Abstract
Objective
To quantify the impact of the severe acute respiratory syndrome coronavirus 2 pandemic on emergency department volumes and patient presentations and evaluate changes in community mortality for the purpose of characterizing new patterns of emergency care use.
Patients and Methods
This is an observational cross-sectional study using electronic health records for emergency department visits in an integrated multihospital system with academic and community practices across 4 states for visits between March 17 and April 21, 2019, and February 9 and April 21, 2020. We compared numbers and proportions of common and critical chief symptoms and diagnoses, triage assessments, throughput, disposition, and selected hospital lengths of stay and out-of-hospital deaths.
Results
In the period of interest, emergency department visits decreased by nearly 50% (35037 to 18646). Total numbers of patients with myocardial infarctions, stroke, appendicitis, and cholecystitis diagnosed decreased. The percentage of visits for mental health symptoms increased. There was an increase in deaths, driven by out-of-hospital mortality.
Conclusion
Fewer patients presenting with acute and time-sensitive diagnoses suggests that patients are deferring care. This may be further supported by an increase in out-of-hospital mortality. Understanding which patients are deferring care and why will allow us to develop outreach strategies and ensure that those in need of rapid assessment and treatment will do so, preventing downstream morbidity and mortality.
Abbreviations and Acronyms: COVID-19, coronavirus disease 2019; ED, emergency department; EHR, electronic health record; ESI, emergency severity index; LOS, length of stay; ME, medical examiner; MI, myocardial infarction; MN, Minnesota; NSTEMI, non–ST-elevation myocardial infarction; SARS-CoV-2, severe acute respiratory syndrome coronavirus 2; SMRMEO, Southern Minnesota Regional Medical Examiner’s Office; STEMI, ST-elevation myocardial infarction
The onset of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic in the United States has brought significant changes to the operations of our health care system and country. Efforts to mitigate the spread of the novel coronavirus resulted in health care systems canceling all but the most urgent visits and developing plans to manage surges of critically ill patients. As noted in media reports from across the country,1, 2, 3, 4, 5 emergency departments (EDs) have reported large decreases in patient volumes. Reports from areas with earlier peaks of coronavirus disease 2019 (COVID-19) infection have reported decreases in numbers of ST-elevation myocardial infarctions (STEMIs)6, 7, 8 and ischemic strokes,9 suggesting that patients may be deferring care for serious conditions for which the prevalence would be expected to be stable. In a recent correspondence, Solomon et al10 describe a decline in myocardial infarctions (MIs) in both pre–COVID-19 and year-over-year comparisons, exploring concerns that patients may be deferring care due to fear of exposure to the novel coronavirus. These fears further extrapolate to concerns that delays in emergency care may lead to more individuals dying at home.11 No study to date has objectively assessed the impact of the COVID-19 pandemic on presentations to EDs.
In this study, the objectives were to characterize the impact of the COVID-19 pandemic on volume, chief symptom, and characteristics of patients presenting to 21 EDs across an integrated health system in 4 states. We also assess the impact on the rates of out-of-hospital deaths in an 8-county region in Minnesota.
Patients and Methods
Study Design
This study was approved by our Institutional Review Board and reporting adheres to the Strengthening the Reporting of Observational Studies in Epidemiology guideline for reporting epidemiologic studies.12 A protocol was written before beginning the study.
Setting
Mayo Clinic is a hospital system with 3 academic tertiary-care centers (Rochester, Minnesota [MN]; Jacksonville, Florida; and Scottsdale, Arizona) and a community health system in Minnesota and Wisconsin that includes 18 EDs and 16 hospitals ranging from critical access in rural communities to larger hubs with subspecialty care. The ED visits among sites are 1,500 to 78,000 annually and in 2019 were 359,932 across the enterprise. The Rochester, Minnesota, campus is a level I trauma center and includes a dedicated pediatric ED. All facilities use a common electronic health record (EHR; Epic Systems).
Participants
All patients who presented to any Mayo Clinic ED during the study periods between March 17 and April 21, 2019 and February 9 to April 21, 2020 were included, with the following predefined exceptions: urgent care visits and nurse only visits. A total of 91,353 patient visits were included.
Variables
We defined March 17 to April 21, 2020, as the time after the broad institution of distancing measures in response to the COVID-19 pandemic and term this the COVID period. To account for seasonal variation seen in emergency medicine, we compared this with both the 4 weeks before the COVID period (February 9 to March 16, 2020) and the same period in 2019 (March 17 to April 21). We termed these baseline comparators the peri-COVID and pre-COVID periods, respectively, and the aggregate is termed the baseline period. Investigators extracted patient demographic characteristics, chief symptom, diagnosis, disposition, and relevant time stamps to determine ED length of stay (LOS) and hospital LOS when appropriate.
To assess patient acuity, we considered each patient’s emergency severity index (ESI). The ESI is a front-end triage algorithm to categorize ED patients by illness acuity and resource needs (nursing care, medications, and therapeutic interventions). Level 1 is most urgent and level 5 is the least urgent.13
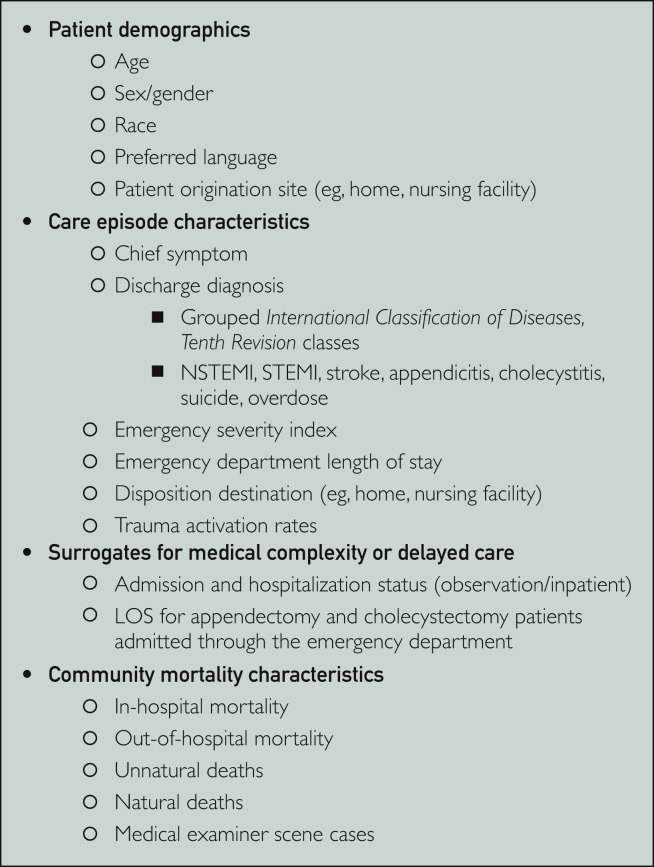
For evaluation of delayed and/or presentations, we selected diagnoses that would be expected to have stable rates among a population (MI, stroke, cholecystitis, and appendicitis). We identified surrogate markers that may indicate complicated courses, including hospital LOS for patients with appendicitis and cholecystectomy, rates of inpatient and observation hospitalization, and mortality. In the 8-county area serviced by the medical examiner (ME) affiliated with the Rochester, Minnesota, campus, we evaluated rates of in-hospital and out-of-hospital mortality that were referred to the ME. Figure 1 includes the complete listing of all variables analyzed.
