Abstract
A hallmark of complex humanitarian emergencies is the collective exposure, often over extended periods of time, to political violence in the forms of war, terrorism, political intimidation, repression, unlawful detention, and forced displacement. Populations in complex humanitarian emergencies have higher risks of multiple co-morbidities: mental disorders, infectious diseases, malnutrition, and chronic non-communicable diseases. However, there is wide variation in the health impacts both across and within humanitarian emergencies. Syndemic theory is an approach to conceptualizing disease and social determinants to understand differential patterns of multi-morbidity, elucidate underlying mechanisms, and better design interventions. Syndemic theory, if applied to complex humanitarian emergencies, has the potential to uncover origins of localized patterns of multi-morbidity resulting from political violence and historical inequities. In this paper, we present two case studies based on mixed-methods research to illustrate how syndemic models can be applied in complex humanitarian emergencies. First, in a Nepal case study, we explore different patterns of posttraumatic stress disorder (PTSD) and depression co-morbidity among female former child soldiers returning home after war. Despite comparable exposure to war-related traumas, girl soldiers in high-caste Hindu communities had 63% co-morbidity of PTSD and depression, whereas girl soldiers in communities with mixed castes and religions, had 8% PTSD prevalence, but no cases of PTSD and depression co-morbidity. In the second case study, we explore the high rates of type 2 diabetes during a spike in political violence and population displacement. Despite low rates of obesity and other common risk factors, Somalis in Ethiopia experienced rising cases of and poor outcomes from type-2 diabetes. Political violence shapes healthcare resources, diets, and potentially, this epidemiological anomaly. Based on these case studies we propose a humanitarian syndemic research agenda for observational and intervention studies, with the central focus being that public health efforts need to target violence prevention at family, community, national, and global levels.
Keywords: Humanitarian emergencies, Political violence, Syndemic, War, Conflict, Mental health, Non-communicable diseases (NCDs)
1. Introduction
Political violence -- including internal conflicts, international wars, terrorism, political intimidation and repression, unlawful detentions of dissidents, and population displacement -- is commonplace around the world and has devastating consequences on human health (Herbert et al., 2011; Krug et al., 2002; Wenzel et al., 2015). The presence of political violence distinguishes complex humanitarian emergencies from other humanitarian emergencies. A “complex humanitarian emergency” is defined as a crisis when there is a breakdown in a country's political system or sovereign authority resulting from internal or external conflict, necessitating an international response (Burkle, 2006). As such, complex humanitarian emergencies are defined by their association with various forms of political violence (Edkins, 1996; Macrae and Zwi, 1994), their embeddedness in long histories of inequity, colonialism, and conflict (Albala-Bertrand, 2000), and a subsequent cascading effects on population health (Hammer et al., 2018; Salama et al., 2004; Toole and Waldman, 1997).
Populations affected by complex humanitarian emergencies experience increased rates of physical injuries, increased rates of acute and chronic forms of malnutrition, increased risk of infectious diseases, increased rates of mental illness, and disruptions or gaps in care for chronic and non-communicable conditions (Charlson et al., 2019; Chen et al., 1999; Hammer et al., 2018; Jobanputra et al., 2016; Salama et al., 2004; Toole and Waldman, 1997). Multi-morbidity is more the rule than the exception. However, little epidemiological or other research examines how exposures to political violence affect subsequent patterns of multi-morbidity in humanitarian emergency-affected populations. Epidemiological research in complex humanitarian emergencies predominantly presents descriptive data on the patterns of health outcomes in a population with less attention to how different health conditions, exposures to different forms of violence, and contextual factors interact.
Health needs vary significantly during complex humanitarian settings. Within populations affected by the same conflict, there may be tremendous epidemiological heterogeneity in the burdens of disease, capacities to manage disease across different demographic groups and parties to the conflicts at hand. Standard epidemiological models often have been limited in understanding patterns of health outcomes in complex humanitarian emergencies and in determining how best to respond or prevent the confluence and interactions of multiple health problems. Guidelines for responding to health needs in humanitarian crises such as the Sphere Handbook (2018) continue to rely upon single-disorder approaches to disease classification, rather than employing an integrative or interactive perspective on the potential of interacting multi-morbidities, i.e., standard reporting does not routinely present rates and prevalences of multi-morbidities.
Syndemic theory presents an innovative way to conceptualize and advocate for responses in complex humanitarian emergencies to address multi-morbidity and the exponentiation of interacting negative health outcomes (Kohrt et al., 2019). The basic principle of syndemic theory is that particular sociocultural settings can contribute to increased risk of co-morbid conditions. The concept of syndemic emerged early in understanding HIV in the United States. The medical anthropologist Merrill Singer observed that HIV rates were especially high among persons with substance abuse disorders who also had experiences of exposure to violence (Singer, 1996). The pattern was not simply explained by HIV transmission in the context of substance abuse (e.g., sharing needles), it was also important to account for violence histories that shaped risk-taking behaviors and limited people's access to and use of social and health services. Singer's Substance Abuse Violence AIDS (SAVA) syndemic model was instrumental in understanding variation in exposure to and rates of HIV in different communities. More recently, the Violence Immigration Depression and Diabetes (VIDDA) syndemic model has been used to understand why Mexican immigrants are more likely to have greater co-morbidity of depression and diabetes compared to the non-immigrant, non-Mexican populations in Chicago (Mendenhall, 2012).
Notably, each of these models integrates measures of people's exposure to different forms of violence to better understand the exacerbation of risks for compounding negative health outcomes. In the case of SAVA, Singer highlights the manifold effects of different forms of community violence. In the VIDDA model, Mendenhall examines the manifold effects of intimate partner violence. Violence, in both models, is key to the exacerbation of risk of multi-morbidity. The role of violence is similarly important to understand interacting multi-morbidity in the context of complex humanitarian emergencies. Violence has both internal effects on the body and external effects on lived experience. Witnessing violence, experiencing violence, and the threat of violence impact stress pathways both to trigger inflammatory processes and to suppress viral responses (Lindqvist et al., 2014; Kohrt et al., 2016). Exposure to violence impacts metabolism, cardiovascular function, and pain pathways (Alhalal et al., 2018; Kaur, 2017; Kliewer et al., 2019; Konstam and Konstam, 2019; Liu et al., 2020; Rivara et al., 2019). Outside the body, violence transforms the social world by reducing access to restorative social relationships, decreasing access to health, educational, and social services, and limiting economic and livelihood opportunities (Carruth, 2014; Willman and Team, 2009; Yodanis et al., 2000). In the context of political violence, these impacts are not limited to a few individuals but transforms entire societies (Galtung, 1969, 1990). Given these internal and external impacts of political violence, we cannot assume that health conditions will follow the same epidemiological and clinical profiles as one observes among populations with less exposure to state-level, community, and interpersonal violence.
Just as human bodies and minds bring different resources and vulnerabilities to the impact of violence, people's histories also influence how violence transforms health. For example, in societies with long histories of economic exploitation, colonial occupation, social divisions in the form of gender, racial, ethnic, and religious discrimination, and the undermining of civic institutions, political violence is more likely to have dramatic health impacts (Farmer, 2003). This is evident more than ever with the major disparities in COVID-19 morbidity and mortality among populations subjected to prolonged histories of structural and direct violence, as demonstrated by the health burden among Black American, Latinx, and immigrant communities in the United States (Gravlee, 2020; Poteat et al., 2020). The COVID-19 syndemic of pre-existing health conditions, COVID-19, and exposure to violence highlights the need to advance syndemic research among populations affected by political violence.
To explore this proposed model of syndemic effects in the context of complex humanitarian emergencies, we present two case studies. These studies did not involve an a priori test of syndemic models in these two contexts, but instead we apply a conceptual model of syndemic effects to prior research conducted in complex humanitarian emergencies. We retrospectively examine data collected during separate research projects in Nepal and Ethiopia (Carruth et al., 2020; Carruth and Mendenhall, 2019; Kohrt et al., 2008, 2010a) to theorize how the notion of syndemics potentially helps to overcome both the fragmentation of humanitarian responses and the siloed nature of epidemiological research during these emergencies. This sets the stage for a research agenda on syndemic effects and syndemic-informed care in complex humanitarian emergencies. In the first case study, we evaluate the co-morbidity of PTSD and depression among female former child soldiers in Nepal. We explore why some communities had low rates of PTSD and depression co-morbidity, whereas other communities had extremely high rates. These findings can best be understood via the interaction of political violence exposure with differences in historical and current discrimination against women.
In the second case study, we explore high-rates of type-2 diabetes alongside food insecurity among Somalis in Ethiopia. Given the low prevalence of common risk factors for type-2 diabetes, such as obesity and smoking, among people there, diabetes prevalence and symptoms are surprising. However, attention to the potential physiological effects of political violence on the body and recognition of how political violence has changed local diets, may help explain these health outcomes. We conclude with recommendations for designing both epidemiological studies and healthcare responses for complex humanitarian emergencies within a model of syndemic effects.
2. Case study 1: differential co-morbidity of depression and PTSD among child soldiers in Nepal
The first case study explores patterns of mental health co-morbidity in Nepal among adolescent girls exposed to war, including girls who became child soldiers. From 1996 to 2006, there was a civil war in Nepal between the Communist Party of Nepal (Maoists) and the Hindu monarchy government. The Maoists regularly recruited minors into their armed forces. By the end of the war in 2006, there were more than 9000 youth under the age of 18 who were part of the fighting forces. One of the striking features of the Maoist conflict in Nepal was that girls were typically recruited as combatants in the same roles as boys. This contrasts with East and West Africa where girls were more likely kidnapped and forced into sexual relationships and marriage with male combatants.
