Abstract
Background
Electronic cigarettes (e-cigarettes) have been characterised as significantly less harmful than cigarettes by many health agencies and regulators globally. In this study, we examined to what extent perceived relative harms of e-cigarettes compared to cigarettes have changed in the USA.
Methods
We analysed the data from the longitudinal and nationally representative, Population Assessment of Tobacco and Health Study to assess the relative perceived harm of e-cigarettes amongst US adults between 2013 and 2016.
Results
The proportion of US adults who correctly perceived e-cigarettes as less harmful than cigarettes decreased each year from 41.1% (CI 40.1–42.1%) in 2013–2014, 31.5% (CI 30.8–32.2%) in 2014–2015 and 25.3% (CI 24.6–26.0%) in 2015–2016. Concurrently, the proportion of US adults who perceived e-cigarettes as equally, or more, harmful than cigarettes increased from 53.7% (CI 52.3–55.1%), 64.9% (CI 63.6–66.2%) to 72.7% (CI 71.5–73.9%) respectively. The proportion of US adults who held negative relative harm perceptions of e-cigarettes increased regardless of current smoking or vaping status by 24.6% and 29.6% respectively within 3 years. In Wave 3, the proportion of current smokers who perceived the relative harm of e-cigarettes as less harmful was lower at 29.3% (CI 28.2–30.4%) compared to current e-cigarette users at 43.5% (CI 40.3–46.7%). Former smokers who used e-cigarettes and believed that they were equally, or more, harmful than cigarettes in 2014–2015 had significantly higher rates of smoking relapse in the following year, 29% and 37% (p < 2.2e−16), respectively, compared to those with positive relative harm perceptions who reported relapse rates of 19%.
Conclusions
In this study, the proportion of US adults who incorrectly perceived e-cigarettes as equal to, or more, harmful than cigarettes increased steadily regardless of smoking or vaping status. Current adult smokers appear to be poorly informed about the relative risks of e-cigarettes yet have potentially the most to gain from transitioning to these products. The findings of this study emphasise the urgent need to accurately communicate the reduced relative risk of e-cigarettes compared to continued cigarette smoking and clearly differentiate absolute and relative harms. Further research is required to elucidate why the relative harm of e-cigarettes is misunderstood and continues to deteriorate.
Keywords: E-cigarettes, Relative harm perception, Harm reduction, Public health, Tobacco, Cigarette
Introduction
There are currently over 1 billion smokers in the world [1]. Over the last 50 years, public health authorities have worked to ensure that the harms associated with smoking are well understood. Despite these efforts, the World Health Organisation estimates that the number of smokers will increase to 1.1 billion by 2025 [2]. Whilst combustible cigarettes continue to remain the most commonly used nicotine product globally, the use of electronic cigarettes(s) (EC) is increasing worldwide by adult smokers who are seeking less harmful alternatives to combustible tobacco. There is scientific agreement that the most detrimental effects of smoking are due to the formation of toxicants from tobacco combustion and inhalation of tobacco smoke, and not by nicotine. According to the FDA, a key aspect of the organisation’s comprehensive plan for tobacco and nicotine regulation involves demonstrating a greater awareness that nicotine is delivered through products that represent a continuum of risk, and that delivery is most harmful when delivered through smoke particles in cigarettes [3]. The emergence, awareness and use of EC, which do not contain, nor combust, tobacco leaf has led to a transformation in the way adult smokers consume nicotine. This has subsequently triggered significant debate on the role of nicotine within society, beyond tobacco combustion, when decoupled from tobacco smoke.
As epidemiological data is limited, due to the relatively short time EC have been commercially available, the potential long-term health effects of EC are not yet fully understood. However, there is a growing global body of evidence which indicates EC are likely to be significantly less harmful compared to smoking tobacco [4–6]. This view has been reaffirmed by several public health authorities including Public Health England, The American Cancer Society and the US National Academies of Science, Engineering and Medicine [4–8]. In addition, several organisations have endorsed the use of EC as a smoking cessation aid [5, 7–9] and recognise the role that EC can play in tobacco harm reduction strategies.
Recently, the Centers for Disease Control and Prevention (CDC) estimated that the prevalence of current EC use amongst US adults is between 2.8 and 3.5% [10, 11], the majority of whom are reported to be either “current” or “former” smokers, who use EC “every day” or “some days” [11–13]. The rise in EC use has been associated with the first statistically significant increase in smoking cessation rates among US adult smokers at the population level, after 15 years of cessation rate stagnation [14, 15]. The prevalence of current cigarette smoking amongst the US adult population has declined from 24.7% in 1997 to 14.4% in 2017 [16, 17] and whilst cigarettes are still the most commonly used nicotine product in the US, smoking prevalence is at the lowest levels recorded since the National Health Interview Survey started collecting data in 1965 [10].
To reduce the health burden at a population level, harm reduction policies focus on well-established public health concepts which concentrate on modifying, rather than, eliminating behaviours. The principle of tobacco harm reduction recognises that many adults continue to smoke, despite the implementation of strong tobacco controls and awareness of the associated health risks. It is possible for EC to have a positive and legitimate role to play in public health, particularly among those adults who are uninterested or unwilling to quit smoking, or in those who do not find traditional nicotine replacement therapies (NRT) effective, especially as EC are widely accepted by adult smokers and are a viable alternative to smoking [5, 18]. Adult smokers commonly report using EC to reduce or replace their smoking [19–21] and EC use is associated with a reduction in cigarette consumption [22, 23]. Researchers have reported that whilst some adult smokers who use EC may occasionally have a smoking lapse, EC use does not lead to a full relapse back to cigarettes, suggesting that EC can prevent long-term relapse [24]. Recent clinical research indicates that EC are almost twice as effective at helping adult smokers quit cigarettes compared to medically licensed NRT [25]. Notably, recent data from the UK smoking toolkit reports that EC surpassed over-the-counter NRT in 2013 as the most common product used in quit attempts and has remained the most popular to date [26]. This is especially noteworthy considering that in many countries NRT products are available only with a prescription.
Despite the fact that one of the most commonly cited reasons that adult smokers choose to use EC is to reduce risk to their health [19–21], a growing body of research suggests that US adults lack awareness about the potential relative reduced harm of EC, and increasingly hold beliefs that these products are either as harmful as cigarettes, or more concerningly, that they are worse than smoking [27–32]. Previous research has demonstrated that safety and health concerns are a prominent reason given by adult smokers for either not trying EC [32] or stopping EC use, and returning to smoking cigarettes [33]. In addition, recent work by Brose and colleagues report that perceived relative harm of EC predicted subsequent use in current and former smokers [28]. Therefore, adult smokers who are poorly informed, or hold inaccurate beliefs or misconceptions about the relative harm of EC may be deterred from trying these products, potentially resulting in sustained smoking or relapse to smoking following a quit attempt. An accurate perception of the relative harm of EC is therefore critical in motivating adult smokers to try, and remain, using these products over exclusive lifelong cigarette use. The potential contribution that EC can have on public health at the population level can only be realised if the adult smoking population is clear on the relative risk of EC compared to smoking. However, little is known about how the overall perception of EC risk is evolving over time in US adults. To quantify this, we conducted an analysis of the first three waves of longitudinal data from the US Population Assessment of Tobacco and Health (PATH) study.
