Abstract
Aim
Out-of-hospital cardiac arrest (OHCA) during COVID-19 has been reported by countries with high case numbers and overwhelmed healthcare services. Imposed restrictions and treatment precautions may have also influenced OHCA processes-of-care. We investigated the impact of the COVID-19 pandemic period on incidence, characteristics, and survival from OHCA in Victoria, Australia.
Methods
Using data from the Victorian Ambulance Cardiac Arrest Registry, we compared 380 adult OHCA patients who received resuscitation between 16th March 2020 and 12th May 2020, with 1218 cases occurring during the same dates in 2017−2019. No OHCA patients were COVID-19 positive. Arrest incidence, characteristics and survival rates were compared. Regression analysis was performed to understand the independent effect of the pandemic period on survival.
Results
Incidence of OHCA did not differ during the pandemic period. However, initiation of resuscitation by Emergency Medical Services (EMS) significantly decreased (46.9% versus 40.6%, p = 0.001). Arrests in public locations decreased in the pandemic period (20.8% versus 10.0%; p < 0.001), as did initial shocks by public access defibrillation/first-responders (p = 0.037). EMS caseload decreased during the pandemic period, however, delays to key interventions (time-to-first defibrillation, time-to-first epinephrine) significantly increased. Survival-to-discharge decreased by 50% during the pandemic period (11.7% versus 6.1%; p = 0.002). Survivors per million person-years dropped in 2020, resulting in 35 excess deaths per million person-years. On adjusted analysis, the pandemic period remained associated with a 50% reduction in survival-to-discharge.
Conclusion
The COVID-19 pandemic period did not influence OHCA incidence but appears to have disrupted the system-of-care in Australia. However, this could not completely explain reductions in survival.
Keywords: Out-of-hospital cardiac arrest, COVID-19 pandemic, System-Of-Care, Survival, Patient outcomes
Introduction
Planning and preparation for disease outbreaks is critical to maintaining healthcare services during a pandemic. The novel coronavirus disease 2019 (COVID-19) pandemic has introduced unprecedented challenges and implications for healthcare services worldwide, including pre-hospital emergency medical services (EMS). This has been particularly pertinent for medical emergencies such as out-of-hospital cardiac arrest (OHCA) that require a time-dependent emergency response.
Annually, over 6500 cases of OHCA are attended by Ambulance Victoria (AV) paramedics in Victoria, Australia1. Survival from OHCA is low at just 10–12%, reflecting global figures1. For the pre-hospital response to OHCA, a highly co-ordinated system-of-care that optimises survival and functional outcomes is paramount. System elements include time-dependent intervention strategies in the pre-hospital setting (e.g. early defibrillation) and use of appropriate diagnostic and treatment strategies at receiving hospitals. Any disruption to this system-of-care could significantly influence patient outcomes.
To date, the narrative of OHCA during COVID-19 has been defined by countries devastated by huge case numbers and overwhelmed healthcare services2, 3, 4, 5, 6, 7. Italy experienced a 58% increase in OHCA incidence compared to 2019 and a 15% increase in death, with 77.4% of the increase in cases directly associated with COVID-19 infection2. A similar story was seen in New York with an increase in patients deceased on arrival increasing over 6-fold3. In Paris, the proportion of patients who had an OHCA and were admitted to hospital alive decreased from 22.8% to 12.8% and COVID-19 infection accounted for a third of the increase in OHCA incidence during the pandemic period4.
For countries where infection and case-fatality rates have been low, imposed social restrictions and treatment precautions may also have influenced OHCA processes-of-care. Australia is a key example of a country with low infection and case-fatality during the first wave of COVID-19. Despite low cases, time-sensitive OHCA interventions have been interrupted by the need for donning personal protective equipment (PPE) and changes in arrest management have been introduced including altered approaches to airway management in basic and advanced life support algorithms8, 9, 10, 11, 12. In addition, the GoodSAM mobile phone system used to alert bystanders to a nearby arrest was switched off meaning that co-responding members of the community were not able to contribute to resuscitation efforts. The impact of these changes on the OHCA “Chain of Survival” is yet to be completely elucidated. Therefore, we investigated the impact of the COVID-19 pandemic period on the incidence, arrest characteristics, and survival from OHCA in Victoria, Australia.
