Abstract
Tuberculosis of the cervical spine differs from other vertebral localizations by its extreme rarity, the clinical images are very diversified, the radiological measurements allow a good diagnostic orientation and specifically the MRI which allows a multi-planar study of the various lesions. Only bacteriological evidence can confirm the diagnosis. The treatment is based on a 12-month antituberculosis multidrug therapy and much debate upon the surgical indication. In our case, the patient presented with bilateral cervicobrachialgia with pain on examination at the mobilization of the cervical spine. A standard X-ray, a cervical CT scan, and a cervical MRI were performed, showing a C4 vertebral body compression of a probably infectious origin. The biopsy confirmed the diagnosis of a Cervical Pott's Disease that had been treated with anterior arthrodesis and TB treatment with rehabilitation, the patients' neurological symptoms improved, and he was doing well.
Keywords: Arthrodesis, tuberculosis, spinal tuberculosis, spinal arthrodesis
Introduction
The most common extra-pulmonary skeletal form of tuberculosis is within the spine, with a predilection for the thoracic and lumbar regions [1]. Tuberculosis of the cervical spine is distinguished from other vertebral localizations by its extreme rarity, representing approximately 2-3% of spinal TB cases [1-3]. Therefore, its clinical and radiological semiology is quite distinctive, as the cervical spine can be affected by lesions that lead to instability and neurological deficits, and its prognosis is conditioned by the risk of bulbo-medullary compression. The conduct of the cervical spine TB can involve a variety of interventions, ranging from TB treatment to surgery, although chemotherapy is the mainstay of the treatment [2].
Patient and observation
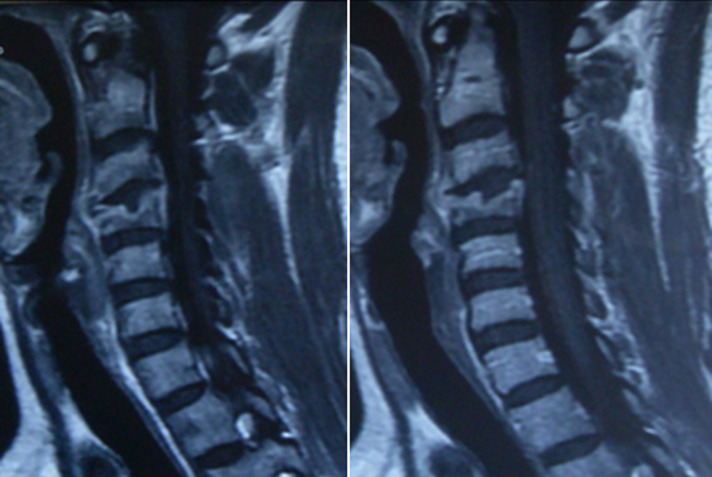
Patient K.R., 42 years old, without any particular pathological antecedents, who has had bilateral cervicobrachialgia for the past 9 months without any sensorimotor deficit, evolving in an unquantified weight loss context. On clinical examination, there was noticeable pain on the mobilization of the cervical spine. Standard radiography showed osteolysis with compression of the body of C4 (Figure 1). Magnetic resonance imaging confirmed the CT scan data and revealed a compression of the C4 vertebral body with epiduritis, or spinal epidural abscess and infiltration of the paravertebral soft tissues, suggesting primarily an infectious origin (Figure 2). The biopsy confirmed the diagnosis of active tuberculosis. The patient was treated with an anterior arthrodesis (Figure 3) and quadruple tuberculosis chemotherapy for 12 months. Post-rehabilitation showed improvement in patients' neurological symptoms, and his wellbeing with no signs of tuberculosis recurrence.
Figure 1.

standard radiography showed osteolysis with compression of the vertebral body of C4
Figure 2.
magnetic resonance imaging revealed a compression of the C4 body with epiduritis, or spinal epidural abscess, and infiltration of the paravertebral soft tissues, suggesting primarily an infectious origin
Figure 3.