Method
Data source and sample
The Population Assessment for Tobacco and Health (PATH) study is a nationally representative longitudinal cohort study conducted by the National Institute on Drug Abuse and the FDA’s Center for Tobacco Products. The first wave (September 2013) contains baseline information for the study population and continuing follow-up data becomes available as the consortium collects subsequent waves of data. The PATH study uses audio computer-assisted self-interviews available in English and Spanish to collect information on tobacco use patterns and associated health behaviors. Address-based area probability sampling with an in-person household screening procedure was used to recruit participants. PATH study data collection involves a rigorous, multi-level sampling and a weighting scheme to ensure that data are representative nationwide and adjusted for oversampling and nonresponse. Weighted estimates produced by the PATH study are representative of the non-institutionalised, US civilian population [34]. We used data from the first three waves of the PATH study (2013 to 2016) which were publicly available at the time of this publication. Wave 1 (September 2013–December 2014), Wave 2 (October 2014–October 2015) and Wave 3 (October 2015–2016) adult interviews were analysed in this study.
To assess the trend in perceived relative harm among US adults, we selected individuals who participated as adults at the first wave and who attended the next two waves. Individuals who were unaware about EC at Wave 1 were excluded in this study. In total, this study focused on 21,693 US adults.
Measure of perceived relative harm
Perceived harm of EC relative to cigarettes was assessed in each wave of the PATH study by a single question (AE1099) which differed between Waves 1 and 2 and Wave 3. During Waves 1 and 2 question, AE1099 focused on EC specifically, "Is using e-cigarettes less harmful, about the same, or more harmful than smoking cigarettes?". During Wave 3, the question AE1099 expanded to “Is using e-cigarettes or other electronic nicotine products less harmful, about the same, or more harmful than smoking cigarettes?”. Five relevant response categories were constructed based on respondents answer to AE1099; “1, less harmful”, “2, about the same”, “3, more harmful”, “− 8, do not know”, “− 7, refused”. Respondents who had missing or incomplete responses for this key measure were dropped from the analysis. Respondents were further categorised into two response categories: individuals who answered, “less harmful” and those who answered “same or more harmful” in response to question AE1099.
Smoking and vaping status
The smoking and vaping status for 21,693 US adults was assigned according to the definitions given in the PATH study [34] as either “current smokers” or “current vapers”, “former smokers” or “former vapers” or “never smokers” or “never vapers”. For clarity, adult smokers or vapers who were considered as “current experimental” and “current established” were regrouped as “current smokers” or “current vaper” and “former experimental” and “former established” were regrouped as “former smokers” and “former vapers” respectively.
Future trends in relative harm perception amongst US adult smokers
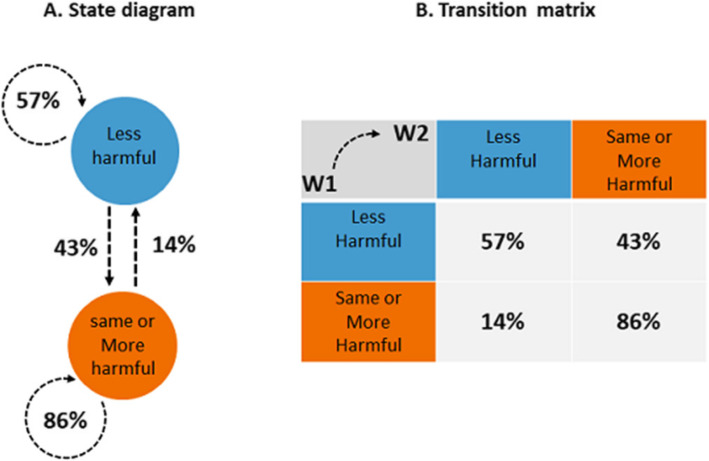
To estimate future trends in relative harm perception amongst US adult smokers, we created a model based on the changes in relative harm perception observed amongst the smoking population between Wave 1 and Wave 2. A matrix of transitions and the corresponding state diagram using a directed graph to picture the state transitions was built. Figure 1 represents the state diagram and the transition matrix. The states represent whether adult smokers believe EC are “less harmful than conventional cigarette” or if EC “is about same or more harmful than conventional cigarette”. These two states have been renamed respectively “less harmful” and “same or more harmful”.
Fig. 1.
State diagram and the associated transition matrix from Wave 1 to Wave 2. a Harm perception state diagram. b The associated transition matrix from Wave 1 to Wave 2
A discrete time Markov chain [35] was applied to model the transition probabilities between discrete states and to forecast the prevalence of US smokers who would perceive EC the “same or more harmful than conventional cigarette” if effective intervention is not implemented to correct misconceptions within the adult smoking population.
Statistical analysis
First, we presented descriptive statistics of the study demographic and analysed cigarette and EC status. The proportions of responses about perceived harm relative to cigarettes were analysed across all three waves. The trends in perceived harm from Wave 1 to Wave 3 for all selected adults were plotted with 95% confidence intervals (CI) for the response category proportions for relative perceived harm. Finally, the impact of smoking and vaping status on relative harm perception trends were investigated. All analyses were conducted using R version 3.5.1 R Core Team. We used chi-square statistical analysis to assess changes in perceived relative harm to investigate whether negative relative harm perceptions amongst former smokers and current vapers at Wave 2 was associated with a return to smoking at Wave 3. The level of statistical significance was set at p < 0.05.
Results
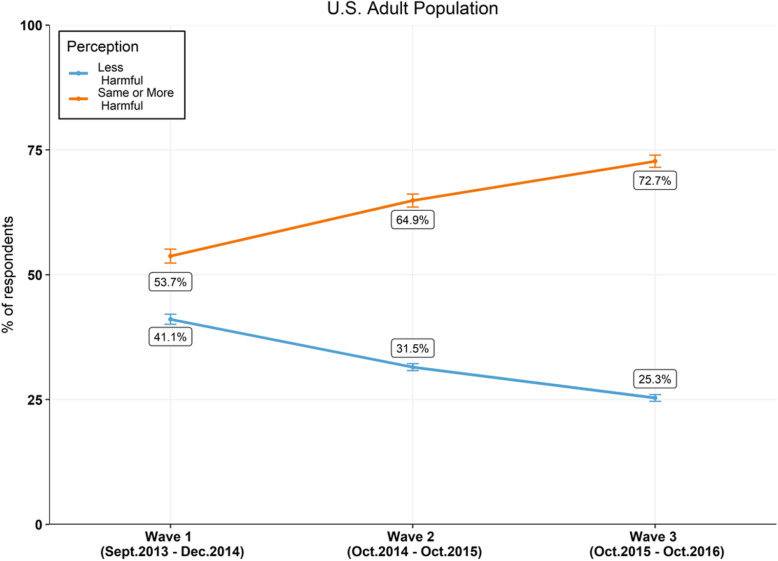
The proportion of US adults who perceived EC as less harmful than combustible cigarettes has consistently declined each year from 41.1% (CI 40.1–42.1%) in Wave 1 (W1), 31.5% (CI 30.8–32.2%) in Wave 2 (W2) and 25.3% (CI 24.6–26.0%) Wave 3 (W3) (Table 1). Concurrently, during the same time frame, the proportion of the US adult population believing that EC were as harmful or more harmful than smoking combustible cigarettes increased from 53.7% (CI 52.3–55.1%), to 64.9% (CI 63.6–66.2%) to 72.7% (CI 71.5–73.9%) between Waves 1, 2 and 3 respectively (Fig. 2).