Figure 1.
Variables for analysis of impact of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic on emergency department visits, March 17, 2019, to April 21, 2019, and February 9, 2020, to April 21, 2020. LOS = length of stay; NSTEMI = non–ST-elevation myocardial infarction; STEMI = ST-elevation myocardial infarction.
Data Sources/Measurement
Discrete fields in the EHR were queried to obtain the data for individual visits. Community mortality data were acquired from ME records.
Bias
Only information available in the EHR and from the ME was included in this analysis. Academic and community centers were studied independently and in combination to account for variable populations. These data are representative of the range of care and communities served by our institution and may not be generalizable for all health care systems. The ME data are representative of only a subset of our communities and may not be generalizable to the entire health system that was evaluated for ED visits.
Study Size
Our analysis for the peri-COVID and COVID period in early 2020 included 56,325 ED visits among all sites. For the pre-COVID to COVID comparison, 53,683 patient visits were analyzed. All patient visits in these periods were eligible for inclusion.
Quantitative Variables
Variables from the EHR included patient age, sex, race, preferred language, chief symptom, patient originating site (eg, clinic and other health care facility), ESI, ED LOS, hospital LOS for patients with appendicitis and cholecystitis, trauma activation level, final diagnosis, diagnosis class, and disposition. Natural and unnatural death, in-hospital deaths, out-of-hospital mortality, and ME scene deaths in the southeast Minnesota region were evaluated.
Statistical Methods
For hospital data, continuous features are summarized as median and interquartile range. Categorical features are summarized as frequency count and percentage. Chi-squared and Fisher exact tests were used to compare ED visits between periods. Comparisons of continuous features between periods were performed using Wilcoxon rank sum tests. All tests were 2 sided.
Data regarding community mortality include cause of death summarized as count and percentage. Chi-squared and Fisher exact tests were applied to compare deaths between periods. All tests were 2 sided. All P values were adjusted using the false discovery rate correction to prevent type I error. Adjusted P<.05 was considered significant, corresponding to an unadjusted P=.0244. Statistical analyses were performed using R (R Foundation for Statistical Computing, Vienna, Austria), version 3.6.2.
Results
Participants
The ED visits were divided into 2 main groups: visits to Mayo Clinic academic hospitals in Minnesota, Arizona, and Florida and visits to Mayo Clinic Health System community hospitals in Minnesota and Wisconsin. There were 91,353 visits to EDs captured between March 17 and April 21 in 2019 and February 9 through April 21 in 2020. Of these visits, 52,254 (57.2%) were to community hospitals and 56,316 (61.6%) occurred during 2020.
Descriptive Data
Of 91,353 patient visits, 85% (n=77,653) were adult and 15% (n=13,718) were pediatric. Most patients were white (86%; 78,585 of 91,353), with English as the preferred language (96%; 87,704 of 91,353), and 53.6% (48,978 of 91.353) of patients were female. A detailed breakdown of demographic information can be found in Supplemental Table 1 (available online at http://www.mayoclinicproceedings.org).
Main Results
Table 1 includes findings based on symptom and diagnosis. Compared with both the preceding 4 weeks (n=37,670), and the prior year (n=35,037), ED visits decreased 49% and 53.2% (n=18,646), respectively. The proportion of pediatric visits declined to 11.3% (2,104 of 18,646) of all visits, from 16.5% (n=6,205 of 37,670) 4 weeks prior and 15.4% (n=5,409 of 35,037) the prior year. There was a small decline in the proportion of women compared with men in both comparisons with baseline. There were small but statistically significant changes in the races of patients presenting, as well as minimal changes to the preferred languages of patients. There were fewer patients of all ethnicities who presented to academic and community settings (P<.001), with the exception of individuals of African origin, who did not experience a change in patient presentations to community hospitals (P=0.52) when comparing pre-COVID with during COVID. There were decreases visits for patients in all language groups (P<.001), with the exception of Somali (P=0.13) when comparing pre-COVID with COVID times in community hospitals, and Arabic (P=0.13) in community sites during both pre- and per-COVID compared with during COVID.
Table 1.
Change in Diagnoses in Pre-COVID, Peri-COVID, and COVID Era in Academic and Community Hospitalsa
| Peri-COVID (2/9-3/16/20) vs COVID Period (3/17-4/21/20) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Academic Hospitals |
Community Hospitals |
Overall |
|||||||
| 2/9/20-3/16/20 (N=16,181) | 3/17/20-4/21/20 (N=7779) | P | 2/9/20-3/16/20 (N=21,489) | 3/17/20-4/21/20 (N=10,867) | P | 2/9/20-3/16/20 (N=37,670) | 3/17/20-4/21/20 (N=18,646) | P | |