Methods
Study design
We conducted a retrospective cohort study of adult OHCA patients (aged>15 years) attended by paramedics in Victoria, Australia between 16th March and 12th May every year over 4 years (2017–2020). EMS witnessed OHCA events and patients for whom a Do-Not-Resuscitate order/Advanced Care Directive was in place were excluded from analyses. The COVID-19 pandemic period was defined as 16th March 2020 (State of Emergency declared) through to midnight on 12th May (Stage 3 restrictions eased). Stage 3 restrictions involved social distancing and individuals remaining at home except for essential shopping, care and caregiving, daily exercise, work and study (if this could not be done from home). For the pre-pandemic comparator period, we combined data from the same dates in 2017−2019. This study was approved by the Monash University Human Research Ethics Committee (Project#: 24377).
Setting
This study was conducted in Victoria, Australia which has a population of 6.4 million people spread over almost 227,500km2. Over 4.9 million people live in the state’s capital city of Melbourne. AV is the sole provider of EMS in the state. AV comprises ambulance paramedics who have advanced life support skills including supraglottic airway and intravenous epinephrine administration, and Mobile Intensive Care Ambulance paramedics who are authorised to perform endotracheal intubation and administer intravenous amiodarone, atropine and provide transcutaneous pacing. Mechanical CPR is available for prolonged arrests and selected patients requiring CPR to hospital.
AV cardiac arrest management guidelines follow recommendations of the Australian Resuscitation Council1. First-responders (fire services and community volunteers) are also alerted and dispatched to suspected cardiac arrests at the point of the emergency call13.
From January 2020, a Health Incident Action Plan (with revisions according to updated Governmental guidelines) and a COVID-19 Clinical Practice Guideline were implemented by AV. For OHCA cases, AV treatment guidelines were based on guidance from the International Liaison Committee on Resuscitation (ILCOR)8, Australian Resuscitation Council9 and American Heart Association9, 10 and recommended suspension of bag-valve-mask ventilation, early use of endotracheal intubation and mechanical CPR, and minimisation of airway suctioning (where possible) to limit aerosol exposure. During this period, donning of airborne precaution PPE was required for every confirmed OHCA11, 12. Also, the system for alerting community first-responders to nearby arrests was suspended due to concerns over appropriate PPE use.
Data sources
We used data from the Victorian Ambulance Cardiac Arrest Registry (VACAR) to quantify the impact of the COVID-19 pandemic period on OHCA incidence and outcomes. The methodology of the registry has been described previously13. Briefly, data for every potential OHCA is uploaded to VACAR from the AV Data Warehouse and patient care records are also used to complete case records. Each potential case is reviewed for registry inclusion. Patients of all ages who suffer a documented cardiac arrest which occurs in the state of Victoria, patients who are pulseless on EMS arrival or become pulseless in the presence of EMS and patients who were successfully defibrillated prior to EMS arrival are included in VACAR1. Demographics, vital signs, symptoms, case-related time intervals, in-hospital management and outcomes are collected. In-patient data is obtained from treating hospitals and death data is obtained from the Registry of Births, Deaths and Marriages Victoria. Population data (estimated resident population by single year of age in Victoria) was obtained from the Australian Bureau of Statistics (ABS)14. EMS emergency caseload data was obtained from the Computer-Aided Dispatch system and AV Clinical Data Warehouse and included all cases where an emergency ambulance attended. Data on COVID-19 positive cases were obtained daily from the Victorian Department of Health and Human Services and linked to AV patient records via probabilistic linkage to identify any COVID-19 positive OHCAs.