Table 1.
Weighted prevalence for gender, ethnicity, age and perceived relative harm for across all three waves
| Characteristics | Modalities | Wave 1 | Wave 2 | Wave 3 |
|---|---|---|---|---|
| Sex | 1 = Male | 47.9% | 48.7% | 49.1% |
| Sex | 2 = Female | 52.1% | 51.3% | 50.9% |
| Race/ethnicity | 1 = Non-Hispanic White | 68.3% | 68.2% | 68.3% |
| Race/Ethnicity | 2 = Non-Hispanic Black | 10.9% | 10.7% | 10.6% |
| 3 = Non-Hispanic other | 6.5% | 6.7% | 6.8% | |
| Race/Ethnicity | 4 = Hispanic | 11.1% | 11.1% | 11.1 % |
| Category of age | 1 = 18 to 24 years old | 13.5% | 11.8% | 9.9% |
| Category of Age | 2 = 25 to 34 years old | 17.9% | 18.5% | 18.7% |
| Category of Age | 3 = 35 to 44 years old | 17% | 17% | 16.9% |
| Category of Age | 4 = 45 to 54 years old | 18.8% | 17.9% | 17.9% |
| Category of Age | 5 = 55 to 64 years old | 17.4% | 18.1% | 18.3% |
| Category of Age | 6 = 65 to 74 years old | 10.7% | 11.5% | 12.3% |
| Category of Age | 7 = 75 years old or older | 4.7% | 5.3% | 6% |
| Relative harm perception | − 8 = Do not know | 5% | 3.4% | 1.8% |
| Risk Perception | − 7 = Refused | 0.2% | 0.2% | 0.1% |
| Risk Perception | 1 = Less harmful | 41.1% | 31.5% | 25.3% |
| Risk Perception | 2 = About the same | 47.2% | 55.3% | 62.9% |
| Risk Perception | 3 = More harmful | 6.5% | 9.6% | 9.8% |
Race/ethnicity was categorized as white non-Hispanic, black non-Hispanic, non-Hispanic other (i.e. American Indian/Alaskan Natives, Native Hawaiian, Pacific Islander, Multi-racial) and Hispanic of any race. Gender categories included male and female. Ages were categorized into the following groups: 18–24, 25–34, 35–44, 45–54, 55–64, 65–74 and 75 and older. Categories as defined by the PATH study
Fig. 2.
US adult population perceived harm of EC relative to cigarettes between 2013 and 2016. Percentages are weighted. Error bars indicate 95% CI
When smoking and vaping status across all three waves was analysed (Table 2), current non-smoker non-vaper (including former or never users) was the most prevalent status in each wave, 76.0% (W1), 69.5% (W2) and 62.4% (W3), followed by never users of either products 28.5%, 27.8% and 26.8% at Waves 1, 2 and 3, respectively. In contrast, dual use of both cigarettes and EC remained low, reducing across the waves from 4.9%, 4.4% to 3.3% at Waves 1, 2 and 3, respectively. Overall, US adult never users of cigarettes who currently use EC (NVR; CUR) was nominally reported in 0.1–0.2% of the population between Waves 1 and 3.
Table 2.
Weighted prevalence of smoking and vaping status for all three waves
| Cigarette; EC | Wave 1 | Wave 2 | Wave 3 |
|---|---|---|---|
| ___ ; ___ | 0.0% | 0.1% | 0.7% |
| ___; CUR | 0.0% | 0.0% | 0.1% |
| ___;FMR | 0.0% | 0.2% | 0.4% |
| ___;NVR | 0.4% | 4.4% | 10.2% |
| CUR;___ | 0.0% | 2.7% | 3.7% |
| CUR;CUR | 4.9% | 4.4% | 3.3% |
| CUR;FMR | 8.6% | 8.2% | 8.6% |
| CUR;NVR | 8.7% | 6.5% | 5.5% |
| FMR;___ | 0.0% | 1.8% | 2.6% |
| FMR;CUR | 1.2% | 1.6% | 1.7% |
| FMR;FMR | 4.5% | 5% | 5.3% |
| FMR;NVR | 42.5% | 36.2% | 29.5% |
| NVR;___ | 0% | 0.3% | 0.6% |
| NVR;CUR | 0.1% | 0.1% | 0.2% |
| NVR;FMR | 0.5% | 0.5% | 0.8% |
| NVR;NVR | 28.5% | 27.8% | 26.8% |
A small proportion of respondents have at least one undefined status for vaping and/or smoking. CUR corresponds to current smoker or vapers, including “current experimental” (defined as Wave 3 adult respondents who have not smoked at least 100 cigarettes in their lifetime, and currently smoke every day or some days or have ever used an EC, have never used fairly regularly, and uses every day or some days) and “current established” (defined as Wave 3 adult respondents who have smoked at least 100 cigarettes in their lifetime, and currently smoke every day or some days or have ever used an EC, have used fairly regularly, and uses every day or some days). NVR corresponds to never smoker or vapers (defined as never smoked a cigarette, even one or two puffs or never used an EC, even once or twice) FMR corresponds to former smoker or vapers including “former experimental” (defined as ever smoked a cigarette, has not smoked more than 100 cigarettes in lifetime, and now does not smoke at all or have ever used an EC, have never used fairly regularly, and does not use at all) and “former established” (defined as ever smoked a cigarette, has smoked more than 100 cigarettes in lifetime, and now does not smoke at all or have ever used an EC, has used fairly regularly, and currently does not use at all). ___ means that the status has not been defined
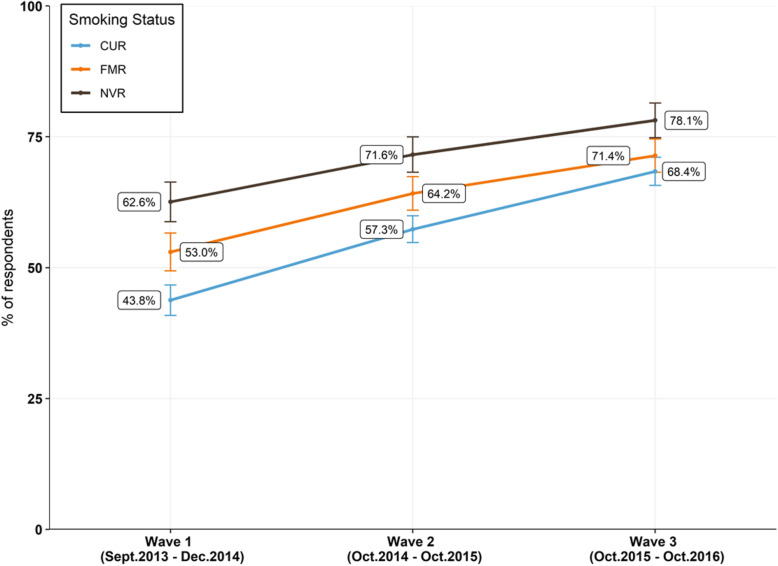
Regardless of smoking status, the proportion of adult smokers who believed EC were equally or more harmful than cigarettes increased substantially between 2013 and 2016 (Fig. 3). Among current adult smokers, the percentage of those that held an incorrect relative harm perception increased across all waves by a total of 24.6% percentage points in 3 years, from 43.8% (CI 40.9–46.7%) in W1 to 68.4% (CI 65.7–71.1%) in W3.