| Chief symptoms, no. (%) | |||||||||
| Abdominal pain | 1627 (10.1) | 806 (10.4) | .60 | 1739 (8.1) | 914 (8.4) | .50 | 3366 (8.9) | 1720 (9.2) | .38 |
| Back pain | 365 (2.3) | 163 (2.1) | .60 | 514 (2.4) | 267 (2.5) | .84 | 879 (2.3) | 430 (2.3) | .92 |
| Chest pain | 999 (6.2) | 553 (7.1) | .016b | 1156 (5.4) | 762 (7.0) | <.001b | 2155 (5.7) | 1315 (7.1) | <.001 |
| Other pain | 1579 (9.8) | 643 (8.3) | <.001b | 2008 (9.3) | 1099 (10.1) | .059 | 3587 (9.5) | 1742 (9.3) | .62 |
| Cough | 794 (4.9) | 564 (7.3) | <.001b | 1527 (7.1) | 637 (5.9) | .001b | 2321 (6.2) | 1201 (6.4) | .30 |
| Diarrhea | 148 (0.9) | 70 (0.9) | .99 | 200 (0.9) | 91 (0.8) | .59 | 348 (0.9) | 161 (0.9) | .62 |
| Earache or infection | 101 (0.6) | 48 (0.6) | >.99 | 363 (1.7) | 126 (1.2) | .002b | 464 (1.2) | 174 (0.9) | .003b |
| Fever | 846 (5.2) | 506 (6.5) | <.001b | 1193 (5.6) | 348 (3.2) | <.001b | 2039 (5.4) | 854 (4.6) | .001b |
| Gunshot wound | 0 (0) | 2 (0.0) | .30 | 3 (0.0) | 1 (0.0) | >.99 | 3 (0.0) | 3 (0.0) | .77 |
| Head injury or headache | 474 (2.9) | 181 (2.3) | .019b | 581 (2.7) | 271 (2.5) | .40 | 1055 (2.8) | 452 (2.4) | .023b |
| Laceration | 159 (1.0) | 99 (1.3) | .092 | 350 (1.6) | 264 (2.4) | <.001b | 509 (1.4) | 363 (1.9) | <.001 |
| Motor vehicle crash | 108 (0.7) | 45 (0.6) | .60 | 165 (0.8) | 55 (0.5) | .019b | 273 (0.7) | 100 (0.5) | .024b |
| Shortness of breath | 1038 (6.4) | 766 (9.8) | <.001b | 1352 (6.3) | 941 (8.7) | <.001b | 2390 (6.3) | 1707 (9.2) | <.001b |
| Skin rash | 99 (0.6) | 33 (0.4) | .14 | 192 (.9) | 81 (.7) | .29 | 291 (0.8) | 114 (0.6) | .077 |
| Throat symptoms | 151 (0.9) | 92 (1.2) | .14 | 442 (2.1) | 197 (1.8) | .24 | 593 (1.6) | 289 (1.5) | .92 |
| Vomiting | 406 (2.5) | 153 (2.0) | .024b | 700 (3.3) | 229 (2.1) | .001b | 1106 (2.9) | 382 (2.0) | .002b |
| Other | 7287 (45.0) | 3055 (39.3) | <.001b | 9004 (41.9) | 4584 (42.2) | .75 | 16,291 (43.2) | 7639 (41.0) | <.001b |
| Specific diagnosis, no. (%) | |||||||||
| Appendicitis | 54 (0.3) | 23 (0.3) | .81 | 65 (0.3) | 50 (0.5) | .064 | 119 (0.3) | 73 (0.4) | .26 |
| Cholecystitis | 47 (0.3) | 28 (0.4) | .59 | 51 (0.2) | 24 (0.2) | .92 | 98 (0.3) | 52 (0.3) | .92 |
| NSTEMI | 80 (0.5) | 38 (0.5) | >.99 | 92 (0.4) | 25 (0.2) | .018b | 172 (0.5) | 63 (0.3) | .090 |
| STEMI | 41 (0.3) | 10 (0.1) | .12 | 37 (0.2) | 21 (0.2) | .85 | 78 (0.2) | 21 (0.1) | .035b |
| Stroke | 183 (1.1) | 71 (0.9) | .22 | 126 (0.6) | 63 (0.6) | >.99 | 209 (0.6) | 134 (0.7) | .047b |
| Suicide | 25 (0.2) | 14 (0.2) | .85 | 39 (0.2) | 22 (0.2) | .85 | 64 (0.2) | 36 (0.2) | .73 |
| Overdose | 1 (0.0) | 1 (0.0) | >.99 | 4 (0.0) | 4 (0.0) | .65 | 5 (0.0) | 5 (0.0) | .58 |
| General diagnosis class by system, no. (%) | |||||||||
| Blood | 136 (0.8) | 61 (0.8) | .81 | 80 (0.4) | 25 (0.2) | .085 | 216 (0.6) | 86 (0.5) | .16 |
| Circulatory system | 727 (4.5) | 386 (5.0) | .18 | 599 (2.8) | 368 (3.4) | .008b | 1326 (3.5) | 754 (4.0) | .006b |
| Digestive system | 988 (6.1) | 622 (8.0) | <.001b | 1095 (5.1) | 771 (7.1) | <.001b | 2083 (5.5) | 1393 (7.5) | <.001b |
| Eyes or ears | 280 (1.7) | 90 (1.2) | .002b | 567 (2.6) | 210 (1.9) | .001b | 847 (2.2) | 300 (1.6) | .001b |
| Nervous system | 236 (1.5) | 91 (1.2) | .14 | 339 (1.6) | 140 (1.3) | .090 | 575 (1.5) | 231 (1.2) | .019b |
| Respiratory system | 1649 (10.2) | 902 (11.6) | .003b | 3687 (17.2) | 1315 (12.1) | <.001b | 5336 (14.2) | 2217 (11.9) | <.001b |
| Endocrine, nutritional, or metabolic disease | 336 (2.1) | 178 (2.3) | .44 | 348 (1.6) | 205 (1.9) | .15 | 685 (1.8) | 383 (2.1) | .11 |
| Factors influencing health status | 379 (2.3) | 189 (2.4) | .81 | 636 (3.0) | 266 (2.4) | .021b | 1016 (2.7) | 457 (2.5) | .15 |
| Genitourinary | 676 (4.2) | 456 (5.9) | <.001b | 810 (3.8) | 550 (5.1) | <.001b | 1486 (3.9) | 1006 (5.4) | <.001b |
| Infectious and parasitic disease | 341 (2.1) | 227 (2.9) | <.001b | 716 (3.3) | 315 (2.9) | .078 | 1057 (2.8) | 542 (2.9) | .62 |
| Injury, poisoning, or external cause | 1924 (11.9) | 900 (11.6) | .60 | 2788 (13.0) | 1793 (16.5) | <.001b | 4749 (12.6) | 2722 (14.6) | <.001b |
| Mental, behavioral, and neurodevelopmental | 429 (2.7) | 266 (3.4) | .003b | 670 (3.1) | 486 (4.5) | <.001b | 1104 (2.9) | 752 (4.0) | <.001b |
| Musculoskeletal system | 1093 (6.8) | 440 (5.7) | .003b | 1344 (6.3) | 735 (6.8) | .14 | 2437 (6.5) | 1175 (6.3) | .60 |
| Neoplasms | 39 (0.2) | 14 (0.2) | .59 | 16 (0.1) | 5 (0.0) | .60 | 55 (0.1) | 19 (0.1) | .32 |
| Pregnancy or childbirth | 27 (0.2) | 17 (0.2) | .60 | 95 (0.4) | 61 (0.6) | .26 | 122 (0.3) | 78 (0.4) | .15 |
| Skin and subcutaneous tissue | 416 (2.6) | 150 (1.9) | .008b | 468 (2.2) | 288 (2.7) | .021b | 884 (2.3) | 438 (2.3) | >.99 |
| Abnormal findings, not classified elsewhere | 5748 (35.5) | 2533 (32.6) | <.001b | 6588 (30.7) | 3058 (28.1) | <.001b | 12,356 (32.8) | 5596 (30.0) | <.001b |
| None | 318 (2.0) | 38 (0.5) | <.001b | 222 (1.0) | 27 (0.2) | .001b | 540 (1.4) | 65 (0.3) | <.001b |
| Pre-COVID (3/17-4/21/19) vs COVID Period (3/17-4/21/20) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Academic Hospitals |
Community Hospitals |
Overall |
|||||||
