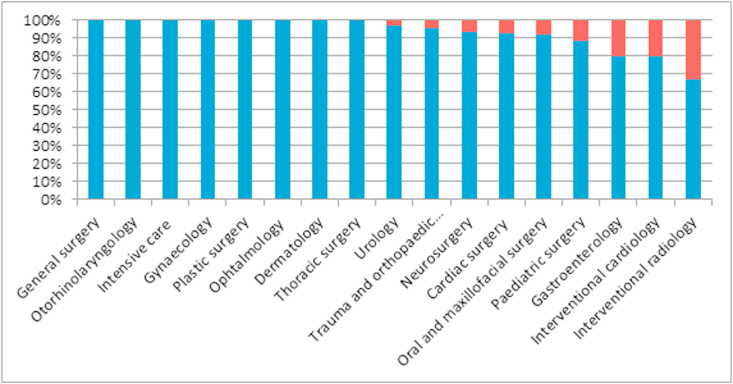
An average of 93.7% responded that a voice recognizer without headset would be conceivable for documentation during treatment or an examination. For most physicians of different specialties, a headset-free solution is conceivable (Table 1, Fig. 2).
Table 1.
Desirable requirements of a medical ASR system according to respondents.
| Desirable requirements | % |
|---|---|
| Over 95% reliability | 93.10% |
| Easy data entry/documentation via speech | 72.41% |
| No headset microphone | 71.84% |
| Multiple devices to be controlled by voice | 67.24% |
| Access patient data during surgery | 60.34% |
| Offline use | 56.32% |
| Interaction between user and device during operation | 50.57% |
| Training mode | 47.13% |
Fig. 2.
Percentage of participants who can imagine using a headset-free solution in the OR divided into different specialties.
Additionally, we asked participants to rate whether they consider the possibility of controlling medical devices by thoughts through an EEG headset to be promising for the future, of which 30.6% answered positively.
3.3. Subgroup statistical analysis
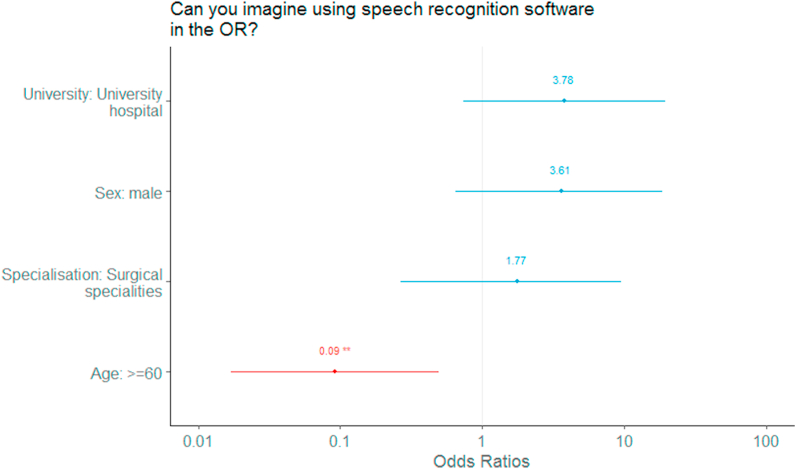
When age is matched with responses regarding the use of ASR, it is noteworthy that 58.3% of physicians over the age of 60 consider the use of speech recognition without a headset to be personally applicable, while 41.7% cannot imagine this application (Fig. 3).
Fig. 3.
Odds ratio of subgroup analysis regarding the imaginability of using ASR.