Fig. 3.
US adults who perceived EC as equally or more harmful than cigarettes and smoking status. US adults who perceived EC as about the same, or more harmful, than cigarettes across all three waves, stratified by smoking status. “CUR” corresponds to current smoker or vapers, “FMR” corresponds to former smoker or vapers and “NVR” corresponds to never smoker or vapers. Percentages are weighted. Error bars indicate 95% CI
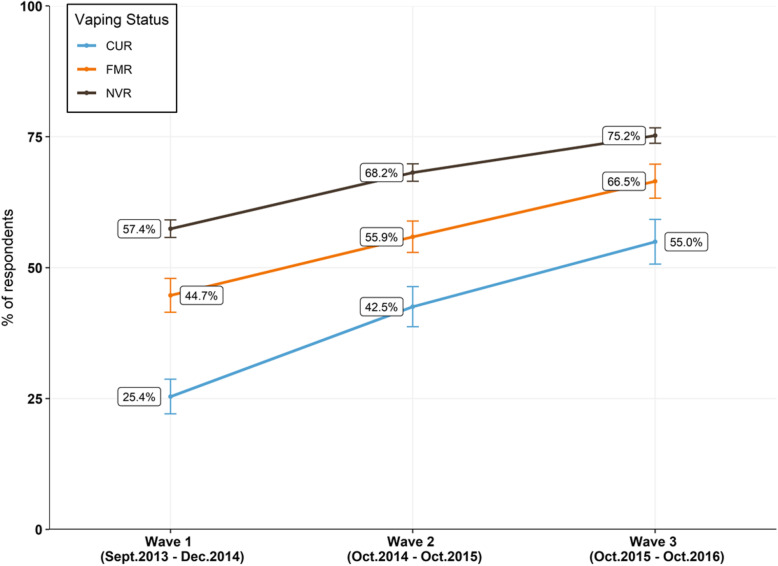
To further understand the relationship between perceived relative harm and product use, perceived harm and vaping status was investigated. Similar to what was observed with smokers, regardless of vaping status, the proportion of US adults who perceived the relative harm of EC equally to, or more harmful than, smoking increased substantially across all three waves (Fig. 4). The percentage of current adult EC users who perceived the relative harm of EC equal to, or more harmful than, cigarettes increased by 29.6% over time, from 25.4% (CI 22.1–28.7%) in W1 to 55.0% (CI 50.7–59.2%) in W3. Compared to smoking status, a wider distribution in relative harm perception was observed when data was stratified by vaping status. Overall, a higher proportion of current adult EC users perceived EC as less harmful than cigarettes (43.5%, CI 40.3–46.7%) compared to current smokers (29.3%, CI 28.2–30.4%), never vapers (22.7%, CI 21.9–23.5%) or never smokers (20.8%, CI 19.4–22.2%) in W3.
Fig. 4.
US adults who perceived EC as equally or more harmful than cigarettes and vaping status. US adults who perceived EC as equal to, or more, harmful than cigarettes across all three waves, stratified by vaping status. “CUR” corresponds to current smoker or vapers, “FMR” corresponds to former smoker or vapers and “NVR” corresponds to never smoker or vapers. Percentages are weighted. Error bars indicate 95% CI
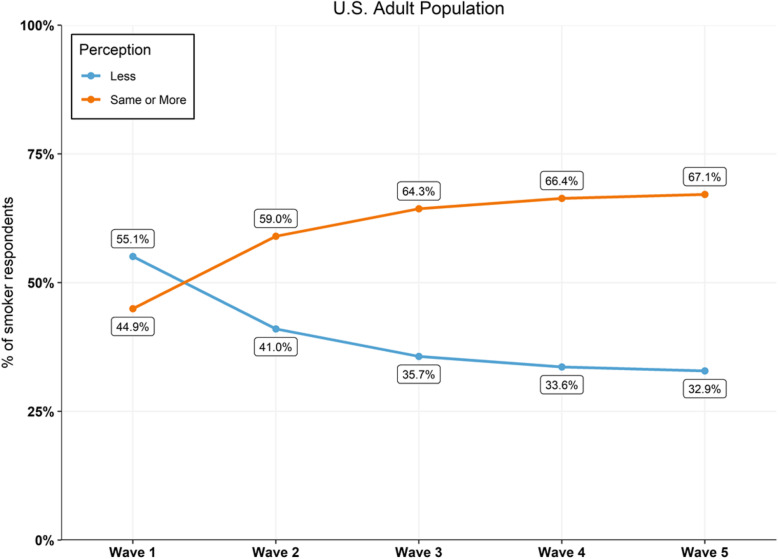
To estimate future trends in relative harm perception amongst US adult smokers, a model was constructed and validated by retrospectively comparing estimated percentages against published PATH data. For Wave 3, the model estimated that 64.3% of US adult smokers would report EC as being equal to, or more harmful, than cigarettes (Fig. 5), a difference of 4.1% percentage points compared to the PATH data (68.4%). When the analysis was expanded to project future relative perceptions if the current trend continues, the model estimated that the percentage of US adult smokers who would incorrectly perceive the relative harm of EC would increase to 67.1% by Wave 5. As the model appears to underestimate the trend in inaccurate perceptions among US adult smokers, it is likely to expect that by Wave 5 the percentage of adult smokers who report incorrect relative harm perceptions of EC would exceed 70% if the trend continues.
Fig. 5.