Through a study commissioned by UNICEF, the rates of mental health problems of youth who had informally returned home at the end of war were studied (Kohrt et al., 2008). (Ethical approval provided by the Nepal Health Research Council and Emory University.) “Informal return” refers to the process where youth left the armed forces and returned home independently rather than through formal Disarmament, Demobilization, and Reintegration programs (DDR). In DDR programs, standing militaries are first inspected by humanitarian actors. Then persons under 18 years of age are removed and entered in temporary housing programs while family members to receive them are identified. After this, they can be formally returned to the community with service packages. Our study, in contrast to traditional DDR processes, worked with the informally returning youth and found wide variations in the rates of mental health problems among former child soldiers and youth throughout the country. In some regions of the country, more than half of former child soldiers were above cut-offs for depression and PTSD on culturally and clinically validated assessment tools (Kohrt et al., 2011). However, in other regions of the country, rates were only to 1 out of 10. The disparity in prevalence rates was strongest among girl soldiers. Moreover, the rates of co-morbidity varied widely, with some regions showing an association between PTSD and depression, but not in other regions.
2.1. Ethnographic research to identify sociocultural and contextual contributors to a syndemic pattern
Ethnographic research and other qualitative methods were used to explore why these differences existed, to propose statistical analyses, and to determine what needed to be done to address the burden of mental health and psychosocial problems (Kohrt et al., 2010b). A team of Nepali researchers were trained in qualitative and ethnographic methods and the first author spent time conducting participant observation in different regions of the country. The team found that although the types of traumatic events during the war appeared to be similar for child soldiers across the country, the experience of reintegration varied widely (Kohrt et al., 2010a). In some regions of the country, child soldiers were discriminated against when they came home. Female former child soldiers, in particular, were discriminated against by their families and communities. However, in other regions of the country, girl soldiers were welcomed back into their families and communities, even without formal programs from UNICEF or other humanitarian agencies.
The ethnographic and other qualitative work suggested that the discrimination against women in these communities played a role in these reintegration differences (Kohrt et al., 2010b). In some communities, discrimination against women in general and discrimination against girl soldiers was frequently described. In these communities, the girl soldiers were more likely to described high levels of distress. In other communities, there was less qualitatively reported general gender discrimination, and less discrimination against girl soldiers specifically. One distinguishing feature between the two types of communities was that the communities with high levels of gender discrimination and stigmatization of former girl soldiers were more likely to be predominantly high-caste Hindu groups.
In the high-caste Hindu communities, there was more focus on describing girls in terms of their ritual purity, with former girl solders described as being ‘polluted’ (Nepali: jutho) and no longer religiously pure (choko). In contrast, in regions with mixed caste/ethnicity including high- and low-caste as well as Buddhist ethnic groups, the former child soldiers were less likely to describe experiencing discrimination in with the framing of these Hindu concepts of purity. The gender discrimination played out in other differences between the communities, such as lower female literacy, lower female school completion, and other performance on Gender Development Indices (Kohrt et al., 2010a). This suggests that although trauma levels were comparable for the girls in the two types of communities, the differences in gender discrimination likely set the stage for differences in mental health sequelae of the trauma.
2.2. Assessing differences in comorbidities by sociocultural context
Based on our prior quantitative and qualitative findings, we conducted exploratory analyses to assess a potential syndemic model. In our model, the specific co-morbidity of interest was PTSD and depression. Globally—whether referring to humanitarian conflicts in low-income countries or working with veterans in high-income countries—PTSD is often co-morbid with depression (Nesterko et al., 2020; Peconga and Høgh Thøgersen, 2019; Stander et al., 2014). However, the rates of co-morbidity vary widely by populations and settings. In some conflict affected populations rates of depression without PTSD are high, and other in other populations there may be high comorbidity of depression and PTSD (Kohrt et al., 2012; Nesterko et al., 2020; Trief et al., 2006). We wanted to determine the rates of co-morbidity in the child soldier and civilian children populations in post-conflict Nepal. The socio-cultural context of interest was the comparison of predominantly high-caste Hindu communities with communities that were more mixed by ethnicity and caste.
Because the socio-cultural context appeared to particularly influence girls’ mental health, we limited our syndemic analysis to female former child soldiers and comparison civilian girls. The sample included 148 girls: 75 female former child soldiers, and 73 civilian girls (see Kohrt et al., 2008 for recruitment and sample details). We analyzed the samples comparing girls living in predominantly high-caste Hindu communities (63 child soldiers and 60 civilians) vs. girls in mixed ethnic and caste communities (12 child soldiers and 13 civilians). Because the study was not originally designed to test this syndemic association, the sample sizes are not equal between the two types of communities.
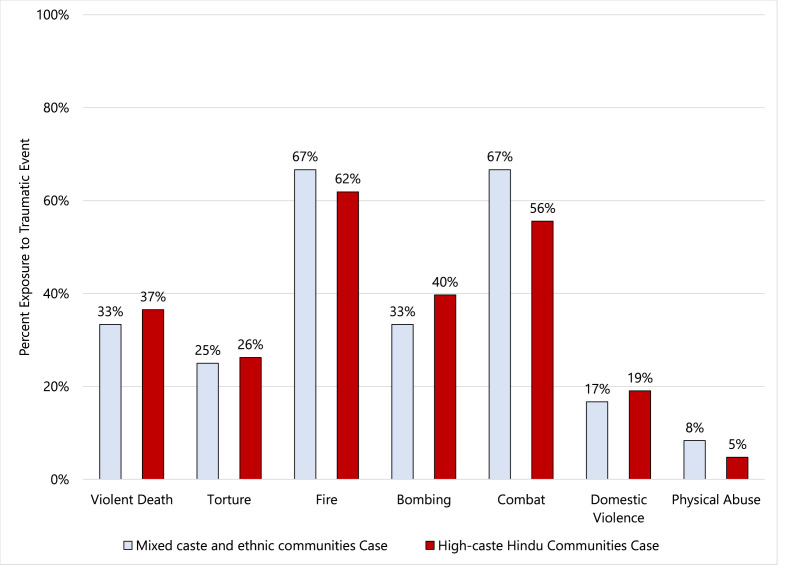
We then evaluated whether female former child soldiers in the high-caste Hindu communities and female civilians in the mixed ethnic-caste communities had comparable levels of war-related and other traumas. We found that female former child soldiers in both communities had similar levels of exposure to war traumas (witnessing violent death, witnessing torture, experiencing bombing, war-related fires, and exposure to combat) and pre-war traumas (domestic violence and physical abuse), see Fig. 1 .
Fig. 1.
Exposure to traumatic events among female former child soldiers in mixed caste/ethnic communities vs. high-caste communities.
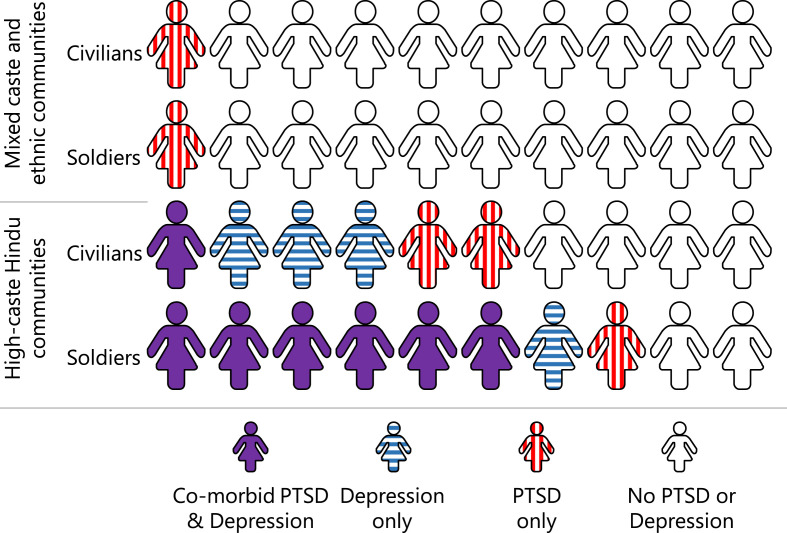
We then evaluated co-morbidity rates of PTSD and depression in the two communities. We found that PTSD and depression symptom scores were not correlated in the mixed religious/caste communities (r = 0.04, p = 0.87). However, the PTSD and depression symptom scores were strongly correlated in the high-caste Hindu communities (r = 0.58, p<0.001). Using a culturally and clinically validated cut-off for PTSD and depression (Kohrt et al., 2011), we then identified the number of child soldier and civilian girls scoring above the cut-offs for these conditions. In the mixed religious and ethnicity communities, 8% of female child soldiers and 8% of female civilians scored above the cut-off for PTSD, but none of the girls in either group were above the cut-off for depression. In the high-caste Hindu communities, among civilian girls, 17% had PTSD only, 32% had depression only, and 8% had co-morbid PTSD and depression. For female former child soldiers, 11% had PTSD only, 11% had depression only, and 63% had co-morbid PTSD and depression (see Fig. 2 ).
Fig. 2.
Percentage of civilian girls and girls soldiers with PTSD and depression by type of community.