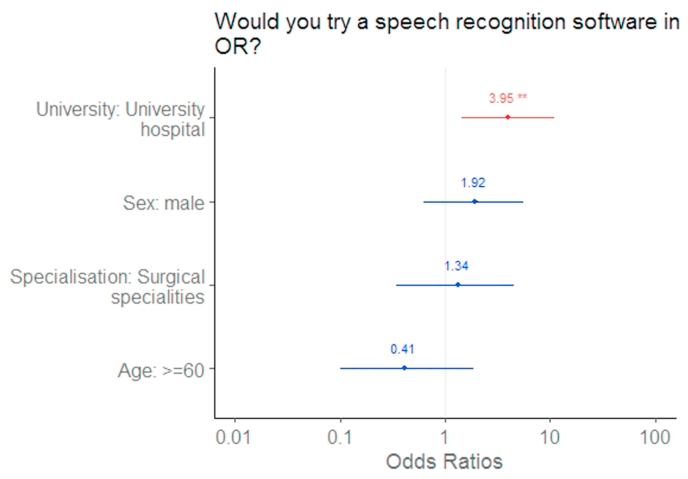
Among the under 60-year-olds, 157 (96.3%) can imagine an ASR application in the OR while 6 (3.68%) do not envision it (p < 0.001). Furthermore, there was a significant difference between ≥60 and < 60 years old participants regarding the potential of ASR in the OR (p = 0.006) (Fig. 3). However, when participants were subdivided by age groups, chi-squared analysis revealed no significant association between age and the use of ASR in the operating room (p = 0.236). Furthermore, the association between university and non-university hospitals and the willingness to try ASR remained statistically significant (p = 0.001) (Fig. 4).
Fig. 4.
Odds ratio of subgroup analysis regarding the openness to try ASR.
There were overall no statistically significant differences regarding physicians' gender and the professional position. However, regarding the specialty, 90.1% of participants with surgical specialties see potential in the use of ASR, while 73.7% of physicians working in non-surgical specialties evaluate its future potential as high (p = 0.01).
4. Discussion
In summary, regardless of age, gender, specialty, professional experience and position, it is agreed that the implementation of ASR in the OR is a desirable tool required in the near future.
A homogeneous result was also achieved concerning the requirements for a future ASR system in ORs. The majority esteems voice control for the position of the operating video- and documentation system, room lighting, and setup menu of the endoscope's light source as desirable. A disproportion between desire and reality in the application of ASR is hereby shown. Coupled to the fact that the basic technical requirements for an intelligent ASR are available, even in noisy environments, it is assumed that an ASR-controlled operating theatre is not far from becoming a reality [8,12].
Interesting findings are revealed when combining different queried characteristics of the interviewees with their opinions towards ASR. It is noteworthy that only 41.7% of physicians over the age of 60 consider the use of a speech recognizer without a headset to be personally imaginable for them, compared to 96.3% of the physicians under the age of 60. Consequently, it is the new generation of doctors who will be the driving force behind the innovative changes and further technological developments towards a future “intelligent operating room”. Although interventional radiologists and endoscopy/hemodynamic internists also frequently work in an OR– it was interesting to see differences in their opinion towards ASR in the OR. Surgical specialists evaluate the potential of ASR in the OR to a greater extent, which is presumably attributed to the fact that they spend a considerable amount of their working time in the OR.
Physicians working in university hospitals would consider testing an ASR to a greater extent. In a university hospital, new promising research projects are often part of studies and everyday practice, which might lead to greater openness in this regard.
Miscommunication is a common problem in the OR. In 2008, the WHO introduced and recommended the Surgical Safety Checklist [13]. By using ASR for basic instructions to control technical equipment, the focus of communication with OR nurses could be concentrated on essential content that is of vital importance for patient safety [11].
Considering that in the operating theatre there are often heterogeneous noise levels and constantly changing personnel, the ASR has to filter out the “commanding physician” and could place obstacles in the way.
In the context of studies evaluating intelligent ORs, voice control systems were tested and found to be feasible [14]. Further voice control studies in the OR should be carried out to investigate which technical challenges still have to be overcome. There is presently a dearth of studies available about the implementation of ASR in surgery.
In summary, it can be stated that in times in which artificial intelligence, robotic-assisted surgery, and virtual reality have found their way into the OR, it seems appropriate to introduce ASR combined with technical equipment control which can be regarded as contemporary [15,16].
The increased technical support could lead to a smoother workflow, safer surgical procedures and better patient outcomes since interpersonal conversations can be focussed on patient-related issues.
There are certain limitations to the study. There is no validated e-mail distribution list of representatives of different surgical disciplines in Germany. In the study's design, we made an effort to map a representative sample of such physicians. However, we could not verify whether the messages in the e-mail accounts are actively accessed which is why we decided to activate a reminder.
The study had a low response rate which can be explained, among other things, by the fact that a considerable number of the doctors that were contacted work in private practices. Presumably, they have to deal with less complicated surgical systems, do not perform complex surgical procedures or could not answer the survey due to time constraints.