Prediction model estimates for relative harm perceptions amongst US adult smokers
Next, we focused on former smokers who used EC in Wave 2 and estimated the weighted proportions of individuals who reported smoking relapse according their relative harm perception in Wave 3. Former smokers who reported using EC at Wave 2 had significantly higher rates of smoking relapse at Wave 3 if they perceived EC as being equal to, or more harmful, relative to cigarettes. Table 3, (29% and 37%, respectively, p < 2.2e−16) compared to those who perceived EC as relatively less harmful, where relapse was reported at 19%.
Table 3.
Smoking relapse between Waves 2 and 3 according to relative harm perception in former smokers
| Relative harm perception | Still former smoker | Relapse smoking | % relapse |
|---|---|---|---|
| 1 = less harmful | 2004002 | 462707 | 19 |
| 2 = about the same | 696429 | 282810 | 29 |
| 3 = more harmful | 81604 | 47060 | 37 |
Discussion
Our findings confirm that despite many health organisations and regulators adopting a strategy which encourages adult smokers to transition to EC if they are uninterested or unwilling to quit smoking, there is widespread confusion and misconception about the actual relative harm of EC among US adults. Four principle findings emerged from this study. First, analysing data from a nationally representative longitudinal study demonstrates that the proportion of US adults who perceive EC as less harmful than cigarettes decreased substantially between 2013 and 2016. Second, during the same time period, the proportion of US adults who perceived EC to be equally or more harmful than cigarettes increased substantially. Third, compared to ‘never’, ‘former’ or ‘current’ smokers, a lower proportion of current EC users perceived EC equally or more harmful than cigarettes. However, even amongst current users the proportion who perceived the relative harm of EC equal to or more harmful than cigarettes increased between 2013 and 2016. Fourth, former smokers who used EC were more likely to report smoking relapse if they held negative relative harm perceptions compared to those who correctly perceived the relative harm of EC.
Our finding that most US adults perceive the relative harm of EC as equally or more harmful than cigarettes is consistent with findings from several previous studies across multiple countries [27–32, 36]. Our findings do, however, differ from a recent literature review [37] which concluded that the majority of study respondents perceived the relative harm of EC as less harmful than cigarettes. Importantly, this publication reviewed literature up until 2014, and whilst the increase in popularity of EC with adult smokers became noticeable in 2010, a greater increase in use was not observed until 2014. In addition, our findings show that current adult smokers are less likely than current EC users to perceive EC as less harmful than combustible cigarettes. Our study supports others who have reported that relative harm perception of EC compared to cigarettes has deteriorated in more recent years [27, 29, 38], particularly among adult smokers who may benefit most by transitioning to EC rather than continued smoking [39]. Furthermore, our model suggests that inaccurate misperceptions amongst adult smokers will continue to deteriorate unless effective intervention is implemented.
The growing misperception of the relative harm of EC among the adult smoking population may in fact be deterring adult smokers from even trying or continuing the use of these products. Negative beliefs and the further upward trend of perceiving EC as equally or more harmful than cigarettes in Wave 3 warrants heightened consideration and should be investigated further. This is especially critical considering that one of the most commonly cited reasons why adult smokers report using EC is to reduce the impact on their health and to either reduce or replace their smoking [19–21]. Our findings that negative beliefs of EC relative harm was associated with smoking relapse support others who report that positive perceptions of the relative harm of EC is associated with subsequent use in smokers and ex-smokers [19, 28, 40] and is a strong predictor of exclusive use among adult smokers who completely transition from cigarettes [41].
How the relative harm of these products is communicated to the public, and adult smokers more specifically, is critical and requires unique consideration. Studies have found that potential health warnings may inadvertently deter smokers from initiating EC use and that messages conveying reduced harm may be more effective [42, 43].
In addition, it has been reported that statements which do not differentiate relative risks are misinterpreted by consumers to mean that EC are just as harmful as cigarettes [44]. Therefore, effective public communication which accurately interprets the scientific data and clearly differentiates the absolute from the relative risk of EC will increase consumers’ knowledge of the risk differential. Correctly understanding the relative harms of EC could potentially create the health incentive required for those adult smokers who wish to transition for health reasons. Information based on comparative harm is commonplace for many harm reduction strategies; however, tobacco use appears to be exempt from this approach in many countries [45]. Whilst there has been some concern that providing adult smokers with less harmful nicotine-containing products may obstruct smoking cessation, the use of snus in Sweden, a less harmful alternative to cigarettes [46], appears to have facilitated record low smoking prevalence and the lowest levels of tobacco-related mortality amongst men in Europe [47]. The example of snus in Sweden strongly suggests that reduced harm products can positively impact the smoking population. Some researchers have voiced criticism that the dominant public health messages continue to focus on the absolute risk of using any tobacco product rather than the relative risk between categories of products that have the potential to reduce risk and cigarettes [45]. For example, it has been reported that major US health information websites have either stated that smokeless tobacco carried the same risks as cigarettes [48] or made modest efforts to inform consumers on the significantly lower risk of these types of products compared to continued lifelong cigarette use [45]. Health agencies and regulators globally should aim to provide adult smokers with clear, objective and evidence-based health information on the differential risks between using cigarettes and other products. Such information is necessary for individuals to be able to exercise personal autonomy and make informed decisions on which product to use to either reduce or replace their cigarette consumption. Accurate communication of the risk differentials should not be underestimated considering that consumers primarily trust information on the health risks and benefits of EC from prominent public health agencies over other sources [49, 50]. Consequently, information provided by regulators, health agencies and independent scientists about harm reduction may be directly influencing the populations harm perception of EC.
Misconceptions of the relative harm of EC may also be being driven by misunderstandings of the harm of nicotine use and the wider impact of negative media coverage [39]. Inaccurate knowledge of nicotine, and the misattribution of the portion of risk in smoking to nicotine, may have indirectly contributed to the misperceptions surrounding EC [51]. Furthermore, media coverage which reports that EC and e-liquids are linked to toxicant exposure [52], health-related problems [53, 54] or serious injury [55, 56] are frequent. In addition, the absence of a strong distinction between absolute and relative risk may be contributing to a communication bias where media reports are overstating the absolute harm and not contextualising relative risk against continued smoking. That said, it is important that the public are fully informed that ECs are not risk-free, are a harm reduction tool for adult smokers who would otherwise continue to smoke combustible cigarettes and should never be used by non-smokers or vulnerable populations. Moreover, there is a need to fully understand the potential absolute harms of ECs. As evidenced by the recent outbreaks of e-cigarette, or vaping, product use-associated lung injury (EVALI) in the USA, associated with the addition of the thickening agent vitamin E acetate to illicit tetrahydrocannabinol (THC)-containing vaping devices, ECs must only be used as intended by the manufacturer and not adulterated, tampered with or modified with other substances, which may introduce novel EC harms.