It is striking that female former child soldiers with comparable levels of trauma exposure had such different mental health profiles: in the mixed religious and ethnic communities, no girls had co-morbid PTSD and depression, but in high-caste communities, 6 out of 10 girl soldiers had co-morbid PTSD and depression. These findings were supported by assessment of discrimination and stigma, with both civilian and child soldier girls in high-caste communities reporting higher levels of discrimination compared to girls in mixed-religious communities; in prior analyses, we have shown that children in high-caste Hindu districts reported experiencing greater levels of family and community discrimination and lower levels of supports (Kohrt et al., 2010a). One possible explanation for the differences is that the likelihood of developing depression was already greater in the high-caste Hindu communities. There is evidence to support this with large gender differences in depression rates in high-caste Hindu regions of Nepal (Kohrt et al., 2009, 2012). Therefore, the girls in these communities were already likely to develop depression during adolescence and young adulthood. Then, the traumatic experience in the context of gender discrimination, low social support, and a social context predisposing for depression contributed to the increased likelihood of developing PTSD.
This provides a useful illustration for how syndemics may work in humanitarian settings. Although the traumas of interest (combat and other war-related exposures) were comparable for girl soldiers in two different types of communities, the rates of mental health problems and co-morbidities were strikingly different. This suggests that it is vital to understand the community context that trauma survivors grow up in and return to after their exposure to being a child soldier. These findings suggest that differences in the religious/ethnic composition of the communities influenced the experiences of children in the community and particularly the experience of female former child soldiers (Kohrt et al., 2010b). From a mechanistic perspective, caste-based Hindu discrimination may contribute to greater levels of stress in daily living for girls which is a risk factor for depression, and depression may then increase the likelihood of PTSD. It is also possible that the discrimination leads to lower levels of social support, which we documented, and this increases the risk of PTSD, with the greater severity of PTSD increasing likelihood of depression. This points to the need to target aspects of gender-based discrimination related to high-caste Hindu culture to interrupt the interaction of PTSD and depression in this context.
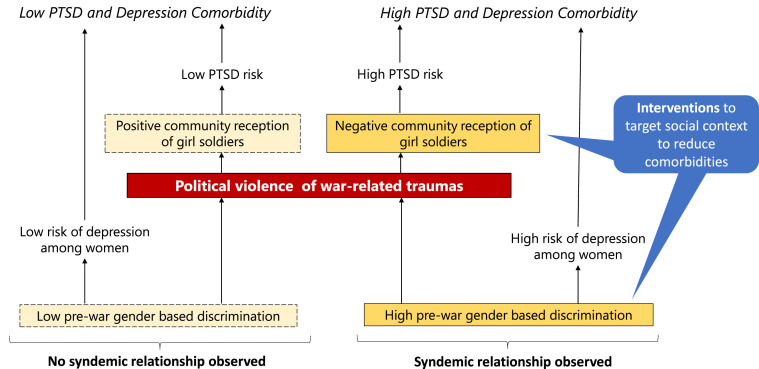
2.3. Interventions targeting sociocultural components of syndemics
Using a syndemic lens, it is possible to re-evaluate how interventions for former child soldiers may have worked in post-conflict Nepal. Given that the sociocultural context of the returning soldiers appeared to play a major role in determining the regional differences in burden and co-morbidity of mental health problems, we developed an intervention that focused on community-level support of former child soldiers (Kohrt et al., 2015), rather than an exclusively trauma-focused individual treatment. From a syndemic perspective, the sociocultural context of high rates of discrimination and social exclusion was contributing to the comorbid depression and PTSD (see Fig. 3 ). The intervention involved training cadres of community psychosocial workers (CPSWs) with a 28-day curriculum delivered in 4 different modules over a 4-month period (Kohrt et al., 2015). CPSWs were trained to work with teachers, community leaders, parents and relatives, religious leaders, health workers, and other community stakeholders engaged in children's and adolescents' lives. This program emphasized activities such as reducing discrimination by teachers in schools directed toward former girl soldiers. CPSWs worked with teachers to help reduce the teachers' biases and discrimination against girl soldiers. In addition, through UNICEF support programs, girl soldiers were given opportunities to pursue activities they were most interested in for their future, including returning to formal schools, informal education, skills training (e.g., seamstress), and livelihood programs (e.g., receiving livestock and training).
Fig. 3.
Pathways in different types of communities leading to low vs. high rates of PTSD and depression comorbidity based on absence or presence of a symdemic relationship.
Rates of depression and PTSD among former child soldiers significantly reduced one year after the program and reached comparable levels to civilian children; in contrast, socioeconomic interventions (e.g., education, livelihood training, small grants) that targeted specific children (rather than the community) did not show relative differences in benefit (Kohrt et al., 2015, Adhikari et al., 2014). This suggests that the community level effects may have been more beneficial than individual supports received by a specific child. These findings highlight that when differences in sociocultural risk factors are found to be associated with differences in multi-morbidity, then intervening on the sociocultural risk factors may contribute to reduction in health problems. Ultimately, mitigating the effects of political violence on multi-morbidity likely requires addressing current social inequities that shape the form and severity of trauma's impact.
3. Case study 2: diabetes, anxiety, persistent wounds, and humoral dysfunction in the Somali Region of Ethiopia
The case study on diabetes in Somali communities in eastern Ethiopia builds on findings from the second author's long-term ethnographic research on medical care and humanitarian assistance in the Somali Region of Ethiopia during five extended research stints from 2007 to 2018 (Carruth, 2014; Carruth, 2016; Carruth, 2018). During this larger project, even during droughts and outbreaks of political violence, local clinicians remarked on several occasions that rates of type-2 diabetes mellitus among Somalis in Ethiopia seemed to be rising and were unexpectedly high given low rates of obesity, but there was (and still is) no systematic, population-based research to investigate this possibility.
In response to this, four researchers who have known each other for 10 years collected additional data related to diabetes and diet among Somali Ethiopians in Ethiopia: a university professor, two local Somali research assistants, and a local community health worker (in Ethiopia, called a “health extension worker”). Another university professor with experience in studying diabetes and public health assisted with research design and data analysis (Carruth, 2020). The field team in Ethiopia recruited and collected basic survey and anthropometric data from 108 individuals including 85 Somali-Ethiopians who self-reported a type-2 diabetes diagnosis and 23 additional persons who are adult siblings of these persons with diabetes living in communities nearby. Anthropometric data included weight, height, and both hip and waist circumferences. We used these metrics to calculate participants’ Body Mass Index (BMI) as well as their waist-to-hip ratio as a proxy of abdominal adiposity, as recommended by the World Health Organization and diabetes researchers working in sub-Saharan Africa (Mbanya et al., 2010; Vazquez et al., 2007; World Health Organization, 2008). We collected basic survey data including, as appropriate, age, residential location, typical diet, dietary changes, seasonal dietary shifts, food insecurity, therapeutic regimens, current and past symptoms, and more. Additionally, with all 108 participants we collected finger stick blood samples, which were placed on Dried Blood Spot (DBS) cards, refrigerated, and mailed to the University of Washington Department of Laboratory Medicine for analysis. The DBS samples were analyzed for levels of hemoglobin A1c (abbreviated as HbA1c), cholesterol (CHO), high-density lipoproteins (HDL), triglycerides (TRG), and C-Reactive Protein (CRP); see Table 1 for a summary of anthropometric and biological results.
Table 1.
Anthropometrics and Biomarkers associated with chronic anxiety and stress and higher risk additional chronic non-communicable diseases.
| Women (n = 68) | Men (n = 40) | No Diabetes Diagnosis (n = 23) | Diabetes Diagnosed (n = 85) | Total (n = 108) | |
|---|---|---|---|---|---|
| Age | 46.7 years | 48.9 years | 41.6 years | 49.1 years | 47.5 years |
| BMI | 27.4 | 22.1 | 27.9 | 24.7 | 25.4 |
| Waist-to-Hip Ratio | 0.89 | 0.92 | 0.88 | 0.91 | 0.90 |
| HbA1c (direct) | 7.66 | 7.34 | 6.06 | 8.8 | 7.5 |
| Cholesterol (direct) | 165 | 156 | 113 | 123 | 161 |
| HDL (Direct) | 55.4 | 55.6 | 40.6 | 36.5 | 55.5 |
| TRG (Direct) | 254.6 | 257.1 | 220.7 | 226.0 | 255.5 |
| CRP (Direct) | 4.83 | 2.98 | 3.42 | 2.97 | 4.13 |
*all data are reported as averages per group unless otherwise specified.
At the time of the biological and anthropometric data collection, we also conducted 16 in-depth semi-structured qualitative interviews with a sub-set of patients with T2DM diagnoses and two semi-structured interviews with their siblings living in close proximity. We also carried out in-depth interviews plus additional participant-observation over the course of eight weeks in rural and urban clinics, hospitals, and community spaces where patients with T2DM work and live, and we carried out several informal conversations and semi-structured qualitative interviews with two local community health workers, two physicians serving the Somali patient population, one hospital administrator, two persons who served as health policymakers within the regional government, and three policymakers within international nongovernmental agencies (totaling 28 qualitative interview participants). This study was approved by the IRBs at Anonymized University, Anonymized University, and Anonymized University in Ethiopia.