Statistical analysis
Categorical variables are presented as frequencies and proportions, and continuous variables are presented as median and interquartile range (IQR) or mean and standard deviation (SD), where appropriate. Differences in continuous data between the two time periods were assessed using the independent t-test for normally distributed data and the Wilcoxon rank-sum test for non-parametric data. Differences in categorical data between the two time periods were determined using the Chi-square (χ2) test. Incidence rates and rates of survivors per million person-years were calculated using population figures from the ABS as at 30th June in the year prior. Adjusted multivariable logistic regression was used to calculate Odds Ratios (ORs) and 95% Confidence Intervals (CIs) to assess the effect of the pandemic period on event survival (pulse present at hospital) and survival to hospital discharge, in patients with an attempted resuscitation. Logistic regression was conducted in the overall cohort (all rhythms) and separately for those presenting in a shockable rhythm (VF/VT) both for survival to hospital and survival to discharge. Covariates used for adjustment included factors known to influence survival from OHCA. Demographic factors (age, gender), response time, arrest rhythm, cardiac aetiology, public arrest location, having a bystander witness the arrest, provision of bystander CPR and, for those in a shockable rhythm, who provided the first shock (PAD versus first responder or AV) were included in the model. Call-to-patient time was also included due to the introduction of PPE. Data were analysed using Stata Statistical software 15 (StataCorp, 2017, College Station, TX). A two-sided p-value of <0.05 was considered statistically significant.
Results
Between 16th March 2020 (State of Emergency declared) and 12th May 2020 (Stage 3 restrictions lifted), 935 OHCA were attended by EMS in Victoria, Australia. During the same time period, 1453 cases of COVID-19 were laboratory-confirmed with an incidence of 159 per 100,000 person-years15. Eighteen of these cases were fatal, providing a case fatality rate of 1.24%15, 16. For the same time period in 2017–2019, 2599 OHCA were attended. Of all attendances to cardiac arrest, 380 and 1218 arrests received EMS attempted resuscitation in the pandemic and comparator periods, respectively. The incidence rate of attended adult arrests during the pandemic period was not significantly different from the comparator period (127 per 100,000 person-years versus 123 per 100,000 person-years, respectively). However, the proportion of EMS attended OHCA that received any attempt at resuscitation significantly decreased during the pandemic period (46.9% in the comparator period versus 40.6% in the pandemic period, p = 0.001).
Table 1 summarises the patient, arrest and management characteristics of patients in the pandemic and comparator periods who received EMS attempted resuscitation. Patient age and gender distribution did not differ between the two periods. Arrests occurring in public locations significantly decreased by more than 50% in the pandemic period (20.8% in the comparator period versus 10.0% during the pandemic; p < 0.001) and initial shocks by public access defibrillation (PAD)/first-responders also decreased (6.9% versus 3.9% during the pandemic period, p = 0.037). Bystander CPR significantly increased by more than 5% during the pandemic period; it was bystander CPR provided in private residences and not in public locations that significantly increased.