Our study has a number of limitations and the data should be viewed in the context of these. In particular, the PATH study was not originally designed to assess relative harm perception in the US adult population, and the current study design only provides a single item for such assessments which may somewhat limit the reliability of the findings. Furthermore, the single question used to assess perceived relative harm differed in Wave 3 from Waves 1 and 2. It is important to note that the expansion of the question during Wave 3 encompasses other electronic nicotine delivery products which could be interpreted as including other products such as heated tobacco, electronic pipe and water pipe devices. This variation in wording may influence comparability across data waves. In addition, the generic question in the PATH survey to assess relative harm may not have captured various aspects of harm on the perceived health risks associated with use. Assessing relative perceived harm of EC associated with specific health endpoints (e.g. heart or lung disease) may result in different harm perceptions compared to overall harm perceptions in general. It is important to also note that due to the design of the PATH study and the availability of the associated public use files, only data from Wave 1 (September 2013–December 2014), Wave 2 (October 2014–October 2015), Wave 3 (October 2015–October 2016) was available for analysis. Given the significant time lag in data availability, an analysis of more recent EC perceptions was not possible. Future work will include an analysis of the public use files for Wave 4 (December 2016–January 2018) when released to determine if EC perceptions have improved or deteriorated further. Furthermore, given the timings and public availability of the PATH data, it was not possible to analysis any potential association between the recent outbreak of EVALI in the USA and EC perceptions, which may have resulted in an even greater change. The outbreak of EVALI, which received extended news coverage worldwide, was associated with the inhalation of the thickening agent vitamin E acetate added to illicit tetrahydrocannabinol (THC)-containing vaping devices; however, news reports often failed to distinguish these important facts from regular nicotine-containing ECs. Consequently, post-EVALI, this may have increased confusion about the relative harms of nicotine-containing ECs, and vaping as an alternative to smoking more generally, which will not be apparent until future waves of the PATH study have been published and data analysed. Those limitations notwithstanding, the findings from this study are consistent with others who have found that the relative harm perception of EC compared to cigarettes is continuing to deteriorate over time.
Conclusion
The lack of accurate and consistent messaging from both public health agencies and the media may be contributing to public, and more specifically adult smokers’, perceptions about the relative risk of nicotine when decoupled from combustion and tobacco smoke. Until the advent of new nicotine products such as EC, nicotine and tobacco had frequently been seen as indistinguishable in terms of harm. Our findings show that overtime, perceptions of the relative harmfulness of ECs has continued to deteriorate and diverge from the scientific evidence. This highlights an urgency to communicate the relative risks of nicotine and EC use to the public, especially to adult smokers who are unwilling or uninterested in quitting smoking and have not even tried EC, but who would gain the most in terms of a potential health benefit if they did. Whilst deterring non-smokers is a critical objective of EC health messaging, this goal needs to be carefully balanced so that messaging is compelling enough to prevent any unintended consequences of reducing the appeal or minimising the health incentive of EC to those adult smokers who may be considering and motivated to transition. Confusion may potentially be discouraging adult smokers from using alternative, less hazardous products which may ultimately result in a missed opportunity to positively impact health at both an individual and population level. For the harm reduction potential of EC to be fully realised, the relative risks of using these products, compared to cigarettes, must be evidence based and clearly communicated to the public from several trusted sources. Ensuring that the risk differential is unambiguously understood and accepted as accurate by those who currently use combustible tobacco will be critical. Misconceptions need to be urgently addressed with a need for corrective communications by public health bodies to address the confusions created by previously unclear and contradictory EC messaging. Future research and policy-makers should aim to elucidate why the relative harm of EC compared to smoking is widely misunderstood and continues to deteriorate.
Acknowledgements
We would like to thank Dr. Nveed Chaudhary (Imperial Brands Plc) for the constructive feedback and discussions.
Abbreviations
- EC
Electronic cigarette
- PATH
Population Assessment of Tobacco and Health
- NRT
Nicotine replacement therapy
Authors’ contributions
XC, TV and MG conducted the data analysis and created the model. LM interpreted the data and created the manuscript. TW, GO and SW were involved in critically reviewing the manuscript for important intellectual content. All authors read and approved the final manuscript.
Funding
The paper was funded by Imperial Brands Plc.
Availability of data and materials
The dataset(s) supporting the conclusions of this article are available in the Population Assessment of Tobacco and Health (PATH) study [USA] Public-Use Files (ICPSR 36498) repository, https://www.icpsr.umich.edu/icpsrweb/NAHDAP/studies/36498.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
All authors are employees of Imperial Brands Plc.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Layla Malt, Email: Layla.Malt@uk.imptob.com.
Thomas Verron, Email: Thomas.Verron@fr.imptob.com.
Xavier Cahours, Email: Xavier.Cahours@fr.imptob.com.
Mengran Guo, Email: Mengran.Guo@fr.imptob.com.
Sarah Weaver, Email: Sarah.Weaver@uk.imptob.com.
Tanvir Walele, Email: Tanvir.Walele@uk.imptob.com.
Grant O’Connell, Email: Grant.Oconnell@uk.imptob.com.
References
- 1.WHO Global report on trends in prevalence of tobacco smoking 2000–2025 . Second edition. Geneva: World Health ORganisation; 2018. [Google Scholar]
- 2.Bilano V, Gilmour S, Moffiet T, d'Espaignet ET, Stevens GA, Commar A, et al. Global trends and projections for tobacco use, 1990-2025: an analysis of smoking indicators from the WHO Comprehensive Information Systems for Tobacco Control. 2015. [published correction appears in Lancet. 2015 Jun 13;385(9985):2354]. Lancet. 2015;385(9972):966-976. doi:10.1016/S0140-6736(15)60264-1. [DOI] [PubMed]
- 3.Food and Drug Administration. Advancing Medicinal Nicotine Replacement Therapies as New Drugs – A new step in FDA’s comprehensive approach to tobacco and nicotine. 2017 [Available from: https://www.fda.gov/NewsEvents/Newsroom/FDAVoices/ucm612005.htm. Access date: 25 August 2020.
- 4.McNeill A, Brose LS, Calder R, Bauld L, Robson D. Evidence review of e-cigarettes and heated tobacco products: Public Health England; 2018.
- 5.Royal College of Physicians . Nicotine without smoke: Tobacco harm reduction. London: RCP; 2016. [Google Scholar]
- 6.National Academies of Sciences, Engineering, and Medicine . Public Health Consequences of E-Cigarettes. Washington, DC: The National Academies Press; 2018. [PubMed] [Google Scholar]
- 7.McNeill AD, Brose LS, Calder RI, Hitchman SCB, Hajek P, McRobbie H. E-cigarettes: an evidence update: A report commissioned by Public Health England. 2015. [Google Scholar]
- 8.American Cancer Society. Position Statement on Electronic Cigarettes. 2018 [Available from: https://www.cancer.org/healthy/stay-away-from-tobacco/e-cigarette-position-statement.html. Access date: 25 August 2020.