3.1. Repeated conflicts, displacements, and disasters in the Somali Region of Ethiopia
Ethiopia has achieved remarkably high and consistent economic growth rates over the last fifteen years and is a model “developmental state” (Clapham, 2018). Ethiopia is also frequently portrayed as a global health model (Østebø et al., 2018). Its governmental health extension worker program, for example, has deployed thousands of healthcare providers to rural parts of the country and helped to improve many Ethiopian's access to basic primary healthcare and vaccinations (Maes, 2016). This and other programs have contributed to a nearly halving of nationwide infant and child mortality rates, and rates of both acute and chronic forms of malnutrition among children continue to fall (Demographic and Health Survey Program, 2016; UNICEF, 2019).
However, disparities between the Somali Region and the rest of Ethiopia persist (Demographic and Health Survey Program, 2016; UNICEF, 2018, 2019). Infant and maternal mortality rates in the Somali Region are higher than almost anywhere else in the country; people's access to and use of regulated primary healthcare facilities is lower there than in other regions; and major investments in technology, industry, and agriculture are few and far between in the Somali Region compared to other parts of Ethiopia (Demographic and Health Survey Program, 2016; Human Rights Watch, 2018). Despite notable political reforms since the ascension of Prime Minister Abiy Ahmed to the office of Prime Minister in 2018 (Devermont and Temin, 2019), political insecurity, population displacement, human rights abuses, and outbreaks of violence in eastern Ethiopia continue (Human Rights Watch, 2018; International Organization for Migration, 2019; ReliefWeb, 2019).
Recurrent droughts in different parts of the Somali Region prior to this field work in 2003–2004, 2008–2009, 2010–2012, and again in 2015–2016, together with increases in the numbers of violent conflicts and population displacements from 2016 to 2018, increased local rates of food insecurity and malnutrition throughout the region (Integrated Regional Information Network, 2017). Cases of water-borne diarrheal diseases, including cholera and dysentery, repeatedly spiked in emergency-affected places and in camps of displaced people (UNICEF, 2018; UNICEF, 2019). Markets of fresh milk, sorghum, and livestock declined in these difficult years, and prices for staple goods increased. Many families were forced to sell their livestock or resettle elsewhere. Droughts also exacerbated fights over access to pastureland and water along regional boundaries (Integrated Regional Information Network, 2017; ReliefWeb, 2019; UNOCHA, 2018).
Data collection for the case study of diabetes among Somalis happened during a period of political violence and a complex humanitarian emergency characterized by internal population displacement, political violence, and increases in incidences of diarrheal diseases and malnutrition in July–August 2018. Specifically, in, in early August 2018, conflict erupted in and around Jigjiga when the Ethiopian Prime Minister Abiy Ahmed ordered the arrest of the Somali Regional President Abdi Iley. The President's loyalists protested and retaliated against government officials and suspected traitors in and around the regional capital. At least 100 people were killed and nearly 150,000 people fled the immediate area (Human Rights Watch, 2018; UNICEF, 2018; UNOCHA, 2018). Due to this violence and other conflicts, by December 2018, there were nearly 3 million internally displaced persons (or IDPs) throughout Ethiopia (UNICEF, 2018)--more than any other country in the world (International Organization for Migration, 2019).
When violence broke out in Jigjiga mid-way through this study, members of the field team fled for safety to the outskirts of the city of Dire Dawa and then traveled to stay in rural communities closer to the borders of Djibouti and Somaliland. We continued recruiting and enrolling participants throughout this period, even as people were frequently displaced or away from their homes. Consequently, the humanitarian crisis unfolding around us presented an opportunity to better understand the challenges patients and caregivers face in accessing medical care and treatments during periods of concurrent social upheaval in the context of chronic food insecurity.
3.2. Surprising symptoms and comorbidities
Anthropometric and biological data collected with the diabetes patients and a few of their siblings living nearby revealed a few important patterns. First, as we discuss in greater detail in other publications (Carruth et al., 2020), persons who had received a previous diabetes diagnosis were on average older, shorter, lighter in weight, compared to their siblings who had not been diagnosed with diabetes, and had a body mass index within the international standard “healthy range” of between 20 and 25. The diabetes patients also had smaller waist and hip circumferences compared to those who had not received a diabetes diagnosis, although they had a slightly larger waist-hip ratio. Overall, overweight and obesity were not significantly associated with diabetes outcomes, although a larger sample size would help elucidate additional potential associations.
Persons in our sample who had received a diabetes diagnosis previously had higher HbA1c levels (a measure of average blood glucose levels, across the previous two to three months), in the range that indicates their diabetes was poorly controlled, compared to those without a diabetes diagnosis who on average demonstrate no diabetes or low diabetes risk. Those with a previous diabetes diagnosis also had higher cholesterol and triglycerides, but lower HDL and C-Reactive Protein compared to those who had never been diagnosed with diabetes, indicating a higher average risk of chronic comorbidities like cardiovascular disease, compared to their non-diabetic siblings (see Table 1) (see also Carruth et al., 2020).
At the time of their diagnosis, the patients with a diagnosis with type-2 diabetes reported insatiable thirst and frequent urination. However in addition to these expected symptoms, patients also reported dramatic and progressive weight loss (weydow), loss of appetite, progressively worsening bodily weakness (daal), slowed wound healing and recurrent infections in their extremities, and loss of teeth and tooth decay, that in all but two cases, did not improve with standard, recommended biomedical treatments of metformin and/or insulin. Three of the elderly patients >60 years old had previously lost toes, and continued to struggle to manage multiple chronic infections in their extremities. Compliance with therapeutic regimens did not result in control of average blood glucose levels and an amelioration of symptoms, comorbidities, and other related medical complications (Carruth and Mendenhall, 2019).
3.3. Humoral and digestive dysfunctions as comorbidities
In the medical literature, type 2 diabetes is described as partially hereditary and triggered by combinations of obesity, individual behaviors like poor diet and smoking tobacco, and increasingly, exposure to environmental toxins such as air pollution (Zimmet, 2017). Among Somalis in Ethiopia, by contrast, diabetes is typically defined as a humoral pathology, marked by disruptions or excesses of humoral flows (Carruth, 2020; Carruth and Mendenhall, 2019). Consequently, in discussions about their experience of type 2 diabetes, most people with diabetes mentioned comorbid humoral dysfunctions including indigestion, gastritis, heartburn, and most commonly, constipation (calool istaag). Additionally, the most common symptoms that motivated people to seek medical care were also described to us as humoral dysfunctions, including frequent urination and sudden weight loss. In other words, what was most concerning for these patients was the uncontrolled and continuous draining of their humoral flows (Carruth, 2020). The pathological losses of their urine and healthy fatness (subaq) were perceived as physical symptoms of deeper disease, depletion, and stress – including but not limited to diabetes and the anxiety chronic disease produces.
Humoral pathologies were also discussed not as individual problems related solely to behaviors or choices like sugar consumption, but as consequent of widespread food insecurity and the progressive sedentarization and displacement of pastoralist and semi-pastoralist livestock herders throughout the region. Diets low in fresh, locally-grown foods, but high in “oily” (saliid leh), “soft,” (jilicsan) or “sweet” (macaan) foods, seen as the products of these broader social and economic changes, were perceived to disrupt humoral flows and increase vulnerability to diseases including diabetes (Carruth and Mendenhall, 2019). A change from living out of doors, walking long distances to care for livestock and trade, and living on “fresh foods,” patients opined, caused community-wide increases in internal, humoral disruptions including type-2 diabetes.
In general, multiple simultaneous and interacting humoral pathologies including diabetes were managed by Somalis through compliance with recommended courses of medications, but in addition to this, through self-induced vomiting or gut evacuation (bixin), consuming camel milk, taking herbal remedies such as special teas or oils, feasting, fasting, or otherwise changing the diet (buulee), and halting consumption of khat leaves (a popular mild narcotic). The management of internal humoral dysfunctions including type-2 diabetes required regulating what was consumed and felt from the external environment.
3.4. Emergency as etiology
Self-reported feelings of anxiety and stress were also perceived by our respondents to trigger and manifest alongside diabetes (Carruth and Mendenhall, 2019). This echoes findings elsewhere: stress, trauma, clinical depression, and violence play a causal role in the diagnosis and experience of diabetes, as well as their own interpretations of diabetes etiologies in places around the world (Carruth and Mendenhall, 2018; Lee et al., 2014; Mendenhall, 2019; Smith-Morris, 2008; Solomon, 2016; Wiedman, 2012). Exposures to stressful life events and intense emotions were the most commonly reported proximate cause of diabetes among these crisis-affected Somalis. Many people described the onset of their symptoms as consequent of sudden and forced migrations, loss of livestock, local outbreaks of violence, anxiety about the actions of the police or military, anger (cadho) between persons within their household, and/or what people called “thinking too much” (fikir badan)--an idiom of distress documented elsewhere in East Africa and in Latin America (Kaiser et al., 2015).
Other persons we spoke with also suspected diet changes pursuant to recurrent complex humanitarian emergencies and dependence on limited food aid rations caused or contributed to their diabetes. Many explained that years ago, especially prior to crises in the mid-1980s, people would eat what they called in Somali traditional foods (cunto dhaqmeed) such as whole-grain sorghum with fresh or soured livestock milk, maize alone or made into a porridge, bone broths, and occasional goat, sheep, cattle, or camel meat. But today, most people's diets have dramatically changed. Most of the people we spoke with -- in rural and urban locations – consumed pasta or rice on a daily basis. Our respondents also reported daily consumption of candy, sodas, and heavily sweetened, spiced tea. In rural communities outside the cities of Jigjiga and Dire Dawa, persons additionally reported chronic food insecurity and a lack of fresh vegetables and fruits for months at a time (including during the long winter dry season, or jiilal, and during drought years).