Table 1.
Characteristics of adult OHCA patients with attempted resuscitation (excluding EMS witnessed events) during the COVID-19 pandemic period compared to a pre-pandemic comparator period in Victoria, Australia.
| Characteristic | Arrests during COVID-19 pandemic period (n = 380) | Arrests during pre-pandemic comparator period (n = 1218) | p value |
|---|---|---|---|
| Female, n (%) | 130 (34.2%) | 373 (30.6%) | 0.081 |
| Median age, years (IQR) | 69 (54, 80) | 67 (52, 78) | 0.304 |
| Aged ≥ 75 years, n (%) | 141 (37.1%) | 414 (34.0%) | 0.265 |
| Median call-to-dispatch time, mins (IQR) | 1.0 (1.0, 2.0) | 1.0 (1.0, 2.0) | 0.226 |
| Median response time, mins (IQR) | 8.0 (6.5, 10.6) | 7.5 (6.0, 10.2) | 0.001 |
| Median call-to-patient time, mins (IQR) | 9.8 (8.0, 12.8) | 8.5 (6.6, 11.4) | <0.001 |
| Median at scene-to-at patient time, mins (IQR) | 2.0 (1.0, 3.0) | 1.0 (1.0, 2.0) | <0.001 |
Precipitating event, n (%)
|
269 (72.3%) 24 (6.3%) 22 (5.8%) 15 (4.0%) 18 (4.7%) 24 (6.3%) | 929 (77.9%) 50 (4.1%) 60 (4.9%) 44 (3.6%) 58 (4.8%) 51 (4.2%) | 0.025 0.073 0.505 0.762 0.984 0.087 |
| Public location of arrest, n (%) | 38 (10.0%) | 253 (20.8%) | <0.001 |
| Bystander witnessed, n (%) | 201 (52.9%) | 644 (52.9%) | 0.994 |
Bystander CPR, n (%)
|
299 (78.7%) 35 (92.1%) 264 (77.2%) | 889 (73.0%) 204 (80.6%) 685 (70.9%) | 0.026 0.085 0.027 |
| Initial/arrest rhythm VF/VT, n (%) | 90 (23.7%) | 318 (26.1%) | 0.344 |
| Shocked first by PAD or first responder, n (%) | 15 (3.9%) | 84 (6.9%) | 0.037 |
| Median time-to-first shock, mins (IQR) | 14.0 (10.0, 19.5) | 11.0 (9.0, 17.0) | <0.001 |
Median resuscitation duration, mins (IQR)
|
14.5 (6.0, 32.0) 23.0 (13.0, 33.5) 10.0 (4.0, 30.5) 11.0 (5.0, 32.0) | 17.0 (6.0, 32.0) 16.0 (8.0, 26.0) 18.0 (5.0, 33.0) 19.0 (5.0, 33.0) | 0.525 <0.001 0.015 0.125 |
| Intubation, n (%) | 171 (45.8%) | 594 (48.8%) | 0.323 |
| Mechanical CPR, n (%) | 56 (14.7%) | 177 (14.5%) | 0.921 |
| Amiodarone, n (%) | 72 (19.0%) | 188 (15.4%) | 0.105 |
| Atropine, n (%) | 11 (2.9%) | 40 (3.3%) | 0.706 |
| Epinephrine, n (%) | 193 (50.8%) | 742 (60.9%) | <0.001 |
| ROSC achieved at scene, n (%) | 112 (29.5%) | 416 (34.2%) | 0.090 |
| Died at scene, n (%) | 285 (75.0%) | 827 (67.9%) | 0.009 |
| Transported with CPR, n (%) | 3 (0.8%) | 30 (2.5%) | 0.045 |
| Transported with ROSC, n (%) | 91 (24.0%) | 360 (29.6%) | 0.034 |
|
92 (24.3%) 22 (6.1%) 17 (20.0%) | 359 (29.5%) 142 (11.7%) 116 (36.7%) | 0.050 0.002 0.004 |
Resuscitation duration during the pandemic period was shortened by a median 2.5 minutes; median duration was significantly longer for patients with return of spontaneous circulation (ROSC) and significantly shorter for those where ROSC was not achieved (Table 1). No confirmed COVID-19 positive patient was in cardiac arrest on EMS arrival during the study period.
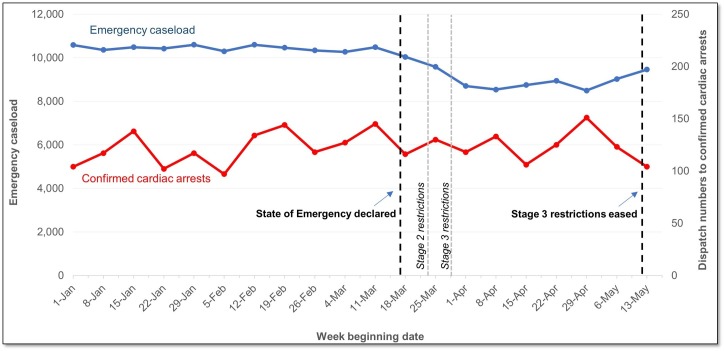
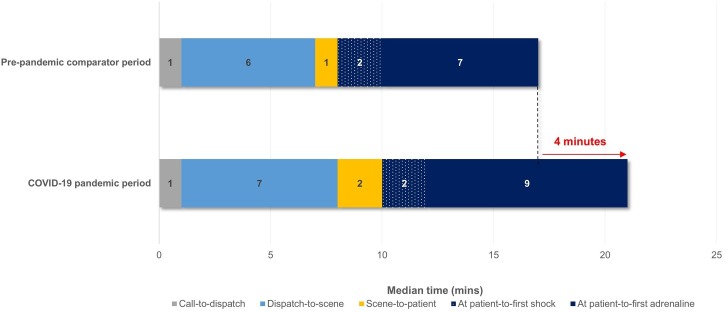
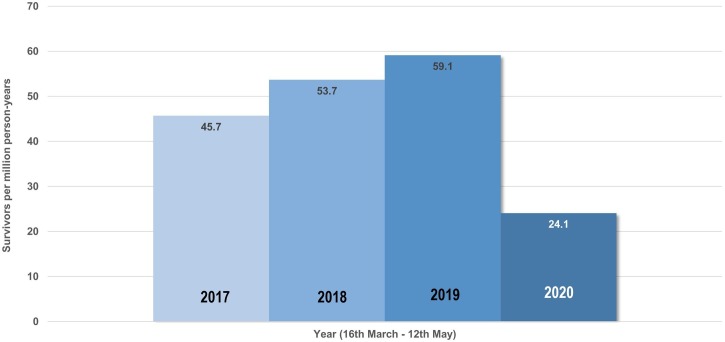