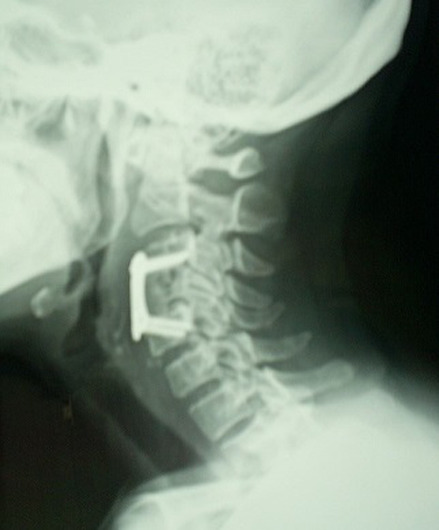
anterior arthrodesis
Discussion
The tuberculosis localization in the cervical spine is very rare [3]. The clinical pictures are varied and can range from isolated neuralgia cervicobrachial to tetraplegia [4]. Weight loss, night fever, cervical lymphadenopathies and retropharyngeal abscesses should be brought to the attention of the clinician [4,5]. Radiological data is propitious for diagnosis, but CT and MRI scans allow a better definition of bone and soft tissue abnormalities. for a precise multi-planar study MRI is more accurate than a CT scan [3,6,7], it achieves a better tissue differentiation, allows a demonstration of the marrow in relation to the envelopes, the study of the spinal disc, and the tissue surrounding of the spine. It can also detect the earliest signs of disco-vertebral tubercular disease at an infra-radiological stage on both regular X-rays and CT scans [3,6,7]. Only bacteriological proof, either by biopsy of pre-vertebral soft tissues or by direct access to the focal point, can confirm the diagnosis [7,8], but sometimes the presumptive diagnosis is based on epidemiological, clinical, and radiological evidence. The treatment is based on poly anti-tuberculosis chemotherapy lasting approximately 12 months. The surgical indications are still much controversial [7,9]. The persistence of bone destruction with spinal instability is an indicator of surgical intervention. This treatment must be urgent in given the aggravation of a probable spinal cord compression [7]. Healing results in weight gain, biological normalization, and bone reconstruction with the fusion of bone lysed structures on X-ray.
Conclusion
The cervical localization of Pott's disease is extremely rare. The clinical and radiological findings are often deceptive, requiring the use of modern imaging equipment to enable an accurate diagnosis of anatomical lesions. Treatment is based on antibiotic therapy and immobilization of the cervical spine.
Footnotes
Cite this article: Maher Teka et al. Cervical spine tuberculosis. Pan African Medical Journal. 2020;37(7). 10.11604/pamj.2020.37.7.25226
Competing interests
The authors declare no competing interests.
Authors' contributions
Maher Teka: data collection, interpretation and drafting the case report; Hazem Ben Ghozlen: data collection, interpretation and drafting the case report; Akram Yassine Zaier: data collection and revising the case report; Majdi Ben Hnia: data collection and revising the case report; Nader Naouar: data collection and revising the case report; Faouzi Abid: Supervising and revising the case report. All the authors have read and agreed to the final manuscript.
References
- 1.Ahmed-Ramadan Sadek, William Wallage, Thiagarajan Jaiganesh. Cervical spine tuberculosis causing instability and neurological compromise. JRSM Short Rep. 2011 Jun;2(6):47. doi: 10.1258/shorts.2011.011040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Xin Hua Yin, Bao Rong He, Zhong Kai Liu, Ding Jun Hao. The clinical outcomes and surgical strategy for cervical spine tuberculosis: a retrospective study in 78 cases. Medecine (Baltimore) 2018 Jul;97(27):e11401. doi: 10.1097/MD.0000000000011401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fareeha Rauf, Umair Rashid Chaudhry, Mohammad Atif, Mujib ur Rahaman. Spinal tuberculosis: our experience and a review of imaging methods. Neuroradiol J. 2015 Oct;28(5):498–503. doi: 10.1177/1971400915609874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tao Shi, Zehua Zhang, Fei Dai, Qiang Zhou, Qingyi He, Fei Luo, et al. Retrospective study of 967 patients with spinal tuberculosis. Orthopedics. 2016 Sep 1;39(5):e838–43. doi: 10.3928/01477447-20160509-03. [DOI] [PubMed] [Google Scholar]
- 5.Hongwei Wang, Changqing Li, Jian Wang, Zhengfeng Zhang, Yue Zhou. Characteristics of patients with spinal tuberculosis: seven-year experience of a teaching hospital in Southwest China. International Orthopaedics (SICOT) 2012 Jul;36(7):1429–34. doi: 10.1007/s00264-012-1511-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Backer AID, Mortelé KJ, Vanschoubroeck IJ, Deeren D, Vanhoenacker FM, Keulenaer BLD, et al. Tuberculosis of the spine: CT and MRI features. JBR-BTR. 2005;88(2):92–77. [PubMed] [Google Scholar]
- 7.Garg RK, Somvanshi DS. Spinal tuberculosis: a review. The Journal of Spinal Cord Medicine. 2011 Sep;34(5):440–54. doi: 10.1179/2045772311Y.0000000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ali A, Musbahi O, White VLC, Montgomery AS. Spinal Tuberculosis: a literature review. JBJS Reviews. 2019 Jan;7(1):e9. doi: 10.2106/JBJS.RVW.18.00035. [DOI] [PubMed] [Google Scholar]
- 9.Khanna K, Sabharwal S. Spinal tuberculosis: a comprehensive review for the modern spine surgeon. The Spine Journal. 2019 Nov;19(11):1858–70. doi: 10.1016/j.spinee.2019.05.002. [DOI] [PubMed] [Google Scholar]