While there is no ASR sufficiently developed for an OR on the market, it is hard to estimate the usefulness for those having no experience with ASR at all. Further studies should be conducted with a working ASR in the OR.
In conclusion, for an ASR system to be implemented in the OR, it needs to be sophisticated and updatable since there are still several requirements to be fulfilled. Its application in the OR would have to be further researched and improved to be individually tailored to the needs on-site. This is of vital importance since the aim is to provide an enhancement rather than a time-consuming gadget. To go one step further, almost a third of those surveyed consider the possibility of controlling medical devices with an EEG headset to have a promising future. This can be interpreted as a future perspective on the path to more technological medicine.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethical standards
No patients were included in this study and the survey was completed anonymously.
Author contributions
A.S., study design and manuscript drafting; D.W., conceptualization, P.F.P., manuscript editing; R.S., manuscript drafting and editing; E.P., statistical analyses; A.M., project supervision.
Provenance and peer review
Not commissioned, externally peer reviewed.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The article processing charge was funded by the Baden-Wuerttemberg Ministry of Science, Research and Art and the University of Freiburg in the funding programme Open Access Publishing.
References
- 1.Levis J., Suvorov R. Automatic speech recognition. In: Chapelle C., editor. Encyclopedia of Applied Linguistics. Blackwell; 2012. [Google Scholar]
- 2.Pieraccini R. From audrey to siri: is speech recognition A solved problem? 2012. http://www.icsi.berkeley.edu/pubs/speech/audreytosiri12.pdf
- 3.Juang B.H., Rabiner L.R. 2004. Automatic Speech Recognition – A Brief History of the Technology Development. [Google Scholar]
- 4.Keshet J. Automatic speech recognition: a primer for speech-language pathology researcher. Int. J. Speech-Language Pathol. 2019;20(6):599–609. doi: 10.1080/17549507.2018.1510033. [DOI] [PubMed] [Google Scholar]
- 5.Ballard K.J. Feasibility of automatic speech recognition for providing feedback during tablet-based treatment for apraxia of speech plus aphasia. Am. J. Speech Lang. Pathol. 2019;28(2S):818–834. doi: 10.1044/2018_AJSLP-MSC18-18-0109. [DOI] [PubMed] [Google Scholar]
- 6.Grasso M.A. Automated speech recognition in medical applications. M Comput. 1995;12(1) [PubMed] [Google Scholar]
- 7.Renato A. 2019. Design And Evaluation Of an Automatic Speech Recognition Model For Clinical Notes In Spanish in a Mobile Online Environment Studies in Health Technology and Informatics; p. 264. [DOI] [PubMed] [Google Scholar]
- 8.Miehle J. The next step: intelligent digital assistance for clinical operating rooms. Innov. Surg. Scie. 2017;2(3) doi: 10.1515/iss-2017-0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ginsberg H.S. Noise levels in modern operating rooms during surgery. J. Cardiothorac. Vasc. Anesth. 2013;27(3):528–530. doi: 10.1053/j.jvca.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Dekker M.L. vol. 1281. Elsevier International Congress Series; 2005. pp. 653–655. (Virtual Microphones in the Operating Theatre). [Google Scholar]
- 11.Gillespie Brigid M. Team communications in surgery – creating a culture of safety. J. Interprof. Care. 2013;27(5) doi: 10.3109/13561820.2013.784243. [DOI] [PubMed] [Google Scholar]
- 12.Chan Z.Y., Shum P. the 2nd International Symposium. 2018. Smart office: a voice-controlled workplace for everyone. [Google Scholar]
- 13.Holtel M. 2017. Kommunikation: Die wichtigste Nebensache im OP. Deutsches Ärzteblatt; p. 114. [Google Scholar]
- 14.Kubben P.L., Sinlae R.S.N. Feasibility of using a low-cost head-mounted augmented reality device in the operating room. Surg. Neurol. Int. 2019;10(26) doi: 10.4103/sni.sni_228_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.I A. Artificial intelligence and robotics: a combination that is changing the operating room. World J. Urol. 2019 doi: 10.1007/s00345-019-03037-6. [DOI] [PubMed] [Google Scholar]
- 16.Sparwasser P.M. Augmented reality and virtual reality in the operating theatre status quo und quo vadis. Aktuelle Urologie. 2018 doi: 10.1055/a-0759-0029. [DOI] [PubMed] [Google Scholar]