Overall EMS emergency caseload decreased significantly during the pandemic period (Fig. 1 ). However, delays to key life-saving interventions in the OHCA system-of-care increased (Fig. 2 ). Time-to-first defibrillation and time-to-first epinephrine were delayed by a further 2 minutes, resulting in a median 4-minute total delay during resuscitation efforts. The proportion of OHCA patients discharged alive during the pandemic period decreased by almost 50% (11.7% in the comparator period versus 6.1% in the pandemic period; p = 0.002) as it did for patients presenting in a shockable rhythm (36.7% during the comparator period versus 20.0% in the pandemic period, p = 0.004). Survivors per million person-years dropped to 24 in the pandemic period in 2020 from 59 per million person-years for the same timeframe in 2019 and 54 per million person-years in 2018, resulting in an estimated 35 excess deaths per million person-years (Fig. 3 ). Extrapolated over 12 months, this would result in 186 excess deaths from OHCA in Victoria.
Fig. 1.
Overall emergency caseload and confirmed cardiac arrest attendances in Victoria, Australia – 1st January 2020 to 13th May 2020.
Fig. 2.
Median times to key elements of the EMS response to adult OHCA where resuscitation was attempted (excluding EMS witnessed events) during the COVID-19 pandemic period (16th March 2020 – 12th May 2020) relative to the pre-pandemic comparator period (16th March – 12th May in 2017, 2018 and 2019 combined) in Victoria, Australia.
Fig. 3.
Survivors per million person-years of adult OHCA with resuscitation attempted (excluding EMS witnessed events) during the COVID-19 pandemic period 16th March 2020 – 12th May 2020 and during the same dates in 2017, 2018 and 2019 in Victoria, Australia.
Despite adjustment for delays to arriving at-patient and changes in arrest characteristics, the risk-adjusted odds of survival to hospital discharge for all attempted resuscitations reduced by 54% during the pandemic period (OR 0.46, 95% CI 0.25−0.86, p = 0.015; Table 2 ). The same was demonstrated in patients presenting in a shockable rhythm (OR 0.50, 95% CI 0.26−0.96, p = 0.037; Table 3 ). In comparison, the impact of the pandemic period on event survival (pulse present at hospital arrival) was not significant after adjustment for the same factors (for the overall cohort: OR 0.73, 95% CI 0.49–1.11, p = 0.140; for patients presenting in a shockable rhythm: OR 0.64, 95% CI 0.39–1.06, p = 0.085) (Supplementary Tables S1 and S2).
Table 2.
Adjusted odds ratio of the effect of the pandemic period on survival to hospital discharge in all patients with EMS attempted resuscitation.
| OR (95% CI) | p value | |
|---|---|---|
| Pandemic period | 0.46 (0.25−0.86) | 0.015 |
| Age (every year increase) | 0.96 (0.94−0.97) | <0.001 |
| Male gender | 0.91 (0.52−1.60) | 0.748 |
| Call-to-patient time (every minute increase) | 0.87 (0.82−0.93) | <0.001 |
| Presumed cardiac aetiology | 9.16 (1.89−44.42) | 0.006 |
| Public arrest location | 2.39 (1.44−3.96) | 0.001 |
| Bystander witnessed | 4.32 (2.31−8.09) | <0.001 |
| Bystander CPR | 1.95 (0.93−4.07) | 0.075 |
| Who shocked first (reference PAD): | ||
| First Responder | 0.59 (0.22−1.55) | 0.283 |
| Ambulance Victoria | 0.37 (0.18−0.75) | 0.006 |
OR = odds ratio; CI = confidence interval; CPR = cardiopulmonary resuscitation; PAD = Public Access Defibrillation.
Table 3.