The diabetes patients who had experienced recent temporary displacements due to political insecurity or attacks on their livestock or property also reported lacking some or all of the kinds of fresh ingredients their doctors recommended. Additionally, most of the people with diabetes we spoke to belonged to households that were chronically food insecure and as such, qualified for occasional or regular distributions of food aid -- most often bags of wheat grains, bags of corn-soy blended flour, lentils, split peas, and/or cans of vegetable oil. In times of crisis, when people sought refuge with family members or traveled frequently, it was difficult or impossible for them to manage a diet different from what their family members and hosts were already eating, or outside the limited rations offered by international aid organizations.
In sum, Somali diabetes patients in eastern Ethiopia, during this recent time of political upheaval and displacement, experienced a form of diabetes frequently concomitant with several other conditions including humoral dysfunctions, digestive problems, slow wound-healing, infections of the extremities, tooth decay, tooth loss, and anxiety and stress over their individual and collective circumstances. These diabetes patients also experienced chronic weight loss, loss of appetite, lethargy, weakness, high cholesterol, high triglycerides, and persistently high HbA1c even while taking prescribed medications and/or insulin. Furthermore, these patients described type-2 diabetes not as a chronic condition, but rather an acute and life-threatening disease.
In the four months preceding data collection, two individuals in their mid-30's and 40's in communities the field team knew well died of complications of diabetes. Then in the fourteen months following data collection, a total of four of the 85 diabetes patients we spoke to also passed away. Several of the patients and healthcare providers we spoke with for this research expressed to us their fear of untimely death and “wasting away” from diabetes. “It is like an epidemic among Somalis,” one aid worker in the city of Jigjiga said to us. The lack of preventive care, dietary support, insulin supplies, and refrigeration diabetes patients require are absolutely matters of life and death – especially during humanitarian emergencies. What local Somali healthcare providers and policymakers suggested to us were humanitarian interventions that better met the needs of both adults with chronic diseases like diabetes as well as children and their parents, and programs to address people's both chronic conditions as well as acute infections associated with crisis and displacement.
Humanitarian crisis-affected persons in eastern Ethiopia needed and desired dietary support including vegetables, fruits, and high-fiber grains like whole-grain teff and sorghum (and not standard foods supplied in ration distributions, like biscuits, wheat, and oil) beyond the food commodities provided in rations. Higher quality and greater variety of foods offered in humanitarian responses would surely improve the health outcomes for all food aid recipients, but for diabetes patients, access to these foods was absolutely necessary to maintain their digestive health, humoral flows, and ability to resist or recover from infections. Patients additionally needed better access to healthcare providers who could prescribe and monitor responses to medications and insulin, as well as access to local refrigeration to store insulin supplies. Patients needed dental care and wound-care specialists, and needed their local healthcare providers to also have training in the community-based management of common complications and chronic comorbidities in general. Humanitarian responses that narrowly target children and mothers, or offer only interventions for singular infectious diseases and undernutrition in children would fail to address many of the most pressing health needs in these communities.
4. Discussion
The most pressing health concerns that emerge during relief operations typically highlight not the general patterns of morbidity and mortality across different humanitarian emergencies, but rather, the longstanding healthcare needs of the particular communities facing a complex humanitarian emergency. The constellations of multi-morbidities that emerge are the products of particular local contexts and long histories of recurrent crises. Humanitarian crises can worsen individuals’ existing health problems and at the same time exacerbate existing collective health inequities, as well as thwart efforts to provide comprehensive and community-based primary healthcare. The most pressing health concerns that emerge during humanitarian responses may often reflect the longstanding needs of communities facing complex humanitarian emergencies. Our prior research in two different contexts suggests that outbreaks of political violence, for example, can increase risks of both acute and chronic diseases, as well as communicable and non-communicable conditions, making many chronic, non-communicable diseases matters of immediate concern. At the same time, political violence can also prevent the efficient recognition and effective and continuous management of both mental illness and other chronic noncommunicable diseases more difficult.
However, reconceptualizing complex humanitarian crises as sites of discernible syndemics may help reorient and broaden humanitarian interventions to focus on the exacerbation and interplay of these longstanding and multifaceted healthcare challenges in crisis-affected communities, rather than remaining focused on reactionary interventions to address single health domains or narrow demographic groups. Recognition of these contingent and cascading constellations of risks and outcomes demands intervention designs focused on integrated chronic disease, infectious disease, and mental health care -- in other words, expansive and sustainable primary health care -- even in the face of overwhelmed or disintegrated health systems. Consequently, efforts to improve health outcomes must address both the multi-morbidity that clusters in humanitarian crisis-affected populations and the roots of political violence. This kind of syndemic approach can elucidate the specific effects and patterns of negative health outcomes and violence within populations and help improve humanitarian interventions.
In Nepal, we found that rates of mental health problems varied substantially among female former child soldiers despite comparable burdens of trauma exposure. In some parts of the country, female former child soldiers had high rates of PTSD and depression co-morbidity, but in other communities there were lower rates of PTSD and depression. A syndemic theory that connects co-morbidities and the sociocultural context interacting with political violence is helpful to interpret these differences. One contributor to the differences appeared to be the sociocultural context that former child soldiers returned to after the war, with some communities having greater levels of gender-based discrimination, that likely preceded the war and also influenced how women were treated after the war. Girls in communities dominated by high-caste Hindu groups reported more experiences of discrimination compared to girls in mixed caste/ethnic communities (Kohrt et al., 2010b). A community-based intervention designed to increase social supports and social inclusion appeared to mitigate some of the burden of PTSD and depression.
In the case of providing better health care to Somalis in Ethiopia during a complex humanitarian emergency characterized by population displacement and political upheaval, it may be necessary for responses to attend to cases of acute malnutrition and the spread of infectious diseases, but also, to consider how complex humanitarian emergencies precipitate and exacerbate suffering from type-2 diabetes, chronic disease prevention and care in general, mental health concerns such as anxiety, chronic digestive and humoral dysfunctions, persistent infections and wounds, and even loss of teeth and dental caries consequent of these other outcomes. Diabetes as it manifests in this emergency-affected population involved unexpected symptoms including dramatic and persistent weight loss, loss of appetite, lethargy, and weakness despite patients’ compliance with recommended medications and/or insulin, which are more typical of later-stage diabetes rather than the ongoing chronic management seen in most high-income settings or stable, peacetime context in settings with functioning health systems. Patients lacked continuing health care, access to diets of fresh foods, and refrigeration for their insulin, and these challenges were made worse during the acute phase of the emergency. Our research therefore suggests that persons with pre-existing and/or undiagnosed chronic conditions may be at heightened risk of infectious diseases, malnutrition, or poor health outcomes. Persons may also struggle to access the medications, treatments, regular preventive healthcare, and technologies their health depends on.
4.1. Limitations
The main limitation of this study is that the case studies were not designed a priori to test syndemic models of causality. Intriguing patterns were identified in the findings in these complex humanitarian emergencies that raised the potential for considering them in light of syndemic relationships. To statistically demonstrate the exponentiation of health effects needed to identify the presence of a syndemic relationship, we would need samples powered for appropriate moderator effects on associations by context. Future studies should follow recommendations for analyses to empirically test for syndemics (Tsai and Venkataramani, 2016; Tsai, 2018). Therefore, the current findings should be taken as case studies to reflect upon how syndemics may present in complex humanitarian emergencies, but the findings are not definitive for specific syndemics given the retrospective analysis of studies designed with other analytic models in mind.
4.2. Agenda for applying syndemic theory in complex humanitarian emergencies
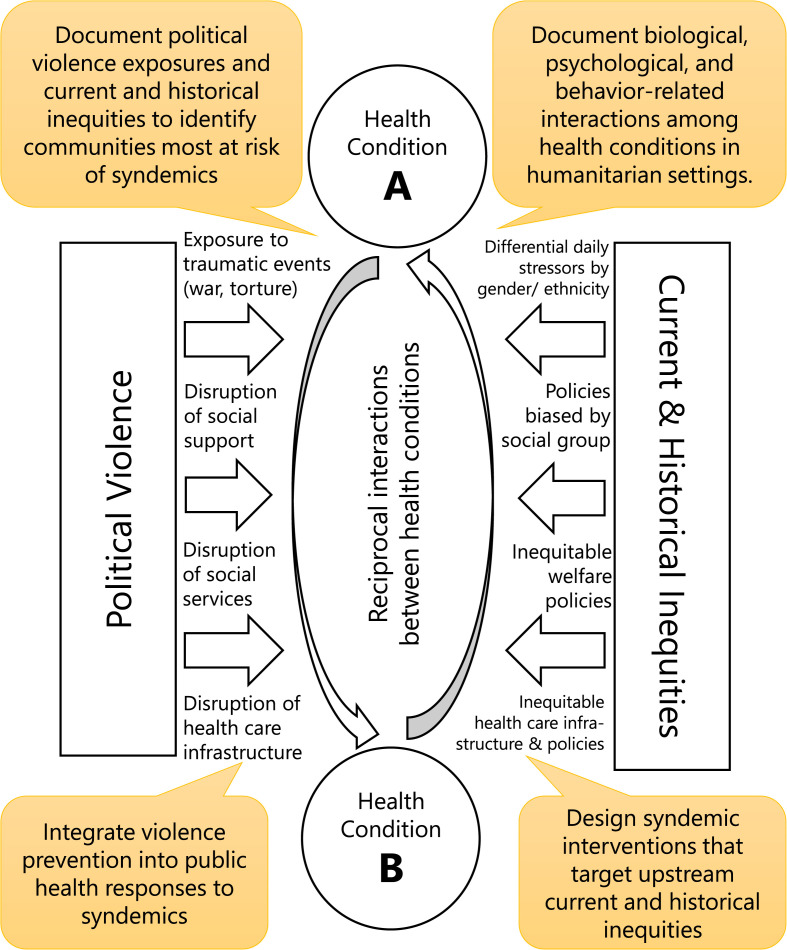
Given the nature of complex humanitarian emergencies and the effects of political violence on other health outcomes, our case studies support Willen et al.‘s model for intervening in syndemics when human rights are threatened: “(1) mapping the effect of social, political, and structural determinants on health; (2) identifying opportunities for upstream intervention; and (3) working collaboratively to tackle the structures, institutions, and processes that cause and exacerbate health inequities,” (Willen et al., 2017). Below, we apply these three tenets to syndemic health responses in complex humanitarian emergencies (see Fig. 4 ).