| 2019 (N=15,139) | 2020 (N=7779) | P | 2019 (N=19,898) | 2020 (N=10,867) | P | 2019 (N=35,037) | 2020 (N=18,646) | P | |
| Chief symptom, no. (%) | |||||||||
| Abdominal pain | 1704 (11.3) | 806 (10.4) | .077 | 1834 (9.2) | 914 (8.4) | .039b | 3538 (10.1) | 1720 (9.2) | .003b |
| Back pain | 431 (2.8) | 163 (2.1) | .001b | 550 (2.8) | 267 (2.5) | .19 | 981 (2.8) | 430 (2.3) | .002b |
| Chest pain | 1019 (6.7) | 553 (7.1) | .40 | 1287 (6.5) | 762 (7.0) | .12 | 2306 (6.6) | 1315 (7.1) | .075 |
| Other pain | 1631 (10.8) | 643 (8.3) | <.001b | 2070 (10.4) | 1099 (10.1) | .55 | 3701 (10.6) | 1742 (9.3) | <.001b |
| Cough | 412 (2.7) | 564 (7.3) | <.001b | 832 (4.2) | 637 (5.9) | <.001b | 1244 (3.6) | 1201 (6.4) | <.001b |
| Diarrhea | 136 (0.9) | 70 (0.9) | >.99 | 163 (0.8) | 91 (0.8) | .99 | 299 (0.9) | 161 (0.9) | >.99 |
| Earache or infection | 97 (0.6) | 48 (0.6) | .99 | 288 (1.4) | 126 (1.2) | .076 | 385 (1.1) | 174 (0.9) | .13 |
| Fever | 550 (3.6) | 506 (6.5) | <.001b | 695 (3.5) | 348 (3.2) | .27 | 1245 (3.6) | 854 (4.6) | <.001b |
| Gunshot wound | 3 (0.0) | 2 (0.0) | >.99 | 3 (0.0) | 1 (0.0) | >.99 | 6 (0.0) | 3 (0.0) | >.99 |
| Head injury or headache | 490 (3.2) | 181 (2.3) | <.001b | 569 (2.9) | 271 (2.5) | .11 | 1059 (3.0) | 452 (2.4) | .001b |
| Laceration | 179 (1.2) | 99 (1.3) | .73 | 436 (2.2) | 264 (2.4) | .27 | 615 (1.8) | 363 (1.9) | .19 |
| Motor vehicle accident | 123 (0.8) | 45 (0.6) | .10 | 175 (0.9) | 55 (0.5) | .002b | 298 (0.9) | 100 (0.5) | .002b |
| Shortness of breath | 862 (5.7) | 766 (9.8) | <.001b | 1219 (6.1) | 941 (8.7) | <.001b | 2081 (5.9) | 1707 (9.2) | <.001b |
| Skin rash | 124 (0.8) | 33 (0.4) | <.001b | 177 (0.9) | 81 (0.7) | .29 | 301 (0.9) | 114 (0.6) | .005b |
| Throat symptoms | 119 (0.8) | 92 (1.2) | .010b | 322 (1.6) | 197 (1.8) | .30 | 441 (1.3) | 289 (1.5) | .014b |
| Vomiting | 361 (2.4) | 153 (2.0) | .086 | 587 (3.0) | 229 (2.1) | <.001b | 948 (2.7) | 382 (2.0) | .001b |
| Other | 6898 (45.6) | 3055 (39.3) | <.001b | 8691 (43.7) | 4584 (42.2) | .020b | 15,589 (44.5) | 7639 (41.0) | <.001b |
| Specific diagnosis, no. (%) | |||||||||
| Appendicitis | 64 (0.4) | 23 (0.3) | .25 | 76 (0.4) | 50 (0.5) | .45 | 140 (0.4) | 73 (0.4) | >.99 |
| Cholecystitis | 51 (0.3) | 28 (0.4) | .97 | 43 (0.2) | 24 (0.2) | >.99 | 94 (0.3) | 52 (0.3) | .98 |
| NSTEMI | 74 (0.5) | 38 (0.5) | >.99 | 78 (0.4) | 25 (0.2) | .051 | 152 (0.4) | 63 (0.3) | .18 |
| STEMI | 21 (0.1) | 10 (0.1) | >.99 | 22 (0.1) | 21 (0.2) | .15 | 43 (0.1) | 21 (0.1) | .96 |
| Stroke | 169 (1.1) | 71 (0.9) | .25 | 121 (0.6) | 63 (0.6) | .95 | 290 (0.8) | 134 (0.7) | .27 |
| Suicide | 24 (0.2) | 14 (0.2) | .95 | 35 (0.2) | 22 (0.2) | .83 | 59 (0.2) | 36 (0.2) | .72 |
| Overdose | 5 (0.0) | 1 (0.0) | .77 | 3 (0.0) | 4 (0.0) | .53 | 8 (0.0) | 5 (0.0) | >.99 |
| General diagnosis class, no. (%) | |||||||||
| Blood | 125 (0.8) | 61 (0.8) | .93 | 76 (0.4) | 25 (0.2) | .067 | 201 (0.6) | 86 (0.5) | .16 |
| Circulatory system | 689 (4.6) | 386 (5.0) | .25 | 664 (3.3) | 368 (3.4) | .95 | 1353 (3.9) | 754 (4.0) | .41 |
| Digestive system | 941 (6.2) | 622 (8.0) | <.001b | 1122 (5.6) | 771 (7.1) | <.001b | 2063 (5.9) | 1393 (7.5) | <.001b |
| Eyes or ears | 279 (1.8) | 90 (1.2) | .001b | 520 (2.6) | 210 (1.9) | <.001b | 799 (2.3) | 300 (1.6) | <.001b |
| Nervous system | 257 (1.7) | 91 (1.2) | .005b | 352 (1.8) | 140 (1.3) | .005b | 609 (1.7) | 231 (1.2) | .002b |
| Respiratory system | 1034 (6.8) | 902 (11.6) | <.001b | 2198 (11.0) | 1315 (12.1) | .014b | 3232 (9.2) | 2217 (11.9) | <.001b |
| Endocrine, nutritional, or metabolic disease | 308 (2.0) | 178 (2.3) | .30 | 321 (1.6) | 205 (1.9) | .14 | 629 (1.8) | 383 (2.1) | .074 |
| Factors influencing health status | 393 (2.6) | 189 (2.4) | .59 | 597 (3.0) | 266 (2.4) | .014b | 990 (2.8) | 457 (2.5) | .027b |
| Genitourinary system | 677 (4.5) | 456 (5.9) | <.001b | 885 (4.4) | 550 (5.1) | .035b | 1562 (4.5) | 1006 (5.4) | <.001b |
| Infectious and parasitic disease | 227 (1.5) | 227 (2.9) | <.001b | 494 (2.5) | 315 (2.9) | .064 | 721 (2.1) | 542 (2.9) | <.001b |
| Injury, poisoning, or external cause | 1899 (12.5) | 900 (11.6) | .068 | 3059 (15.4) | 1793 (16.5) | .023b | 4958 (14.2) | 2722 (14.6) | .25 |
| Mental, behavioral, and neurodevelopmental | 386 (2.5) | 266 (3.4) | <.001b | 646 (3.2) | 486 (4.5) | <.001b | 1032 (2.9) | 752 (4.0) | <.001b |
| Musculoskeletal system | 1165 (7.7) | 440 (5.7) | <.001b | 1428 (7.2) | 735 (6.8) | .26 | 2593 (7.4) | 1175 (6.3) | <.001b |
| Neoplasms | 45 (0.3) | 14 (0.2) | .20 | 12 (0.1) | 5 (0.0) | .93 | 59 (0.2) | 19 (0.1) | .12 |
| Pregnancy or childbirth | 45 (0.3) | 17 (0.2) | .44 | 135 (0.7) | 61 (0.6) | .34 | 177 (0.5) | 78 (0.4) | .26 |
| Skin and subcutaneous tissue | 450 (3.0) | 150 (1.9) | <.001b | 499 (2.5) | 288 (2.7) | .59 | 949 (2.7) | 438 (2.3) | .029b |
| Abnormal findings, not classified elsewhere | 5640 (37.3) | 2533 (32.6) | <.001b | 6303 (31.7) | 3058 (28.1) | <.001b | 11,943 (34.1) | 5596 (30.0) | <.001b |
| None | 116 (0.8) | 38 (0.5) | .039b | 203 (1.0) | 27 (0.2) | <.001b | 369 (1.1) | 65 (0.3) | <.001b |
COVID = coronavirus disease; NSTEMI = non–ST-elevation myocardial infarction; STEMI = ST-elevation myocardial infarction.