Adjusted odds ratio of the effect of the pandemic period on survival to hospital discharge in patients presenting in a shockable rhythm (VF/VT) with EMS attempted resuscitation.
| OR (95% CI) | p value | |
|---|---|---|
| Pandemic period | 0.50 (0.26−0.96) | 0.037 |
| Age (every year increase) | 0.95 (0.94−0.97) | <0.001 |
| Male gender | 0.75 (0.40−1.40) | 0.364 |
| Call-to-patient time (every minute increase) | 0.88 (0.82−0.94) | <0.001 |
| Presumed cardiac aetiology | 11.68 (1.19−114.88) | 0.035 |
| Public arrest location | 2.17 (1.26−3.73) | 0.005 |
| Bystander witnessed | 2.77 (1.42−5.41) | 0.003 |
| Bystander CPR | 1.38 (0.61−3.09) | 0.436 |
| Who shocked first (reference PAD): | ||
| First Responder | 0.54 (0.20−1.44) | 0.217 |
| Ambulance Victoria | 0.54 (0.26−1.11) | 0.094 |
OR = odds ratio; CI = confidence interval; CPR = cardiopulmonary resuscitation; PAD = Public Access Defibrillation.
Discussion
In contrast to other locations devastated by high incidence of COVID-19 and overwhelmed healthcare systems2, 3, 4, 5, 6, 7, the nature of the impact of COVID-19 was unique in Victoria, Australia during the first wave of infections between 16th March 2020 and 12th May 2020. Strictly imposed social restrictions involving a stay-at-home directive and social distancing resulted in a low burden of COVID-19 disease and a decrease in pre-hospital emergency caseload. Incidence of OHCA did not increase during the pandemic period unlike other countries around the world. In addition, concern regarding increased incidence in OHCA due to a reduction in patients seeking care for urgent cardiac conditions such as acute coronary syndrome was not seen.
We found that rates of attempted resuscitation were significantly decreased during the pandemic period, indicating that paramedics encountered more patients who were deceased on arrival, or paramedics were less aggressive in their resuscitation attempts. Fear of COVID-19 infection may also have influenced paramedic decision-making. Fewer arrests occurred in public locations and fewer patients received early defibrillation. However, rates of bystander CPR significantly increased and, although counterintuitive, it is understandable as people remained at home, often with others, during the pandemic period. We have also shown previously that the most likely person to perform CPR is a family member17. Resuscitation duration in non-survivors was significantly shorter in the pandemic period than in the non-pandemic comparator period. It has been previously reported in patients experiencing in-hospital cardiac arrest that hospitals that were faster at terminating resuscitation on non-survivors had lower survival rates compared to hospitals that continued resuscitation for longer18. It is, therefore, possible that early withdrawal of care may have contributed to the observed reduction in survival. For patients presenting in a shockable rhythm, median resuscitation duration was significantly longer in the pandemic period. Although this suggests that paramedics were not systematically terminating resuscitation earlier, longer resuscitation duration has also been shown to be associated with poorer neurological outcome and decreased survival19.
Survival from OHCA was significantly adversely impacted during the COVID-19 pandemic period (March – May 2020) in Victoria. Our data suggests that survival was impacted by increased delays to care, fewer public arrests, and fewer shocks by PAD/first responders. Despite adjusting for these factors and other known influencing factors, however, the risk-adjusted odds of survival remained 50% lower during the pandemic period, suggesting that additional factors in pre-hospital arrest management and in post-arrest care provided by receiving hospitals may have also influenced patient outcomes. Other changes to processes-of-care, for example, earlier introduction of mechanical CPR and intubation, and de-emphasising the use of aerosol-generating procedures (e.g. airway suctioning) may have influenced patient outcomes by reducing hands-on-chest time and CPR quality. In addition, it is possible that changes to in-hospital practices also contributed to these reductions in survival. This could be due to changes in the patterns of care and approach to post-resuscitation interventions (e.g. targeted temperature management and percutaneous coronary intervention). Also unknown is the possibility of patients delaying seeking medical attention for treatable cardiac symptoms in the time prior to OHCA due to reduced primary and tertiary care in the COVID era20.