Fig. 4.
Model for responding to syndemics in humanitarian settings.
-
1.
In humanitarian emergencies, it is important to map not only the differential distribution of health problems, but also the regional and local differences in political, structural, and historical determinants of health, and the clustering of multi-morbidities. Whereas most humanitarian emergency responses are moving to digital based approaches such as Global Positioning System (GPS) tagging of regions with infectious disease outbreaks and, malnutrition cases, etc., it would be helpful to also have tracking that merges this information with mental health and other non-communicable disease epidemiology. In addition, human rights documentation of political violence, exposure to sexual and physical violence, and experiences of trauma and displacement could identify sites with particular vulnerability. Localized documentation of human rights violations is typically done in complex humanitarian emergencies, e.g., INSEC in Nepal during its civil war (INSEC, 2005) or Human Rights Watch reports in Ethiopia (Human Rights Watch, 2018), but mapping activities as part of these research initiatives are rarely overlaid on health data to reveal patterns of morbidity and mortality.
-
2.
Identify opportunities for upstream community-based and political interventions during and after humanitarian crises to mitigate the drivers of health differentials. If public health practitioners exclusively focus on health outcomes, the drivers of health disparities will remain in place. Therefore, interventions should mitigate local and regional contributors to these differences. This can be local initiatives such as the Nepal example, in which discrimination was tackled at the school and community level. This can and should also include further upstream efforts such as trying to mitigate the encampment of or stressful migrations of displaced persons crises and the origins of other humanitarian emergencies, but it may also include local upstream targets like, in the Somali Region of Ethiopia, ensuring safe elections, peaceful transfers of power, the provision of medical care to displaced persons, and community-based primary healthcare in underserved and politically insecure locations. Interventions can also address violence related to law enforcement and security personnel in humanitarian emergencies to improve health (Boazak et al., 2020; Kohrt et al., 2015; Weine et al., 2020). Representativeness of local leadership should be documented. In regions where the community control of post-emergency resources is dominated by one ethnic or religious group, or where women are not equally represented in humanitarian response activities, and when humanitarian responses fail to meet the needs of people on the move, these sociopolitical factors will likely contribute to poorer health outcomes even if basic medical supplies and services are distributed. The mapping of the relative representativeness of local and regional coordinating bodies can be used to intervene at the level of planning and coordinating committees. A successful intervention may not change the total amount of health resources needed but may change how they are allocated. Pre-humanitarian emergency local indicators related to factors such as voting rights and female literacy may also be good indicators of settings where the greatest comorbidities may arise (c.f., Kohrt et al., 2010a). If women and ethnic minority groups are represented in health, education, and livelihood planning post-emergency, this may lead to more inclusive and salutogenic response strategies.
-
3.
Collaborative approaches are needed to transform structures, institutions, and processes to respond at the level of social, political, and economic determinants with upstreamand political interventions. Only through these collaborations will it be possible to effectively address the first two recommendations above. In Nepal, the program would not have been successful without partnering with local groups advocating for rights of women, low-caste groups, and ethnic minorities. In Ethiopia, the de-escalation of the conflict in the Somali Region and the use of traditional methods of conflict resolution with Somali elders helped people return to their homes, re-establish connections with community-based health workers, and get control of their diets and medication regimens within a few months. Given that syndemic understandings cannot be developed without accounting for historical and current inequities and the nature of the political violence at hand, solutions cannot be achieved without working in partnership with the communities that constitute these institutions, structures, and social relations.
5. Conclusion
Humanitarian interventions risk being less effective when siloed by single medical conditions with a narrow focus on responding to acute infectious disease outbreaks and distributions of material goods like vaccines and food aid. There are increasing efforts through mechanism such as cluster systems to improve communication of health programs with sectors of protection, security, education, and economic livelihoods, as well as initiatives in political reforms and peace and reconciliation. However, from a health perspective there has been a dearth of theoretical frameworks to understand how these domains interact. Syndemic theory provides one way of conceptualizing these relationships and designing interventions to respond. When considering how to respond to chronic social injustice this also raises questions about the scope of neutrality. Maintaining neutrality in conflict settings and focusing narrowly on the efficient provision of basic life-saving goods and services has been an operational tactic for nongovernmental humanitarian organizations to maintain access to populations in need (IFRC, 2020; Slim, 2015). And yet, in practice, this principle also either ignores or stands in the way of relief operations’ necessary engagement with the political roots of complex emergencies, and their necessary partnerships with local aid groups, governmental agencies, politicians, and advocates (Ali and Murphy, 2020; Benton and Atshan, 2016; Kihato and Landau, 2017). One way forward to reducing the fragmentation of relief work, human rights work, and political action might be to embrace use of theoretical models that can address both multi-morbidity and the social, economic, and political structures that shape risk factors and health. Applying syndemic theory to humanitarian emergencies, in situations like we describe here, can therefore foster re-thinking and expanding the objectives, mechanisms, and focus of emergency responses.
Credit statement
The authors contributed equally to the conceptualization of the manuscript, data collection, analysis, and manuscript writing.
Funding
We would like to acknowledge funding from U.S. National Institutes of Health (F31MH075584), UNICEF Nepal, and an internal faculty grant from American University.
Acknowledgments
For the Nepal case study, the authors thank Transcultural Psychosocial Organization (TPO) Nepal and collaborators including Hari Krishna Adhikari, Joseph Adhikari, Manju Adhikari, Arti Jha, Rajesh Jha, Mark Jordans, Ramesh Karki, Rohit Karki, Deepti Khati, Suraj Koirala, Nabin Lamichhane, Sujen Maharjan, Em Perera, Bindu Prasai, Pragya Shrestha, Prami Sigdel, Reena Thapa, Wietse Tol, and Nawaraj Upadhaya.