Statistically significant.
There was a decline in the absolute number of all chief symptoms with the exception of gunshot wounds. The proportion of patients with a chief symptom of shortness of breath and chest pain increased during the COVID period (9.2% [1,707 of 18,646] and 7.1% [1,315 of 18,646]) from among all sites compared with peri-COVID (6.3% [2,390 of 37,670]; P<.001; 5.7% [2,155 of 37,670]; P<.001) and pre-COVID (5.9% [2,081 of 35,037]; P<.001; 6.6% [2,306 of 35,037]; P=.04) and were the only chief symptoms to have this consistency.
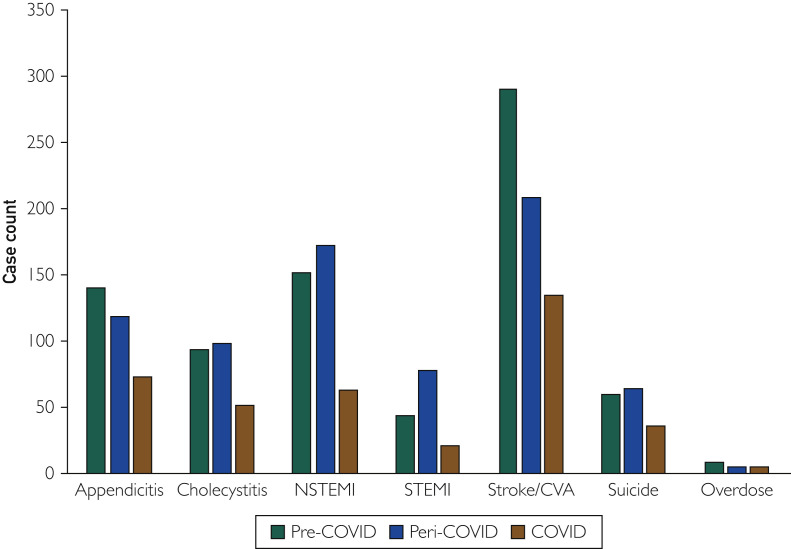
There was an absolute decrease in the number of presentations for diagnoses that were expected to remain static. For the community cohort, there was no change in the proportion of patients with all diagnoses excepting non-STEMI (NSTEMI), which decreased compared with pre-COVID levels (P=.025) and the peri-COVID period (P=.007) despite the 50% (35,037 and 37,637 to 18,646) decrease in patient volumes. Overall, there were fewer patients with a diagnosis of NSTEMI (peri-COVID: P=.047; pre-COVID: P =.11) and STEMI (peri-COVID: P=.016; pre-COVID: P=.85) compared with baseline periods. No difference was detected in the number or percentage of patients with a diagnosis of overdose (Figure 2 ).
Figure 2.
Changes in the number of patients diagnosed with ST-elevation myocardial infarction (STEMI), non-STEMI (NSTEMI), stroke/cerebrovascular accident (CVA), suicide, overdose, appendicitis, and cholecystitis during pre–coronavirus disease (COVID), peri-COVID, and COVID periods.
When diagnoses were divided into classes based on organ systems, there were increases in the percentages of patients with digestive, genitourinary, and mental health diagnoses. Respiratory system diagnoses were variable, with a significantly increased percentage compared with pre-COVID (9.2% [3,232 of 35,037] to 11.9% [1,707 of 18,646]; P<.001) driven by presentations to academic hospitals, and a small decrease compared with peri-COVID (14.2% [5,336 of 37,670] to 11.9% [1,707 of 18,646]; P<.001) due to a decrease in presentations to the community.
More patients during the COVID period (93.7%; 14,740 of 18,646) presented from a nonmedical setting (91.3% [31,996 of 35,037]; P<.001; 92% [34,657 of 37,670]; P<.001) and fewer were referred from clinics (4.5% [1,561 of 35,037] pre-COVID; P<.001; 4.1% [1,548 of 37,670] peri-COVID; P<.001). There was a small decrease in patients who were transferred to the academic centers from outside medical facilities, 1.9% (150 of 7779) during COVID, 2.9% (462 of 16,181) pre-COVID (P=<.001), and 1.1% (374 of 15139) peri-COVID (P<.001).
Table 2 shows markers for patient acuity. A small but overall increase in ESI 1 (+0.1%; P=.02 compared with pre-COVID) and 3 (+1.2%; P=.002 and +1.7%, P<.001 versus pre- and peri-COVID) and decrease in ESI 4 (−1.2%; P=0002 vs pre-COVID, −1.9%; P<.001 vs peri-COVID) was detected. The increased proportion of ESI 1 and 3 suggests an increase in acuity. The ED LOS decreased during March 17 to April 21, 2020, in both baselines in both academic and community sites. The admission rate increased in the COVID period (15%; 2,789 of 18,646) compared with both baselines (14.2% [4,974 of 35,037] pre-COVID; P=.018; 13.5% [5,069 of 37,670] peri-COVID; P<.001), driven by academic center activity that had more marked changes. Irregular departures decreased compared with both baselines.