Fewer countries have experienced lower incidence and lower case-fatality rates from COVID-19 than Australia during the first wave of the pandemic. Other reports providing insights into OHCA during COVID-19 have come from France, Italy, UK, and the USA where COVID-19 incidence has been over 2.5 to 11-fold higher than in Victoria during the pandemic period defined in this study16. Case-fatality rates have been between 4.5 and 15-fold higher16. Seattle/King County (USA) and Padua (Italy) similarly reported no increase in OHCA incidence during the COVID-19 pandemic5, 6 but in Victoria, we demonstrated no increase in OHCA incidence, low COVID-19 incidence, and low COVID-19 case-fatality. Findings out of Padua also reported delays in key response time intervals (call-to-dispatch and dispatch-to-departure)7, however, the major delays we identified occurred after arrival at scene. These differences in COVID-19 incidence, case-fatality and time delays make the experience in Australia unlike that of others. The indirect influence of the pandemic on the OHCA system-of-care is potentially almost exclusively the result of social restrictions and personal protective practices. This highlights that efforts should be focused on maintaining the chain-of-survival in the pre-hospital setting. Given that a significant increase in the mortality rate of OHCA was identified during the pandemic period in Victoria, EMS pandemic preparedness not only requires planning and control of the disease itself, but optimisation of the response to OHCA.
Limitations
There are some limitations of this work that require comment. The observational study design has inherent risks of bias that cannot be controlled for and causality cannot be inferred. We were unable to account for migration out of Melbourne during the pandemic which may have influenced OHCA incidence. Multiple comparisons for patient and arrest characteristics were not performed due to study size and the exploratory nature of this work. Differences in comorbidities between patients in the pandemic period and comparator period are not known and may have influenced patient outcomes. Given the size of the pandemic period in our study, we were unable to adjust for clustering effects and temporal factors. We also did not examine CPR performance data during the pandemic period. The distinction between mediating and confounding factors and the impact of these on outcomes also requires investigation.
Conclusion
While other international studies have seen high incidence of COVID-19 and attributed decreased survival from OHCA to high COVID-19 infection rates, we demonstrated no such impact to OHCA patient outcomes in a context of low COVID-19 incidence, low case-fatality rate and no COVID-19 positive OHCA patients. Instead, we demonstrated that COVID-19 initiated collateral damage to the OHCA system-of-care in Victoria, resulting in significantly longer delays to key time-sensitive interventions. However, this did not completely explain reductions in survival. Further research is required to understand additional management factors and potential in-hospital factors that may have influenced patient survival.
Contributions
All authors have made substantial contributions to this Report including in all the following: (1) the conception and design of the study, analysis and interpretation of data. (2) drafting the article and revising it critically for important intellectual content, and (3) final approval of the version submitted.
Conflicts of interest
The authors have no conflicts of interest to declare.
Acknowledgements
JB (APP1112829) and ZN (APP1146809) are supported by Early Career Fellowships from the National Health and Medical Research Council of Australia. JB is also supported by a Postdoctoral Fellowship (Award Reference 100950) from the National Heart Foundation of Australia.
Footnotes
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.resuscitation.2020.09.017.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Ball J., Smith K. 2020. The Victorian Ambulance Cardiac Arrest Registry 2018-2019 Annual Report. Blackburn North, Victoria: Ambulance Victoria. [Google Scholar]
- 2.Baldi E., Sechi G.M., Mare C. Out-of-Hospital Cardiac Arrest during the Covid-19 Outbreak in Italy. N Engl J Med. 2020;383:496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Daily Chart . 2020. Deaths from cardiac arrests have surged in New York City. The Economist.https://www.economist.com/graphic-detail/2020/04/13/deaths-from-cardiac-arrests-have-surged-in-new-york-city) (Accessed 14th April 2020 at: [Google Scholar]