References
- Adhikari RP, Kohrt BA, Luitel NP, Upadhaya N, Gurung D, Jordans MJD. Protective and risk factors of psychosocial wellbeing related to the reintegration of former child soldiers in Nepal. Journal of Mental Health and Psychosocial Support in Conflict Affected Areas. 2014;12(3):367–378. [Google Scholar]
- Albala-Bertrand J.-M. Responses to complex humanitarian emergencies and natural disasters: an analytical comparison. Third World Q. 2000;21:215–227. [Google Scholar]
- Alhalal E., Ford-Gilboe M., Wong C., AlBuhairan F. Factors mediating the impacts of child abuse and intimate partner violence on chronic pain: a cross-sectional study. BMC Wom. Health. 2018;18:160. doi: 10.1186/s12905-018-0642-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali Degan, Murphy Marie-Rose Romain. Black Lives Matter is also a reckoning for foreign aid and international NGOs. Open Democracy. 2020;(19 July) https://www.opendemocracy.net/en/transformation/black-lives-matter-also-reckoning-foreign-aid-and-international-ngos/ [Google Scholar]
- Benton A., Atshan S.e. Springer; 2016. “Even War Has Rules”: on Medical Neutrality and Legitimate Non-violence. [DOI] [PubMed] [Google Scholar]
- Boazak M, Yoss S, Kohrt BA, Gwaikolo W, Strode P, Compton MT, Cooper J. Law enforcement and mental health clinician partnerships in global mental health: outcomes for the Crisis Intervention Team (CIT) model adaptation in Liberia, West Africa. Global Mental Health. 2020;7 doi: 10.1017/gmh.2019.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burkle F.M. Complex humanitarian emergencies: a review of epidemiological and response models. J. Postgrad. Med. 2006;52:110. [PubMed] [Google Scholar]
- Carruth Lauren. Camel milk, amoxicillin, and a prayer: Medical pluralism and medical humanitarian aid in the Somali Region of Ethiopia. Social Science & Medicine. 2014;120:405–412. doi: 10.1016/j.socscimed.2019.03.026. [DOI] [PubMed] [Google Scholar]
- Carruth Lauren. Peace in the Clinic: Rethinking ‘“Global Health Diplomacy”’ in the Somali Region of Ethiopia. Culture, Medicine & Psychiatry. 2016;40:181–197. doi: 10.1007/s11013-015-9455-6. [DOI] [PubMed] [Google Scholar]
- Carruth Lauren. Kinship, nomadism, and humanitarian aid among Somalis in Ethiopia. Disasters. 2018;42(1):141–168. doi: 10.1111/disa.12236. [DOI] [PubMed] [Google Scholar]
- Carruth Lauren. Rethinking fatness, rethinking diabetes. American Anthropologist. 2020;122(3):643–645. doi: 10.1111/aman.13440. [DOI] [Google Scholar]
- Carruth Lauren, Jama Ateye Mohamed, Nassir Ahmed, Mussa Hosh Farah, Mendenhall Emily. Diabetes in a humanitarian crisis: Atypical clinical presentations and challenges to clinical- and community-based management among Somalis in Ethiopia. Global Public Health. 2020;15(6):828–839. doi: 10.1080/17441692.2020.1718735. [DOI] [PubMed] [Google Scholar]
- Carruth Lauren, Mendenhall Emily. Social aetiologies of type 2 diabetes. BMJ. 2018;361:k1795. doi: 10.1136/bmj.k1795. [DOI] [PubMed] [Google Scholar]
- Carruth Lauren, Mendenhall Emily. “Wasting away”: Diabetes, food insecurity, and medical insecurity in the Somali Region of Ethiopia. Social Science & Medicine. 2019;228:155–163. doi: 10.1016/j.socscimed.2019.03.026. [DOI] [PubMed] [Google Scholar]
- Charlson F., van Ommeren M., Flaxman A., Cornett J., Whiteford H., Saxena S. New WHO prevalence estimates of mental disorders in conflict settings: a systematic review and meta-analysis. Lancet. 2019;394:240–248. doi: 10.1016/S0140-6736(19)30934-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen L.C., Briggs S.M., Leaning J. Harvard University Press; 1999. Humanitarian Crises: the Medical and Public Health Response. [Google Scholar]
- Clapham C. The Ethiopian developmental state. Third World Q. 2018;39:1151–1165. [Google Scholar]
- Demographic and Health Survey Program . 2016. Ethiopia: Standard DHS 2016.https://dhsprogram.com/what-we-do/survey/survey-display-478.cfm [Google Scholar]
- Devermont J., Temin J. Africa's democratic moment: the five leaders who could transform the region. Foreign Aff. 2019;98:131. [Google Scholar]
- Edkins J. Legality with a vengeance: famines and humanitarian relief in'complex emergencies. Millennium. 1996;25:547–575. [Google Scholar]
- Farmer P. University of California Press; Berkeley: 2003. Pathologies of Power : Health, Human Rights, and the New War on the Poor. [Google Scholar]
- Galtung J. Violence, peace, and peace research. J. Peace Res. 1969;6:167–191. [Google Scholar]
- Galtung J. Cultural violence. J. Peace Res. 1990;27:291–305. [Google Scholar]
- Gravlee C.C. Systemic racism, chronic health inequities, and COVID-19: a syndemic in the making? Am. J. Hum. Biol. 2020 doi: 10.1002/ajhb.23482. n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammer C.C., Brainard J., Hunter P.R. Risk factors and risk factor cascades for communicable disease outbreaks in complex humanitarian emergencies: a qualitative systematic review. BMJ Global Health. 2018;3 doi: 10.1136/bmjgh-2017-000647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbert H.K., Hyder A.A., Butchart A., Norton R. Global health: injuries and violence. Infectious Disease Clinics. 2011;25:653–668. doi: 10.1016/j.idc.2011.06.004. [DOI] [PubMed] [Google Scholar]
- Human Rights Watch . 2018. We Are like the Dead": Torture and Other Human Rights Abuses in Jail, Ogaden, Somali Regional State, Ethiopia.https://www.hrw.org/report/2018/07/04/we-are-dead/torture-and-other-human-rights-abuses-jail-ogaden-somali-regional [Google Scholar]
- IFRC . International Committee of the Red Cross; Geneva: 2020. The Fundamental Principles of the International Red Cross and Red Crescent Movement, Ref. 4046. [Google Scholar]
- INSEC . Informal Sector Service Centre (INSEC); Kathmandu, Nepal: 2005. Nepal Human Rights Yearbook 2005; p. 366. [Google Scholar]
- Integrated Regional Information Network . 2017. Ethiopia Survives its Great Drought, but a Way of Life May Not.http://www.irinnews.org/feature/2016/06/13/ethiopia-survives-its-great-drought-way-life-may-not [Google Scholar]
- International Organization for Migration . 2019. Humanitarian Needs Overview.https://www.humanitarianresponse.info/sites/www.humanitarianresponse.info/files/2019/03/02_HNO_Summary_030619.pdf [Google Scholar]
- Jobanputra K., Boulle P., Roberts B., Perel P. Three steps to improve Management of Noncommunicable Diseases in humanitarian crises. PLoS Med. 2016;13 doi: 10.1371/journal.pmed.1002180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser B.N., Haroz E.E., Kohrt B.A., Bolton P.A., Bass J.K., Hinton D.E. “Thinking too much”: a systematic review of a common idiom of distress. Soc. Sci. Med. 2015;147:170–183. doi: 10.1016/j.socscimed.2015.10.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur G. Chronic pain in refugee torture survivors. J Glob Health. 2017;7 doi: 10.7189/jogh.07.020303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kihato C.W., Landau L.B. Stealth humanitarianism: negotiating politics, precarity and performance management in protecting the urban displaced. J. Refug. Stud. 2017;30:407–425. [Google Scholar]
- Kliewer W., Robins J.L., Borre A. Community violence exposure, sleep disruption, and insulin resistance in low-income urban adolescents. Int. J. Behav. Med. 2019;26:437–442. doi: 10.1007/s12529-019-09801-7. [DOI] [PubMed] [Google Scholar]
- Kohrt BA, Blasingame E, Compton MT, Dakana SF, Dossen B, Lang F, Strode P, Cooper J. Adapting the Crisis Intervention Team (CIT) Model of Police–Mental Health Collaboration in a Low-Income, Post-Conflict Country: Curriculum Development in Liberia, West Africa. American Journal of Public Health. 2015;105(3):e73–e80. doi: 10.2105/AJPH.2014.302394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Burkey M, Stuart EA, Koirala S. Alternative approaches for studying humanitarian interventions: propensity score methods to evaluate reintegration packages impact on depression, PTSD, and function impairment among child soldiers in Nepal. Global Mental Health. 2015;2 doi: 10.1017/gmh.2015.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Hruschka DJ, Worthman CM, Kunz RD, Baldwin JL, Upadhaya N, Acharya NR, Koirala S, Thapa SB, Tol WA, et al. Political violence and mental health in Nepal: prospective study. British Journal of Psychiatry. 2012;201(4):268–275. doi: 10.1192/bjp.bp.111.096222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Jordans MJD, Koirala S, Worthman CM. Designing mental health interventions informed by child development and human biology theory: A social ecology intervention for child soldiers in Nepal. Am J Human Biol. 2015;27(1):27–40. doi: 10.1002/ajhb.22651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt B.A., Jordans M.J., Tol W.A., Luitel N.P., Maharjan S.M., Upadhaya N. Validation of cross-cultural child mental health and psychosocial research instruments: adapting the Depression Self-Rating Scale and Child PTSD Symptom Scale in Nepal. BMC Psychiatry. 2011;11(1) doi: 10.1186/1471-244X-11-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Jordans MJ, Tol WA, Perera E, Karki R, Koirala S, Upadhaya N. Social ecology of child soldiers: child, family, and community determinants of mental health, psychosocial well-being, and reintegration in Nepal. Transcultural Psychiatry. 2010;47(5):727–753. doi: 10.1177/1363461510381290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt B.A., Jordans M.J.D., Tol W.A., Speckman R.A., Maharjan S.M., Worthman C.M., Komproe I.H. Comparison of mental health between former child soldiers and children never conscripted by armed groups in Nepal. JAMA. 2008;300(6):691–702. doi: 10.1001/jama.300.6.691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt B.A., Mistry A.S., Anand N., Beecroft B., Nuwayhid I. Health research in humanitarian crises: an urgent global imperative. BMJ Global Health. 2019;4(6) doi: 10.1136/bmjgh-2019-001870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Speckman RA, Kunz RD, Baldwin JL, Upadhaya N, Acharya NR, Sharma VD, Nepal MK, Worthman CM. Culture in Psychiatric Epidemiology: Using Ethnography and Multiple Mediator Models to Assess the Relationship of Caste with Depression and Anxiety in Nepal. Annals of Human Biology. 2009;36(3):261–280. doi: 10.1080/03014460902839194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kohrt BA, Tol WA, Pettigrew J, Karki R. In: The War Machine and Global Health. Singer M, Hodge GD, editors. Altamira Press: Rowan & Littlefield Publishers, Inc.; Lanham, Maryland: 2010. Children and Revolution: The Mental Health and Psychosocial Wellbeing of Child Soldiers in Nepal’s Maoist Army; pp. 89–116. [Google Scholar]