Table 2.
Patient Acuity Measures and Surrogates of These During COVID Period Compared With Baseline in Academic Centers, Community Hospitals, and in Aggregatea
| Peri-COVID (2/9-3/16/20) vs COVID Period (3/17-4/21/20) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Academic Hospitals |
Community Hospitals |
Overall |
|||||||
| 2/9/20-3/16/20 (N=16,181) | 3/17/20-4/21/20 (N=7779) | P | 2/9/20-3/16/20 (N=21,489) | 3/17/20-4/21/20 (N=10,867) | P | 2/9/20-3/16/20 (N=37,670) | 3/17/20-4/21/20 (N=18,646) | P | |
| ESI, no. (%) | |||||||||
| Level 1 | 133 (0.8) | 67 (0.9) | .94 | 163 (0.8) | 108 (1.0) | .078 | 296 (0.8) | 175 (0.9) | .14 |
| Level 2 | 3262 (20.2) | 1615 (20.8) | .43 | 3244 (15.1) | 1583 (14.6) | .34 | 6506 (17.3) | 3198 (17.2) | .90 |
| Level 3 | 9825 (60.7) | 4727 (60.8) | >.99 | 11,586 (53.9) | 6202 (57.1) | <.001b | 21,411 (56.9) | 10,929 (58.6) | <.001b |
| Level 4 | 2824 (17.5) | 1300 (16.7) | .28 | 5646 (26.3) | 2536 (23.53) | <.001b | 8470 (22.5) | 3836 (20.6) | <.001b |
| Level 5 | 81 (0.5) | 39 (0.5) | >.99 | 687 (3.2) | 368 (3.4) | .54 | 768 (2.0) | 407 (2.2) | .42 |
| ED length of stay (h), median (interquartile range) | 3.8 (2.5-.4) | 3.2 (2.0-4.5) | <.001b | 2.4 (1.4-3.7) | 2.2 (1.3-3.4) | .001b | 2.9 (1.8-4.5) | 2.6 (1.5-3.9) | <.001b |
| Trauma activation level | |||||||||
| None | 16,110 (99.6) | 7745 (99.6) | >.99 | 21,368 (99.4) | 10,789 (99.3) | .21 | 37,487 (99.5) | 18,534 (99.5) | .30 |
| Green | 9 (0.1) | 7 (0.1) | .65 | 14 (0.1) | 12 (0.1) | .39 | 23 (0.1) | 19 (0.1) | .24 |
| Yellow | 22 (0.1) | 11 (0.1) | >.99 | 75 (0.3) | 47 (0.4) | .43 | 97 (0.3) | 58 (0.3) | .43 |
| Red | 40 (0.2) | 16 (0.2) | .81 | 32 (0.1) | 19 (0.2) | .85 | 72 (0.2) | 35 (0.2) | >.99 |
| ED disposition, no. (%) | |||||||||
| Catheterization laboratory | 27 (0.2) | 4 (0.1) | .078 | 17 (0.1) | 9 (0.1) | >.99 | 44 (0.1) | 13 (0.1) | .24 |
| Discharge | 10,508 (65.0) | 4988 (64.1) | .35 | 16,968 (79.0) | 8535 (78.6) | .55 | 27,476 (72.9) | 13,523 (72.5) | .47 |
| Hospital admission | 3538 (21.8) | 1879 (24.2) | <.001b | 1531 (7.1) | 910 (8.4) | <.001b | 5069 (13.5) | 2789 (15.0) | <.001b |
| Hospital/ED observation | 1476 (9.1) | 742 (9.5) | .46 | 1262 (5.9) | 629 (5.8) | .89 | 2738 (7.3) | 1371 (7.4) | .87 |
| Irregular departure | 399 (2.5) | 77 (1.0) | <.001b | 327 (1.5) | 108 (1.0) | .002b | 726 (1.9) | 185 (1.0) | .001b |
| Operating room | 91 (0.6) | 44 (0.6) | >.99 | 101 (0.5) | 72 (0.7) | .076 | 192 (0.5) | 116 (0.6) | .20 |
| Transfer to health care facility | 117 (0.7) | 32 (0.4) | .016b | 1240 (5.8) | 579 (5.3) | .21 | 1357 (3.6) | 611 (3.3) | .11 |
| Other | 25 (0.2) | 13 (0.2) | >.99 | 43 (0.2) | 25 (0.2) | .81 | 55 (0.1) | 44 (0.2) | .048 |
| Pre-COVID (3/17-4/21/19) vs COVID Period (3/17-4/21/20) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Academic Hospitals |
Community Hospitals |
Overall |
|||||||
| 2019 (N=15,139) | 2020 (N=7779) | P | 2019 (N=19,898) | 2020 (N=10,867) | P | 2019 (N=35,037) | 2020 (N=18,646) | P | |
| ESI, no. (%) | |||||||||
| Level 1 | 129 (0.9) | 67 (0.9) | >.99 | 134 (0.7) | 108 (1.0) | .010b | 263 (0.8) | 175 (0.9) | .049b |
| Level 2 | 3121 (20.6) | 1615 (20.8) | .97 | 2885 (14.5) | 1583 (14.6) | .99 | 6006 (17.1) | 3198 (17.2) | >.99 |
| Level 3 | 9032 (59.7) | 4727 (60.8) | .21 | 11,037 (55.5) | 6202 (57.1) | .021b | 20,069 (57.3) | 10,929 (58.6) | .007b |
| Level 4 | 2721 (18.0) | 1300 (16.7) | .024b | 4891 (24.6) | 2536 (23.4) | .021b | 7612 (21.7) | 3836 (20.6) | .007b |
| Level 5 | 84 (0.6) | 39 (0.5) | .85 | 758 (3.8) | 368 (3.4) | .13 | 842 (2.4) | 407 (2.2) | .21 |
| ED length of stay (h), median (interquartile range) | 3.6 (2.4-5.1) | 3.2 (2.0-4.5) | <.001b | 2.3 (1.4-3.6) | 2.2 (1.3-3.4) | .001b | 2.9 (1.7-4.3) | 2.6 (1.5-3.9) | <.001b |
| Trauma activation level, no. (%) | |||||||||
| None | 15,066 (99.5) | 7745 (99.6) | .88 | 19,777 (99.4) | 10,789 (99.3) | .43 | 34,843 (99.4) | 18,534 (99.4) | .70 |
| Green | 11 (0.1) | 7 (0.1) | .96 | 23 (0.1) | 12 (0.1) | >.99 | 34 (0.1) | 19 (0.1) | >.99 |
| Yellow | 21 (0.1) | 11 (0.1) | >.99 | 72 (0.4) | 47 (0.4) | .55 | 93 (0.3) | 58 (0.3) | .55 |
| Red | 41 (0.3) | 16 (0.2) | .58 | 26 (0.1) | 19 (0.2) | .58 | 67 (0.2) | 35 (0.2) | >.99 |
| ED disposition, no. (%) | |||||||||
| Catheterization laboratory | 24 (0.2) | 4 (0.1) | .10 | 11 (0.1) | 9 (0.1) | .66 | 35 (0.1) | 13 (0.1) | .48 |
| Discharge | 10,011 (66.1) | 4988 (64.1) | .007b | 15,562 (78.2) | 8535 (78.5) | .67 | 25,573 (73.0) | 13,523 (72.5) | .39 |
| Hospital admission | 3361 (22.2) | 1879 (24.2) | <.001b | 1613 (8.1) | 910 (8.4) | .56 | 4974 (14.2) | 2789 (15.0) | .024b |
| Hospital/ED observation | 1308 (8.6) | 742 (9.5) | .054b | 1222 (6.1) | 629 (5.8) | .35 | 2530 (7.2) | 1371 (7.4) | .76 |
| Irregular departure | 234 (1.5) | 77 (1.0) | .001b | 282 (1.4) | 108 (1.0) | .007b | 516 (1.5) | 185 (1.0) | .001b |
| Operating room | 89 (0.6) | 44 (0.6) | >.99 | 96 (0.5) | 72 (0.7) | .11 | 185 (0.5) | 116 (0.6) | .30 |
| Transfer to health care facility | 89 (0.6) | 32 (0.4) | .19 | 1069 (5.4) | 579 (5.3) | .99 | 1158 (3.3) | 611 (3.3) | .99 |
| Other | 23 (0.2) | 13 (0.2) | >.99 | 43 (0.2) | 25 (0.2) | >.99 | 66 (0.2) | 44 (0.2) | .43 |
COVID = coronavirus disease; ED = emergency department; ESI = emergency severity index.