- 9.NICE. Stop smoking interventions and services: National Institute of Clinical Health and Care Excellence; 2018 [Available from: https://www.nice.org.uk/guidance/ng92/chapter/rationale-and-impact. Access date: 25 August 2020.
- 10.Wang TW, Asman K, Gentzke AS, et al. Tobacco Product Use Among Adults — United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67:1225–1232. doi: 10.15585/mmwr.mm6744a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.QuickStats: Cigarette Smoking Status Among Current Adult E-cigarette Users, by Age Group — National Health Interview Survey, United States, 2015. MMWR Morb Mortal Wkly Rep 2016;65:1177. DOI: 10.15585/mmwr.mm6542a7. [DOI] [PubMed]
- 12.Glasser AM, Collins L, Pearson JL, et al. Overview of Electronic Nicotine Delivery Systems: A Systematic Review. Am J Prev Med. 2017;52(2):e33–e66. doi: 10.1016/j.amepre.2016.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amato MS, Boyle RG, Levy D. How to define e-cigarette prevalence? Finding clues in the use frequency distribution. Tob Control. 2016;25(e1):e24–e29. doi: 10.1136/tobaccocontrol-2015-052236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhu SH, Lee M, Zhuang YL, Gamst A, Wolfson T. Interventions to increase smoking cessation at the population level: how much progress has been made in the last two decades? Tob Control. 2012;21(2):110–118. doi: 10.1136/tobaccocontrol-2011-050371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhu SH, Zhuang YL, Wong S, Cummins SE, Tedeschi GJ. E-cigarette use and associated changes in population smoking cessation: evidence from US current population surveys. BMJ. 2017;358:j3262. doi: 10.1136/bmj.j3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.CDC. Early Release of Selected Estimates based on Data from the Nation Health Interview Survey, January-June 2017. Department of Health and Human Services, Centers for Disease Control and Prevention. National Center for Health statistics.2017 [Available from: https://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201712_08.pdf. Access date: 25 August 2020.
- 17.CDC. Cigarette Smoking Among Adults -- United States, 1997 1999 [Available from: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm4843a3.htm#tab1. Access date: 25 August 2020.
- 18.Steinberg MB, Zimmermann MH, Delnevo CD, et al. E-cigarette versus nicotine inhaler: comparing the perceptions and experiences of inhaled nicotine devices. J Gen Intern Med. 2014;29(11):1444–1450. doi: 10.1007/s11606-014-2889-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Adkison SE, O'Connor RJ, Bansal-Travers M, et al. Electronic nicotine delivery systems: international tobacco control four-country survey. Am J Prev Med. 2013;44(3):207–215. doi: 10.1016/j.amepre.2012.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rutten LJ, Blake KD, Agunwamba AA, et al. Use of E-Cigarettes Among Current Smokers: Associations Among Reasons for Use, Quit Intentions, and Current Tobacco Use. Nicotine Tob Res. 2015;17(10):1228–1234. doi: 10.1093/ntr/ntv003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhu S-H, Gamst A, Lee M, Cummins S, Yin L, Zoref L. The Use and Perception of Electronic Cigarettes and Snus among the U.S. Population. PLoS One. 2013;8(10):e79332. doi: 10.1371/journal.pone.0079332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McKeganey N, Miler JA, Haseen F. The Value of Providing Smokers with Free E-Cigarettes: Smoking Reduction and Cessation Associated with the Three-Month Provision to Smokers of a Refillable Tank-Style E-Cigarette. Int J Environ Res Public Health. 2018;15(9):1914. Published 2018 Sep 3. doi:10.3390/ijerph15091914. [DOI] [PMC free article] [PubMed]
- 23.Gomajee R, El-Khoury F, Goldberg M, et al. Association Between Electronic Cigarette Use and Smoking Reduction in France [published online ahead of print, 2019 Jul 15] JAMA Intern Med. 2019;179(9):1193–1200. doi: 10.1001/jamainternmed.2019.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Notley C, Ward E, Dawkins L, Holland R, Jakes S. Vaping as an alternative to smoking relapse following brief lapse. Drug Alcohol Rev. 2019;38(1):68–75. doi: 10.1111/dar.12876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hajek P, Phillips-Waller A, Przulj D, et al. A Randomized Trial of E-Cigarettes versus Nicotine-Replacement Therapy. N Engl J Med. 2019;380(7):629–637. doi: 10.1056/NEJMoa1808779. [DOI] [PubMed] [Google Scholar]
- 26.West R, Beard E, Brown J. Trends in electronic cigarette use in England. University College London: Smoking in England; 2019 [Available from: www.smokinginengland.info/latest-statistics/. Access date: 25 August 2020.
- 27.Huang J, Feng B, Weaver SR, Pechacek TF, Slovic P, Eriksen MP. Changing Perceptions of Harm of e-Cigarette vs Cigarette Use Among Adults in 2 US National Surveys From 2012 to 2017. JAMA Netw Open. 2019;2(3):e191047. Published 2019 Mar 1. doi:10.1001/jamanetworkopen.2019.1047. [DOI] [PMC free article] [PubMed]
- 28.Brose LS, Brown J, Hitchman SC, McNeill A. Perceived relative harm of electronic cigarettes over time and impact on subsequent use. A survey with 1-year and 2-year follow-ups. Drug Alcohol Depend. 2015;157:106–111. doi: 10.1016/j.drugalcdep.2015.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Majeed BA, Weaver SR, Gregory KR, et al. Changing Perceptions of Harm of E-Cigarettes Among U.S. Adults, 2012-2015. Am J Prev Med. 2017;52(3):331–338. doi: 10.1016/j.amepre.2016.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kiviniemi MT, Kozlowski LT. Deficiencies in public understanding about tobacco harm reduction: results from a United States national survey. Harm Reduct J. 2015;12:21. doi: 10.1186/s12954-015-0055-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tan AS, Bigman CA. E-cigarette awareness and perceived harmfulness: prevalence and associations with smoking-cessation outcomes [published correction appears in Am J Prev Med. 2016 May;50(5):674-6] Am J Prev Med. 2014;47(2):141–149. doi: 10.1016/j.amepre.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Action on Smoking and Health. ASH Fact Sheet: Use of ElectronicCigarettes (Vapourisers) Among Adults in Great Britain 2015 [Available from: http://ash.org.uk/information-and-resources/fact-sheets/use-of-e-cigarettes-among-adults-in-great-britain-2018/. Access date: 25 August 2020.
- 33.Biener L, Hargraves JL. A longitudinal study of electronic cigarette use among a population-based sample of adult smokers: association with smoking cessation and motivation to quit. Nicotine Tob Res. 2015;17(2):127–133. doi: 10.1093/ntr/ntu200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.United States Department of Health and Human Services. National Institutes of Health. National Institute on Drug Abuse, and United States Department of Health and Human Services. Food and Drug Administration. Center for Tobacco Products. Population Assessment of Tobacco and Health (PATH) Study [United States] Public-Use Files. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor], 2018-09-28. https://doi.org/10.3886/ICPSR36498.v8.