- 4.Marijon E., Karam N., Jost D. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020;5:E437–43. doi: 10.1016/S2468-2667(20)30117-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baldi E., Sechi G.M., Mare C. COVID-19 kills at home: the close relationship between the epidemic and the increase of out-of-hospital cardiac arrests. Eur Heart J. 2020 doi: 10.1093/eurheartj/ehaa508. ehaa508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lai P.H., Lancet E.A., Weiden M.D. Characteristics Associated With Out-of-Hospital Cardiac Arrests and Resuscitations During the Novel Coronavirus Disease 2019 Pandemic in New York City. JAMA Cardiol. 2020:e202488. doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paoli A., Brischigliaro L., Scquizzato T., Favaretto A., Spagna A. Out-of-hospital cardiac arrest during the COVID-19 pandemic in the Province of Padua, Northeast Italy. Resuscitation. 2020;154:47–49. doi: 10.1016/j.resuscitation.2020.06.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.International Liaison Committee on Resuscitation (ILCOR) 2020. COVID-19 infection risk to rescuers from patients in cardiac arrest. Consensus on Science with Treatment Recommendations [Internet] Brussels, Belgium: International Liaison Committee on Resuscitation (ILCOR)http://ilcor.org March 30. Available from: [Google Scholar]
- 9.Australian Resuscitation Council (ARC) 2020. ARC Statements on COVID-19. Australian Resuscitation Council.https://resus.org.au/guidelines/ Available from: [Google Scholar]
- 10.American Heart Association . 2020. Interim Guidance for Healthcare Providers during COVID-19 Outbreak.https://cpr.heart.org/en/resources/coronavirus-covid19-resources-for-cpr-training 19 March [Internet]. Available at: [Google Scholar]
- 11.Australian Government Department of Health . 2020. Guidance on the use of personal protective equipment (PPE) in hospitals during the COVID-19 outbreak. Australian Government Department of Health.https://www.health.gov.au/resources/publications/guidance-on-the-use-of-personal-protective-equipment-ppe-in-hospitals-during-the-covid-19-outbreak) (Accessed 24th August, at: [Google Scholar]
- 12.Australian Government Department of Health . 2020. Coronavirus Disease (COVID-19): Information for paramedics and ambulance first responders. Australian Government Department of Health.https://www.health.gov.au/resources/publications/coronavirus-covid-19-information-for-paramedics-and-ambulance-first-responders) (Accessed 24th August, at: [Google Scholar]
- 13.Nehme Z., Bernard S., Cameron P. Using a cardiac arrest registry to measure the quality of emergency medical service care: decade of findings from the Victorian Ambulance Cardiac Arrest Registry. Circ Cardiovasc Qual Outcomes. 2015;8:56–66. doi: 10.1161/CIRCOUTCOMES.114.001185. [DOI] [PubMed] [Google Scholar]
- 14.Australian Bureau of Statistics . 2020. Australian Demographic Statistics, “Table 52. Estimated Resident Population By Single Year of Age, Victoria”, time series spreadsheet, cat. no. 3101.0.52. Australian Bureau of Statistics.https://www.abs.gov.au/ausstats/abs@.nsf/mf/3101.0 Available at: [Google Scholar]
- 15.2020. Victorian coronavirus (COVID-19) data. Victorian Department of Health and Human Services.https://www.dhhs.vic.gov.au/victorian-coronavirus-covid-19-data) (Accessed 24th August 2020, at: [Google Scholar]
- 16.Centres for Disease Control and Prevention (CDC) COVID Data Tracker . 2020. Centres for Disease Control and Prevention.https://covid.cdc.gov/covid-data-tracker/?utm_source=morning_brew#cases) (Accessed 24th August 2020 at: [Google Scholar]
- 17.Haskins B., Smith K., Cameron P. The impact of bystander relation and medical training on out-of-hospital cardiac arrest outcomes. Resuscitation. 2020;150:72–79. doi: 10.1016/j.resuscitation.2020.02.036. [DOI] [PubMed] [Google Scholar]
- 18.Goldberger Z.D., Chan P.S., Berg R.A. Duration of resuscitation efforts and survival after in-hospital cardiac arrest: an observational study. Lancet. 2012;380:1473–1481. doi: 10.1016/S0140-6736(12)60862-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nehme Z., Andrew E., Bernard S., Smith K. Impact of cardiopulmonary resuscitation duration on survival from paramedic witnessed out-of-hospital cardiac arrests: An observational study. Resuscitation. 2016;100:25–31. doi: 10.1016/j.resuscitation.2015.12.011. [DOI] [PubMed] [Google Scholar]
- 20.Nehme Z., Bernard S., Andrew E., Cameron P., Bray Je, Smith K. Warning symptoms preceding out-of-hospital cardiac arrest: Do patient delays matter? Resuscitation. 2018;123:65–70. doi: 10.1016/j.resuscitation.2017.12.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.