Statistically significant.
Trauma presentations in our system are classified as “green” (minor), “yellow,” and “red” (severe). Compared with both baselines, the percentages of traumas were similar. However, the absolute number of red (n= 35 during COVID; n=72 peri-COVID; and n=67 pre-COVID) and yellow (n=58 during COVID; n=97 peri-COVID; and n=93 pre-COVID) declined overall, driven by a decrease at academic centers by nearly 60% (n=41 and 40 pre/peri-COVID, n=16 during COVID) for red traumas and 50% (n=21 and 22 pre/peri-COVID, n=11 during COVID) for yellow.
In addition to the diagnoses, we evaluated hospital LOS for patients with appendicitis and cholecystitis as a surrogate for a complicated hospital course, with the assumption that a longer LOS may be indicative of complications, potentially due to delayed presentation. There was no increased hospital LOS for patients with either appendicitis or cholecystitis.
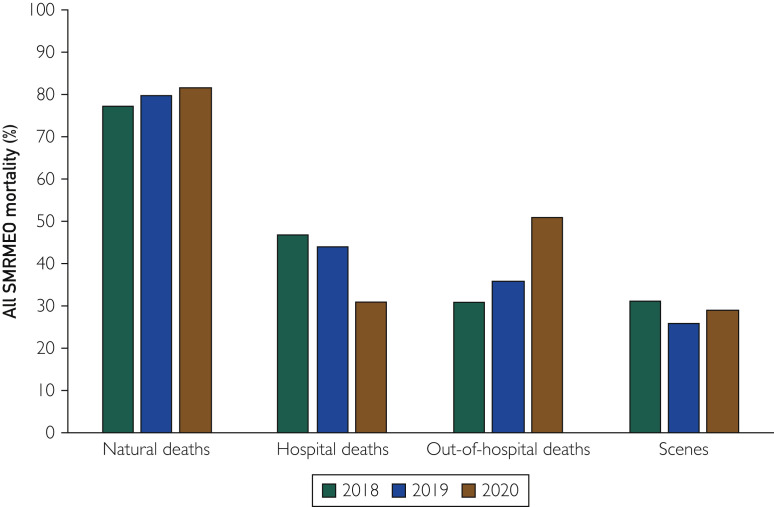
Mortality was considered a surrogate for delayed/deferred emergency care. Southern Minnesota Regional ME’s Office data showed an increase in natural deaths during the COVID period (n=250) vs pre-COVID (n=204) baseline (P=.037). Out-of-hospital mortality for natural and non-natural deaths (non–COVID-related) increased from 35.8% (73 of 204 deaths) pre-COVID to 51.2% (128 of 251 deaths) during the COVID period (P=.001). The significant increase in out-of-hospital mortality drives the overall mortality increase (Figure 3 ; Supplemental Table 2, available online at http://www.mayoclinicproceedings.org).
Figure 3.
Medical examiner mortality data for 8-county region in southern Minnesota during 2020 pandemic compared with the same 4-week period for years prior. SMRMEO = Southern Minnesota Regional Medical Examiner’s Office.
Discussion
Key Results
Our health system, which represents a variety of practice types, experienced a dramatic decrease in ED visits during the early SARS-CoV-2 pandemic. This included decreases in patient presentations for almost all variables studied, the exception being no change in the small number of gunshot wounds. Increased admission rate and increased presenting acuity based on ESI both suggest that patients who presented were sicker than those in the baseline periods.
We found declines in the absolute numbers of patients with STEMI, NSTEMI, stroke, appendicitis, and cholecystitis, which would not be expected to result from social distancing measures. With fewer of these time-sensitive diagnoses being made in EDs, there is concern that delayed or deferred care may result in downstream morbidity (eg, heart failure or hemiparesis) or mortality. We did not find evidence of prolonged hospital stays for patients with appendicitis/cholecystitis, suggesting that although we are seeing smaller numbers, there is no morbidity increase, using this as a surrogate.
There was a decline in the number of patients with a mental health diagnosis class. However, the proportion of patients who presented increased. This indicates that patients with mental health concerns continued to visit the ED when other potential patients chose to defer care.
During the COVID era, there was an increase in ME-reported natural (non–COVID-related) deaths compared with baseline periods, which is extremely concerning. Recognizing the limitations of these data and that this represents correlation and not causation, this supports the concern that patients are deferring emergency care, resulting in mortality.
Limitations
There have been variable recommendations and executive orders from included state governments, which may have an effect on behaviors of patients seeking ED care that we are unable to measure.
Our use of county-based morality data introduces a degree of bias because not all deaths within all communities evaluated are included in that data set. Limitations due to availability of information affected our ability to obtain these data and meant that only a single region was able to be included. We believed that despite the incomplete data set, this was an important finding that warranted inclusion and analysis. Use of these data limits the ability to comment on broader patterns of mortality in all communities for which we assessed ED visits.
The scope of this study does not include other potential causes for shifts in visits. Broadly, there was a sharp decline in outpatient visits and surgeries within our system, and rapid introduction of new visit types such as telephone and telehealth visits changed the way we delivered care during this time, which may have affected patterns of ED visits.