- 35.Matthes K. Resnick, Sydney I.: Adventures in Stochastic Processes. Birkhäuser Verlag AG, Basel-Boston-Berlin 1992, xii, 626 S., sFr. 128,—; DM 138,—. Biometrical Journal. 1995;37(3):272-.
- 36.Farsalinos KE, Siakas G, Poulas K, Voudris V, Merakou K, Barbouni A. Electronic cigarette use in Greece: an analysis of a representative population sample in Attica prefecture. Harm Reduct J. 2018;15(1):20. Published 2018 Apr 13. doi:10.1186/s12954-018-0229-7. [DOI] [PMC free article] [PubMed]
- 37.Czoli CD, Fong GT, Mays D, Hammond D. How do consumers perceive differences in risk across nicotine products? A review of relative risk perceptions across smokeless tobacco, e-cigarettes, nicotine replacement therapy and combustible cigarettes. Tob Control. 2017;26(e1):e49–e58. doi: 10.1136/tobaccocontrol-2016-053060. [DOI] [PubMed] [Google Scholar]
- 38.NINTS. Health Information National Trends Survey: National Cancer Institute; [Available from: https://hints.cancer.gov/view-questions-topics/question-details.aspx?nq=1&qid=1282. Access date: 25 August 2020.
- 39.McNeill A, Brose LS, Calder R, Bauld L, Robson D. Evidence review of e-cigarettes and heated tobacco products 2018.: Public Health England. 2018. [Google Scholar]
- 40.Atzendorf J, Aschenbrenner AB, Gomes de Matos E, et al. E-Zigaretten: Einschätzung von Gesundheitsgefahren und Nutzung zur Tabakentwöhnung [E-cigarettes: Perceived harmfulness and use for smoking cessation] Bundesgesundheitsbl Gesundheitsforsch Gesundheitsschutz. 2018;61(11):1415–1421. doi: 10.1007/s00103-018-2822-z. [DOI] [PubMed] [Google Scholar]
- 41.Farsalinos KE, Romagna G, Voudris V. Factors associated with dual use of tobacco and electronic cigarettes: A case control study. Int J Drug Policy. 2015;26(6):595–600. doi: 10.1016/j.drugpo.2015.01.006. [DOI] [PubMed] [Google Scholar]
- 42.Kimber C, Frings D, Cox S, Albery I, Dawkins L. The effects of the European e-cigarette health warnings and comparative health messages on non-smokers' and smokers' risk perceptions and behavioural intentions. BMC Public Health. 2018;18(1):1259. Published 2018 Nov 14. doi:10.1186/s12889-018-6161-7. [DOI] [PMC free article] [PubMed]
- 43.Cox S, Frings D, Ahmed R, Dawkins L. Messages matter: The Tobacco Products Directive nicotine addiction health warning versus an alternative relative risk message on smokers' willingness to use and purchase an electronic cigarette. Addict Behav Rep. 2018;8:136-139. Published 2018 Sep 21. doi:10.1016/j.abrep.2018.09.006. [DOI] [PMC free article] [PubMed]
- 44.Wackowski OA, Hammond D, O'Connor RJ, Strasser AA, Delnevo CD. Smokers' and E-Cigarette Users' Perceptions about E-Cigarette Warning Statements. Int J Environ Res Public Health. 2016;13(7):655. Published 2016 Jun 30. doi:10.3390/ijerph13070655. [DOI] [PMC free article] [PubMed]
- 45.Kozlowski LT, Sweanor D. Withholding differential risk information on legal consumer nicotine/tobacco products: The public health ethics of health information quarantines. Int J Drug Policy. 2016;32:17–23. doi: 10.1016/j.drugpo.2016.03.014. [DOI] [PubMed] [Google Scholar]
- 46.Nutt DJ, Phillips LD, Balfour D, et al. Estimating the harms of nicotine-containing products using the MCDA approach. Eur Addict Res. 2014;20(5):218–225. doi: 10.1159/000360220. [DOI] [PubMed] [Google Scholar]
- 47.Ramström L, Borland R, Wikmans T. Patterns of Smoking and Snus Use in Sweden: Implications for Public Health. Int J Environ Res Public Health. 2016;13(11):1110. Published 2016 Nov 9. doi:10.3390/ijerph13111110. [DOI] [PMC free article] [PubMed]
- 48.Kozlowski LT, O'Connor RJ. Apply federal research rules on deception to misleading health information: an example on smokeless tobacco and cigarettes. Public Health Rep. 2003;118(3):187–192. doi: 10.1093/phr/118.3.187.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Owusu D, Weaver SR, Yang B, Ashley DL, Popova L. Trends in Trust in the Sources of Health Information on E-Cigarettes Among US Adults, 2015-2017. Am J Public Health. 2019;109(1):145–147. doi: 10.2105/AJPH.2018.304754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Weaver SR, Jazwa A, Popova L, Slovic P, Rothenberg RB, Eriksen MP. Worldviews and trust of sources for health information on electronic nicotine delivery systems: Effects on risk perceptions and use. SSM Popul Health. 2017;3:787-794. Published 2017 Sep 29. doi:10.1016/j.ssmph.2017.09.003. [DOI] [PMC free article] [PubMed]
- 51.Wilson S, Partos T, McNeill A, Brose LS. Harm perceptions of e-cigarettes and other nicotine products in a UK sample. Addiction. 2019;114(5):879–888. doi: 10.1111/add.14502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Bitter Taste Vapers ‘at risk of irreversible POPCORN LUNG’ if they puff on flavoured e-cigarettes.: The Sun; 2018. Available from: https://www.thesun.co.uk/news/7784504/vapers-popcorn-lung-ecigarettes/. Access date: 25 August 2020.
- 53.E-cigarettes impair immune responses more than tobacco. Medical News Today; 2016. Available from: https://www.medicalnewstoday.com/articles/306444.php. Access date: 25 August 2020.
- 54.Vaping could be worse for your health than actual cigarette smoking research claims.: Mirror; 2018. Available from: https://www.mirror.co.uk/news/uk-news/vaping-could-worse-your-health-13406157. Access date: 25 August 2020.
- 55.Man seriously injured by e-cigarette explosion: CBS News; 2015. Available from: https://www.cbsnews.com/news/man-seriously-injured-by-e-cigarette-explosion/. Access date: 25 August 2020.
- 56.A man dies after his e-cigarette explodes in his face: CNN Health; 2019. Available from: https://edition.cnn.com/2019/02/05/health/exploding-vape-pen-death-trnd/index.html. Access date: 25 August 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset(s) supporting the conclusions of this article are available in the Population Assessment of Tobacco and Health (PATH) study [USA] Public-Use Files (ICPSR 36498) repository, https://www.icpsr.umich.edu/icpsrweb/NAHDAP/studies/36498.