- Kohrt B.A., Worthman C.M., Adhikari R.P., Luitel N.P., Arevalo J.M.G., Ma J., McCreath H., Seeman T.E., Crimmins E.M., Cole S.W. Psychological resilience and the gene regulatory impact of posttraumatic stress in Nepali child soldiers. Proceedings of the National Academy of Sciences. 2016;113(29):8156–8161. doi: 10.1073/pnas.1601301113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konstam M.A., Konstam A.D. Gun violence and cardiovascular health. Circulation. 2019;139:2499–2501. doi: 10.1161/CIRCULATIONAHA.118.039504. [DOI] [PubMed] [Google Scholar]
- Krug E.G., Mercy J.A., Dahlberg L.L., Zwi A.B. The world report on violence and health. Lancet. 2002;360:1083–1088. doi: 10.1016/S0140-6736(02)11133-0. [DOI] [PubMed] [Google Scholar]
- Lee C., Tsenkova V., Carr D. Childhood trauma and metabolic syndrome in men and women. Soc. Sci. Med. 2014;105:122–130. doi: 10.1016/j.socscimed.2014.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindqvist D., Wolkowitz O.M., Mellon S., Yehuda R., Flory J.D., Henn-Haase C., et al. Proinflammatory milieu in combat-related PTSD is independent of depression and early life stress. Brain Behav. Immun. 2014;42:81–88. doi: 10.1016/j.bbi.2014.06.003. [DOI] [PubMed] [Google Scholar]
- Liu X., Logan J., Alhusen J. Cardiovascular risk and outcomes in women who have experienced intimate partner violence: an integrative review. J. Cardiovasc. Nurs. 2020;35(4):400–414. doi: 10.1097/JCN.0000000000000654. [DOI] [PubMed] [Google Scholar]
- Macrae J., Zwi A. 1994. Famine, Complex Emergencies and International Policy in Africa: an Overview. War and Hunger: Rethinking international Responses to Complex Emergencies; pp. 6–36. [Google Scholar]
- Maes K. Taylor & Francis; 2016. The Lives of Community Health Workers: Local Labor and Global Health in Urban Ethiopia. [Google Scholar]
- Mbanya J.C.N., Motala A.A., Sobngwi E., Assah F.K., Enoru S.T. Diabetes in sub-saharan africa. Lancet. 2010;375:2254–2266. doi: 10.1016/S0140-6736(10)60550-8. [DOI] [PubMed] [Google Scholar]
- Mendenhall E. Left Coast Press; 2012. Syndemic Suffering: Social Distress, Depression, and Diabetes Among Mexican Immigrant Women. [Google Scholar]
- Mendenhall E. Cornell University Press; 2019. Rethinking Diabetes: Entanglements with Trauma, Poverty, and HIV. [Google Scholar]
- Nesterko Y., Jäckle D., Friedrich M., Holzapfel L., Glaesmer H. Prevalence of post-traumatic stress disorder, depression and somatisation in recently arrived refugees in Germany: an epidemiological study. Epidemiol. Psychiatr. Sci. 2020;29:e40. doi: 10.1017/S2045796019000325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Østebø M.T., Cogburn M.D., Mandani A.S. The silencing of political context in health research in Ethiopia: why it should be a concern. Health Pol. Plann. 2018;33:258–270. doi: 10.1093/heapol/czx150. [DOI] [PubMed] [Google Scholar]
- Peconga E.k., Høgh Thøgersen M. Post-traumatic stress disorder, depression, and anxiety in adult Syrian refugees: what do we know? Scand. J. Publ. Health. 2019 doi: 10.1177/1403494819882137. [DOI] [PubMed] [Google Scholar]
- Poteat T., Millett G.A., Nelson L.E., Beyrer C. Understanding COVID-19 risks and vulnerabilities among black communities in America: the lethal force of syndemics. Ann. Epidemiol. 2020;47:1–3. doi: 10.1016/j.annepidem.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ReliefWeb . 2019. Ethiopia: Drought - 2015-2019. Glide: DR-2015-000109-ETH.https://reliefweb.int/disaster/dr-2015-000109-eth [Google Scholar]
- Rivara F., Adhia A., Lyons V., Massey A., Mills B., Morgan E., et al. The effects of violence on health. Health Aff. 2019;38:1622–1629. doi: 10.1377/hlthaff.2019.00480. [DOI] [PubMed] [Google Scholar]
- Salama P., Spiegel P., Talley L., Waldman R. Lessons learned from complex emergencies over past decade. Lancet. 2004;364:1801–1813. doi: 10.1016/S0140-6736(04)17405-9. [DOI] [PubMed] [Google Scholar]
- Singer M. A dose of drugs, a touch of violence, a case of AIDS: conceptualizing the SAVA syndemic. Free Inq. 1996;24:99–110. [Google Scholar]
- Slim H. Oxford University Press; 2015. Humanitarian Ethics: A Guide to the Morality of Aid in War and Disaster. [Google Scholar]
- Smith-Morris C. University of Arizona Press; 2008. Diabetes Among the Pima: Stories of Survival. [Google Scholar]
- Solomon H. Duke University Press; 2016. Metabolic Living: Food, Fat, and the Absorption of Illness in India. [DOI] [PubMed] [Google Scholar]
- Sphere . 2018. The Sphere Handbook 2018.https://spherestandards.org/handbook-2018/ [Google Scholar]
- Stander V.A., Thomsen C.J., Highfill-McRoy R.M. Etiology of depression comorbidity in combat-related PTSD: a review of the literature. Clin. Psychol. Rev. 2014;34:87–98. doi: 10.1016/j.cpr.2013.12.002. [DOI] [PubMed] [Google Scholar]
- Toole M.J., Waldman R.J. The public health aspects of complex emergencies and refugee situations. Annu. Rev. Publ. Health. 1997;18:283–312. doi: 10.1146/annurev.publhealth.18.1.283. [DOI] [PubMed] [Google Scholar]
- Trief P.M., Ouimette P., Wade M., Shanahan P., Weinstock R.S. Post-traumatic stress disorder and diabetes: Co-morbidity and outcomes in a male veterans sample. J. Behav. Med. 2006;29:411–418. doi: 10.1007/s10865-006-9067-2. [DOI] [PubMed] [Google Scholar]
- Tsai A.C., Venkataramani A.S. Syndemics and health disparities: a methodological note. AIDS Behav. 2016;20:423–430. doi: 10.1007/s10461-015-1260-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai A.C. Syndemics: a theory in search of data or data in search of a theory? Soc. Sci. Med. 2018;206:117–122. doi: 10.1016/j.socscimed.2018.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNICEF . 2018. Ethiopia Humanitarian Situation Report #12 to December 2018. UNICEF Ethiopia. Addis Ababa, Ethiopia.https://www.unicef.org/appeals/files/UNICEF_Ethiopia_Humanitarian_Situation_Report_Dec_2018.pdf [Google Scholar]
- UNICEF . 2019. Ethiopia Humanitarian Situation Report.https://www.unicef.org/ethiopia/reports/humanitarian-situation-report-september-2019 [Google Scholar]
- UNOCHA . 2018. Ethiopia: Oromia-Somali Conflict-Induced Displacement.https://reliefweb.int/sites/reliefweb.int/files/resources/ethiopia_-_oromia_somali_conflict_induced_displacement_june_2018c.pdf Situation Report No. 4. Ethiopia. Addis Ababa, Ethiopia. [Google Scholar]
- Vazquez G., Duval S., Jacobs D.R., Jr., Silventoinen K. Comparison of body mass index, waist circumference, and waist/hip ratio in predicting incident diabetes: a meta-analysis. Epidemiol. Rev. 2007;29:115–128. doi: 10.1093/epirev/mxm008. [DOI] [PubMed] [Google Scholar]
- Weine S, Kohrt BA, Collins PY, Cooper J, Lewis-Fernandez R, Okpaku S, Wainberg ML. Justice for George Floyd and a reckoning for global mental health. Global Mental Health. 2020;7 doi: 10.1017/gmh.2020.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenzel T., Kienzler H., Wollmann A. Facing violence - a global challenge. Psychiatr. Clin. 2015;38:529–542. doi: 10.1016/j.psc.2015.05.008. [DOI] [PubMed] [Google Scholar]
- Wiedman D. Native American embodiment of the chronicities of modernity: reservation food, diabetes, and the metabolic syndrome among the Kiowa, Comanche, and Apache. Med. Anthropol. Q. 2012;26:595–612. doi: 10.1111/maq.12009. [DOI] [PubMed] [Google Scholar]
- Willen S.S., Knipper M., Abadía-Barrero C.E., Davidovitch N. Syndemic vulnerability and the right to health. Lancet. 2017;389:964–977. doi: 10.1016/S0140-6736(17)30261-1. [DOI] [PubMed] [Google Scholar]
- Willman A., Team V. World Bank; Washington, DC: 2009. Valuing the Impacts of Domestic Violence: A Review by Sector. The Costs of Violence; pp. 57–96. [Google Scholar]
- World Health Organization . 2008. Waist Circumference and Waist-Hip Ratio Report of a WHO Expert Consultation.http://apps.who.int/iris/bitstream/handle/10665/44583/9789241501491_eng.pdf;jsessionid=361573DDBF84B40B572F2B5F0A0FA1FC?sequence=1 [Google Scholar]
- Yodanis C.L., Godenzi A., Stanko E.A. The benefits of studying costs: a review and agenda for studies on the economic costs of violence against women. Pol. Stud. 2000;21:263–276. [Google Scholar]
- Zimmet P.Z. Diabetes and its drivers: the largest epidemic in human history? Clinical diabetes and endocrinology. 2017;3:1. doi: 10.1186/s40842-016-0039-3. [DOI] [PMC free article] [PubMed] [Google Scholar]