Interpretation
Overall, ED visits decreased by approximately 50% both year over year and in the 4-week lead up to the period of interest from March 17 to April 21, 2020.
During the COVID period, most ED presenting symptoms decreased proportionally compared with the year and weeks prior. This included presentations for which numbers would be expected to remain constant due to the baseline community incidence of disease, suggesting that some patients may be deferring care. The difference between presentations to community vs academic centers in STEMI diagnosis may in part be due to a decrease in travel for medical care and an effective decline in the population served by academic centers, while community hospitals would maintain their population base. However, this was not seen in other selected diagnoses.
From March 17 to April 21, 2020, the number of patient presentations for severe trauma decreased during the time frame studied while minor trauma visit numbers increased. The interaction between statewide stay-at-home orders, decreased travel, and closures of nonessential businesses and schools have dramatically changed daily lives, and this may translate to different risks and actualization of severe injury.
Prior studies have shown that in the setting of natural disasters, a disruption of usual medical maintenance,14 patients with chronic diseases may similarly defer care during a pandemic due to concerns over infection or limited access to outpatient care.
Generalizability
Our results can be evaluated in both the context of a broad range of community practices and academic centers. Our data demonstrate findings that may be expected; for academic centers that attract patients from other communities, effectively increasing the local population, there is a decreased number of diagnoses that remain stable in community practice, such as MI, cerebrovascular accident, appendicitis, and cholecystitis. Our sites do not include any safety net hospitals in urban areas, and results may not reflect their experiences. Finally, the prevalence and rate of increase of SARS-CoV-2 infection varied dramatically across the country. During the study period, our sites had relatively flat curves compared with other regions, potentially limiting the generalizability of our findings.
Conclusion
Our study confirms that ED visits decreased in the setting of the SARS-Cov-2 pandemic. We do not have complete understanding of the reasons for these declines, and we do not know what the downstream effects of the change in pattern of ED presentations will be. This work is important for several reasons.
Deferred Acute Care
Patients may defer care for a variety of reasons, including fear of exposure. The increase in out-of-hospital deaths is a worrisome finding, suggesting that deferred care may have grave consequences. Although we did not find a difference in our surrogate markers for medical complications, our scope was narrow and the time frame was short. As we emerge from the pandemic and health care systems resume operations with new precautions, these patients will need to be identified and appropriately prioritized to manage potential complications.
Reimbursement Models
Emergency departments rely on predictable volumes to guide staffing and maintain the infrastructure to provide around-the-clock care. Disruptions to these volumes threaten the financial viability of these bedrock safety nets that are more essential than ever in the midst of a global pandemic.
Pandemic Planning
As we plan for coming waves of this pandemic and unknown crises on the horizon, we need to analyze the impact of our responses and make informed plans to understand and mitigate the collateral impact of our actions. We have crossed the threshold of 200,000 deaths in the United States, and should remember that the impact of the pandemic will not end with those with significant morbidity and mortality due to the infection. We need to find ways to ensure that patients seek and receive necessary emergent care even as we flatten the curve.
Footnotes
Potential Competing Interests: The authors declare no competing interests.
Supplemental material can be found online at http://www.mayoclinicproceedings.org. Supplemental material attached to journal articles has not been edited, and the authors take responsibility for the accuracy of all data.
Supplemental Online Material
References
- 1.Bernstein L., Sellers F.S., Health Patients with heart attacks, strokes and even appendicitis vanish from hospitals. The Washington Post. April 19, 2020. https://www.washingtonpost.com/health/patients-with-heart-attacks-strokes-and-even-appendicitis-vanish-from-hospitals/2020/04/19/9ca3ef24-7eb4-11ea-9040-68981f488eed_story.html
- 2.Molseed J. Lifestyle. Health officials: emergency rooms are open. Rochester Post Bulletin. COVID-19 Coverage. April 16, 2020. https://www.postbulletin.com/life/health/health-officials-emergency-rooms-are-open/article_7ab4677e-8029-11ea-a2ef-0b0bd7648eba.html
- 3.Stradling R. Local. Fewer people are going to Triangle emergency rooms, and that could be a bad thing. The News and Observer. April 21, 2020. https://www.newsobserver.com/news/local/article242133886.html
- 4.Alvarez F. Health Care. As heart attack rates plummet, doctors worry patients are avoiding the ER. Sacramento Business Journal. April 27, 2020. https://www.bizjournals.com/sacramento/news/2020/04/27/as-heart-attack-rates-plummet-doctors-worry.html
- 5.Krumholz H.M. Doctors. Where have all the heart attacks gone? The New York Times. April 6, 2020. Updated May 14, 2020. https://www.nytimes.com/2020/04/06/well/live/coronavirus-doctors-hospitals-emergency-care-heart-attack-stroke.html
- 6.De Filippo O., D’Ascenzo F., Angelini F. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. https://doi.org/10.1056/NEJMc2009166 [published online ahead of print April 28, 2020]. N Engl J Med. [DOI] [PMC free article] [PubMed]
- 7.Garcia S., Albaghdadi M.S., Meraj P.M. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Metzler B., Siostrzonek P., Binder R.K., Bauer A., Reinstadler S.J. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. https://doi.org/10.1093/eurheartj/ehaa314 [published online ahead of print April 16, 2020]. Eur Heart J. [DOI] [PMC free article] [PubMed]
- 9.Morelli N., Rota E., Terracciano C. The baffling case of ischemic stroke disappearance from the casualty department in the COVID-19 era. Eur Neurol. 2020;83:213–215. doi: 10.1159/000507666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Solomon M.D., McNulty E.J., Rana J.S. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383(7):691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 11.Gillum J., Song L., Kao J. There’s been a spike in people dying at home in several cities. That suggests that coronavirus deaths are higher than reported. ProPublica. Coronavirus. April 14, 2020. https://www.propublica.org/article/theres-been-a-spike-in-people-dying-at-home-in-several-cities-that-suggests-coronavirus-deaths-are-higher-than-reported
- 12.Von Elm E., Altman D.G., Egger M., Pocock S.J., Gotzsche P.C., Vandenbroucke J.P., STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–577. doi: 10.7326/0003-4819-147-8-200710160-00010. [DOI] [PubMed] [Google Scholar]
- 13.Gilboy N., Tanabe P., Travers D., Rosenau A.M. AHRQ; Rockville, MD: November 2011. Emergency Severity Index (ESI): A Triage Tool for Emergency Department Care, Version 4. Implementation Handbook 2012 Edition. Publication No. 12-0014. [Google Scholar]
- 14.Miller A.C., Arquilla B. Chronic diseases and natural hazards: impact of disasters on diabetic, renal and cardiac patients. Prehosp Disaster Med. 2008;23(2):185–194. doi: 10.1017/s1049023x00005835. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.